Abstract
Viscum album (VA) preparations are extensively used as complementary therapy in cancer and are shown to exert anti-tumor activities which involve the cytotoxic properties, induction of apoptosis, inhibition of angiogenesis and several other immunomodulatory mechanisms. In addition to their application in cancer therapy, VA preparations have also been successfully utilized in the treatment of several inflammatory pathologies. Owing to the intricate association of inflammation and cancer and in view of the fact that several anti-tumor phytotherapeutics also exert a potent anti-inflammatory effect, we hypothesized that VA exerts an anti-inflammatory effect that is responsible for its therapeutic benefit. Since, inflammatory cytokine-induced cyclo-oxygenase-2 (COX-2) and prostaglandin E2 (PGE2) play a critical role in the pathogenesis of inflammatory diseases, we investigated the anti-inflammatory effect of VA on regulation of cyclo-oxygenase expression and PGE2 biosynthesis by using human lung adenocarcinoma cells (A549 cells) as a model. A549 cells were stimulated with IL-1β and treated with VA preparation (VA Qu Spez) for 18 hours. PGE2 was analysed in the culture supernatants by enzyme immunoassay. Expression of COX-2 and COX-1 proteins was analyzed by immunoblotting and the expression of COX-2 mRNA was assessed by semi-quantitative RT-PCR. We found that VA Qu Spez inhibit the secretion of IL-1β-induced PGE2 in a dose-dependent manner. Further, we also show that this inhibitory action was associated with a reduced expression of COX-2 without modulating the COX-1 expression. Together these results demonstrate a novel anti-inflammatory mechanism of action of VA preparations wherein VA exerts an anti-inflammatory effect by inhibiting cytokine-induced PGE2 via selective inhibition of COX-2.
Introduction
VA preparations are standardized aqueous extracts of Viscum album L. (commonly known as European mistletoe, a semi-parasite that grows on different host trees), composed mainly of mistletoe lectins and viscotoxins [1]–[3] and several other biologically active molecules like flavonoids, several enzymes, peptides (such as viscumamide), amino acids, thiols, amines, polysaccharides, cyclitoles, lipids, phytosterols, triterpines, phenylpropanes and minerals [4]. Based on the host tree and the method of extraction, currently at least three VA preparations are available for therapeutic application: VA Qu Spez (oak tree), VA P (pini) and VA M (mali). For a long time, VA preparations have been used as complementary therapy for several types of cancer, mainly in Europe and also to some extent in other parts of the world [5], [6]. Therapeutic benefit of VA preparations when utilized along with surgery, chemotherapy or radiotherapy contributes to the overall improvement in the quality of life in cancer patients [7]–[10]. In addition, VA preparations are also implicated as conventional phytotherapeutics in the treatment of several conditions associated with the nervous system abnormalities, allergic reactions, and immuno-inflammatory disorders [11]–[16].
Despite their use for the past several decades, the precise mechanisms associated with anti-tumoral effects of VA are not completely understood. Several mutually non-exclusive mechanisms have been proposed, which include induction of apoptosis and cytotoxicity in tumor cells and inhibition of process of angiogenesis [10]–[22]. VA preparations also exert several immuno-stimulatory mechanisms by interacting with the cellular and humoral compartments of the immune system thus potentiating an anti-tumor immune response [22]–[30]. However, the mechanisms of action of Viscum album underlying their therapeutic benefits in inflammatory pathologies are yet to be explored. In this study, we therefore investigated the anti-inflammatory mechanisms of VA preparations.
Inflammation is a basal physiological phenomenon that occurs as a complex set of responses to an infectious agent or to a tissue injury so as to eliminate the causative agent and to initiate the healing process. It is a physiopathological symptom in a variety of conditions of infectious, autoimmune or of tumoral origin. Interaction of innate and adaptive immune cells as well as non-immune cells such as endothelial cells and fibroblasts with inflammatory stimulus induces the production of several molecular mediators such as cytokines, chemokines, bioactive amines, eicosanoids, and products of proteolytic cascades, such as bradykinin [31]–[37]. These inflammatory mediators acts on various target tissues and exert changes in their homeostatic functions and therefore inflammation has to be kept in check which can be acieved by various anti-inflammatory agents including steroids, non-steroidal antiinflammatory agents, intravenousimmunoglobulins, immunosuppressor cells, neutralizing monoclonal antibodies to inflammatory cytokines [38]–[45].
PGE2, a derivative of eicosanoids, plays an important role as molecular mediator of inflammatory response. Overproduction of PGE2 is observed in many of the human pathologies associated with inflammation and pro-tumoral condition [46]–[49]. PGE2 is synthesized by cyclo-oxygenases, COX-1 (expressed constitutively) and COX-2 (induced in response to inflammatory stimulus). COX-2 is transcriptionaly activated and over expressed in response to many pro-inflammatory stimuli like IL-1β, IFN-γ, TNF-α and also pathogen stimuli such as lipopolysaccharides leading to an enhanced biosynthesis of PGE2 [50]. Therefore, pharmacological strategies to suppress the COX-2 expression and PGE2 secretion are of great interest and are being exploited to develop potent therapeutics to resolve inflammation and several pro-tumor conditions [51]–[56]. Indeed, several phytotherapeutics and plant-derived molecules like curcumin, some of the flavonoids and polyphenols that have anti-tumor properties also exert anti-inflammatory activity by down-regulating the expression of COX-2 and PGE2 biosynthesis [57]–[67]. Though there are few reports showing anti-inflammatory activity of certain molecules isolated from Viscum album, precise mechanisms of action associated with its therapeutic benefit are yet to be explored [68], [69].
Here, we therefore examined the hypothesis that VA exerts anti-inflammatory effect by interfering with the expression and biochemical functioning of COX-2 which explains in part, the mechanisms of actions of VA in several inflammatory pathologies.
Results
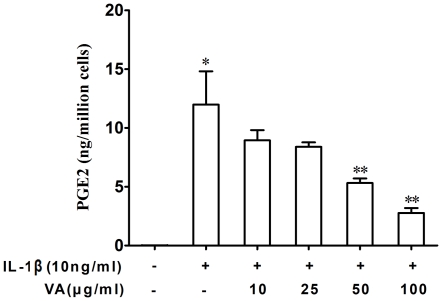
Viscum album inhibits cytokine-induced PGE2 secretion in A549 cells
Human lung adenocarcinoma-derived A549 cells were stimulated with IL-1β for 18 hours in the presence or absence of VA Qu Spez, a therapeutic preparation of Viscum album that grows on oak trees. PGE2 was estimated in the culture supernatants by enzyme immunoassay as explained in Materials and Methods. Inflammatory cytokine IL-1β significantly induced the secretion of PGE2. We found that VA Qu Spez inhibits the IL-1β-induced PGE2 secretion in a dose-dependent manner (Figure 1). At 50 µg/ml and 100 µg/ml, VA Qu Spez significantly inhibited the secretion of IL-1β-induced PGE2 secretion.
Figure 1. Inhibition of PGE2 secretion by Viscum album in A549 cells.
Cells were treated with IL-1β (10 ng/ml) and increasing concentrations of VA Qu Spez for 18 hours. PGE2 was analyzed in culture supernatants by EIA. Results are mean±SEM from 4 independent experiments (*p<0.05 versus control cells, **p<0.05 versus cells treated with IL-1β, analyzed by paired Student-t-test).
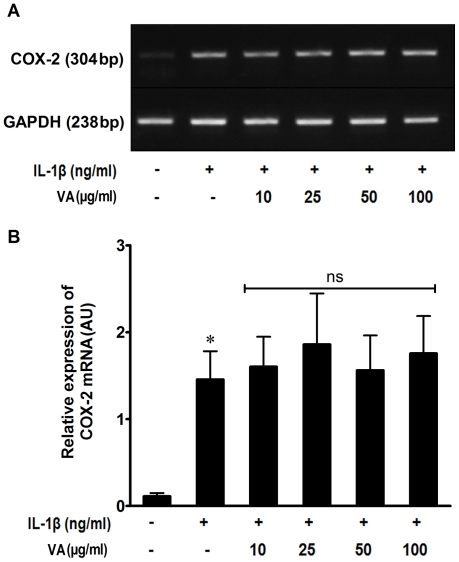
Viscum album does not inhibit the cytokine-induced COX-2 mRNA expression
Since the induction of PGE2 by pro-inflammatory cytokines is known to be associated with the over expression of cox-2 gene, we analyzed the modulation of mRNA expression of COX-2 by VA. IL-1β stimulated-A549 cells were harvested following the treatment with VA Qu Spez and their total cellular RNA was subjected to reverse transcription and polymerase chain reaction. Unstimulated cells showed a basal amount of COX-2 mRNA and it was significantly up-regulated by IL- 1β. However, we found that VA Qu Spez did not inhibit the cytokine-induced COX-2 mRNA expression (Figure 2). Indeed, no significant change in the amount of COX-2 mRNA expression was observed even at the highest concentration of VA (100 µg/ml) used in our experiment.
Figure 2. Effect of VA Q Spez on IL-1β-induced COX-2 transcription.
Total cellular RNA was isolated from A549 cells that were cultured either in medium alone or stimulated with IL-1β (10 ng/ml) with or without various concentrations of VA for 18 hours. mRNA expression of COX-2 was analyzed by semi quantitative RT-PCR using COX-2-specific primers. Amplification of a house keeping gene GAPDH is used as an internal control. (A) PCR products were separated on 1% agarose gel and a representative gel picture is shown. (B) Relative expression (mean ± SEM) of COX-2 mRNA from six independent experiments as quantified by densitometry (ratio of density of COX-2: that of GAPDH). * P<0.05 analyzed by paired Student-t-test, ns refers to non-significant, compared to IL-1β stimulated cells.
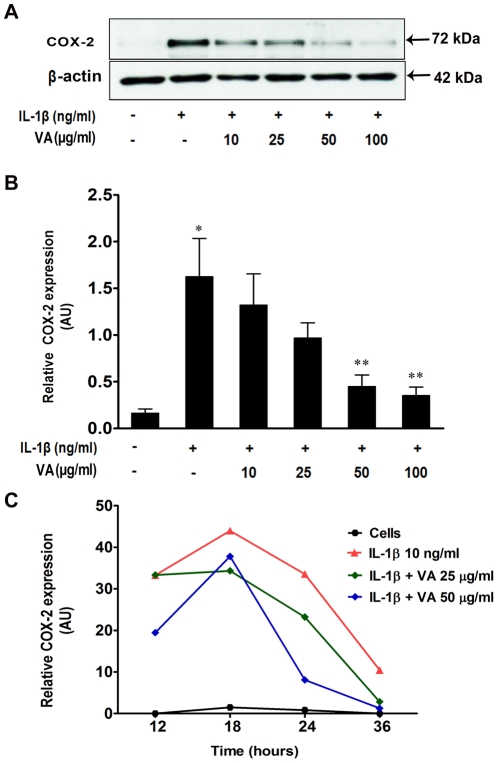
Viscum album inhibits cytokine-induced COX-2 protein expression
In order to investigate whether VA-mediated inhibition of the cytokine-induced PGE2 secretion (Figure 1) correlated with the reduced level of COX-2 protein, we analyzed the expression of COX-2 protein in IL-1β-stimulated cells following VA treatment, by immunoblotting.
Figure 3A depicts a representative blot of the expression pattern of COX-2 in different culture conditions. Protein expression was quantified by using densitometry analysis of the blots from 4 independent experiments and relative COX-2 expression normalized to that of β-actin is shown in the histogram (Figure 3B). IL-1β significantly induced the expression of COX-2 protein. Of interest and in contrast to mRNA profiles, VA Qu Spez inhibited the IL-1β-induced expression of COX-2 protein in a dose-dependent manner. Furthermore, we followed the expression profiles of IL-1β induced COX-2 in the presence and absence of VA at different time points (12, 18, 24 and 36 hours) following cytokine stimulation. Kinetic analysis of COX-2 at two different concentrations of VA is shown in Figure 3C. IL-1β induced the maximum expression of COX-2 at 18 hours and then onwards, the expression was gradually declined. At 25 µg /ml, VA inhibited the COX-2 protein expression at 18, 24 and 36 hours and at 50 µg/ml, inhibited COX-2 expression at 18 hours and more drastically after 24 hours.
Figure 3. Inhibition of cytokine-induced COX-2 protein expression by Viscum album in A549 cells.
A549 cells were either cultured in medium alone or treated with IL-1β (10 ng/ml) with or without increasing concentration of VA Qu Spez for 18 hours. Using 20 µg of total cellular protein, expression of COX-2 was analyzed by western blotting. A. A representative western-blot depicting the effect of VA on expression of IL-1β-induced COX-2. B. Relative expression (mean ± SEM) of COX-2 protein from four independent experiments as quantified by densitometry (ratio of density of COX-2: that of β-actin). *P<0.05 versus control cells and ** p<0.05 versus IL-1β-stimulated cells as analyzed by paired Student-t-test. C. Kinetics of COX-2 protein expression upon treatment of A549 cells with various doses of VA. The cells were either cultured in medium alone or stimulated with IL-1β with our without VA for 12, 18, 24 and 36 hours. Expression of COX-2 protein was analyzed by western blotting and relative expression of COX-2 protein was quantified by densitometry (ratio of density of COX-2: that of β-actin). Results are representative of two experiments.
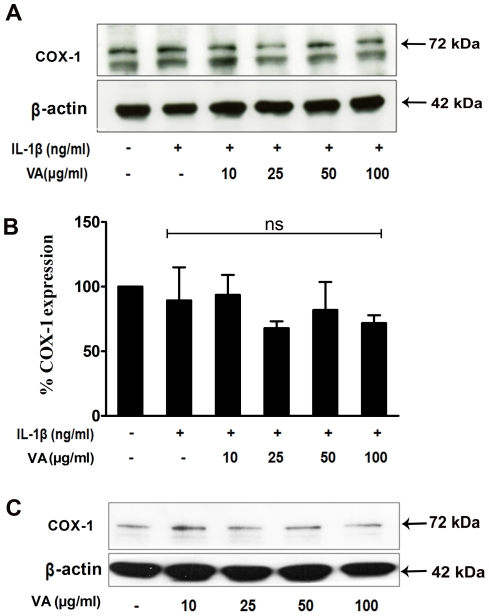
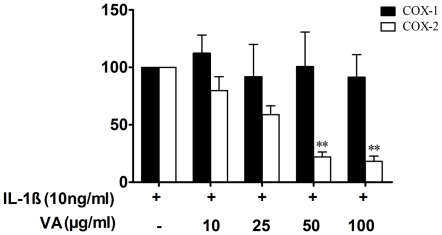
Viscum album does not modulate the expression of COX-1 protein
Since both COX-1 and COX-2 play an important regulatory role in the biosynthesis of PGE2, we then analysed the effect of VA on the expression of COX-1 protein, which is a constitutively expressed isoform of cyclo-oxygenase and is implicated in the functional homeostasis of the cell. We found that A549 cells constitutively express COX-1 and the expression of which was not modified upon treatment of cells with IL-1β (Figure 4A). However, VA Qu Spez did not modulate either the constitutive expression of COX-1 protein nor the expression of COX-1 in IL-1β-stimulated cells (Figure 4A and B). As VA displayed a strong inhibitory effect on IL-1β-induced COX-2 expression without modulating the COX-1 level, our results demonstrate that VA selectively inhibits the expression of COX-2 (Figure 5).
Figure 4. Effect of Viscum album on COX-1 expression in A549 cells.
A and B. A549 cells were treated with increasing concentrations of VA Qu Spez in presence of IL-1β (10 ng/ml) for 18 hours. Protein expression of COX-1 was analyzed by western blot. A representative western-blot depicting the effect of VA on COX-1 expression under IL-1β-stimulated culture conditions (A). Relative expression (mean ± SEM) of COX-1 protein from three independent experiments as quantified by densitometry (ratio of density of COX-1: that of β-actin). ns, non-significant (B). C. Cells were cultured either in medium alone or treated with increasing concentrations of VA Qu Spez without IL-1β for 18 hours. 20 µg of total cellular protein was separated by 10% SDS-PAGE followed by western blotting to analyze the expression of COX-1. Results are representative of two experiments.
Figure 5. Selective inhibition of COX-2 expression by Viscum album.
Quantitative comparison between expression of COX-1 and COX-2 proteins as revealed by western blot. Protein expression was quantified by densitometry and expressed as percentage protein expression normalized to that in cells stimulated with IL-1β. Results (mean ± SEM) obtained from 3 independent experiments are presented. * P<0.05 versus control cells for COX-2 and ** p<0.05 versus IL-1β-stimulated cells for COX-2 as analyzed by paired Student-t-test. The values for COX-1 are non-significant.
Discussion
The therapeutic benefit of VA in diverse pathologies is attributed to the method of preparation, the proportion of various bioactive compounds present within the extracts and also to the host trees. Several lines of evidence have revealed that VA preparations exert an anti-tumoral effect because of their ability to induce apoptosis and to inhibit cell proliferation, providing a strong basis for their application as complementary therapy in cancer. However, successful utilization of these preparations in the treatment of certain inflammatory pathologies raises several questions related to their mechanisms of action. With the aim of understanding the role of VA in modulating the immuno-inflammatory response, we analysed the effect of VA on the PGE2 axis and its regulation at cyclo-oxygenase level.
Cyclo-oxygenases are the regulatory enzymes of PGE2 biosynthetic pathway which catalyse the rate limiting step. They convert the free arachidonic acid in the cell cytosol obtained upon degradation of membrane phospholipids into prostaglandin H2 (PGH2), an active precursor for the synthesis of various prostanoids. Among the isoforms of cyclo-oxygenases, COX-1 is constitutively expressed in the cells whereas COX-2 is induced in response to inflammatory stimuli and contributes majorly to the induction of PGE2 [70]. PGE2 is a molecular mediator of several homeostatic functions including those of gastric mucosa and vascular endothelium [71]. However, it also exerts potent pro-inflammatory effects including the induction fever and pain. Overproduction of PGE2 occurs in response to pro-inflammatory stimuli and correlates with the severity of certain infectious and inflammatory conditions [46]–[49]. PGE2 exerts autocrine and paracrine actions on the target cells and can induce pro-inflammatory reactions. Cyclo-oxygenases have thus constituted attractive targets for designing the anti-inflammatory molecules such as non-steroid anti-inflammatory drugs (NSAID) and for the conception of novel phytotherapeutics [51], [52].
Our results demonstrate that the anti-inflammatory function of VA implicates inhibition of IL-1β-induced PGE2 biosynthesis. In order to understand the mechanisms underlying the VA-mediated inhibition of PGE2 secretion, we analyzed the expression pattern of cytokine-induced COX-2 in the presence of VA. RT-PCR results confirmed that IL-1β induces the expression of COX-2 mRNA while VA does not modulate this cytokine-induced expression of COX-2 mRNA. On the contrary, VA significantly inhibited COX-2 protein expression induced by IL-1β. These results suggest that VA exerts a post-transcriptional regulatory effect on COX-2 expression [72].
The effect of VA was not restricted to IL-1β-induced COX-2 alone. VA also showed an inhibitory effect on IFN-γ and TNF-α-induced COX-2 expression (data not shown). Since, inflammation is a consequence of signaling of various inflammatory cytokines released by innate and adaptive immune cells, endothelial cells and epithelial cells, our results thus indicate that suppression of COX-2 by VA is not restricted to an inflammation created by a particular cytokine rather VA inhibits COX-2 expression mediated by a wide range of cytokines. This inhibitory effect of VA at the protein expression level suggests its probable action in interfering with the process of translation resulting in the quantitative reduction of the protein. Further, kinetic analysis of COX-2 expression induced by IL-1β showed a typical time-dependant increase in protein expression reaching a maximum at 18 hours followed by a decline at later time points. At each time point, treatment of the cells with VA resulted in the reduced expression of COX-2 induced by IL-1β. This reduction in the presence of VA was more pronounced at 24 and 36 hours as compared to cells treated with IL-1β alone indicating a possible effect of VA on protein degradation. Together, modulation of COX-2 by VA strongly favours the role of VA as an anti-inflammatory therapeutic.
From the viewpoint of an anti-inflammatory therapeutic, inhibition of PGE2 synthesis by acting at the level of cyclo-oxygenases exposes a major concern of reducing the homeostatic levels of PGE2 because of the simultaneous inhibition of COX-1 and COX-2. Owing to the structural and functional homology between the COX-1 and COX-2, most of the NSAID which are synthetically designed to inhibit the enzymatic activity of COX-2 also inhibit COX-1, thereby affecting the overall level of PGE2 and are therefore known to cause several severe side effects [73]. Thus, specific inhibitors of COX-2 represent attractive therapeutic alternatives for several inflammatory pathologies [51]. Interestingly, in our study, at all the concentrations of VA which inhibited COX-2, we did not observe any change in the expression of COX-1, irrespective of a robust stimulation by IL-1β. These findings suggest a strong selectivity in anti-inflammatory mechanism of VA by inhibiting COX-2 expression.
Long-term side effects of NSAID in various pathological conditions and the increasing body of evidence for anti-inflammatory activity of plant-derived molecules together encourage the conception of phytotherapeutics as potent alternatives to classical anti-inflammatory drugs [73], [74]. Several clinical studies have revealed the selectivity of certain plant-derived molecules in inhibiting COX-2 that are as efficient as synthetic COX-2-specific antagonists (rofecoxib and celecoxib) in rescuing from both acute and chronic inflammatory conditions and some of these plant-derivatives are superior to synthetic molecules in their anti-inflammatory and analgesic effect [74], [75]. With the growing interest of promising new generation anti-inflammatory therapeutics, exploring and characterizing the novel phytotherapeutics with strong selectivity towards COX-2 are of great value. Together, our results demonstrate that VA exerts an anti-inflammatory effect by interfering with the cytokine-induced PGE2 biosynthesis through a selective inhibition of COX-2 protein suggesting its beneficial role with minimal side effects. These results are relevant in understanding the mechanism of action of VA and may provide an insight for further exploration of anti-inflammatory mechanisms of VA and other plant-derived molecules in diverse pathologies.
Materials and Methods
Viscum album preparations
VA Qu Spez was a kind gift from Weleda AG (Arlesheim, Switzerland). VA Qu Spez is a therapeutic preparation of Viscum album growing on oak trees and is obtained as an isotonic solution of 5 mg/ml and 10 mg/ml formulated in 0.9% NaCl. It is free from endotoxin and contains the standardized levels of mistletoe lectins (0.375 ng/ml) and viscotoxins (0.12 ng/ml).
Culture of A549 cells
Human lung adenocarcinoma cell line A549 was a kind gift from Dr. Maria Castedo-Delrieu, Institute Gustave Roussy, Villejuif, France. A549 cells were grown in 75 cm2 culture flasks in Dulbecco's modified Eagle's medium (DMEM) F-12, GIBCO®, BRL Life Technologies, Grand Island, NY, USA)) supplemented with 10% fetal calf serum and 50 U/ml penicillin and 50 µg/ml of streptomycin (GIBCO®, BRL, Cergy Pontoise, France). Cells are incubated at 37°C with 5% CO2 in humidified atmosphere to obtain the cells of about 80–90% confluence and used for all experiments.
Induction of COX-2 and treatment with VA Qu Spez
Cells grown in complete medium were harvested by tripsinisation using 0.5% trypsin (Biological Industries, Kibbutz Beit Haemek, Israel) and are seeded in six well culture plates (1×106 cells per well), and incubated at 37°C till they reach confluence of 80–90%. Wells containing the adherent A549 are then replenished with the complete medium containing recombinant human IL-1β (10 ng/ml) (Immuno Tools, Friesoythe, Germany) in the presence and absence of VA Qu Spez and incubated for 18 hours at 37°C and 5% CO2. After 18 hours of incubation culture supernatants were collected and used for the estimation of PGE2 and cells are used for estimating the mRNA and protein levels of COX-2/COX-1.
Enzyme immunoassay for PGE2
PGE2 is estimated in the culture supernatants by using competitive enzyme immunoassay (EIA) kit (Cayman Chemicals Co, Ann Arbor, MI, USA) according to the manufacturer's instructions. Cell free supernatants were analysed for the free PGE2 released.
Isolation of total RNA and RT-PCR
Total cellular RNA was isolated using RNA isolation kit (Invitrogen, Life technologies, France) according to the manufacturers' instructions. 0.2 µg of total RNA was reverse transcribed to obtain the cDNA using the Superscript II from (Invitrogen, Life technologies, France) Semi-quantitative PCR is carried out using COX-2 specific primers. Amplification of housekeeping gene GAPDH is used as an internal control. Oligonucleotide primers were purchased from Eurogentech, France. Sequences of oligonucleotides are as given in Table 1.
Table 1. Oligonucleotide primers used in the study.
| Human COX-2 (sense) 5′-TTCAAATGAGATTGTGGGAAAATTGCT-3′ |
| Human COX-2 (antisense) 5′-AGATCATCTCTGCCTGAGTATCTT-3′ |
| Human GAPDH (sense) 5′GAGTCAACGGATTTGGTCGT3′ |
| Human GAPDH (antisense) 5′TTGATTTTGGAGGGATCTCG-3′ |
Immunoblotting of COX-2 and COX-1
Following the appropriate treatment, cells were harvested by a mild tripsinisation and washed with 1× phosphate buffered saline. Cells were lysed using lysis buffer containing 50 mM Tris-HCl (pH 7.4), 0.25% sodium deoxycholate, 150 mM NaCl, 1 mM EDTA, 1% NP-40, 1 mM PMSF and 1× protease inhibitor cock-tail (Sigma-Aldrich, Lyon, France). Cells were suspended in the lysis buffer (100 µl/million cells) and incubated on ice for 30 mins. Supernatants were collected following the centrifugation at 13200 rpm for 20 mins. Total cellular protein is estimated by Bradford method and 20 µg of each sample is loaded on SDS polyacrylamide gel and subjected for electrophoretic migration. Proteins separated on gel were then transferred on to an activated PVDF membrane by semi-dry western transfer (2 hours at 50 mA). Non-specific binding of antibodies is blocked by treating the membrane with 5% non fat milk in tris buffered saline with tween 20 (TBST-20 mM Tris- HCl (pH 7.4), 137 mM NaCl and 0.1% Tween 20) for 2 hours at room temperature. Membranes were incubated with primary antibodies diluted according to the manufactures' instructions in 5% BSA overnight at 4°C. Following the three washes with TBST, Blots were then treated with HRP-conjugated secondary antibodies in 5% BSA (1/4000) for 2 hours at room temperature. Primary antibodies against human COX-2, β-Actin, and the HRP labelled secondary antibodies were procured from Cell Signalling Technology (Ozyme, France). Human anti-COX-1 is obtained from Santa Cruz Biotechnology (CA, USA). Blots were washed well with TBST with minimum three changes for an hour and then revealed using ECL plus western lightening reagent (Perkin Elmer, Waltham, MA, USA) according to manufactures' instructions.
Statistical analysis
Densitometric analysis of the immunoblots was performed using BIO-1D analysis software. Densitometric values were expressed as arbitrary units and subjected for statistical analysis by paired Student-t- test. All the observations are expressed as Mean±SEM. Graphpad Prism 5.0 is used for all the statistical analysis. P values less than 0.05 were considered to be statistically significant.
Footnotes
Competing Interests: Part of the research was supported by Weleda AG, Switzerland.
Funding: This work is Supported by Institut National de la Santé et de la Recherche Médicale (INSERM), Centre National de la Recherche Scientifique (CNRS), Université Pierre et Marie Curie and Université Paris Descartes, regional program Bio-Asie 2011 and Weleda AG, Switzerland. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Olsnes S, Stirpe F, Sandvig K, Pihl A. Isolation and characterization of viscumin, a toxic lectin from Viscum album L. (mistletoe). J Biol Chem. 1982;257:13263–13270. [PubMed] [Google Scholar]
- 2.Khwaja TA, Dias CB, Pentecost S. Recent studies on the anticancer activities of mistletoe (Viscum album) and its alkaloids. Oncology. 1986;43(Suppl 1):42–50. doi: 10.1159/000226419. [DOI] [PubMed] [Google Scholar]
- 3.Franz H, Ziska P, Kindt A. Isolation and properties of three lectins from mistletoe (Viscum album L.). Biochem J. 1981;195:481–484. doi: 10.1042/bj1950481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Urech K, Schaller G, Jaggy C. Viscotoxins, mistletoe lectins and their isoforms in mistletoe (Viscum album L.) extracts Iscador. Arzneimittelforschung. 2006;56:428–434. doi: 10.1055/s-0031-1296808. [DOI] [PubMed] [Google Scholar]
- 5.Kaegi E. Unconventional therapies for cancer: 3. Iscador. Task Force on Alternative Therapies of the Canadian Breast Cancer Research Initiative. CMAJ. 1998;158:1157–1159. [PMC free article] [PubMed] [Google Scholar]
- 6.Bock PR, Friedel WE, Hanisch J, Karasmann M, Schneider B. [Efficacy and safety of long-term complementary treatment with standardized European mistletoe extract (Viscum album L.) in addition to the conventional adjuvant oncologic therapy in patients with primary non-metastasized mammary carcinoma. Results of a multi-center, comparative, epidemiological cohort study in Germany and Switzerland]. Arzneimittelforschung. 2004;54:456–466. doi: 10.1055/s-0031-1296999. [DOI] [PubMed] [Google Scholar]
- 7.Klopp R, Schmidt W, Werner E, Werner M, Niemer W, et al. Influence of complementary Viscum album (Iscador) administration on microcirculation and immune system of ear, nose and throat carcinoma patients treated with radiation and chemotherapy. Anticancer Res. 2005;25:601–610. [PubMed] [Google Scholar]
- 8.Augustin M, Bock PR, Hanisch J, Karasmann M, Schneider B. Safety and efficacy of the long-term adjuvant treatment of primary intermediate- to high-risk malignant melanoma (UICC/AJCC stage II and III) with a standardized fermented European mistletoe (Viscum album L.) extract. Results from a multicenter, comparative, epidemiological cohort study in Germany and Switzerland. Arzneimittelforschung. 2005;55:38–49. doi: 10.1055/s-0031-1296823. [DOI] [PubMed] [Google Scholar]
- 9.Bussing A, Bischof M, Hatzmann W, Bartsch F, Soto-Vera D, et al. Prevention of surgery-induced suppression of granulocyte function by intravenous application of a fermented extract from Viscum album L. in breast cancer patients. Anticancer Res. 2005;25:4753–4757. [PubMed] [Google Scholar]
- 10.Kienle GS, Kiene H. Review article: Influence of Viscum album L (European mistletoe) extracts on quality of life in cancer patients: a systematic review of controlled clinical studies. Integr Cancer Ther. 2010;9:142–157. doi: 10.1177/1534735410369673. [DOI] [PubMed] [Google Scholar]
- 11.Radenkovic M, Ivetic V, Popovic M, Mimica-Dukic N, Veljkovic S. Neurophysiological effects of mistletoe (Viscum album L.) on isolated rat intestines. Phytother Res. 2006;20:374–377. doi: 10.1002/ptr.1865. [DOI] [PubMed] [Google Scholar]
- 12.Tusenius KJ, Spoek AM, van Hattum J. Exploratory study on the effects of treatment with two mistletoe preparations on chronic hepatitis C. Arzneimittelforschung. 2005;55:749–753. doi: 10.1055/s-0031-1296925. [DOI] [PubMed] [Google Scholar]
- 13.Tenorio FA, del Valle L, Gonzalez A, Pastelin G. Vasodilator activity of the aqueous extract of Viscum album. Fitoterapia. 2005;76:204–209. doi: 10.1016/j.fitote.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Karagoz A, Onay E, Arda N, Kuru A. Antiviral potency of mistletoe (Viscum album ssp. album) extracts against human parainfluenza virus type 2 in Vero cells. Phytother Res. 2003;17:560–562. doi: 10.1002/ptr.1163. [DOI] [PubMed] [Google Scholar]
- 15.Tusenius KJ, Spoek JM, Kramers CW. Iscador Qu for chronic hepatitis C: an exploratory study. Complement Ther Med. 2001;9:12–16. doi: 10.1054/ctim.2000.0408. [DOI] [PubMed] [Google Scholar]
- 16.Christen-Clottu O, Klocke P, Burger D, Straub R, Gerber V. Treatment of clinically diagnosed equine sarcoid with a mistletoe extract (Viscum album austriacus). J Vet Intern Med. 2010;24:1483–1489. doi: 10.1111/j.1939-1676.2010.0597.x. [DOI] [PubMed] [Google Scholar]
- 17.Bussing A, Schietzel M. Apoptosis-inducing properties of Viscum album L. extracts from different host trees, correlate with their content of toxic mistletoe lectins. Anticancer Res. 1999;19:23–28. [PubMed] [Google Scholar]
- 18.Stein GM, Pfuller U, Schietzel M, Bussing A. Toxic proteins from European mistletoe (Viscum album L.): increase of intracellular IL-4 but decrease of IFN-gamma in apoptotic cells. Anticancer Res. 2000;20:1673–1678. [PubMed] [Google Scholar]
- 19.Stein GM, Pfuller U, Schietzel M, Bussing A. Intracellular expression of IL-4 and inhibition of IFN-gamma by extracts from European mistletoe is related to induction of apoptosis. Anticancer Res. 2000;20:2987–2994. [PubMed] [Google Scholar]
- 20.Duong Van Huyen JP, Bayry J, Delignat S, Gaston AT, Michel O, et al. Induction of apoptosis of endothelial cells by Viscum album: a role for anti-tumoral properties of mistletoe lectins. Mol Med. 2002;8:600–606. [PMC free article] [PubMed] [Google Scholar]
- 21.Duong Van Huyen JP, Delignat S, Kazatchkine MD, Kaveri SV. Comparative study of the sensitivity of lymphoblastoid and transformed monocytic cell lines to the cytotoxic effects of Viscum album extracts of different origin. Chemotherapy. 2003;49:298–302. doi: 10.1159/000074530. [DOI] [PubMed] [Google Scholar]
- 22.Duong Van Huyen JP, Delignat S, Bayry J, Kazatchkine MD, Bruneval P, et al. Interleukin-12 is associated with the in vivo anti-tumor effect of mistletoe extracts in B16 mouse melanoma. Cancer Lett. 2006;243:32–37. doi: 10.1016/j.canlet.2005.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Heinzerling L, von Baehr V, Liebenthal C, von Baehr R, Volk HD. Immunologic effector mechanisms of a standardized mistletoe extract on the function of human monocytes and lymphocytes in vitro, ex vivo, and in vivo. J Clin Immunol. 2006;26:347–359. doi: 10.1007/s10875-006-9023-5. [DOI] [PubMed] [Google Scholar]
- 24.Stein GM, Bussing A, Schietzel M. Stimulation of the maturation of dendritic cells in vitro by a fermented mistletoe extract. Anticancer Res. 2002;22:4215–4219. [PubMed] [Google Scholar]
- 25.Hostanska K, Hajto T, Spagnoli GC, Fischer J, Lentzen H, et al. A plant lectin derived from Viscum album induces cytokine gene expression and protein production in cultures of human peripheral blood mononuclear cells. Nat Immun. 1995;14:295–304. [PubMed] [Google Scholar]
- 26.Elluru SR, Duong van Huyen JP, Delignat S, Kazatchkine MD, Friboulet A, et al. Induction of maturation and activation of human dendritic cells: a mechanism underlying the beneficial effect of Viscum album as complimentary therapy in cancer. BMC Cancer. 2008;8:161. doi: 10.1186/1471-2407-8-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Duong Van Huyen JP, Sooryanarayana, Delignat S, Bloch MF, Kazatchkine MD, et al. Variable sensitivity of lymphoblastoid cells to apoptosis induced by Viscum album Qu FrF, a therapeutic preparation of mistletoe lectin. Chemotherapy. 2001;47:366–376. doi: 10.1159/000048545. [DOI] [PubMed] [Google Scholar]
- 28.Yoon TJ, Yoo YC, Kang TB, Her E, Kim SH, et al. Cellular and humoral adjuvant activity of lectins isolated from Korean mistletoe (Viscum album colaratum). Int Immunopharmacol. 2001;1:881–889. doi: 10.1016/s1567-5769(01)00024-8. [DOI] [PubMed] [Google Scholar]
- 29.Gardin NE. Immunological response to mistletoe (Viscum album L.) in cancer patients: a four-case series. Phytother Res. 2009;23:407–411. doi: 10.1002/ptr.2643. [DOI] [PubMed] [Google Scholar]
- 30.Frank U, Engels I, Wagner A, Lacour M, Daschner FD. Influence of mistletoe ( Viscum album) extracts on phagocytosis/burst activity of human phagocytes. Eur J Clin Microbiol Infect Dis. 2003;22:501–503. doi: 10.1007/s10096-003-0964-9. [DOI] [PubMed] [Google Scholar]
- 31.Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- 32.Aimanianda V, Haensler J, Lacroix-Desmazes S, Kaveri SV, Bayry J. Novel cellular and molecular mechanisms of induction of immune responses by aluminum adjuvants. Trends Pharmacol Sci. 2009;30:287–295. doi: 10.1016/j.tips.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 33.Medzhitov R. Inflammation 2010: new adventures of an old flame. Cell. 2010;140:771–776. doi: 10.1016/j.cell.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 34.Bayry J. Immunology: TL1A in the inflammatory network in autoimmune diseases. Nat Rev Rheumatol. 2010;6:67–68. doi: 10.1038/nrrheum.2009.263. [DOI] [PubMed] [Google Scholar]
- 35.Libby P. Inflammatory mechanisms: the molecular basis of inflammation and disease. Nutr Rev. 2007;65:S140–146. doi: 10.1111/j.1753-4887.2007.tb00352.x. [DOI] [PubMed] [Google Scholar]
- 36.Maddur MS, Kaveri SV, Bayry J. Basophils as antigen presenting cells. Trends Immunol. 2010;31:45–48. doi: 10.1016/j.it.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 37.Kaveri SV, Mouthon L, Bayry J. Basophils and nephritis in lupus. N Engl J Med. 2010;363:1080–1082. doi: 10.1056/NEJMcibr1006936. [DOI] [PubMed] [Google Scholar]
- 38.Tomlinson KL, Davies GC, Sutton DJ, Palframan RT. Neutralisation of interleukin-13 in mice prevents airway pathology caused by chronic exposure to house dust mite. PLoS One. 2010;5:e13136. doi: 10.1371/journal.pone.0013136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bayry J, Siberil S, Triebel F, Tough DF, Kaveri SV. Rescuing CD4+CD25+ regulatory T-cell functions in rheumatoid arthritis by cytokine-targeted monoclonal antibody therapy. Drug Discov Today. 2007;12:548–552. doi: 10.1016/j.drudis.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 40.Achoui M, Appleton D, Abdulla MA, Awang K, Mohd MA, et al. In vitro and in vivo anti-inflammatory activity of 17-O-acetylacuminolide through the inhibition of cytokines, NF-kappaB translocation and IKKbeta activity. PLoS One. 2010;5:e15105. doi: 10.1371/journal.pone.0015105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andre S, Tough DF, Lacroix-Desmazes S, Kaveri SV, Bayry J. Surveillance of antigen-presenting cells by CD4+ CD25+ regulatory T cells in autoimmunity: immunopathogenesis and therapeutic implications. Am J Pathol. 2009;174:1575–1587. doi: 10.2353/ajpath.2009.080987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Correa-Costa M, Semedo P, Monteiro AP, Silva RC, Pereira RL, et al. Induction of heme oxygenase-1 can halt and even reverse renal tubule-interstitial fibrosis. PLoS One. 2010;5:e14298. doi: 10.1371/journal.pone.0014298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bayry J. Autoimmunity: CTLA-4: a key protein in autoimmunity. Nat Rev Rheumatol. 2009;5:244–245. doi: 10.1038/nrrheum.2009.77. [DOI] [PubMed] [Google Scholar]
- 44.Hegeman MA, Hennus MP, van Meurs M, Cobelens PM, Kavelaars A, et al. Angiopoietin-1 treatment reduces inflammation but does not prevent ventilator-induced lung injury. PLoS One. 2010;5:e15653. doi: 10.1371/journal.pone.0015653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bayry J, Negi VS, Kaveri SV. Intravenous immunoglobulin therapy in rheumatic diseases. Nat Rev Rheumatol. 2011;7:349–359. doi: 10.1038/nrrheum.2011.61. [DOI] [PubMed] [Google Scholar]
- 46.Goldyne ME, Winkelmann RK, Ryan RJ. Prostaglandin activity in human cutaneous inflammation: detection by radioimmunoassay. Prostaglandins. 1973;4:737–749. doi: 10.1016/s0090-6980(73)80058-9. [DOI] [PubMed] [Google Scholar]
- 47.Passwell J, Levanon M, Davidsohn J, Ramot B. Monocyte PGE2 secretion in Hodgkin's disease and its relation to decreased cellular immunity. Clin Exp Immunol. 1983;51:61–68. [PMC free article] [PubMed] [Google Scholar]
- 48.Karmali RA, Welt S, Thaler HT, Lefevre F. Prostaglandins in breast cancer: relationship to disease stage and hormone status. Br J Cancer. 1983;48:689–696. doi: 10.1038/bjc.1983.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Redondo S, Ruiz E, Gordillo-Moscoso A, Navarro-Dorado J, Ramajo M, et al. Overproduction of cyclo-oxygenase-2 (COX-2) is involved in the resistance to apoptosis in vascular smooth muscle cells from diabetic patients: a link between inflammation and apoptosis. Diabetologia. 2011;54:190–199. doi: 10.1007/s00125-010-1947-x. [DOI] [PubMed] [Google Scholar]
- 50.Chun KS, Surh YJ. Signal transduction pathways regulating cyclooxygenase-2 expression: potential molecular targets for chemoprevention. Biochem Pharmacol. 2004;68:1089–1100. doi: 10.1016/j.bcp.2004.05.031. [DOI] [PubMed] [Google Scholar]
- 51.Chell S, Kaidi A, Williams AC, Paraskeva C. Mediators of PGE2 synthesis and signalling downstream of COX-2 represent potential targets for the prevention/treatment of colorectal cancer. Biochim Biophys Acta. 2006;1766:104–119. doi: 10.1016/j.bbcan.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 52.Cerella C, Sobolewski C, Dicato M, Diederich M. Targeting COX-2 expression by natural compounds: a promising alternative strategy to synthetic COX-2 inhibitors for cancer chemoprevention and therapy. Biochem Pharmacol. 2010;80:1801–1815. doi: 10.1016/j.bcp.2010.06.050. [DOI] [PubMed] [Google Scholar]
- 53.Vane JR, Botting RM. Mechanism of action of anti-inflammatory drugs. Scand J Rheumatol. 1996;(Suppl 102):9–21. doi: 10.3109/03009749609097226. [DOI] [PubMed] [Google Scholar]
- 54.Zhou HY, Shin EM, Guo LY, Youn UJ, Bae K, et al. Anti-inflammatory activity of 4-methoxyhonokiol is a function of the inhibition of iNOS and COX-2 expression in RAW 264.7 macrophages via NF-kappaB, JNK and p38 MAPK inactivation. Eur J Pharmacol. 2008;586:340–349. doi: 10.1016/j.ejphar.2008.02.044. [DOI] [PubMed] [Google Scholar]
- 55.Hamsa TP, Kuttan G. Evaluation of the anti-inflammatory and anti-tumor effect of ipomoea obscura (L) and its mode of action through the inhibition of pro inflammatory cytokines, nitric oxide and COX-2. Inflammation. 2011;34:171–183. doi: 10.1007/s10753-010-9221-4. [DOI] [PubMed] [Google Scholar]
- 56.Carey MA, Bradbury JA, Rebolloso YD, Graves JP, Zeldin DC, et al. Pharmacologic inhibition of COX-1 and COX-2 in influenza A viral infection in mice. PLoS One. 2010;5:e11610. doi: 10.1371/journal.pone.0011610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sharma C, Kaur J, Shishodia S, Aggarwal BB, Ralhan R. Curcumin down regulates smokeless tobacco-induced NF-kappaB activation and COX-2 expression in human oral premalignant and cancer cells. Toxicology. 2006;228:1–15. doi: 10.1016/j.tox.2006.07.027. [DOI] [PubMed] [Google Scholar]
- 58.Kunnumakkara AB, Diagaradjane P, Anand P, Harikumar KB, Deorukhkar A, et al. Curcumin sensitizes human colorectal cancer to capecitabine by modulation of cyclin D1, COX-2, MMP-9, VEGF and CXCR4 expression in an orthotopic mouse model. Int J Cancer. 2009;125:2187–2197. doi: 10.1002/ijc.24593. [DOI] [PubMed] [Google Scholar]
- 59.Kale A, Gawande S, Kotwal S. Cancer phytotherapeutics: role for flavonoids at the cellular level. Phytother Res. 2008;22:567–577. doi: 10.1002/ptr.2283. [DOI] [PubMed] [Google Scholar]
- 60.Habib SH, Makpol S, Abdul Hamid NA, Das S, Ngah WZ, et al. Ginger extract (Zingiber officinale) has anti-cancer and anti-inflammatory effects on ethionine-induced hepatoma rats. Clinics (Sao Paulo) 2008;63:807–813. doi: 10.1590/S1807-59322008000600017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Rosenkranz HS, Thampatty BP. SAR: flavonoids and COX-2 inhibition. Oncol Res. 2003;13:529–535. doi: 10.3727/000000003108748054. [DOI] [PubMed] [Google Scholar]
- 62.Torres Salazar A, Hoheisel J, Youns M, Wink M. Anti-inflammatory and anti-cancer activities of essential oils and their biological constituents. Int J Clin Pharmacol Ther. 2011;49:93–95. [PubMed] [Google Scholar]
- 63.Jin M, Suh SJ, Yang JH, Lu Y, Kim SJ, et al. Anti-inflammatory activity of bark of Dioscorea batatas DECNE through the inhibition of iNOS and COX-2 expressions in RAW264.7 cells via NF-kappaB and ERK1/2 inactivation. Food Chem Toxicol. 2010;48:3073–3079. doi: 10.1016/j.fct.2010.07.048. [DOI] [PubMed] [Google Scholar]
- 64.Hwang YP, Choi JH, Yun HJ, Han EH, Kim HG, et al. Anthocyanins from purple sweet potato attenuate dimethylnitrosamine-induced liver injury in rats by inducing Nrf2-mediated antioxidant enzymes and reducing COX-2 and iNOS expression. Food Chem Toxicol. 2011;49:93–99. doi: 10.1016/j.fct.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 65.Hong J, Sang S, Park HJ, Kwon SJ, Suh N, et al. Modulation of arachidonic acid metabolism and nitric oxide synthesis by garcinol and its derivatives. Carcinogenesis. 2006;27:278–286. doi: 10.1093/carcin/bgi208. [DOI] [PubMed] [Google Scholar]
- 66.Min KJ, Choi K, Kwon TK. Withaferin A down-regulates lipopolysaccharide-induced cyclooxygenase-2 expression and PGE2 production through the inhibition of STAT1/3 activation in microglial cells. Int Immunopharmacol. 2011;11:1137–1142. doi: 10.1016/j.intimp.2011.02.029. [DOI] [PubMed] [Google Scholar]
- 67.Bereswill S, Munoz M, Fischer A, Plickert R, Haag LM, et al. Anti-inflammatory effects of resveratrol, curcumin and simvastatin in acute small intestinal inflammation. PLoS One. 2010;5:e15099. doi: 10.1371/journal.pone.0015099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Orhan DD, Kupeli E, Yesilada E, Ergun F. Anti-inflammatory and antinociceptive activity of flavonoids isolated from Viscum album ssp. album. Z Naturforsch C. 2006;61:26–30. doi: 10.1515/znc-2006-1-205. [DOI] [PubMed] [Google Scholar]
- 69.Lavastre V, Cavalli H, Ratthe C, Girard D. Anti-inflammatory effect of Viscum album agglutinin-I (VAA-I): induction of apoptosis in activated neutrophils and inhibition of lipopolysaccharide-induced neutrophilic inflammation in vivo. Clin Exp Immunol. 2004;137:272–278. doi: 10.1111/j.1365-2249.2004.02545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pairet M, Engelhardt G. Distinct isoforms (COX-1 and COX-2) of cyclooxygenase: possible physiological and therapeutic implications. Fundam Clin Pharmacol. 1996;10:1–17. doi: 10.1111/j.1472-8206.1996.tb00144.x. [DOI] [PubMed] [Google Scholar]
- 71.Pozzi A, Zent R. Regulation of endothelial cell functions by basement membrane- and arachidonic acid-derived products. Wiley Interdiscip Rev Syst Biol Med. 2009;1:254–272. doi: 10.1002/wsbm.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tetsuka T, Baier LD, Morrison AR. Antioxidants inhibit interleukin-1-induced cyclooxygenase and nitric-oxide synthase expression in rat mesangial cells. Evidence for post-transcriptional regulation. J Biol Chem. 1996;271:11689–11693. doi: 10.1074/jbc.271.20.11689. [DOI] [PubMed] [Google Scholar]
- 73.Meyer-Kirchrath J, Schror K. Cyclooxygenase-2 inhibition and side-effects of non-steroidal anti-inflammatory drugs in the gastrointestinal tract. Curr Med Chem. 2000;7:1121–1129. doi: 10.2174/0929867003374219. [DOI] [PubMed] [Google Scholar]
- 74.Chrubasik S, Kunzel O, Model A, Conradt C, Black A. Treatment of low back pain with a herbal or synthetic anti-rheumatic: a randomized controlled study. Willow bark extract for low back pain. Rheumatology (Oxford) 2001;40:1388–1393. doi: 10.1093/rheumatology/40.12.1388. [DOI] [PubMed] [Google Scholar]
- 75.Cravotto G, Boffa L, Genzini L, Garella D. Phytotherapeutics: an evaluation of the potential of 1000 plants. J Clin Pharm Ther. 2010;35:11–48. doi: 10.1111/j.1365-2710.2009.01096.x. [DOI] [PubMed] [Google Scholar]