Abstract
Two variants of equine infectious anemia virus (EIAV) that differed in sensitivity to broadly neutralizing antibody were tested in direct competition assays. No differences were observed in the growth curves and relative fitness scores of EIAVs of principal neutralizing domain variants of groups 1 (EIAVPND-1) and 5 (EIAVPND-5), respectively; however, the neutralization-resistant EIAVPND-5 variant was less infectious in single-round replication assays. Infectious center assays indicated similar rates of cell-to-cell spread, which was approximately 1,000-fold more efficient than cell-free infectivity. These data indicate that efficient cell-to-cell spread can overcome the decreased infectivity that may accompany immune escape and should be considered in studies assessing the relative levels of fitness among lentivirus variants, including HIV-1.
TEXT
Equine infectious anemia virus (EIAV) induces a persistent lifelong infection characterized by recurrent febrile episodes. Eventually, most horses exert immunological control over replicating virus and enter a prolonged period of clinical quiescence associated with the presence of cytotoxic T cells and broadly neutralizing antibody (bNAb). Over time, however, viral genotypes that resist bNAb evolve, resulting in recrudescence of clinical disease (6, 12). Elucidating mechanisms of viral escape from bNAb is important for the design of effective vaccines for EIAV and related lentiviruses, such as HIV-1.
The V3 region of the EIAV surface envelope glycoprotein (SU) is structurally similar to HIV-1 V1/V2 (5), contains two epitopes recognized by neutralizing monoclonal antibodies (1), and is termed the principal neutralizing domain (PND). Genetic variation in the PND is considered to play an important role in immune escape and EIAV persistence. We previously undertook a longitudinal study of variation in the V2-V4 region of EIAV SU in a pony experimentally inoculated with the virulent Wyo2078 strain of EIAV (EIAVWyo2078) (12). The predominant PND variants clustered into 5 groups, designated PND-1 to PND-5. Genotypes representative of each group were used to generate chimeric infectious molecular clones, designated EIAVPND-1 through EIAVPND-5, that differed only in the V2-V4 region of SU (12). As infection progressed, the chimeric PND virus variants showed increasing resistance to neutralization by autologous and heterologous sera, such that EIAVPND-1 was highly sensitive to neutralization by broadly neutralizing sera, whereas EIAVPND-5 was neutralization resistant (12, 14). Genetic differences in the PND region included amino acid substitutions, size variation, and changes in the numbers and locations of predicted N-linked glycosylation sites. Similar changes in HIV-1 env that mask immune epitopes have been associated with a loss of virus replicative fitness (8–11), suggesting that resistance to bNAb may incur a cost in virus fitness. In the present study, we used growth competition and infectivity assays to determine if EIAV PND variants that differ in sensitivity to neutralization also differ in replicative capacity in vitro.
Direct growth competition experiments were used to determine the relative fitness of chimeric EIAVPND-1 and EIAVPND-5. Equine dermis (ED; ATCC CCL57) cells were inoculated with equivalent numbers of focus-forming units (FFU) of EIAVPND-1 and/or EIAVPND-5 at a multiplicity of infection (MOI) of 0.001 for each virus. Supernatant and cells were collected every 3 days, and supernatant virus and provirus copy numbers were determined by quantitative PCR (Q-PCR). The EIAVPND-1 and EIAVPND-5 genotypes were distinguished using PND-specific primers targeted to the V3 region and a fluorescence probe targeted to a conserved region of env (Table 1). The specificity, sensitivity, and efficiency of the Q-PCR assay were tested in reaction mixtures containing various ratios of PND-1 and PND-5 plasmid DNA and by comparing PND-specific primers/probes with EIAV Gag-specific primers/probes by using proviral DNA templates. Viral RNA was isolated from 140 μl of supernatant using the Qiagen viral RNA isolation minikit and amplified by reverse transcription-PCR (RT-PCR) using the TaqMan RNA-to-CT one-step kit (Applied Biosystems). Each PND genotype was amplified in a separate reaction mixture containing a PND-specific primer pair, and an external standard curve was generated from serial dilutions of EIAV19 Env plasmid DNA using common primers and a common probe. Total cellular DNA was isolated with the Qiagen blood cell DNA isolation kit, and the proviral copy number was determined using primers and probes described for viral RNA. The ED cell copy number was quantified using equine β2 M-specific primers and an equine β2 M-specific probe (Table 1). Genomic DNA isolated from 1 × 107 ED cells was serially diluted to generate a standard curve for cell copy number, and results are reported as numbers of proviral copies/104 cells.
Table 1.
Primer and probe sequences used in this study
| Target | Primer or probea | Sequence (5′–3′)b |
|---|---|---|
| EIAV Env | Common forward | CGG GGT GTA GAC CAT TTC AA |
| Common reverse | TGA CAA TGA TCA CTA TCT GTG CAA | |
| Common probe | HEX-TTA TGA GAC CAA TAG AAG CAT GCA-3IALK_FQ | |
| PND-1 reverse | TCC GTA CTC TCA TTT ACA GGG T | |
| PND-5 reverse | CAG TAA GGG TCG GAG GAA CCT G | |
| EIAV Gag | Gag forward | AGC CAG GAC ATT TAT CTA GTC AAT GTA GAG CAC C |
| Gag reverse | GTG CTG ACT CTT CTG TTG TAT CGG GAA AGT TTG | |
| Gag probe | 56-FAM-ACG GGA AGC AAG GGG CTC AAG GGA GGC C-3IALK_FQ | |
| Luciferase | Firefly luc forward | TAT GAA GAG ATA CGC CCT GGT T |
| Firefly luc reverse | GCC CAT ATC GTT TCA TAG CTT C | |
| Renilla luc forward | GCA ATA GTT CAC GCT GAA AGT G | |
| Renilla luc reverse | CAA CAT GGT TTC CAC GAA GAA GT | |
| Pseudovirus RNA | WHV PRE forward | CTG TTC CTG TTA ATC AAC CTC TGG |
| WHV PRE reverse | ATA CAA GGA GGA GAA AAC GAA AGC | |
| Equine β2M | E-β2M forward | TCT TTC AGC AAG GAC TGG TCT TT |
| E-β2M reverse | CTA CCA CAC CAT TGG GAG TAA A | |
| E-β2M probe | 56-ROXN-ATC TTC TGG TCC ATA CTG A-3IAbRQSp |
luc, luciferase; E-β2M, equine β2 microglobulin.
HEX, hexachlorofluorescein; 3IALK_FQ, Iowa Black FQ quencher (IDT); 56-FAM, 5,6-carboxyfluorescein; 56-ROXN, carboxy-X-rhodamine; 3IAbRQSp, Iowa Black FQ quencher (IDT).
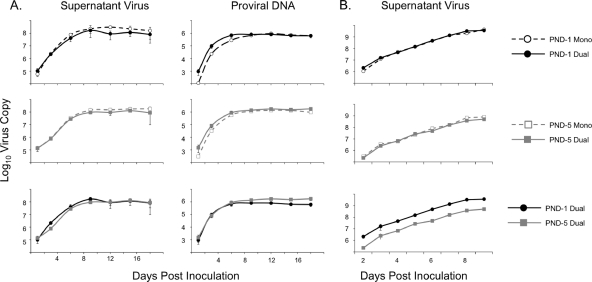
The relative levels of fitness of EIAVPND-1 and EIAVPND-5 were compared in the presence and absence of a competitor virus (Fig. 1). Supernatant virus production from EIAVPND-1-infected cells was remarkably similar to that of EIAVPND-5-infected cells, with respect to both the kinetics of virus production and the maximal output (Fig. 1A). Analysis of proviral copy numbers indicated that the viruses spread through the culture at fairly equivalent rates. Further, the presence of a competitor had no effect on either virus production or cell spread. Competition studies were also performed using virus inocula normalized by virus copy number (6 × 105 copies/well). Under these conditions, there was less supernatant virus produced from EIAVPND-5-infected cells than from cells infected with EIAVPND-1 (Fig. 1B). The decreased virion production appeared to be due to some difference occurring before day 3, since kinetics of virus production were similar after day 3.
Fig. 1.
In vitro competition between EIAVPND-1 and EIAVPND-5. (A) Results of competition studies using inocula normalized by multiplicity of infection. ED cells were inoculated in triplicate with EIAVPND-1 and/or EIAVPND-5, and the replication kinetics of each virus in singly (Mono) or dually infected cells was assessed by measuring supernatant virion production and provirus-infected cells. (B) Results of competition using inocula normalized by RNA copy number. ED cells were inoculated in triplicate with EIAVPND-1 and/or EIAVPND-5. Supernatant was collected at sequential times postinfection for quantitation of virion production. Results are the means ± standard deviations of values from triplicate wells assayed in duplicate.
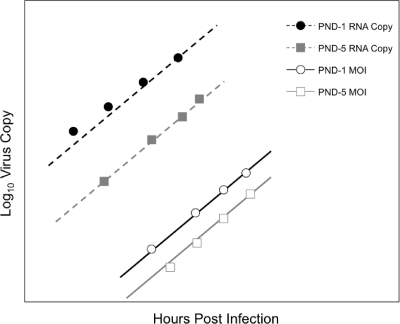
To estimate the relative fitness of EIAVPND-1 and EIAVPND-5, a model of virus exponential growth was fitted to data from all multiround growth assays (Fig. 2). All competition experiments were carried out in duplicate, and each included both single infection with EIAVPND-1 or EIAVPND-5 and a competition infection with both viruses. There was no obvious difference between the results of the single- and dual-infection experiments, especially during the exponential growth phase, so all data were fit simultaneously to enhance power. Visual examination of the data suggested that the exponential part of the growth curve extended from greater than 24 h to less than 168 h (7 days). During this time, the levels of growth of both viruses were similar, and there was no significant difference between the virus growth rates (P = 0.51). Specifically, the fitness of EIAVPND-5 relative to that of EIAVPND-1 was 0.999, with a 95% confidence interval of 0.995 to 1.003. Therefore, the genetic changes in PND-5 that conferred increased resistance to neutralization were not accompanied by a loss in fitness, as measured in multiple-round growth assays in ED cells.
Fig. 2.
Fitting of the competition data to the mathematics model. Copy number (log10) of virus as a function of time for the exponential growth phase of the two competition experiments. For each experiment/virus combination, there were four sets of data, results from duplicates of the single infection and those from duplicates of the dual infection. The lines are the estimated models. A fitness difference between EIAV variants PND-1 and PND-5 would manifest as a difference in slopes for the two viruses.
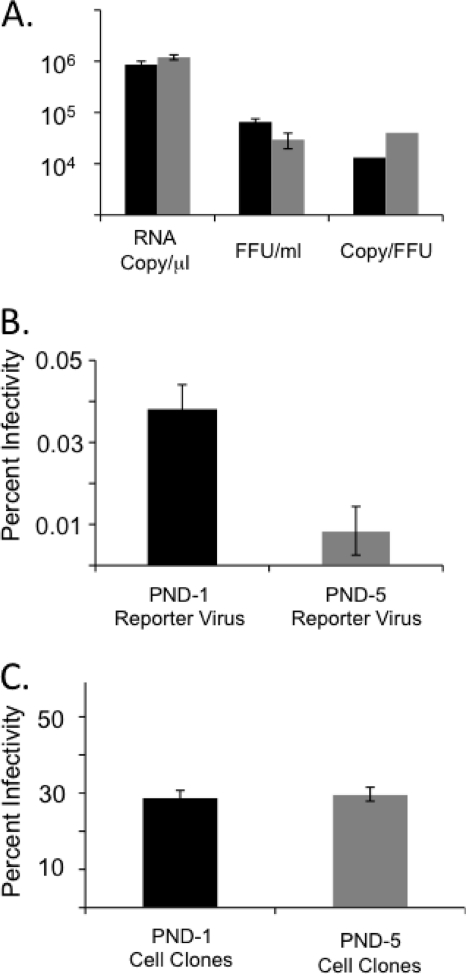
We next explored possible differences in infectivity between PND-1 and PND-5 genotypes. The EIAVPND-5 stocks were consistently less infectious than the EIAVPND-1 stocks, as determined by numbers of FFU/ml (Fig. 3A). On a per-milliliter basis, there were, on average, significantly more virus copies (P = 1 × 10−6) but fewer FFU (P = 2 × 10−9) in the EIAVPND-5 stocks than in the EIAVPND-1 stocks. This resulted in EIAVPND-5 having an approximately 3-fold-higher particle/infectivity ratio than EIAVPND-1, suggesting that EIAVPND-5 is less infectious than EIAVPND-1. To test this hypothesis, we generated replication-defective PND-1 and PND-5 Env-pseudotyped luciferase reporter viruses for analysis in single-cycle infectivity assays. Both firefly luciferase and Renilla luciferase reporter viruses were generated for each PND Env, allowing us to quantify infectivity in coinfected cells by Q-PCR of proviral DNA using luciferase-specific primers. PND-chimeric Env expression plasmids, pLG.PND-1 and pLG.PND-5, were generated by cloning the V2-V4 region of PND-1 or PND-5 into pLGcoSUTM (13), and pseudotyped viruses were produced in HEK 293T cells using an EIAV-based reporter virus system (13). Supernatant pseudovirus copy number was determined by real-time RT-PCR using the Power SYBR green RNA-to-CT one-step kit (Applied Biosystems) and primers targeted to the woodchuck hepatitis virus posttranscriptional regulatory element (WHV PRE).
Fig. 3.
Infectivity of EIAV variants PND-1 (black bars) and PND-5 (gray bars). (A) Cell-free infectivity of EIAVPND-1 and EIAVPND-5 stocks. The RNA copy number and infectious titer (focus-forming units/ml) represent the virus effects ± 1 standard deviation, as estimated from a linear mixed-effect model. (B) Single-cycle infectivity of PND-1- and PND-5-pseudotyped viruses carrying the firefly or Renilla luciferase reporter gene. ED cells were coinfected with equal RNA copy numbers of the viruses, and infectivity was calculated as a ratio, the number of infected cells per RNA copy number. (C) Cell-associated infectivity of EIAVPND-1 and EIAVPND-5, as determined by infectious center assay. Infectivity is calculated as a ratio, the number of infected target cells per donor cell. Two independent cell clones for each virus were assayed in triplicate, and the estimates represent the virus effects ± 1 standard deviation in a linear mixed-effect model, where the cell clone is a random effect.
ED cells seeded at 2 × 105 cells per well in 12-well culture plates were transduced with 2 × 109 copies of pseudotyped reporter viruses, expressing either the firefly or the Renilla luciferase gene. After 6 h, medium was replaced, and cells were expanded in culture for 3 days. Proviral copy number was quantified by real-time Q-PCR using the Power SYBR green PCR master mix (Applied Biosystems) and primers specific for the firefly or Renilla luciferase gene. The total cell copy number was determined using primers targeted to the equine β2 M gene. Using all experiments, we estimated that 0.038% of PND-1 Env pseudoviruses were infectious and that a significantly smaller 0.0084% of PND-5 Env pseudoviruses were infectious (P = 0.00013) (Fig. 3B). This 4.5-fold difference in infectivity is similar to the differences in the particle/infectivity ratios (Fig. 3A) and indicates that changes in the PND region of EIAV SU conferring increased resistance to neutralizing antibody were accompanied by a reduction in virus infectivity.
The PND-5 Env pseudovirus was 4.5-fold less infectious than PND-1, yet the differences in infectivity were not amplified over multiple rounds of virus replication in vitro, as indicated by the results of the direct competition assays (Fig. 1). Lentivirus transmission can also occur via cell-to-cell spread, which can be more efficient than cell-free infection (2–4, 7). To determine if cell-to-cell spread compensated for the differences in cell-free infectivity, we used infectious center assays to measure the efficiency of cell-to-cell spread of the PND variants. Cf2th proviral cell clones stably infected with EIAVPND-1 or EIAVPND-5 (12) were diluted to 1 × 106 cells per ml, exposed to 25 μg/ml of mitomycin C for 30 min at 37°C, and added to 1 × 105 indicator ED cells per well in a 12-well culture plate. Replicate wells not seeded with ED target cells were used as controls. Three days after infection, cells were fixed in methanol and foci of EIAV-infected cells were enumerated, following immunohistochemistry using EIAV convalescent-phase immune sera. Infectivity was calculated as the ratio of infected target cell foci to donor cells. Each infectious center assay used two independent cell lines for each virus. The EIAVPND-1- and EIAVPND-5-infected cells were similar in efficiency of cell-to-cell spread (P value = 0.8), with infectivity of approximately 30% (Fig. 3C). No viable cells were detected in the absence of ED target cells (not shown). We conclude that transmission via cell-to-cell spread is approximately 1,000 times more efficient than transmission via cell-free virus (Fig. 3B and C). This difference in transmission efficiency could easily compensate for differences in cell-free infectivity over multiple rounds of replication. As such, cell-to-cell spread should be considered in studies that examine the relative fitness of lentivirus variants, including HIV-1.
In summary, our results indicate that resistance to neutralization by heterologous antibody was accompanied by a 4-fold loss in cell-free virus infectivity. However, efficient cell-to-cell spread compensated for differences in cell-free infectivity such that PND variants did not differ in relative fitness, as measured in direct competition assays over multiple rounds of replication. Efficient cell-to-cell spread may be an important factor in immune evasion and virus persistence.
Acknowledgments
We thank Cierra Pairett and Brett Sponseller for helpful discussions.
This work was supported in part by U.S. Public Health Service, National Institutes of Health grants CA128568 (S.C.) and AI073101 (R.H.M.).
Footnotes
Published ahead of print on 13 July 2011.
REFERENCES
- 1. Ball J. M., Rushlow K. E., Issel C. J., Montelaro R. C. 1992. Detailed mapping of the antigenicity of the surface unit glycoprotein of equine infectious anemia virus by using synthetic peptide strategies. J. Virol. 66:732–742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bangham C. R. 2003. The immune control and cell-to-cell spread of human T-lymphotropic virus type 1. J. Gen. Virol. 84:3177–3189 [DOI] [PubMed] [Google Scholar]
- 3. Carr J. M., Hocking H., Li P., Burrell C. J. 1999. Rapid and efficient cell-to-cell transmission of human immunodeficiency virus infection from monocyte-derived macrophages to peripheral blood lymphocytes. Virology 265:319–329 [DOI] [PubMed] [Google Scholar]
- 4. Gupta P., Balachandran R., Ho M., Enrico A., Rinaldo C. 1989. Cell-to-cell transmission of human immunodeficiency virus type 1 in the presence of azidothymidine and neutralizing antibody. J. Virol. 63:2361–2365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hotzel I. 2003. Conservation of the human immunodeficiency virus type 1 gp120 V1/V2 stem/loop structure in the equine infectious anemia virus (EIAV) gp90. AIDS Res. Hum. Retroviruses 19:923–924 [DOI] [PubMed] [Google Scholar]
- 6. Howe L., Leroux C., Issel C. J., Montelaro R. C. 2002. Equine infectious anemia virus envelope evolution in vivo during persistent infection progressively increases resistance to in vitro serum antibody neutralization as a dominant phenotype. J. Virol. 76:10588–10597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Igakura T., et al. 2003. Spread of HTLV-I between lymphocytes by virus-induced polarization of the cytoskeleton. Science 299:1713–1716 [DOI] [PubMed] [Google Scholar]
- 8. Joos B., et al. 2005. Low human immunodeficiency virus envelope diversity correlates with low in vitro replication capacity and predicts spontaneous control of plasma viremia after treatment interruptions. J. Virol. 79:9026–9037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lobritz M. A., Marozsan A. J., Troyer R. M., Arts E. J. 2007. Natural variation in the V3 crown of human immunodeficiency virus type 1 affects replicative fitness and entry inhibitor sensitivity. J. Virol. 81:8258–8269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marozsan A. J., et al. 2005. Differences in the fitness of two diverse wild-type human immunodeficiency virus type 1 isolates are related to the efficiency of cell binding and entry. J. Virol. 79:7121–7134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rangel H. R., et al. 2003. Role of the human immunodeficiency virus type 1 envelope gene in viral fitness. J. Virol. 77:9069–9073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sponseller B. A., et al. 2007. Immune selection of equine infectious anemia virus env variants during the long-term inapparent stage of disease. Virology 363:156–165 [DOI] [PubMed] [Google Scholar]
- 13. Tallmadge R. L., et al. 2008. Development and characterization of an equine infectious anemia virus Env-pseudotyped reporter virus. Clin. Vaccine Immunol. 15:1138–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Taylor S. D., Leib S. R., Carpenter S., Mealey R. H. 2010. Selection of a rare neutralization-resistant variant following passive transfer of convalescent immune plasma in equine infectious anemia virus-challenged SCID horses. J. Virol. 84:6536–6548 [DOI] [PMC free article] [PubMed] [Google Scholar]