Abstract
BACKGROUND
To enhance the impact of school nutrition programs on children’s health, more information is needed on the associations between healthy and unhealthy food offerings during school lunch periods and children’s eating behavior. The purpose of this study is to evaluate the contributions of food offerings and participation in school lunch programs on children’s overall (both in- and out-of-school) eating behavior.
METHODS
A cross-sectional observational study was conducted in which 2039 students in 12 elementary and 10 middle schools reported their eating behavior and the frequencies with which they purchased meals and à la carte items in the school cafeteria. Food service managers from each school provided information on the availability of foods and beverages during school lunch periods. Multilevel regression analyses were conducted to identify school- and student-level predictors of children’s eating behavior.
RESULTS
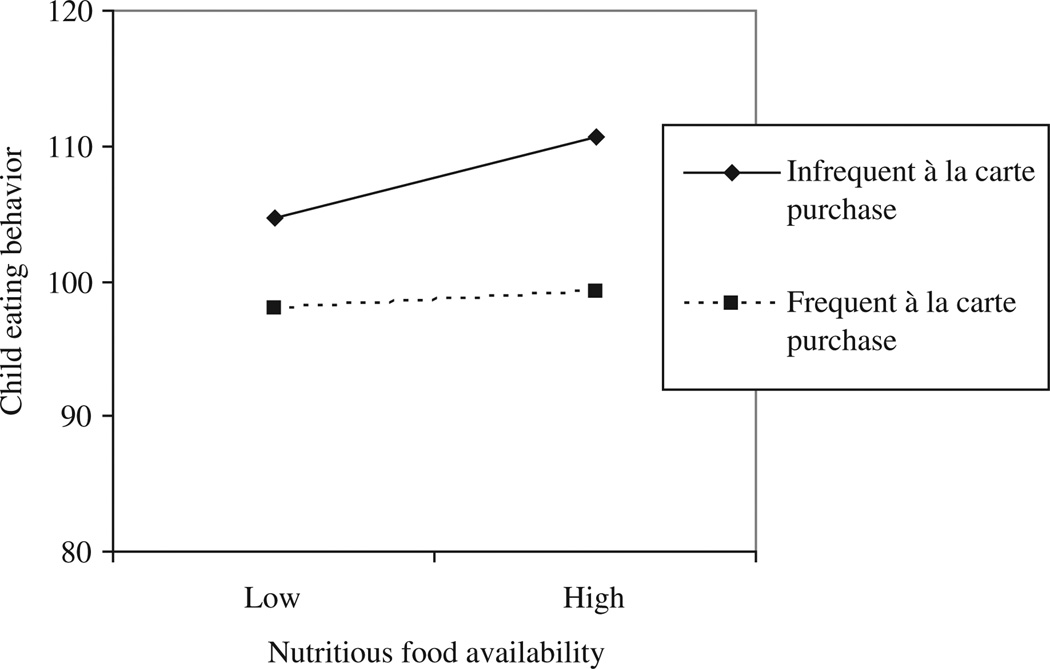
The availability of nutritious foods during school lunch periods was associated with healthier eating behavior among students. However, this effect was observed only among children who infrequently purchased à la carte food items, and not among those who were frequent purchasers.
CONCLUSION
Increased availability of fruits, vegetables, whole grains, and low-fat dairy products as components of school meals may be an effective strategy to promote healthy eating behaviors among children. Improving the nutrition standards for foods offered in competition with federally reimbursable school meals may enhance the positive effects of school meal programs on student eating behavior.
Keywords: school nutrition services, nutrition standards in schools, competitive foods in schools, child eating behavior
School nutrition services provide access to a variety of nutritious foods that promote students’ health and their capacity to attend to academic tasks.1 About 94% of schools in the United States, both private and public, participate in the National School Lunch Program (NSLP). Schools are therefore uniquely positioned to promote healthy eating behaviors and attitudes toward food among the vast majority of American children.2–4
Nutrition service programs in NSLP-participating schools must abide by federal and state policies that mandate compulsory nutrient-based standards for school meals. The Healthy Meals for Healthy Americans Act of 1994 requires that NSLP-participating schools serve balanced and nutritious meals that comply with the United Stated Department of Agriculture (USDA) Dietary Guidelines for Americans.5,6 Participating schools are required to serve lunches that provide at least one third of children’s recommended daily food and nutrient intake, meet specific macronutrient and micronutrient requirements, and include a variety of meat/meat alternatives, whole grains, fruits, vegetables, and low-fat dairy options.6,7
The availability of nutritious foods as part of school meals increases children’s consumption of whole grains,8,9 fruits,10 vegetables,10 and low-fat milk.11,12 In the past decade, there have been several notable improvements to school meals with respect to the nutrient properties of available foods and the use of healthier food preparation practices.3,13,14 In addition, the Centers for Disease Control & Prevention (CDC) and the Institute of Medicine (IOM) issued a set of recommended nutrition standards for foods offered in competition with federally reimbursable meals in 2007.15 Preliminary evidence suggests that high fat/calorie and low nutrient “competitive” foods/beverages are becoming less available in some schools,16,17 but the IOM’s recommendations are not yet legislated at the federal level and the degree to which they have been adopted at local levels is unknown. Currently, high fat/calorie and low nutrient foods remain abundantly available in many schools through à la carte services in the cafeteria, school stores, and vending machines.14,15 Most states (58%) and the majority of school districts (61%) permit the sale of competitive foods and beverages, which are neither regulated by federal nutrition guidelines nor likely to conform to nutrient intake recommendations.15 Access to competitive foods may counteract the beneficial effects of nutritious school meals and pose a significant barrier to the establishment of health-promoting school environments.15,18,19
Despite the potential importance of school nutrition programs to students’ health, there has been limited research attention given to how program policies and practices affect students’ overall eating behavior, particularly outside of school.19 We conducted an observational study to test the hypothesis that the availability of nutritious foods during school lunch periods, as indicated by compliance with USDA recommendations, would be positively associated with children’s healthier eating behavior both in and out of school. Furthermore, we expected that the frequency with which students purchased school meals would enhance the positive effect of healthier food availability on student behavior, whereas the frequency of competitive (à la carte) food purchasing would diminish this effect.
METHODS
Subjects
Food Service Managers
All food service managers employed at the participating schools (N = 22) agreed to complete semistructured interviews regarding their school’s nutrition service policies and practices.
Schools and Students
Data were collected in 22 public schools (12 elementary schools and 10 middle schools) in 3 rural school districts in 2 states. For each school, the percentage of students eligible for free and reduced meals (FARMs) was ascertained from state records. Students’ reports of school nutrition program participation and eating behavior were obtained from 2039 children in grades 5 to 8 who participated in Project Healthy Pathways, a study of children’s health during childhood-to-adolescence transitions. Informed parental consent was obtained for 72% of students eligible to participate and 99% of students with parental consent completed the student questionnaire.
Instruments
The Availability of Healthier Foods During School Lunch Periods
Semistructured interview questions used to assess food availability were derived from the CDC’s School Health Programs and Policies Study (SHPPS) Food Service School Questionnaire, a reliable and valid measure of these policies and practices.13,20,21 For each item, fulfillment of the criteria was coded as 1 and non-fulfillment as 0. An index representing the degree to which schools met the recommended level of food availability was calculated by averaging the items (Table 1).
Table 1.
Percentage of Schools in Compliance With USDA Requirements/Recommendations for Food Availability During School Meal Periods
| Frequencies: SHPPS 2006 |
Frequencies: Present Sample |
|
|---|---|---|
| In the past month, on how many days were… | ||
| students offered at least 1 low-fat or nonfat dairy product, including milk for lunch?† | 98% | 95% |
| students offered at least 1 food containing whole grain for lunch?‡ | 70% | 30% |
| students offered 2 or more different entrees ormain courses for lunch?† | 74% | 75% |
| students offered 2 or more different nonfried vegetables for lunch?† | 69% | 35% |
| students offered 2 or more different types of fruit or 100% fruit juice for lunch?† | 71% | 80% |
| deep-fried foods sold to students as part of a meal or as á la carte items?§ | 31% | 95% |
USDA requirements/recommendations:
Once per day;
5 or more times per week;
never.
Student Participation in School Lunch Programs
The frequency with which students participated in school lunch programs (purchase of meals and à la carte items in the cafeteria) was assessed using 2 questions. Meal participation was determined through students’ responses to the question, “How many days a week do you usually get a meal from the school cafeteria during lunch?” À la carte participation was determined through students’ responses to the question, “How many days a week do you usually get a snack or dessert, like chips, pretzels, or ice cream from the school cafeteria during lunch?” Both questions had 6-point Likert response options with the following categories: no days (coded: 0), 1 day, 2 days, 3 days, 4 days, and 5 days. In all participating schools, students had the option to select a meal, 1 or more à la carte items, or both. School policies did not restrict students from selecting a meal or à la carte item in the absence of the other.
Student Eating Behavior
Students completed an 8-item measure of their positive and negative eating behavior. This scale was primarily composed of items from the Children’s Health and Illness Profile (CHIP), which have been shown to reliability and accurately assess children’s health behavior.22 Three additional items that assess the consumption of chips, sweets, and fast foods were added to the CHIP nutrition behavior scale. Using 5-point Likert scale response options (never, a few days a month, several days a week, about every day, more than once a day), children indicated the frequencies with which they ingested healthy and unhealthy food and beverage items during the past 4 weeks. All items we coded so that higher values indicated healthier eating behavior and a score for the eating behavior subscale was calculated by averaging item responses. In the present sample, the scale had adequate internal consistency reliability (α = .71). The items used to assess student eating behavior and item descriptive statistics are presented in the appendix.
Appendix.
Child Eating Behavior Items and Descriptive Statistics
| Item | Mean (SD) |
Floor (%) |
Ceiling (%) |
|---|---|---|---|
| In the past 4 weeks, how often did you … | |||
| eat fruit† | 3.6 (1.1) | 3.1 | 24.4 |
| eat raw vegetables† | 2.5 (1.2) | 29.2 | 7.1 |
| eat cooked vegetables† | 3.1 (1.2) | 12.1 | 13.5 |
| drink soda or other soft drinks that contain sugar?‡ | 2.7 (1.2) | 22.8 | 5.6 |
| drink milk?† | 3.7 (1.2) | 7.8 | 30.7 |
| eat potato chips, corn chips, or other kinds of chips?‡ | 3.00 (1.1) | 11.3 | 5.8 |
| eat cake, candy, or other sweets?‡ | 3.2 (1.1) | 10.9 | 6.3 |
| eat foods such as hamburgers, French | 3.2 (1.1) | 9.8 | 4.4 |
| fries, or fried chicken bought at a fast food restaurant or market?‡ |
Response options (codes): never (1); a few days a month (2); several days a week (3); about every day (4); more than once a day (5).
Response options (codes): more than once a day (1); about every day (2); several days a week (3); a few days a month (4); never (5).
Procedures
Advanced graduate students administered the semi-structured nutrition service interview to the food service managers who provided informed written consent for their participation in the study. Students with parental consent and child assent completed questionnaires at school. Participating children in fifth grade completed the student questionnaire as a survey administrator read the questions aloud. Students in grades 6 to 8 completed the questionnaire by reading the items silently. All data collection was monitored by research staff and a school staff member. Student questionnaires were administered within 45 days of the food service manager interview.
Data Analysis
Analyses were conducted to identify school- and student-level predictors, as well as cross-level interactions, of eating behavior. Multilevel modeling techniques were applied to address the effects of clustering of students within schools on standard error estimates and because the hypothesized predictor variables operated at different levels (school and student levels) and were expected to interact across levels to predict student eating behavior.
Initially, an unconstrained 1-way random effects ANOVA model was fit to the data. The unconstrained model was used to identify the amount of variance in student eating behavior that exists between-schools for the purpose of determining whether a multilevel model is necessary in subsequent analyses. The model revealed that 15.5% of variation was attributable to differences between schools. The estimated variance component underlying this value was statistically significant (p < .0001), indicating that the between-school variation is consequential and permits explanation.23 Thus, 3 hierarchical linear models were tested to determine and explain the relative proportion of student eating behavior associated with between-schools and between-students variation.
The multilevel analyses were conducted with SAS 12.2 following Singer’s recommendations.24 The purpose of model 1 was to identify the school-level effects that were associated with student eating behavior. This model regressed eating behavior averaged at the school level (ie, the school-level intercept) on healthier food availability, controlling for school type (elementary or middle), and the percentage of FARMs eligibility. The unit of analysis for model 2 was the student. This model assessed the between-students effects of participation in the school lunch program (purchase of meals and à la carte items) on eating behavior. In model 3, we considered slopes-as-outcomes to assess the degree to which student participation modified the effects of healthier food availability on student eating behavior (cross-level interaction models). To enhance interpretation of the multilevel models, eating behavior scores were standardized (mean = 100, SD = 20); the continuous school-level covariates were grand mean centered; and student-level covariates were centered around school means.
RESULTS
Participating students were 49% male, 17% African American, 81% White, 2% of another race, and 3% Hispanic. Based on US Census Bureau poverty thresholds for 2006, 23% of children were from families living below the poverty line. State records for the academic year during which the study was conducted indicated that 58% (range = 24% to 98%) of students in the participating schools were eligible to participate in the USDA Free and Reduced Meal Programs. On average, food service managers had 16.6 (SD = 12.0) years of experience working in school nutrition service programs; 81% had at least a high school diploma or general equivalency diploma (GED); and 91% reported having received school nutrition service training sponsored by their state.
Descriptive analyses of food availability items indicated that relative to schools in nationally representative samples,21,13 schools in the present sample less frequently offered whole grain foods, vegetables, and fried foods (Table 1). On average, students reported that they purchased meals 3.5 (SD = 1.9) days per week and à la carte items 1.9 (SD = 1.7) days per week. Intercorrelations among school variables and student variables aggregated at the school level indicated that the percentage of students eligible for participation in the FARMs program was positively associated with the frequency of purchasing meals (r = .42, p < .05) and negatively associated with healthier eating behavior (r = −.59, p < .01).
Table 2 summarizes multilevel modeling results for analyses predicting students’ eating behavior. The “school/program only” model assessed the extent to which school and program characteristics explained behavior. This model accounted for 79.5% of the explainable between-school variation in student eating behavior. Consistent with bivariate correlations, the most powerful school-level predictor of student eating behavior was the percentage of students eligible for FARMs. School FARMs rates were inversely related to student eating behavior. In addition, the degree to which schools made nutritious foods available during lunch periods was associated with improved eating behavior among students. The “student only” model assessed the extent to which variation in students’ eating behavior was explained by the frequency with which they purchased meals and àla carte items during school lunch periods. This model accounted for 10.4% of the between-student variance in eating behavior. The frequency with which students purchased à la carte items at lunch predicted poorer eating behavior.
Table 2.
Multilevel Models Explaining Child Eating Behavior†
| Child Eating Behavior (estSE) | |||
|---|---|---|---|
| Variables | School/ Program Only (Model 1) |
Student Only (Model 2) |
School/ Program & Student (Model 3) |
| Intercept terms | |||
| Reference intercept | 103.4(1.2) | 101.3(1.1) | 103.2(1.2) |
| FARMs rates | −18.0(5.2)** | −17.1(5.3)** | |
| School type‡ | −4.0(1.5)* | −4.4(1.5)* | |
| Food availability | 10.0(4.7)* | 10.4(4.8)* | |
| Slope terms | |||
| Days purchased meals | 0.4(0.3) | 0.4(0.3) | |
| Days purchased á la carte | −2.8(0.3)**** | −2.8(0.3)**** | |
| Food availability × days purchased meals | 0.4(1.8) | ||
| Food availability × days purchased á la carte | −4.4(1.7)* | ||
p < .05;
p < .01;
p < .0001.
FARMs rates and class program characteristics were centered at the grand mean and student participation variables were centered around school means.
School type: 0 = elementary schools, 1 = middle schools.
The “school/program & student” model assessed the extent to which student participation in the nutrition service program (as indicated by the frequency with which students purchased school meals and à la carte items) modified the effects of healthier food availability on students’ eating behavior. This model accounted for 77.5% of the explainable between-school variation and 10.5% of the between-student variation in eating behavior. The relation between the availability of nutritious foods and eating behavior differed depending on the frequency with which students purchase à la carte items. A plot of the significant 2-way interaction (food availability × student purchase of à la carte items) revealed that the availability of nutritious school lunch offerings had positive effects on the eating behavior of students who infrequently purchased à la carte items, but virtually no effect on the eating behavior of students who frequently purchased à la carte items (Figure 1).
Figure 1.
The Mitigating Effect of à la Carte Food Purchasing in the Relation Between Nutritious Food Availability and Children’s Eating Behavior
DISCUSSION
This study examined the influence of healthier food availability during school lunch on children’s overall eating behavior. The availability of fruits, vegetables, whole grains, and low-fat dairy products were associated with healthier eating behavior. Unfortunately, these positive effects were attenuated by access to poorly regulated competitive foods available for purchase in school cafeterias. Students who frequently purchased a snack or dessert (eg, chips, pretzels, or ice cream) during school lunch periods had poorer eating behavior overall, an effect that undermined the positive contributions of healthier school meals on children’s balanced nutrition. This finding suggests that improving the nutrition standards for competitive school foods may enhance the positive effects of school meal programs.15 In the present sample, children who attended schools with higher rates of FARMs eligibility reported poorer overall eating behavior. Increasing access to nutritious meals and reducing access to unregulated competitive foods in schools may help reduce socioeconomic-based disparities in eating behavior.
Limitations
Several limitations of this study merit discussion. First, there are some differences between the present sample and the nationally representative school sample with respect to food availability. These differences may pose challenges to the generalizability of study findings, but may also reflect recent changes in state-, district-, and school-level policies and practices geared toward improving the nutrient properties of foods offered during school meals (eg, prohibiting or limiting the sale of deep-fried foods). Second, several confounding factors that may impact students’ eating behaviors were not assessed in this study. Student participation in breakfast programs, nutrition education, and the nutrient properties of foods offered outside of the school food service program (eg, vending, fund-raisers) are important components of school food environments that should be considered in future research.17,25 Third, although cafeteria managers were assured that their responses to interview questions were private and confidential, their reports of program quality are susceptible to social desirability bias. Similarly, despite evidence that children are generally reliable and accurate reporters of their eating behaviors,26 we did not corroborate child-reported eating data with that obtained using other valid child nutrition assessment methodologies. Finally, although we recognize that food service programs can differ substantially across school level (eg, decreased program participation and increased availability of à la carte food and beverages in high schools),17,27 this study was conducted exclusively in elementary and middle schools. Future research should explicate the effects of school nutrition program characteristics and student participation on the eating behavior of high school students.
Conclusions
Schools can positively impact children’s eating behavior by increasing the availability of healthy foods such as fruits, vegetables, whole grains, and low-fat dairy products. However, the abundant availability of poorly regulated, often unhealthy foods offered in competition with federally reimbursable school meals undermines the positive effects of school nutrition programs.
IMPLICATIONS FOR SCHOOL HEALTH
This study provides support for mandated implementation of nutrient standards for foods and beverages provided outside of federally funded school meal programs. To be effective, policies must clearly delineate expectations for the many individuals who influence school food environments including district- and school-level food service managers, commercial vendors, school administrators, teachers, parents, and students. Methods to track implementation of the policies as well as their effects on child nutrition and school operations and finances should also be specified. Future research should focus on the effectiveness of these policies and other novel approaches to restricting students’ access to unregulated competitive foods in schools. For example, local education agencies could control the availability of competitive foods by restricting the amount of time that these foods are made available to students. Some schools only allow students access to à la carte foods after USDA-compliant meal service is complete. In addition, future research should focus on identifying factors that are associated with excessive à la carte availability or purchasing (eg, student-level or school-level factors such as monetary access or contracts with food vendors) as these factors may indicate opportunities for healthy eating interventions. The availability and promotion of nutritious foods in schools provide a foundation for other health-promoting efforts such as applied nutrition education and family-school-community collaborative programs, which together, may be among the most promising strategies to undermine the epidemic of poor childhood nutrition.
Human Subjects Approval Statement
This study was approved by the institutional review boards of the Children’s Hospital of Philadelphia and the Johns Hopkins Bloomberg School of Public Health.
Contributor Information
Katherine B. Bevans, Email: bevans@email.chop.edu.
Betty Sanchez, Email: sanchezb@email.chop.edu.
Rachel Teneralli, Email: tenerallir@email.chop.edu.
Christopher B. Forrest, Email: forrestc@email.chop.edu.
REFERENCES
- 1.Caldwell D, Nestle M, Rogers W. School nutrition services. In: Marx E, Wooley SF, Northrop D, editors. Health Is Academic: A Guide to Coordinated School Health Programs. New York, NY: Teachers College Press; 1998. pp. 195–223. [Google Scholar]
- 2.Perez-Rodrigo C, Aracenta J. School-based nutrition education: lessons learned and new perspectives. Public Health Nutr. 2001;4(1A):131–139. doi: 10.1079/phn2000108. [DOI] [PubMed] [Google Scholar]
- 3.Wojcjcki JM, Heyman MB. Healthier choices and increased participation in a middle school lunch program: effects of nutrition policy changes in San Francisco. Am J Public Health. 2006;96(9):1542–1547. doi: 10.2105/AJPH.2005.070946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ralston K, Newman C, Clauson A, Guthrie J, Buzby J, editors. The National School Lunch Program: Background, Trends, and Issues. 2008. No. EER-61. [Google Scholar]
- 5.US Department of Agriculture and US Dept of Health and Human Services. Dietary Guidelines for Americans. [Accessed September 3, 2009];2005 Available at: http://www.health.gov/dietaryguidelines/dga2005/document/default.htm.
- 6.Healthy Meals for Healthy Americans Act. 1994:§ 18. Pub. L. No. 103-448. [Google Scholar]
- 7.US Department of Agriculture, Food and Nutrition Service, Team Nutrition. Menu Planner for Healthy School Meals. [Accessed June 3, 2009]; Available at: http://teamnutrition.usda.gov/Resources/nutrientanalysis.html.
- 8.Chan HW, Burgess Champoux T, Reicks M, Vickers Z, Marquart L. White whole-wheat flour can be partially substituted for refined-wheat flour in pizza crust in school meals without affecting consumption. [Accessed September 15, 2009];J Child Nutr Manage. 2008 32(1) Available at: http://www.schoolnutrition.org/Content.aspx?id=10584. [Google Scholar]
- 9.Rosen R, Sadeghi L, Schroeder N, Reicks M, Marquart L. Gradual incorporation of whole wheat flour into bread products for elementary school children. [Accessed September 15, 2009];J Child Nutr Manage. 2008 32(2) Available at: http://www.schoolnutrition.org/Content.aspx?id=10584. [Google Scholar]
- 10.Thompson V, Cullen KW, Watson K, Zakeri I. Increased availability and marketing of fruit, juice and vegetables to middle school students increase consumption. [Accessed September 15, 2009];J Child Nutr Manage. 2007 31(1) Available at: http://docs.schoolnutrition.org/newsroom/jcnm/07spring/thompson/index.asp. [Google Scholar]
- 11.Connors P, Bednar C. Promoting a calcium initiative in school cafeterias. [Accessed September 15, 2009];J Child Nutr Manage. 2002 26(2) Available at: http://docs.schoolnutrition.org/newsroom/jcnm/02fall/conners/ [Google Scholar]
- 12.Gordon AR, McKinney P. Sources of nutrients in students’ diets. Am J Clin Nutr. 1995;61(1 suppl):232S–240S. doi: 10.1093/ajcn/61.1.232S. [DOI] [PubMed] [Google Scholar]
- 13.O’Toole TP, Anderson S, Miller C, Guthrie J. Nutrition services and foods and beverages available at school: results from the School Health Policies and Programs Study 2006. J Sch Health. 2007;77(8):500–521. doi: 10.1111/j.1746-1561.2007.00232.x. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Agriculture and US Dept of Health and Human Services. SHPPS 2006: Changes Between 2000 and 2006. [Accessed September 3, 2009]; Available at: http://www.cdc.gov/healthyyouth/shpps/2006/factsheets/pdf/FS_Trends_SHPPS2006.pdf.
- 15.Institute of Medicine. Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 16.Terry-McElrath YM, O’Malley PM, Delva J, Johnston LD. The school food environment and study body mass index and food consumption: 2004 to 2007 national data. J Adolesc Health. 2009;45:S45–S56. doi: 10.1016/j.jadohealth.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Story M, Nanney MS, Schwartz MB. Schools and obesity prevention: creating school environments and policies to promote healthy eating and physical activity. Milbank Q. 2009;87(1):71–100. doi: 10.1111/j.1468-0009.2009.00548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harper JD. Childhood obesity: Strategies for prevention. Fam Community Health. 2006;29(4):288–298. doi: 10.1097/00003727-200610000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Leviton LC. Children’s healthy weight and the school environment. Ann AAPSS. 2008;615(1):38–55. [Google Scholar]
- 20.Brener ND, Kann L, Smith TK. Reliability and validity of the school health policies and program study 2000 questionnaires. J Sch Health. 2003;73(1):29–37. doi: 10.1111/j.1746-1561.2003.tb06556.x. [DOI] [PubMed] [Google Scholar]
- 21.Kyle TM, Brener ND, Kann L, et al. Methods: school health policies and programs study 2006. J Sch Health. 2007;77(8):398–407. doi: 10.1111/j.1746-1561.2007.00227.x. [DOI] [PubMed] [Google Scholar]
- 22.Riley AW, Forrest CB, Rebok GW, Starfield B, Green BF, Robertson JA. The child report form of the CHIP-Child Edition: reliability and validity. Med Care. 2004;42(3):221–231. doi: 10.1097/01.mlr.0000114910.46921.73. [DOI] [PubMed] [Google Scholar]
- 23.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Los Angeles, CA: University of California Los Angeles; 2002. [Google Scholar]
- 24.Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;24(4):323–355. [Google Scholar]
- 25.Tester JM. Mobile food vending and after-school environment. Am J Prev Med. 2010;38(1):70–73. doi: 10.1016/j.amepre.2009.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoelscher DM, Days SR, Kelder SH, Ward JL. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. J Am Diet Assoc. 2003;103(1):186–193. doi: 10.1053/jada.2003.50031. [DOI] [PubMed] [Google Scholar]
- 27.U. S. Government Accountability Office. School Meal Programs: Competitive Foods Are Widely Available and Generate Substantial Revenues for Schools. Washington, DC: General Accounting Office; 2005. No. GAO-05-563. [Google Scholar]