Abstract
BACKGROUND
Endometriosis is the most common gynecological diagnosis among women with chronic pelvic pain, but the underlying mechanisms of endometriosis-associated chronic pelvic pain remain unclear. Therefore, the objective of this study was to determine the biopsychosocial predictors of pain improvement among women with endometriosis.
METHODS
One hundred and fifteen women who presented for treatment of endometriosis-associated chronic pelvic pain at a tertiary referral center at a university-based hospital participated in this prospective observational study of clinical practice. Participants completed questionnaires assessing pain, mental health and catastrophizing at entry and 1 year follow-up. The main outcome measure assessed was the interval change in pain report using the McGill pain 1uestionnaire.
RESULT(S)
On average, participants experienced a 37.4% reduction in interval pain (P < 0.001). Adjusted for baseline pain, nulliparity (P = 0.002) and catastrophizing (P = 0.04) were associated with decreased probability of interval improvement in pain. Those referred for physical therapy had less interval pain improvement (P = 0.04). However, undergoing hysterectomy was a strong predictor of improvement in pain (P = 0.008).
CONCLUSION(S)
Our study suggests that chronic pain in endometriosis may be more akin to other idiopathic pain disorders. Specifically, biopsychosocial variables, such as catastrophizing, play an important role in reported severity. Further research on biopsychosocial correlates of chronic pelvic pain in endometriosis is warranted.
Keywords: chronic pelvic pain, endometriosis, catastrophizing, pain-related outcomes, psychological factors
Introduction
Among women with chronic pelvic pain, endometriosis has an estimated prevalence of 33%, making it the most common gynecological diagnosis in this population (Guo and Wang, 2006). To date, the classification and treatment of endometriosis has been based on a biomolecular conceptualization. However, the underlying mechanisms of endometriosis-associated chronic pelvic pain remain unclear. In recent years, there has been a growing interest in the standardized assessment of clinical outcomes in endometriosis. In accordance with the initiative on methods and measurement and pain assessment in clinical trials, such an approach will necessitate the objective assessments in both biomedical and psychosocial domains (Vincent et al., 2010). To this end, this study examines the biopsychological correlates of pain report at 1 year in a group of women undergoing treatment for endometriosis-associated chronic pelvic pain.
Within the larger community of chronic pain patients, there is a growing recognition that biomedical variables, such as disease severity, cannot sufficiently explain levels of pain and psychological adjustment (Vercellini et al., 2007; Taylor and Williams, 2010). We speculate that persistent pain in endometriosis may be similar to other pain disorders in that psychosocial variables may play as great of a role as biomedical factors in pain report. Therefore, the assessment of coping mechanisms such as catastrophizing—a well known modifier of chronic pain treatment outcomes—may shed light on the influence of psychosocial domains on gynecological pain report and treatment outcomes.
Catastrophizing is a term that was originally used by Beck et al. (1979) to describe a maladaptive coping style used by patients with anxiety and depressive disorders. More recently, it has been defined as a negative cognitive and emotional coping response to pain, and it includes the tendency to amplify and focus on pain symptoms as well as feelings of helplessness and pessimism (Sullivan et al., 2001). Catastrophizing has emerged as an important determinant of short- and long-term pain-related outcomes and consistently been associated with higher pain levels. This relationship holds true in a variety of conditions such as neuropathic pain, low back pain and scleroderma (Buer and Linton, 2002; Turner et al., 2002; Sullivan et al., 2005; Edwards et al., 2006a,b; Hanley et al., 2008). Across both non-patient and chronic pain populations, it has been shown that individuals reporting high levels of catastrophizing demonstrate increased musculoskeletal tenderness and heightened pain sensitivity; they also appear to be at a higher risk for the development of post-surgical and persistent pain syndromes (Severeijns et al., 2001, 2004; Granot and Ferber, 2005; Turner et al., 2005).
The exact mechanism through which catastrophizing is related to pain is not entirely understood. It has been postulated that the emotional and cognitive changes that characterize catastrophizing may disrupt descending endogenous pain-inhibitory pathways (Sullivan et al., 2001). Furthermore, catastrophizing is shown to be associated with enhanced activity in the pain-processing regions of the brain (Gracely et al., 2004; Seminowicz and Davis, 2006; Lloyd et al., 2008). Most notably, however, since endometriosis is an inflammatory process, findings of a positive association between catastrophizing and inflammatory cytokines in conditions such as rheumatoid arthritis may be relevant to the study of pain in endometriosis (Evers et al., 2003; Yin et al., 2005; Edwards et al., 2008).
In this study, we hypothesized that among women with endometriosis, those with higher levels of catastrophizing would experience greater pain at baseline and at 1-year. Specifically, we sought to investigate the effect of the following variables on pain report at baseline and 1-year follow up: demographic factors (e.g. age, education, parity), clinical histories (e.g. pain duration, prior treatments), interval treatments (e.g. medical, surgical) and psychosocial factors (e.g. mental health, catastrophizing). For validation purposes, we also investigated whether or not we were able to replicate the findings of others with respect to the beneficial effects of hysterectomy in our cohort (Lamvu, 2011).
Materials and Methods
Sample and procedure
A total of 115 women with endometriosis were consecutively recruited from a tertiary referral pelvic pain clinic between April 2003 and September 2006. The Institutional Review Board of the University of North Carolina (UNC) approved the study. All English-speaking and literate women between the ages of 18 and 65 who were new referrals for evaluation of endometriosis-associated chronic pelvic pain at the UNC pelvic pain clinic were eligible for participation. We did not exclude anyone based on pre-existing psychological and/or physical condition. These patients were part of a larger, previously published study on psychosocial correlates of chronic pelvic pain (Meltzer-Brody et al., 2007). From the larger study (n = 628 enrolled of 722 eligible), 459 were new referrals to the clinic and were asked to be in a longitudinal study. Of those, 310 agreed to participate and returned at least one follow-up questionnaire (67.5% return rate). For the current paper, we studied only those new longitudinal patients with endometriosis-associated chronic pelvic pain (n = 123). We excluded eight patients for whom we could not identify medical record data; thus, our cohort consists of 115 participants. Later, we describe in detail our methodology for ascertainment of endometriosis-associated chronic pelvic pain case status.
Following informed consent and prior to examination, participants completed a battery of questionnaires assessing severity of pain, quality of life and psychosocial variables such as catastrophizing. In addition, participants completed a baseline demographic and medical history questionnaire before undergoing standard evaluation by the clinical team. The examining physicians, regionally recognized as experts in the field of pelvic pain, did not review participants’ questionnaire responses. Their findings, diagnostic impressions and recommended treatments [e.g. medications, surgery, referral to physical therapy (PT)] at baseline and over the follow-up year were recorded in electronic medical records. A team of four trained research associates then abstracted these data.
We used two complimentary methods for ascertaining case status as endometriosis- associated pelvic pain: (i) patient self-report on entry per demographic questionnaire and (ii) review of electronic medical records. Based on our record review, we could confirm a surgically based diagnosis of endometriosis for 111 patients; four women were surgically diagnosed during the study period. Therefore, our cohort consists of 115 women who were surgically diagnosed with endometriosis and experienced intractable pelvic pain despite conventional treatment modalities; 93% completed the 1 year pain questionnaire.
Measures
Demographic and clinical history
The baseline study entry questionnaire provided demographic and medical history information concerning age, years of education, race, marital status, duration of pelvic pain, number of prior surgeries for pelvic pain and previous hysterectomy. Number of prior surgeries for pelvic pain was truncated to six surgeries in order to reduce outliers. As a result of our population demographics, the race and marital status variables were treated as bivariates in data analyses (e.g. Caucasian versus other, married versus not married). When self-reported data were missing for the duration of pelvic pain and previous hysterectomy variables, information on these variables was obtained from the medical records.
Medical records were abstracted for additional demographic and clinical variables (e.g. parity, co-morbid pain disorder) as well as treatments (e.g. surgical versus medical) utilized over the study period. For secondary analyses, we examined those having the most common type of surgery (e.g. hysterectomy) versus other types of pelvic surgery (e.g. oophorectomy, lysis of adhesions). We also abstracted information about the three common types of medical treatments used before the study and during the follow-up year: (i) PT, (ii) hormonal therapies (e.g. oral contraceptive pills, leuprolide, levonorgestrel-releasing intrauterine system) and (iii) central nervous system medications (e.g. antidepressants, anticonvulsants, sleep aids, muscle relaxants). Patients were considered to have another co-morbid pain disorder if any of the following were noted in the electronic medical records from the initial visit: chronic headaches (migraines), irritable bowel syndrome, interstitial cystitis, fibromyalgia, chronic fatigue syndrome, temporomandibular disorder or chronic lower back pain.
Pain
To determine the severity of pelvic pain at baseline and follow-up, the short form McGill pain questionnaire (SF-MPQ) was used (Melzack, 1987). The SF-MPQ has two components, the present pain intensity (PPI) and pain rating index (PRI). The PPI component of the questionnaire consists of a visual analog scale and is conventionally used to assess the present pain levels. Consistent with conventional practice, we used the PRI component (McGill total pelvic pain score) in this study since it provides a global multi-dimensional pain severity rating over time. The McGill total pelvic pain score (PRI component) is composed of 15 groups of qualitative descriptors (11 sensory and 4 affective) that are rated on an intensity scale (0 = none, 1 = mild, 2 = moderate and 3 = severe). Participants were asked to rate the descriptors of the pelvic pain they had experienced in the previous 2 weeks. The McGill total pain score was calculated from the sum of the 15 items, with a range of 0–45. The SF-MPQ is highly correlated with the longer version of the MPQ (Katz et al., 1999). It has demonstrated a high test-rest reliability of 0.96 (Grafton et al., 2005) and a high internal consistency with a Cronbach's α of 0.86 (Mason et al., 2008). Cronbach's α was 0.90 at baseline in the current study.
Mental health
To assess mental health, we used the mental health subscale (norm-based scoring) of the short form 12 Health Survey (SF-12) where a high score indicates better mental health. The SF-12 has a high internal consistency and reproducibility with a Cronbach's α of 0.87 (Ware et al., 2002). It has been shown to be able to discriminate between types and severity of disease between patients with medical disorders alone as well as those with both medical and psychological disorders (McHorney et al., 1993, 1994). The mental health subscale has strong predictive properties for health outcomes with a test-retest reliability of 0.76 (Ware et al., 1996). SF-12 Cronbach's α was 0.89 at baseline in the current study.
Catastrophizing
To measure catastrophizing of pain, we used the catastrophizing subscale of the Coping Strategies Questionnaire: CSQ (Rosenstiel and Keefe, 1983). The CSQ was designed to evaluate cognitive and behavioral coping strategies in chronic pain syndromes. The catastrophizing scale ranges from 0 to 6, with a high score indicating higher catastrophizing (e.g. ‘I feel I can't stand it anymore’; ‘It is terrible and I feel it's never going to get any better’). This scale has been shown to predict poor health in other clinical samples, such as Irritable Bowel Syndrome patients (Drossman et al., 2000). Data analyses were performed with the continuous measure; however, in the text, we report the following groups based on their catastrophizing score (range 0–6): mild (1–2), moderate (3–4) and severe (5–6). The catastrophizing subscale of the CSQ has extensively been utilized in the literature. It has high internal consistency and reliability with a Cronbach's α of 0.78 (Rosenstiel and Keefe, 1983). This scale has been found to have strong predictive properties for health outcomes among patients with painful conditions (Robinson et al., 1997; Schanberg et al., 1997) witha test-retest reliability varying from 0.80 to 0.91 (Rosenstiel and Keefe, 1983). Cronbach's α was 0.73 at baseline in the current study.
Statistical analyses
Statistical analyses were performed using SAS 9.1. Descriptive statistics (mean and standard deviation for continuous variables; frequency and percentages for bivariate variables) for demographics, pain report and psychological variables are reported for the entire cohort in the ‘Descriptive Analyses’ section of the results below. We examined the distributions of the pain variables at baseline and at 12 months to ensure approximate normality. Continuous variables (e.g. catastrophizing) were analyzed as continuous variables but were grouped into categories of mild, moderate and severe for presentation and clarity purposes only. Paired Student's t-tests were used to compare changes in pain over time for the group as a whole.
In order to determine predictors for pain severity at baseline and at 12 months, we ran multiple regression analyses allowing variables with P < 0.10 or those with clinical interest to stay in the models (Table I). For regression analyses of baseline pain (McGill total pelvic pain), we tested the significance of the following predictor variables: (i) demographic factors (age, education, race, marital status, parity), (ii) previous medical history (duration of pelvic pain, number of surgeries for pelvic pain, PT for pain) and (iii) baseline mental health (catastrophizing, SF-12 mental health).
Table I.
Factors associated with baseline pain severitya.
| Baseline McGill total pelvic pain (n= 114) | ||||
|---|---|---|---|---|
| Predictor variables | LS mean | SE | β | P |
| Age | −0.19 | 0.02 | ||
| ≤30 (n= 38; 33%) | 22.10 | 1.36 | ||
| 31–39 (n= 40; 35%) | 18.87 | 1.33 | ||
| ≥40 (n = 36; 32%)b | 17.27 | 1.41 | ||
| Years of education | −0.21 | 0.01 | ||
| High school diploma or less (n = 34; 30%) | 20.78 | 1.36 | ||
| Some college (n = 32; 28%) | 24.04 | 1.40 | ||
| College degree or more (n = 48; 42%)c | 15.42 | 1.15 | ||
| # Prior pelvic surgeries | 0.16 | 0.05 | ||
| None (n = 23; 20%) | 19.36 | 1.77 | ||
| 1–2 (n = 59; 52%) | 17.73 | 1.12 | ||
| ≥3 (n = 32; 28%)d | 22.66 | 1.53 | ||
| Past PT treatment | 0.17 | 0.03 | ||
| Yes (n = 9; 8%) | 25.17 | 2.78 | ||
| No (n = 105; 92%) | 18.95 | 0.81 | ||
| Catastrophizing | 0.35 | <0.001 | ||
| Mild (n = 64; 56%) | 16.78 | 1.08 | ||
| Moderate (n = 37; 33%) | 21.80 | 1.42 | ||
| Severe (n = 13; 11%)e | 25.81 | 2.41 | ||
| R2= 0.35 | ||||
LS, least squared; SE, standard error; β, standardized beta coefficient showing the following: (i) the direction of the relationship and (ii) the amount in standard deviation units that the pain score changed for each unit of the predictor variable.
aTable shows the results of stepwise multiple regression analyses of pain at baseline predicted by demographic, clinical and psychological variables. Only those variables with P < 0.10 are in the final models. P values are based on the non-grouped variables. General linear models controlling for all variables were used to obtain least-squared means and standard errors. Continuous variables (age, years of education, # prior pelvic surgeries, catastrophizing) were grouped for the purposes of presentation and comparison.
bThose who were ≥40 years old had less pain at baseline than those aged younger than 30 years (P = 0.02).
cThose who had at least a college degree had less pain at baseline than those with some college (P < 0.001) or no more than a high school diploma (P = 0.004).
dThose who had undergone ≥3 past pelvic surgeries had more pain at baseline than those who had undergone 1–2 past pelvic surgeries (P = 0.01).
eThose who had severe catastrophizing had more pain at baseline than those with mild catastrophizing (P < 0.001).
For regression analyses of McGill total pelvic pain at 1 year, we first entered baseline pain into the regression models in order to assess the change in pain over time. We then investigated the joint and independent contributions of baseline variables and treatments used during the 1-year follow-up period. Thus, the following variables were included in the predictive models of total pelvic pain at 1 year: (i) baseline McGill total pelvic pain score, (ii) baseline mental health (catastrophizing, SF-12 mental health), (iii) demographic factors (age, race, marital status, education) and (iv) interim treatments (surgery, PT, medications) (Table II). These regression models were run with the continuous form of predictor variables (e.g. catastrophizing, education, age, number of prior pelvic surgeries). For presentation purposes though, we also ran post hoc general linear models with least-squared means (Student's t-tests) for categorical predictors in order to determine which categories of patients (e.g. severe catastrophizing, less than college degree) had more pain. To reduce the number of variables (maximum of nine in all our analysis), we first tested demographic and medical history variables and only included the significant ones in the final model. In addition, due to co-linearity, mental health variables (SF-12 and catastrophizing) were run separately.
Table II.
Predictors of pain severity at 1 year follow-upa.
| 12 months McGill pelvic pain (n = 106) | ||||
|---|---|---|---|---|
| Predictors | LS mean | SE | β | P |
| Baseline McGill pain | 0.30 | 0.003 | ||
| Years of education | −0.15 | 0.07 | ||
| High school diploma or less (n = 31; 29%) | 14.23 | 1.56 | ||
| Some college (n = 29; 27%) | 13.18 | 1.67 | ||
| College degree or more (n = 46; 44%)b | 10.14 | 1.38 | ||
| Parity | −0.25 | 0.002 | ||
| 0 (n = 55; 52%) | 11.89 | 1.89 | ||
| ≥1 (n = 51; 48%) | 6.45 | 1.66 | ||
| Hysterectomy | −0.29 | 0.008 | ||
| Yes (n = 13; 12%) | 5.41 | 2.75 | ||
| No (n = 93; 88%) | 12.94 | 1.04 | ||
| Other pelvic surgery | −0.02 | 0.85 | ||
| Yes (n = 22; 21%) | 8.97 | 2.27 | ||
| No (n = 84; 79%) | 9.38 | 1.35 | ||
| PT treatment | 0.17 | 0.04 | ||
| Yes (n = 49; 46%) | 10.99 | 1.87 | ||
| No (n = 57; 54%) | 7.35 | 1.69 | ||
| Catastrophizing | 0.18 | 0.04 | ||
| Mild (n = 61; 58%) | 11.36 | 1.12 | ||
| Moderate (n = 33; 32%) | 11.56 | 1.50 | ||
| Severe (n = 12; 11%)c | 17.93 | 2.56 | ||
| R2= 0.44 | ||||
LS, least squared; SE, standard error; β, standardized beta coefficient showing the following: (i) the direction of the relationship and (ii) the amount in standard deviation units that the pain variable changed for each unit of the predictor variable.
aTable shows results of stepwise multiple regression of pain at 1 year predicted by demographic, baseline pain, interval treatment and psychological variables. Only those variables with P < 0.10 or of interest are in the final models. P values are based on the non-grouped variables. General linear models controlling for all variables were used to obtain least-squared means and standard errors. Continuous variables (years of education, catastrophizing) were grouped for the purpose of presentation and comparison.
bThose who had at least a college degree tended to have less pain at 1 year than those with a high school diploma or less (P = 0.06), controlling for baseline pain.
cThose with severe catastrophizing had more pain at 1 year than those with moderate catastrophizing (P = 0.03) and those with mild catastrophizing (P = 0.03), controlling for baseline pain.
Descriptive analyses
Our cohort primarily consisted of Caucasian (85%), married women (67%), aged 19–45 (85%) with at least some college education (70%); 46% were parous. With a mean duration of 5.6 (±5.3) years of pelvic pain, the majority of our subjects had underwent two previous surgeries (mean 1.9 ± 1.7) for treatment of pelvic pain; 34% (n = 39) had a previous hysterectomy at entry into the study. Slightly over half of our participants (n = 64; 55.6%) had been diagnosed with at least one other co-morbid pain condition (e.g. fibromyalgia, migraine headache).
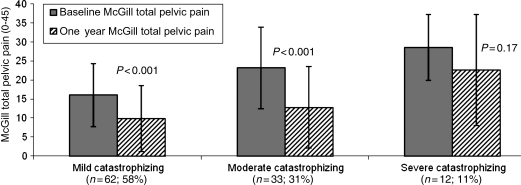
Compared with women in the US population, women in our study were considerably below average (approximate 25th percentile) in their mental health status, with a mean SF-12 score of 42.8 ± 10.3 (Ware et al., 2002). Overall, 43.47% of participants scored moderate to severe on catastrophizing (Fig. 1). Most experienced moderate levels of pain (mean McGill pain score 19.45 ± 10.0), with scores higher than those reported for fibromyalgia (15 ± 6.7) patients (Geisser et al., 2003).
Figure 1.
Differences between baseline and 1-year McGill total pelvic pain within catastrophizing groups (P-values are from paired Student's t-tests between baseline and 1-year McGill total pelvic pain scores within each catastrophizing group).
Most demographic, clinical and psychosocial characteristics did not differ between patients undergoing medical therapy or medical in conjunction with surgical therapy. However, on average, the non-surgical group entered the study having a longer duration of pelvic pain by 2.4 years (P = 0.01), one additional past surgery for pelvic pain (P = 0.05) and a greater likelihood of having a previous hysterectomy (P = 0.008).
Most patients improved in their pain scores from entry to follow-up (74.8%). Patients reported an average of a 37.4% decrease in pain (P < 0.001) during the year. Both surgical and non-surgical patients improved significantly over time (P < 0.001), with a trend for those having surgery to have a greater mean pain improvement (50.3%) compared with those without surgery (31.2%; P = 0.05). The most common medical treatments included hormonal therapies (59.1%) and central nervous system medications (34.8%). The most common surgeries performed over the year included hysterectomy (11.3%), oophorectomy (11.3%) and lysis of adhesions (10.4%). In further analysis, we found that the trend for improved 1-year pain outcomes among those undergoing surgery was attributable to interval hysterectomy. Thus, in later analyses, we focused on hysterectomy rather than all surgeries.
Baseline pain analyses
We first analyzed the demographic, previous medical history and mental health correlates of baseline total pelvic pain. Greater pain at study entry was associated with younger age (P = 0.02), less education (P = 0.01), more previous pelvic surgeries (P = 0.05), past PT treatment (P = 0.03) and coping with pain by catastrophizing (P < 0.001). Specifically, further analysis showed that those 30 years or younger, those having less than a college degree, those having three or more pelvic surgeries and those who cope via severe catastrophizing had the worst pain at baseline. These predictors accounted for ∼35% of the variance in baseline pain scores. Catastrophizing alone in these models explained 21% of the variance in pain scores, with those coping by severe catastrophizing having about a 9-point higher pain score (range 0–45) than those who cope by mild catastrophizing. Since the mental health (SF-12) and catastrophizing measures were highly correlated (r = −0.53; P < 0.001), they could not be in the statistical model simultaneously due to co-linearity. Good mental health (i.e. high SF-12 mental health score) was also associated with less pain at baseline when catastrophizing was not included in the model (β = −0.25; P < 0.001).
Pain at 1 year
Controlling for baseline pain, we examined the demographic, medical history, mental health and interval treatments predicting pelvic pain at 1 year (Table II). Those who had higher pain scores at 1 year after controlling for entry pain were nulliparous (P = 0.002), less likely to have a hysterectomy during the follow-up period (P = 0.008), more likely to receive PT during the follow-up (P = 0.04), slightly more likely to be less educated (P = 0.07) and more likely to cope via catastrophizing at study entry (P = 0.04). Having a hysterectomy explained ∼8% of the variance in pain at 1 year, after controlling for baseline pain. Of the 13 people who had a hysterectomy during follow-up, only one reported follow-up pain above the median pain score for the entire cohort, compared with 59% of those who did not have this surgery.
The predictors of pain at 1 year did not change when we excluded those subjects who entered the study with a previous hysterectomy. Specifically, the standardized parameter estimate and significance (β = −0.287; P = 0.01) for the effect of interim hysterectomy were still notable when those with a prior hysterectomy were excluded from the analyses, compared with the results for the entire cohort shown in Table II.
Catastrophizing was a significant predictor of pain at 1 year, explaining 3% of the variance in pain outcomes. At baseline, however, catastrophizing accounted for 21% of the variance in pain levels. This seemingly unexpected observation is attributable to the inclusion of baseline pain in the 1 year statistical model. Since baseline pain explained a large portion of the variance (41%) in 1 year pain outcomes, not much variance was left to be accounted for by catastrophizing despite its significant association with 1 year pain levels. Changes in pain scores within and between catastrophizing groups (mild, moderate, severe) are shown in Fig. 1. Although all groups tended to decrease in their pain scores, those who exhibited severe catastrophizing at baseline started and ended the study with higher pain levels. Only those with mild (P < 0.001) and moderate (P < 0.001) levels of catastrophizing showed significant pain improvement at 1 year.
Discussion
Our data suggest that biopsychosocial factors, specifically catastrophizing, may play a pivotal role in pain experience among women with endometriosis-associated intractable pain. In our cohort, pain severity at entry and at 1 year was more related to catastrophizing than demographic and conventional clinical variables. This effect is more pronounced when evaluating group differences, with women who demonstrated severe catastrophizing at baseline having a mean pain score 1.5 standard deviation units higher (effect size d) than those demonstrating mild catastrophizing, indicating a large effect size.
The exact mechanism by which catastrophizing influences baseline pain report and its interval improvement—or lack thereof—is not completely understood. Our pilot study suggests that endometriosis-associated pelvic pain may be more complex in some patients in that pre-existing biopsychosocial factors may play a key role in pain-related outcomes.
Within the pain literature, there continues to be a debate over whether catastrophizing is a cause or a result of chronic pain. To date, there are no longitudinal studies that examine whether catastrophizing is modified by a persistent pain state. There is, however, evidence that in both healthy adults and in those with chronic pain, catastrophizing remains stable over weeks and months, and it may not change even after the resolution of acute pain (Keefe et al., 1989; Sullivan et al., 1995; Edwards et al., 2004).
Consistent with findings of other investigators, we found that nulliparity (Bulletti et al., 2010), lower levels of education (Dmowski et al., 1997) and younger age (MacDonald et al., 1999) were associated with higher pain report. Specifically, younger women with lower education were more likely to experience higher pain levels at 1 year following initiation of therapy in our clinics. Nevertheless, the majority of the subjects (74.8%) reported an average of 37.4% reduction in pain at 1 year. Since treatment modalities are guided by clinical judgment and a host of individualized variables, we cannot comment about any specific treatment (surgical versus medical)-related outcomes. However, we can assert that the variables associated with assignment to therapy were consistent with conventional clinical practice. For example, women with previous hysterectomy (P = 0.008), longer duration of pain (likely to be a proxy for previously failed surgical intervention; P = 0.01) and multiple past surgeries for pelvic pain (P = 0.05) were more likely to be managed medically.
We also found that surgical history was related to pain severity and improvement (Leserman et al., 2006). Specifically, women entering the study with three or more past pelvic surgeries had more pain at baseline than those entering with fewer surgeries. This may be due to multiple surgeries being an indicator of intractable pain that does not improve with treatment. Our study additionally confirms the findings of others concerning the beneficial effect of hysterectomy (Carlson et al., 1994; Farquhar et al., 2006), while other types of surgery (e.g. oophorectomy) and medical treatments comparatively were not as effective. In fact, those who had prior PT and/or were referred to PT in the intervening year had more pain at both baseline and follow-up. The association between referral to PT and poorer pain outcomes, which is likely to be a surrogate marker for pelvic floor muscle pain, is consistent with our ‘clinical observation’ in that women with severe pelvic pain often have co-morbid pelvic floor muscle pain and a poor quality of life. This in turn prompts the clinician to make a referral to PT for further evaluation and management.
There are potential limitations that are important in the interpretation of our findings. First, the diagnosis of endometriosis was based on medical records and patient self-report. While all participants had undergone surgical evaluation with subsequent diagnosis of endometriosis-associated intractable pain, we did not have medical record data on histological findings at the time of surgery. Second, due to small sample size, we were unable to investigate the joint and independent contributions of other known psychosocial variables (e.g. histories of trauma and abuse) on interim pain report. Lastly, we were unable to compare the merits of specific treatment modalities in symptom improvement. Treatment allocation was reflective of physicians’ practice pattern and patient preference. Since treatment assignment was based on the doctor patient interaction, it is reasonable to assume the ‘best case scenario’, in that the selected course of therapy had the greatest odds of success in a given patient (Joyce and Piper, 1998; Horne, 1999). Nonetheless, the magnitude of improvement in pain in this study is analogous to that of other chronic pain conditions (Spiegel et al., 2009).
Our data suggest that endometriosis is a complex condition in which the traditional one-dimensional focus on end-organ gynecological factors may not be sufficient in advancing our understanding of the optimal treatment of this condition. In our cohort, psychological factors had a significant influence on pain report. Larger studies are urgently needed to parse out the contributions of the neurobiological and psychosocial domains in the genesis and treatment of persistent pain states in women with endometriosis (Edwards et al., 2006a,b, 2009).Until then, future investigations should take into account the role of psychological factors in pain-related outcomes.
Authors' roles
In the spirit of horizontal collaboration, each author contributed equally to (i) drafting the article or revising it critically for important intellectual content as well as (ii) final approval of the version to be published in addition to (iii) individual contributions to the conception and design, or acquisition of data, or analysis and interpretation of data as follows: C.E.M. was involved in data acquisition, analysis, interpretation of data; E.J. played a role in data acquisition, interpretation, conceptualization/design and analysis; M.E.W. contributed to conceptualization/design, interpretation of data; J.L. took part in analysis, conceptualization/design, acquisition and interpretation of data; D.Z. played a role in conceptualization, data acquisition and interpretation, as well as analysis.
Funding
This research was funded in part by a Summer Undergraduate Research Fellowship and the Department of Obstetrics and Gynecology at the University of North Carolina at Chapel Hill, National Institute of Heath awards K23 HD 053631 and UL1RR025747 from the National Center for Research Resources.
Acknowledgements
The authors thank the Hannah family for their charitable donations which were the seed grant for the inception of the Pelvic Pain Research Unit and its subsequent collaborative work at UNC.
References
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York: Guillford; 1979. [Google Scholar]
- Buer N, Linton SJ. Fear-avoidance beliefs and catastrophizing: occurrence and risk factor in back pain and ADL in the general population. Pain. 2002;99:485–491. doi: 10.1016/S0304-3959(02)00265-8. [DOI] [PubMed] [Google Scholar]
- Bulletti C, Montini A, Setti PL, Palagiano A, Ubaldi F, Borini A. Vaginal parturition decreases recurrence of endometriosis. Fertil Steril. 2010;94:850–855. doi: 10.1016/j.fertnstert.2009.04.012. [DOI] [PubMed] [Google Scholar]
- Carlson KJ, Miller BA, Fowler FJ., Jr The Maine Women's Health Study: II. Outcomes of nonsurgical management of leiomyomas, abnormal bleeding, and chronic pelvic pain. Obstet Gynecol. 1994;83:566–572. doi: 10.1097/00006250-199404000-00013. [DOI] [PubMed] [Google Scholar]
- Dmowski WP, Lesniewicz R, Rana N, Pepping P, Noursalehi M. Changing trends in the diagnosis of endometriosis: a comparative study of women with pelvic endometriosis presenting with chronic pelvic pain or infertility. Fertil Steril. 1997;67:238–243. doi: 10.1016/S0015-0282(97)81904-8. [DOI] [PubMed] [Google Scholar]
- Drossman DA, Leserman J, Li Z, Keefe F, Hu YJ, Toomey TC. Effects of coping on health outcome among women with gastrointestinal disorders. Psychosom Med. 2000;62:309–317. doi: 10.1097/00006842-200005000-00004. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Haythornthwaite JA, Sullivan MJ, Fillingim RB. Catastrophizing as a mediator of sex differences in pain: differential effects for daily pain versus laboratory-induced pain. Pain. 2004;111:335–341. doi: 10.1016/j.pain.2004.07.012. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Goble L, Kwan A, Kudel I, McGuire L, Heinberg L, Wigley F, Haythornthwaite J. Catastrophizing, pain, and social adjustment in scleroderma: relationships with educational level. Clin J Pain. 2006a;22:639–646. doi: 10.1097/01.ajp.0000210918.26159.94. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Smith MT, Stonerock G, Haythornthwaite JA. Pain-related catastrophizing in healthy women is associated with greater temporal summation of and reduced habituation to thermal pain. Clin J Pain. 2006b;22:730–737. doi: 10.1097/01.ajp.0000210914.72794.bc. [DOI] [PubMed] [Google Scholar]
- Edwards RR, Kronfli T, Haythornthwaite JA, Smith MT, McGuire L, Page GG. Association of catastrophizing with interleukin-6 responses to acute pain. Pain. 2008;140:135–144. doi: 10.1016/j.pain.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards RR, Campbell C, Jamison RN, Wiech K. The neurobiological underpinnings of coping with pain. Curr Direct Psychol Sci. 2009;18:237–241. [Google Scholar]
- Evers AW, Kraaimaat FW, Geenen R, Jacobs JW, Bijlsma JW. Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis. Behav Res Ther. 2003;41:1295–1310. doi: 10.1016/s0005-7967(03)00036-6. [DOI] [PubMed] [Google Scholar]
- Farquhar CM, Harvey SA, Yu Y, Sadler L, Stewart AW. A prospective study of 3 years of outcomes after hysterectomy with and without oophorectomy. Am J Obstet Gynecol. 2006;194:711–717. doi: 10.1016/j.ajog.2005.08.066. [DOI] [PubMed] [Google Scholar]
- Geisser ME, Casey KL, Brucksch CB, Ribbens CM, Appleton BB, Crofford LJ. Perception of noxious and innocuous heat stimulation among healthy women and women with fibromyalgia: association with mood, somatic focus, and catastrophizing. Pain. 2003;102:243–250. doi: 10.1016/S0304-3959(02)00417-7. [DOI] [PubMed] [Google Scholar]
- Gracely RH, Geisser ME, Giesecke T, Grant MA, Petzke F, Williams DA, Clauw DJ. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain. 2004;127:835–843. doi: 10.1093/brain/awh098. [DOI] [PubMed] [Google Scholar]
- Grafton KV, Foster N, EWright CC. Test-retest reliability of the short-form McGill pain questionnaire: assessment of intraclass correlation coefficients and limits of agreement in patients with osteoarthritis. Clin J Pain. 2005;21:73–82. doi: 10.1097/00002508-200501000-00009. [DOI] [PubMed] [Google Scholar]
- Granot M, Ferber SG. The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain. 2005;21:439–445. doi: 10.1097/01.ajp.0000135236.12705.2d. [DOI] [PubMed] [Google Scholar]
- Guo SW, Wang Y. The prevalence of endometriosis in women with chronic pelvic pain. Gynecol. Obstet Invest. 2006;62:121–130. doi: 10.1159/000093019. [DOI] [PubMed] [Google Scholar]
- Hanley MA, Raichle K, Jensen M, Cardenas DD. Pain catastrophizing and beliefs predict changes in pain interference and psychological functioning in persons with spinal cord injury. J Pain. 2008;9:863–871. doi: 10.1016/j.jpain.2008.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R. Patients’ beliefs about treatment: the hidden determinant of treatment outcome? J Psychosom Res. 1999;47:491–495. doi: 10.1016/s0022-3999(99)00058-6. [DOI] [PubMed] [Google Scholar]
- Joyce AS, Piper WE. Expectancy, the therapeutic alliance, and treatment outcome in short-term individual psychotherapy. J Psychother Pract Res. 1998;7:236–248. [PMC free article] [PubMed] [Google Scholar]
- Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79:231–252. doi: 10.1016/s0039-6109(05)70381-9. Review. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Brown GK, Wallston KA, Caldwell DS. Coping with rheumatoid arthritis pain: catastrophizing as a maladaptive strategy. Pain. 1989;37:51–56. doi: 10.1016/0304-3959(89)90152-8. [DOI] [PubMed] [Google Scholar]
- Lamvu G. Role of hysterectomy in the treatment of chronic pelvic pain. Obstet Gynecol. 2011;117:1175–1178. doi: 10.1097/AOG.0b013e31821646e1. [DOI] [PubMed] [Google Scholar]
- Leserman J, Zolnoun D, Meltzer-Brody S, Lamvu G, Steege JF. Identification of diagnostic subtypes of chronic pelvic pain and how subtypes differ in health status and trauma history. Am J Obstet Gynecol. 2006;195:554–560. doi: 10.1016/j.ajog.2006.03.071. discussion 560–1. [DOI] [PubMed] [Google Scholar]
- Lloyd D, Findlay G, Roberts N, Nurmikko T. Differences in low back pain behavior are reflected in the cerebral response to tactile stimulation of the lower back. Spine (Phila Pa 1976) 2008;33:1372–1377. doi: 10.1097/BRS.0b013e3181734a8a. [DOI] [PubMed] [Google Scholar]
- MacDonald SR, Klock SC, Milad MP. Long-term outcome of nonconservative surgery (hysterectomy) for endometriosis-associated pain in women <30 years old. Am J Obstet Gynecol. 1999;180:1360–1363. doi: 10.1016/s0002-9378(99)70020-7. [DOI] [PubMed] [Google Scholar]
- Mason ST, Arceneaux LL, Abouhassan W, Lauterbach D, Seebach C, Fauerbach JA. Confirmatory factor analysis of the short form McGill pain questionnaire with burn patients. Eplasty. 2008;8:e54. [PMC free article] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Lu JFR, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): III. tests of data quality, scaling assumptions and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- Meltzer-Brody S, Leserman J, Zolnoun D, Steege J, Green E, Teich A. Trauma and posttraumatic stress disorder in women with chronic pelvic pain. Obstet Gynecol. 2007;109:902–908. doi: 10.1097/01.AOG.0000258296.35538.88. [DOI] [PubMed] [Google Scholar]
- Melzack R. The short-form McGill pain questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- Robinson ME, Riley JL, Myers CD, Sadler IJ, Kvaal SA, Geisser ME, Keefe FJ. The coping strategies questionnaire: a large sample, item level factor analysis. Clin J Pain. 1997;13:43–49. doi: 10.1097/00002508-199703000-00007. [DOI] [PubMed] [Google Scholar]
- Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- Schanberg LE, Keefe FJ, Lefebvre JC, Kredich DW, Gil KM. Pain coping strategies in children with juvenile primary fibromyalgia syndrome: correlation with pain, physical function, and psychological distress. Arthritis Care Res. 1997;9:89–96. doi: 10.1002/1529-0131(199604)9:2<89::aid-anr1790090204>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Seminowicz DA, Davis KD. Cortical responses to pain in healthy individuals depends on pain catastrophizing. Pain. 2006;120:297–306. doi: 10.1016/j.pain.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain. 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. [DOI] [PubMed] [Google Scholar]
- Severeijns R, Vlaeyen JW, van den Hout MA, Picavet HS. Pain catastrophizing is associated with health indices in musculoskeletal pain: a cross-sectional study in the Dutch community. Health Psychol. 2004;23:49–57. doi: 10.1037/0278-6133.23.1.49. [DOI] [PubMed] [Google Scholar]
- Spiegel B, Bolus R, Harris LA, Lucak S, Naliboff B, Esrailian E, Chey WD, Lembo A, Karsan H, Tillisch K, et al. Measuring irritable bowel syndrome patient-reported outcomes with an abdominal pain numeric rating scale. Aliment Pharmacol Ther. 2009;30:1159–1170. doi: 10.1111/j.1365-2036.2009.04144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Lynch ME, Clark AJ. Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain. 2005;113:310–315. doi: 10.1016/j.pain.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Taylor E, Williams C. Surgical treatment of endometriosis: location and patterns of disease at reoperation. Fertil Steril. 2010;93:57–61. doi: 10.1016/j.fertnstert.2008.09.085. [DOI] [PubMed] [Google Scholar]
- Turner JA, Jensen MP, Warms CA, Cardenas DD. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain. 2002;98:127–134. doi: 10.1016/s0304-3959(02)00045-3. [DOI] [PubMed] [Google Scholar]
- Turner JA, Brister H, Huggins K, Mancl L, Aaron LA, Truelove EL. Catastrophizing is associated with clinical examination findings, activity interference, and health care use among patients with temporomandibular disorders. J Orofac Pain. 2005;19:291–300. [PubMed] [Google Scholar]
- Vercellini P, Fedele L, Aimi G, Pietropaolo G, Consonni D, Crosignani PG. Association between endometriosis stage, lesion type, patient characteristics and severity of pelvic pain symptoms: a multivariate analysis of over 1000 patients. Hum Reprod. 2007;22:266–271. doi: 10.1093/humrep/del339. [DOI] [PubMed] [Google Scholar]
- Vincent K, Kennedy S, Stratton P. Pain scoring in endometriosis: entry criteria and outcome measures for clinical trials. Report from the Art and Science of Endometriosis meeting. Fertil Steril. 2010;93:62–67. doi: 10.1016/j.fertnstert.2008.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Turner-Bowker DM, Gandek B. Version 2 of the SF-12 Health Survey, SF-12v2: How to Score Version 2 of the SF-12 Health Survey. Lincoln, RI: QualityMetric Inc.; 2002. [Google Scholar]
- Yin H, Yu M, Cheng H, Zhang F, Gao Y, Lin J, Han B, Zhu L. Beta-endorphin prevents collagen induced arthritis by neuroimmuno-regulation pathway. NeuroEndocrinol Lett. 2005;26:739–744. [PubMed] [Google Scholar]