Abstract
Objective
The incidence and incidence over time of cardiac arrest in hospitalized patients (IHCA) is unknown. We sought to estimate the event rate and temporal trends of adult inhospital cardiac arrest (IHCA) treated with a resuscitation response.
Design
Three approaches were used to estimate the IHCA event rate. First approach: Calculate the IHCA event rate at hospitals (n=433) in the Get With The Guidelines-Resuscitation (GWTG-R) registry, years 2003–2007 and multiply this by US annual bed-days. Second approach: Use the GWTG-R, IHCA event rate to develop a regression model (including hospital demographic, geographic, organizational factors) and use the model coefficients to calculate predicted event rates for acute care hospitals (n=5,445) responding to the American Hospital Association survey. Third approach: Classify acute care hospitals into groups based on academic, urban, bed size-and determine the average event rate for GWTG-R hospitals in each group and then use weighted averages to calculate the national IHCA rate. Annual event rates were calculated to estimate temporal trends.
Setting
GWTG-R registry
Patients
Adult IHCA with a resuscitation response
Measurements and main results
The mean adult treated IHCA event rate at GWTG-R hospitals was 0.92/1000 bed-days (IQR 0.58 to 1.2/1000). In hospitals (n=150) contributing data for all years of the study period, the event rate increased from 2003–2007. With 2.09 million annual US bed-days, we estimated 192,000 IHCA throughout the US annually. Based on the regression model, extrapolating GWTG-R hospitals to hospitals participating in the American Hospital Association survey projected 211,000 annual IHCA. Using weighted averages projected 209,000 annual US IHCA.
Conclusions
There are approximately 200,000 treated cardiac arrests among US hospitalized patients annually and this rate may be increasing. This is important for understanding the burden of IHCA and developing strategies to improve care for hospitalized patients.
Keywords: cardiopulmonary resuscitation, heart arrest, resuscitation
Introduction
In-hospital cardiac arrest (IHCA) is associated with significant morbidity and mortality, yet the incidence of in-hospital arrest treated with a resuscitation response in the US is unknown (1, 2). Estimates of IHCA incidence have typically been reported from single institutions or small groups of hospitals in similar geographic locations (3–5). These estimates are limited in terms of generalizability because of non-uniform definitions of IHCA and marked variability in patient and hospital inclusion criteria (5–7). Furthermore, comprehensive, standardized data about all IHCA events are not available in any national registries or other hospital databases. As a result, it has been difficult to determine the overall rate of treated IHCA at hospitals and if this rate is changing over time. Improved understanding of the scope of this problem is especially important, because wide variability in IHCA survival rates among hospitals suggest an opportunity for improved outcomes (8–10).
Our primary aim was to estimate the event rate of IHCAs that generate a resuscitation response in US hospitals. To determine this estimate, we used data from the American Heart Association’s (AHA) Get With the Guidelines-Resuscitation (GTWG-R), [formerly known as National Registry of Cardiopulmonary Resuscitation, NRCPR] a large multi-center database of IHCA with standardized data derived from the Utstein-style (11) cardiac arrest data reporting guidelines and the American Hospital Association annual survey, which provides detailed demographic information for US hospitals. To determine if incidence was changing over time, we also evaluated temporal patterns of event rate in GWTG-R hospitals.
Materials and Methods
As no single database has detailed information about all IHCAs, three approaches were used to estimate the annual US event rate of treated IHCAs. These are detailed below.
Approach 1: Event rate estimation using GWTG-R and US annual hospital bed-days
The first approach involved determining the event rate of hospitals reporting data to the GWTG-R between January 1, 2003 and December 31, 2007 and then multiplying this by the US annual bed-days during that time period. GWTG-R was used because it represents the only prospective database which includes detailed patient level information about treated in-hospital arrests in the US (12). The AHA’s GWTG-R was constructed primarily for the purpose of quality improvement. Quality control and oversight for all data collection, analysis, reporting and GWTG-R research is provided by AHA.
Data are reported voluntarily from a non-random group of multiple acute care hospitals regarding in-hospital resuscitations-using Utstein definitions for in-hospital arrest (11). Utstein definitions derive from the International Liaison Committeeon Resuscitation (ILCOR) published series of guidelines foruniform reporting of adult in-hospital resuscitation research.(11) The database includes resuscitation events if the event generates an emergency resuscitation response by medical personnel and a resuscitation record. Research coordinators at each facility regularly abstract data from medical records and resuscitation review sheets regarding: patient demographics, pre-event data, event data, and patient outcomes. Additionally, code cart utilization and paging system records are consistently reviewed to ensure accurate identification of all arrests. All data is transmitted to a central database repository without any unique patient or hospital identifiers.
The treated IHCA event rate was estimated as the number of arrests (numerator) divided by bed-days (denominator). Included in the estimation of the numerator were: cardiac arrests in adult patients (age 18 and above) admitted between January 1, 2003 and December 31, 2007 to adult acute care hospitals generating a resuscitation response and reported to the GWTG-R. Pediatric hospitals were excluded. Arrests in hospital employees or visitors were excluded. Subsequent arrests in an individual patient were included in our analysis if designated as discrete IHCA events in the GWTG-R database. The denominator measurement, hospital bed-days was selected to represent the in-hospital population at risk for arrest, similar to person-time (13). Annual hospital bed-days were determined from the American Hospital Association survey and then linked with the GWTG-R corresponding year of data.
The American Hospital Association survey has over 1,000 inputs and collects data regarding hospital organization structure, service lines, personnel, finances, physician organization structures, beds and utilization. Data is collected on a fiscal year basis from over 6500 hospitals throughout the US and associated areas.
Approach two: Event rate estimation using a regression model based on hospitals factors and GWTG-R IHCA rates to predict event rates at US acute care hospitals
The second approach involved using the event rates calculated in hospitals reporting data to GWTG-R to predict the event rates for all US hospitals reporting data to the American Hospital Association annual survey based on these hospitals’ volume, demographic, geographic, and organizational characteristics. The source and specifics of the variables used to characterize hospitals are defined below.
Hospital volume
Measures of hospital volume were obtained from the American Hospital Association annual survey and included: number of beds, nurse to bed ratio, and percentage of intensive care unit (ICU) beds.
Demographics
Hospital-level estimates of inpatient racial composition (percentage of Medicare claims for black patients) were determined because delayed defibrillation has been reported for black patients with IHCA and because of the relevance of this factor in other IHCA investigations (14, 15). Estimates of patient income (mean zip-code linked median household income) were also evaluated based on calculations from a prior study (14).
Geography
The geographic region (North, South, East, and West) of each facility was determined from census records. Regions characterized as urban were determined from the Medicare Hospital Cost Report Information System.
Organizational
Organizational hospital characteristics included trauma designation (level 1, 2 or other) and academic designation (member of the Council of Teaching Hospitals and Health Systems). These variables were ascertained from the American Hospital association annual survey. The capability of a hospital to perform cardiac surgery procedures was also included and ascertained from Medicare claims based on billing codes for International Classification of Diseases, Ninth Revision, ClinicalModification [ICD-9-CM] code 361x or Diagnosis Related Group (DRG) codes (106, 107, 109, 547, 548, 549, 550).
Third approach: Event rate estimation using weighted averages for select covariates
For the third approach, US hospitals were grouped according to academic designation (yes versus no), urban (yes versus no), and bed size (in deciles among US hospitals). The average event rate for GWTG-R hospitals was then determined in each group (academic, urban, bed size). Within each group, hospitals not represented in GWTG-R were assigned the weighted average GWTG-R event rate for that group.
Statistical Analyses
Summary statistics were used to compare GWTG-R hospitals with all acute care US hospitals (n=5,445) reporting data to the American Hospital Association. Statistical significance across groups was determined using the chi-squared test.
First approach
The number of arrest events at each hospital was divided by each hospital’s annual bed-days to determine the event rate of IHCA at GWTG-R hospitals. The numerator was determined from events recorded in GWTG-R and the denominator from the annual reported bed-days per facility. The annual GWTG-R event rate was multiplied by the annual total bed-days at all hospitals (2003–2007) to generate an estimate of the national IHCA event rate. The average rate across years is reported.
Second approach
A multivariable model characterized the incidence of cardiac arrest in GWTG-R data as a function of the following covariates: volume measures (number of beds, nurse-to-bed ratio, and percentage ICU beds), demographic measures (hospital racial composition and income), geographic measures (north, south, east, west, and urban), and hospital organizational measures (trauma, academic status, cardiac surgery capability). A negative binomial regression model of GWTG-R hospitals (with year as a dummy variable) was estimated after determining that event rates were excessively dispersed to satisfy the Poisson model assumptions (16). Generalized estimating equations controlled for multiple observations of the same hospital across years (17). Coefficient estimates from this regression model predicted event rate count for all hospitals who responded to the American Hospital Association survey. The correlation matrix used to model the correlation was autoregressive. The model is provided in Appendix A. Multiple imputation (number=5) estimated the valued of missing covariates (18, 19). Multiple iterations of the imputation procedure were used to ensure that our national event rate estimate was robust to the imputed values.
Third approach
All US hospitals were classified into a matrix: 2(academic) × 2(urban) × 3 (bed size in terciles) for a total of 12 groups. The weighted average event rate for GWTG-R hospitals in each group was determined. Each hospital in each group not represented in GWTG-R was assigned the GWTG-R average event rate for that group. The result was summarized as the average annual IHCA event rate across groups.
Temporal patterns of the IHCA event rate at GWTG-R hospitals
To evaluate the event rate over time, we estimated the event rate in hospitals (n=150) contributing data to GWTG for all years of the study period (2003–2007). We evaluated this subset of hospitals because other hospitals joined the registry at varied times during the study period. The annual event rate for each year of the study period is reported as events per 1000 bed-days and compared across years using the test for trends.
All statistical analysis for this study were performed using SAS version 9.1 (SAS Institute Inc, Cary, North Carolina) and Stata version 11, College Station, Texas. A p-value <.05 was considered statistically significant. The Institutional Review Board at the University of Pennsylvania approved this study.
Results
Hospitals reporting data to GWTG-R (n=433) were compared with all US acute care hospitals (n=5445) with regard to several hospital characteristics (markers of hospital volume, demography, geography, and organizational characteristics). Hospitals participating in GWTG-R were most similar to US acute care hospitals reporting data to the American Hospital Association annual survey with regard to geographic distribution (Table 1).
Table 1.
Characteristics of Get With the Guidelines-Resuscitation hospitals compared with US hospitals
| GWTG-R n=433 | Missing data | US hospitals n=5445 | Missing data | Source | |
|---|---|---|---|---|---|
| GEOGRAPHY | Census | ||||
| West | 81 (19%) | 1045 (19%) | |||
| South | 198 (46%) | 2152 (40%) | |||
| Northeast | 61 (14%) | 727 (13%) | |||
| Midwest | 93 (21%) | 1521 (28%) | |||
| DEMOGRAPHY | |||||
| Volume black patients | 29 | 492 | Medicare | ||
| Low (<5%) | 323 (55%) | 3256 (66%) | |||
| Medium (5–12%) | 80 (20%) | 706 (14%) | |||
| High (>12%) | 101 (25%) | 991 (20%) | |||
| Median per capita income | 29 | 492 | Census | ||
| Low (<$16000) | 33 (8%) | 1182 (24%) | |||
| Medium ($16–21000) | 200 (50%) | 2483 (50%) | |||
| High (>$21000) | 171 (42%) | 1288 (26%) | |||
| Urban | 178 (41%) | 1627 (30%) | HCRIS | ||
| ORGANIZATIONAL | |||||
| Academic | 81 (19%) | 363 (7%) | AHAS | ||
| Trauma services (level1,2) | 10 | 316 | AHAS | ||
| 182 (43%) | 1562 (30%) | ||||
| Cardiac surgery capability | 7 | 232 | |||
| 253 (60%) | 1162 (22%) | Medicare | |||
| VOLUME | AHAS | ||||
| Bed size | |||||
| Small (6–99) | 42 (10%) | 2693 (49%) | |||
| Medium (100–400) | 276 (64%) | 2269 (42%) | |||
| Large (>400) | 115 (27%) | 483 (9%) | |||
| Nurse to bed ratio | AHAS | ||||
| Low | 17 (4%) | 1410 (26%) | |||
| Medium | 161 (37%) | 2171 (40%) | |||
| High | 255 (59%) | 1864 (34%) | |||
| Percent ICU beds | 10 | 316 | AHAS | ||
| Low (<5%) | 61 (14%) | 2132 (42%) | |||
| Medium (5–10%) | 235 (56%) | 1927 (38%) | |||
| High (>10%) | 127 (30%) | 1070 (21%) | |||
GWTG-R, Get With The Guidelines-Resuscitation; US, United States; AHAS, American Hospital Association Survey; ICU, Intensive Care Unit; HCRIS, Healthcare Cost Report Information System
The treated IHCA event rate at GWTG-R hospitals (n=433) was estimated as 0.92/1000 (IQR 0.58 to 1.2/1000) bed-days. Annual US bed-days by year were 2003 (209.5 million), 2004 (210.4 million), 2005 (210.3 million), 2006 (209.6 million), 2007 (206.6 million), yielding an average of 209.3 million bed-days for the study period (2003–2007). Multiplying the annual GWTG-R event rate by the average US bed-days estimates 192,000 treated IHCA events in the US annually.
Using our regression model based on annual GWTG-R event rates and demographic, geographic and organizational hospital factor covariates predicted 211,000 IHCA annually.
Using our model of weighted averages based on bed-days, academic, and urban status projected 209,000 annual US treated IHCA.
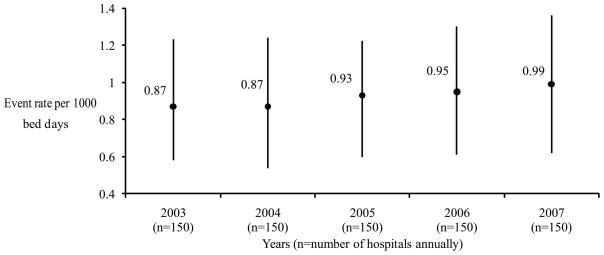
In evaluating a subset of hospitals (n=150) contributing data to GWTG-R every year of the study period 2003–2007, the event rate was noted to increase over time (Table 2 and Figure 1). The mean rate across all 5 years in this subset was 0.92/1000 (IQR 0.61 to 1.18) bed days.
Table 2.
Get With the Guidelines-Resuscitation annual in-hospital cardiac arrest events and bed days (for hospitals [n=150] contributing data for all 5 years, 2003–2007))
| Cardiac arrest events | Bed days | Mean event rate (per 1000 bed days) | P value | |
|---|---|---|---|---|
| Year: | p=0.01 | |||
| 2003 | 10503 | 12,061,231 | 0.87 | |
| 2004 | 11366 | 13,076,891 | 0.87 | |
| 2005 | 12125 | 13,097,347 | 0.93 | |
| 2006 | 12478 | 13,175,055 | 0.95 | |
| 2007 | 11840 | 11,899,325 | 0.99 |
Figure 1. Event rate of in-hospital cardiac arrest in hospitals contributing data to the Get With the Guidelines-Resuscitation Registry for consecutive years 2003–2007.
This figure depicts the annual event rate of in-hospital cardiac arrest for hospitals participating in the Get With the Guidelines-Resuscitation registry. The circular points represent the event rates and the corresponding bars represent the interquartile range.
Discussion
Based on GWTG-R and American Hospital Association data, we estimated that approximately 200,000 hospitalized patients are treated for cardiac arrest in the US annually. These estimates suggest that a similar number of Americans receive attempted resuscitation each year from cardiac arrest in-hospital (~200,000/year) and out-of-hospital (~175,000/year) (2, 20). This is consistent with prior reports estimating the annual incidence of sudden arrhythmic death between 184,000 and 462,000 (1, 21). Because 21% of adults survive (and often with good neurologic outcome) to hospital discharge following resuscitation for IHCA compared with <8% following resuscitation for out-of-hospital (OHCA), the absolute number of Americans who survive cardiac arrests each year is much higher following IHCA than OHCA (2). Collectively, our findings support that nearly 400,000 treated cardiac arrests occur in and outside of the hospital. Estimating this national average is important for understanding the burden of cardiac arrest and further underscores the need for sustained serious efforts to address this disease.
There is a paucity of data regarding the incidence of IHCAs in hospitalized patients. A few reports have estimated treated IHCA event rates (3–5, 22, 23) and these studies varied substantially in terms of inclusion criteria and study populations. Some studies report the event rate for adult patients in a specific age range (e.g. elderly) or hospital location (e.g. non-ICU setting) (4, 23) Other reports vary in terms of cumulative event rate at a group of hospitals compared with event rate at individual facilities (3, 4, 12, 23). The definitions for treated IHCA and event rate also varied widely (5, 6). Such heterogeneity makes comparisons across studies challenging. Further work is needed to better understand the wide variation in the reported incidence and outcomes of both IHCA and OHCA.(1, 21)
In this GWTG-R study, the standardized Utstein-style cardiac arrest data reporting guidelines were used, including consistent definitions and uniform data collection. Our estimates of event rate reflect US registry data from adult patients, in ICU and non-ICU settings, and estimates of event rate that account for individual hospital bed-days (metric commonly used in hospital epidemiology (13)).
It is important to contextualize our estimate of ~200,000 annual treated IHCA in the US and consider what the parameters should be for the national treated arrest rate. It is unrealistic for the national IHCA rate to be zero, as some arrests are not preventable. Inevitably, as hospitals provide care for critically ill patients, some of the ~200,000 IHCA are expected and consistent with the end of the cycle of life. From a policy standpoint, it is important to understand the IHCA event rate in terms of arrests that are not inevitable but that are preventable.
These potentially avoidable arrests may represent a significant proportion of total estimated IHCA as prior work suggests that approximately 100,000 preventable in-hospital deaths occur annually in the US (24). An expert panel, medical chart review (of cases from a district general hospital with house staff) demonstrated that 62% of IHCA were potentially preventable (3). These cases were primarily due to diagnostic errors, delays in responding to abnormal hemodynamic parameters, delays in activating medical personnel, and lack of adherence to resuscitation guidelines/policies. Similarly, other reports using retrospective chart review have illustrated clinical deterioration at least eight hours prior to arrest in up to 84% of hospitalized patients (25–27). Variability in do-not-resuscitate (DNR) policies also likely represents differences in preventable IHCA rates as a hospitals’ approach to end of life care may impact which terminally ill patients receive aggressive resuscitation measures compared with comfort care (3, 28). Overall, to better understand the magnitude of the US IHCA event rate, future work is needed to determine the etiology of arrests (e.g. medical error, differences in DNR policies) that impact the proportion of preventable arrests that can be reduced to improve morbidity and mortality in hospitalized patients. This may also provide insight into some of the variability in IHCA arrest outcomes attributed to arrest time of day/day of the week, (29) time to defibrillation, (10) or potentially modifiable process measures.
To evaluate the IHCA event rate over time, we restricted our analysis to the subset of hospitals (n=150) that contributed data every year of the study period, 2003–2007—this excluded hospitals joining GWTG-R after 2003 or those who joined and then discontinued data entry after 2003. The mean event rate (0.92/1000) for this subset was the same as the larger cohort (n=433) and the event rate in this subset was noted to increase annually.
The increase in IHCA event rates is likely multi-factorial and may reflect differences in reporting and classification or an actual increase in arrest events. Although GWTG-R has strict and structured data collection guidelines, there may be differences in data reporting in this subset of hospitals. These hospitals could also be increasingly providing care for sicker patients, changing their strategies for treating critically ill patients, or changing their policies for end of life care (e.g. DNR status, neurologic prognostication, withdrawal of care).
Our finding may also reflect that there have been few recommendations for how to optimally reduce IHCA rates over the past decade. Most of the recent AHA Emergency Cardiovascular Care Cardiopulmonary Resuscitation guidelines (2010)-and those issued during the study time period (2005) focus on treatment strategies for cardiac arrest rather than best practices for prevention of in-hospital cardiac arrest (30–32). In addition, two approaches, implementing rapid response teams and improving early identification of patients with do not resuscitate status, have not been shown reduce IHCA rates (8, 33, 34). Future studies are certainly needed to better understand the factors contributing to IHCA event rates over time.
Limitations
There are several limitations to our study. Our event rate estimates rely on the completeness of data entered into the GWTG-R registry, and only includes cardiac arrests where resuscitation was attempted. Although participating hospitals are strongly encouraged to enter all event rates consecutively and the AHA provides rigorous quality control and oversight for all GWTG-R data collection and reporting, we cannot confirm that all IHCA resuscitation events were identified at each institution during the study time period using consistent Utstein IHCA definitions. Certainly, some cardiac arrests that occur in operating suites, ICUs and other parts of the hospital may be treated without a hospital-wide resuscitation response and therefore not be included in the GWTG-R database. These limitations suggest that the actual rate of treated IHCAs in the US may be even higher than 200,000/year.
Using our first method, we are limited in our extrapolation of the IHCA event rate in GWTG-R hospitals to US hospitals, and we acknowledge that GWTG-R represents a cohort of non-randomly selected hospitals which differ somewhat from the general population of US hospitals. Some of these differences are due to the large number of US hospitals (relative to GWTG-R hospitals) but reflect less clinically important differences. It is unlikely, that any existing database would capture incidence at small hospitals—and these hospitals are often underrepresented in registries (35, 36). Importantly, however, GWTG-R includes ~24% of large US hospitals and ~12% of medium US hospitals (both of which represent significantly more bed-days then small hospitals).
Additionally, to date, event rates cannot be extrapolated from existing administrative datasets or other national databases. Importantly, the estimate from this simplistic methodology was similar to the estimates from the other two methods.
Our second method is limited in that there may be additional key hospital factors or patient case-mix factors that were not include in our regression model which may provide more optimal estimation of arrest rates. In addition, our use of imputation based on the smaller subset of GWTG-R hospitals to the larger group of all US hospitals (where some of the covariate data was missing) may bias the estimation of confidence intervals.
For our third method, weighted averages were based on three commonly reported, typically relevant hospital factors. Once again, these estimates may be limited however as there may be other factors that may provide more accurate predictions for non-GWTG-R hospitals. Nevertheless, estimates from all three methodologies were remarkably similar.
Regarding the increasing IHCA event rate, individual facilities may have implemented strategies to improve their event rate but this may not be reflected in the cumulative results.
Conclusion
Approximately 200,000 treated IHCA occur annually in the US. A better understanding of the overall burden of treated IHCA in the US is a first step in addressing this major healthcare and healthcare system problem.
Supplementary Material
Acknowledgments
We wish to thank Amy Praestgaard for her assistance with data analysis.
Financial support:
This research was supported by funding from the Robert Wood Johnson Foundation Clinical Scholars program at the University of Pennsylvania (Merchant). This research was also supported by an unrestricted grant from the Institute for Health Technology Studies (Washington, DC), as well as grant 1-R01-HL086919 from the National Heart, Lung, and Blood Institute. This project was also funded, in part, under a grant from the Pennsylvania Department of Health, which specifically disclaims responsibility for any analyses, interpretations, or conclusions. Dr. Groeneveld was additionally supported by a Research Career Development Award from the Department of Veterans Affairs’ Health Services Research and Development Service. None of the above funding sources were involved in the design or conduct of the study, collection, management, analysis, or interpretation of the data, or preparation, review, or approval of the manuscript.
Footnotes
Financial Disclosures
Becker: Speaker honoraria/consultant fees: Philips Healthcare, Seattle, WA. Institutional grant/research support: Philips Healthcare, Seattle, WA, Laerdal Medical, Stavanger, Norway, NIH, Bethesda, MD, Cardiac Science, Bothell, Washington
Berg: Institutional grant/research support: NIH, Bethesda, MD
Nadkarni: Institutional grant/research support: Laerdal Foundation for Acute Care Medicine, Stavanger, Norway, NIH, Bethesda, MD
Nichol: Nichol: Institutional grant/research support: Co-PI, Resuscitation Outcomes Consortium (NIH U01 HL077863-05) 2004–2015, Co-PI, Evaluation of Video Self-Instruction in Compressions-Only CPR (Asmund S. Laerdal Foundation for Acute Medicine) 2007–2010, PI, Randomized Trial of Hemofiltration After Resuscitation from Cardiac Arrest (NHLBI R21 HL093641-01A1) 2009–2011, Co-I, Randomized Field Trial of Cold Saline IV After Resuscitation from Cardiac Arrest (NHLBI R01 HL089554-03) 2007–2012, Co-I, Resynchronization/Defibrillation for Advanced Heart Failure Trial (RAFT) (200211UCT-110607) 2003–2010, Co-I, Novel Methods of Measuring Health Disparities (1RC2HL101759-01) 2009–2011, PI, Cascade HeartRescue Program (Medtronic Foundation) 2010–2015, Research Collaborator: Gambro Renal Inc., Lakewood, CO, Sotera Wireless, San Diego, CA, Lifebridge Medizintechnik AG, Ampfing, Germany, Other: Chair, AHA Executive Database Steering Committee, Chair, Mission:Lifeline EMS Task Force, Co-Chair, AHA Resuscitation Science Symposium Planning Committee, Member, AHA Advanced Cardiac Life Support Subcommittee, Member, AHA Epidemiology and Statistics Committee, Member, Pacific Mountain Affiliate Board of Directors, American Heart Association, Received travel reimbursement, AHA
Carr: Institutional grant/research support: NIH, AHRQ
Abella: Speaker honoraria/consultant fees: Philips Healthcare, Seattle, WA, Medivance Corporation, Louisville, CO. Institutional grant/research support: Philips Healthcare, Andover, MA, Doris Duke Foundation, New York City, NY, American Heart Association, Dallas, TX, NIH, Bethesda, MD. In-kind research support: Laerdal Medical Corp, Stavanger, Norway.
Groeneveld: Federal employee
References
- 1.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart Disease and Stroke Statistics--2011 Update: A Report From the American Heart Association. Circulation. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hodgetts TJ, Kenward G, Vlackonikolis I, et al. Incidence, location and reasons for avoidable in-hospital cardiac arrest in a district general hospital. Resuscitation. 2002;54(2):115–123. doi: 10.1016/s0300-9572(02)00098-9. [DOI] [PubMed] [Google Scholar]
- 4.Skogvoll E, Isern E, Sangolt GK, et al. In-hospital cardiopulmonary resuscitation. 5 years’ incidence and survival according to the Utstein template. Acta Anaesthesiol Scand. 1999;43(2):177–184. doi: 10.1034/j.1399-6576.1999.430210.x. [DOI] [PubMed] [Google Scholar]
- 5.Sandroni C, Nolan J, Cavallaro F, et al. In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med. 2007;33(2):237–245. doi: 10.1007/s00134-006-0326-z. [DOI] [PubMed] [Google Scholar]
- 6.Ballew KA, Philbrick JT, Caven DE, et al. Differences in case definitions as a cause of variation in reported in-hospital CPR survival. J Gen Intern Med. 1994;9(5):283–285. doi: 10.1007/BF02599658. [DOI] [PubMed] [Google Scholar]
- 7.Ebell MH, Becker LA, Barry HC, et al. Survival after in-hospital cardiopulmonary resuscitation. A meta-analysis. J Gen Intern Med. 1998;13(12):805–816. doi: 10.1046/j.1525-1497.1998.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan PS, Khalid A, Longmore LS, et al. Hospital-wide code rates and mortality before and after implementation of a rapid response team. JAMA. 2008;300(21):2506–2513. doi: 10.1001/jama.2008.715. [DOI] [PubMed] [Google Scholar]
- 9.Chan PS, Nichol G, Krumholz HM, et al. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302(11):1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan PS, Krumholz HM, Nichol G, et al. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 11.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association Circulation. 1997;95(8):2213–2239. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 12.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 13.Szklo M, Nieto FJ. Epidemiology: Beyond the Basics. Gaithersburg: Aspen Publishers; 2000. [Google Scholar]
- 14.Groeneveld PW, Laufer SB, Garber AM. Technology diffusion, hospital variation, and racial disparities among elderly Medicare beneficiaries: 1989–2000. Med Care. 2005;43(4):320–329. doi: 10.1097/01.mlr.0000156849.15166.ec. [DOI] [PubMed] [Google Scholar]
- 15.Merchant RM, Becker LB, Yang F, et al. Racial disparities in survival after out-of-hospital cardiac arrest. Am Heart J. in press. accepted February 2011.
- 16.Hougaard P, Lee ML, Whitmore GA. Analysis of overdispersed count data by mixtures of Poisson variables and Poisson processes. Biometrics. 1997;53(4):1225–1238. [PubMed] [Google Scholar]
- 17.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 18.Curran D, Molenberghs G, Fayers PM, et al. Incomplete quality of life data in randomized trials: missing forms. Stat Med. 1998;17:697–709. doi: 10.1002/(sici)1097-0258(19980315/15)17:5/7<697::aid-sim815>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 19.Ford BL. Incomplete data in sample surveys. New York: Academic Press; 1983. An overview of hot-deck procedures. [Google Scholar]
- 20.Nichol G, Thomas E, Callaway CW, et al. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300(12):1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldberger JJ, Cain ME, Hohnloser SH, et al. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and Prevention. Circulation. 2008;118(14):1497–1518. [PubMed] [Google Scholar]
- 22.Tunstall-Pedoe H, Bailey L, Chamberlain DA, et al. Survey of 3765 cardiopulmonary resuscitations in British hospitals (the BRESUS Study): methods and overall results. BMJ. 1992;304(6838):1347–1351. doi: 10.1136/bmj.304.6838.1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361(1):22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barach P, Small SD. Reporting and preventing medical mishaps: lessons from non-medical near miss reporting systems. BMJ. 2000;320(7237):759–763. doi: 10.1136/bmj.320.7237.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Franklin C, Mathew J. Developing strategies to prevent inhospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med. 1994;22(2):244–247. [PubMed] [Google Scholar]
- 26.Schein RM, Hazday N, Pena M, et al. Clinical antecedents to in-hospital cardiopulmonary arrest. Chest. 1990;98(6):1388–1392. doi: 10.1378/chest.98.6.1388. [DOI] [PubMed] [Google Scholar]
- 27.Smith AF, Wood J. Can some in-hospital cardio-respiratory arrests be prevented? A prospective survey. Resuscitation. 1998;37(3):133–137. doi: 10.1016/s0300-9572(98)00056-2. [DOI] [PubMed] [Google Scholar]
- 28.Bedell SE, Pelle D, Maher PL, et al. Do-not-resuscitate orders for critically ill patients in the hospital. How are they used and what is their impact? JAMA. 1986;256(2):233–237. [PubMed] [Google Scholar]
- 29.Peberdy MA, Ornato JP, Larkin GL, et al. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 30.Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPR overview: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 122(18 Suppl 3):S676–684. doi: 10.1161/CIRCULATIONAHA.110.970913. [DOI] [PubMed] [Google Scholar]
- 31.Bhanji F, Mancini ME, Sinz E, et al. Part 16: education, implementation, and teams: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 122(18 Suppl 3):S920–933. doi: 10.1161/CIRCULATIONAHA.110.971135. [DOI] [PubMed] [Google Scholar]
- 32.Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 122(18 Suppl 3):S768–786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 33.Chan PS, Jain R, Nallmothu BK, et al. Rapid Response Teams: A Systematic Review and Meta-analysis. Arch Intern Med. 170(1):18–26. doi: 10.1001/archinternmed.2009.424. [DOI] [PubMed] [Google Scholar]
- 34.Wenger NS, Pearson ML, Desmond KA, et al. Changes over time in the use of do not resuscitate orders and the outcomes of patients receiving them. Med Care. 1997;35(4):311–319. doi: 10.1097/00005650-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 35.Peterson ED, Roe MT, Chen AY, et al. The NCDR ACTION Registry-GWTG: transforming contemporary acute myocardial infarction clinical care. Heart. 96(22):1798–1802. doi: 10.1136/hrt.2010.200261. [DOI] [PubMed] [Google Scholar]
- 36.Rogers WJ, Bowlby LJ, Chandra NC, et al. Treatment of myocardial infarction in the United States (1990 to 1993). Observations from the National Registry of Myocardial Infarction. Circulation. 1994;90(4):2103–2114. doi: 10.1161/01.cir.90.4.2103. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.