Abstract
BACKGROUND
Δ9-Tetrahydrocannabinol (THC) is the primary psychoactive constituent of cannabis and an active cannabinoid pharmacotherapy component. No plasma pharmacokinetic data after repeated oral THC administration are available.
METHODS
Six adult male daily cannabis smokers resided on a closed clinical research unit. Oral THC capsules (20 mg) were administered every 4–8 h in escalating total daily doses (40–120 mg) for 7 days. Free and glucuronidated plasma THC, 11-hydroxy-THC (11-OH-THC), and 11-nor-9-carboxy-THC (THC COOH) were quantified by 2-dimensional GC-MS during and after dosing.
RESULTS
Free plasma THC, 11-OH-THC, and THCCOOH concentrations 19.5 h after admission (before controlled oral THC dosing) were mean 4.3 (SE 1.1), 1.3 (0.5), and 34.0 (8.4) μg/L, respectively. During oral dosing, free 11-OH-THC and THCCOOH increased steadily, whereas THC did not. Mean peak plasma free THC, 11-OH-THC, and THCCOOH concentrations were 3.8 (0.5), 3.0 (0.7), and 196.9 (39.9) μg/L, respectively, 22.5 h after the last dose. Escherichia coli β-glucuronidase hydrolysis of 264 cannabinoid specimens yielded statistically significant increases in THC, 11-OH-THC, and THCCOOH concentrations (P < 0.001), but conjugated concentrations were underestimated owing to incomplete enzymatic hydrolysis.
CONCLUSIONS
Plasma THC concentrations remained >1 μg/L for at least 1 day after daily cannabis smoking and also after cessation of multiple oral THC doses. We report for the first time free plasma THC concentrations after multiple high-dose oral THC throughout the day and night, and after Escherichia coli β-glucuronidase hydrolysis. These data will aid in the interpretation of plasma THC concentrations after multiple oral doses.
Δ9-Tetrahydrocannabinol (THC)4 is the primary psychoactive constituent of cannabis, the most commonly abused illicit drug (1). Although predominantly smoked, oral administration occurs during illicit use and licit pharmacotherapy. Oral synthetic THC (dronabinol) is FDA-approved for treating nausea, vomiting, and anorexia, and there is strong interest in treatment with whole plant extracts containing THC and cannabidiol (2). Dronabinol also suppresses cannabis withdrawal and withdrawal-associated drug relapse (3, 4).
Cannabinoids are commonly detected in impaired and fatally injured drivers (5). Smoked cannabis (6, 7) and oral THC (8) markedly affect cognitive and psychomotor skills. Many US and international jurisdictions have instituted per se laws for THC and/or its inactive metabolite 11-nor-9-carboxy-THC (THCCOOH) in drivers’ blood, although detection times after chronic exposure are unknown.
Chronic heavy cannabis use prolongs blood cannabinoid detection intervals. After acute smoked cannabis in occasional users, blood THC was generally below detection limits within 12 h (9). After frequent use, mean whole blood THC was >1 μg/L (n = 5) after 1 week of monitored abstinence (10). Serum THC was ≥1 μg/L up to 120 h after last use in cannabis smokers reporting 1 to >7 cannabis cigarettes/week (11).
Oral THC bioavailability is only 6%–10%, variable, and influenced by vehicle (12) due to gastric degradation and extensive first-pass metabolism (13). THC is rapidly oxidized to its active metabolite (14) 11-hydroxy-THC (11-OH-THC) and further to THC COOH. Peak THC concentrations are lower after oral than smoked administration (15), but conversely, 11-OH-THC/THC ratios are higher after oral than smoked drug (9, 16, 17). Cannabinoids undergo phase II metabolism with glucuronide and sulfate (13). There are few data on cannabinoid conjugate concentrations after smoked cannabis or oral THC. There is a single supplier for THC-glucuronide and no available 11-OH-THC-glucuronide and cannabinoid sulfate standards. Little is known about the proportions of ether and ester glucuronide conjugates in authentic specimens following oral or smoked cannabis. Furthermore, different hydrolysis efficiencies were reported for β-glucuronidase from Helix pomatia and Escherichia coli and after alkaline hydrolysis (18, 19). Finally, the stability of cannabinoid glucuronide and sulfate conjugates in authentic specimens after cannabis use is unknown. Most cannabinoid research requires frozen storage and specimen analysis after study completion. To our knowledge, rapid authentic plasma analysis without frozen storage has not been previously attempted.
Cannabinoid glucuronides have been estimated by subtracting free cannabinoids from concentrations after enzyme or base hydrolysis (20-22). Available data do not differentiate among individual cannabinoid glucuronides (16, 23) or describe only THCCOOH-glucuronide (21, 24). Knowing free and glucuronidated cannabinoid disposition after smoked and oral THC may improve interpretation of plasma cannabinoid concentrations in clinical and forensic investigations.
Of several published human daily oral THC administration studies (25, 26), none report plasma concentrations during continuous dosing. We previously described plasma cannabinoids after oral THC 3 times/day for 5 days (17), but the highest daily dose was 14.8 mg, much lower than single 20-mg doses prescribed for appetite stimulation. Another study determined only 14C-labeled plasma THC concentrations before and after, not during, continuous dosing (27).
In this study, we characterized free and glucuronidated plasma THC, 11-OH-THC, and THC COOH in daily cannabis users after self-administered smoked cannabis, after 20-mg oral THC, during 2–7 daily THC doses for 7 days, and for 22.5 h after last THC dose. Authentic plasma specimens stored at 4 °C were analyzed generally within 2 weeks.
Materials and Methods
PARTICIPANTS
Participants provided written informed consent for this Institutional Review Board–approved protocol. Inclusion criteria for participants were 18–45 years old, smoked cannabis ≥1 years with daily use >3 months, were urine cannabinoid positive, and had normal cardiac function and IQ ≥85. Clinically significant medical or psychiatric disease; illness within the prior 2 weeks; physical dependence other than cannabis, nicotine, or caffeine; cannabis-related psychosis or seizure; ≥6 alcoholic drinks/day ≥4 times/week; sesame oil allergy; or drug treatment interest were exclusionary. Participants were admitted to the secure research unit 20 h before the first THC dose and were discharged 24 h after the last dose.
ORAL THC ADMINISTRATION AND BLOOD COLLECTION
Participants received oral synthetic THC (dronabinol, Marinol®; Unimed Pharmaceuticals) in 20-mg gelatin capsules with increasing frequency (every 4–8 h) for total doses of 40–120 mg/day (see Supplemental Table 1, which accompanies the online version of this article at www.clinchem.org/content/vol55/issue12). The first dose was day 1 (20 h after admission) and the last at 0930 on day 8. This regimen standardized cannabis tolerance across participants while minimizing adverse events documented with 30-mg doses (26). We collected venous blood (7 mL) into lithium heparin Vacutainer tubes on admission and twice before and every 30 min for 4 h after first dose to evaluate single-dose cannabinoid pharmacokinetics. During continuous dosing, we collected blood daily at about 1000, 2000, and 2200. After last dose, collections occurred every 30–180 min (see online Supplemental Table 1). Collection preceded dosing when both were scheduled at the same time. Blood was centrifuged and plasma separated within 2 h. Plasma was stored at 4 °C (with 1 exception) and analyzed as soon as possible. We assayed free cannabinoids within 10 (5) days and conjugated cannabinoids within 15 (10) days of collection. Participant A’s plasma was stored at −20 °C for approximately 10 weeks owing to laboratory relocation.
CANNABINOID ANALYSIS
We measured free cannabinoids using our previously reported method (28). Briefly, we mixed 1 mL 0.1 mol/L phosphate buffer (pH 6.8), deuterated internal standards, and 1 mL plasma. Proteins were precipitated with 2 mL cold acetonitrile and centrifuged. Solid-phase extraction (ZSTHC020; United Chemical Technologies) was followed by derivatization with 25 μL N,O-bis(trimethylsilyl)trifluoroacetamide and 1% trimethylchlorosilane at 70 °C for 40 min, and 3 μL was injected splitless onto a 2-dimensional (2D) Agilent 6890 GC-MS (GC-FID/5973 MSD) with a Dean’s switch (Agilent Technologies) and cryotrap (Joint Analytical Systems).
We estimated glucuronidated cannabinoids by subtracting free cannabinoids from cannabinoids after E. coli β-glucuronidase hydrolysis. For hydrolysis of cannabinoid glucuronide conjugates, we incubated 1 mL plasma, 1 mL 0.1 mol/L phosphate buffer (pH 6.8), and 5000 U E. coli β-glucuronidase at 37 °C for 16 h. Split calibration curves provided quantification of 0.25–100 μg/L THC and THCCOOH and 0.5–75 μg/L 11-OH-THC. Intra- and interassay imprecision were <11% and <14%, respectively, and analytical recoveries were 86%–113% (28).
EVALUATION OF E. coli β-GLUCURONIDASE HYDROLYSIS
We evaluated cannabinoid hydrolysis in plasma to determine E. coli β-glucuronidase hydrolysis efficiency, glucuronide hydrolysis during derivatization after coextraction of free and glucuronidated cannabinoids, potential sulfate conjugation, and tandem hydrolysis efficiency (see online Supplemental Data). THC-glucuronide was first synthesized by El-Sohly Laboratories (29) and is commercially available on request. We purchased THCCOOH-glucuronide from Cerilliant. Hydrolysis of 11-OH-THC-glucuronide could not be evaluated, as reference standard is not commercially available. For all experiments, glucuronides were hydrolyzed, derivatized, and analyzed according to the procedures described in Materials and Methods.
CALCULATIONS AND STATISTICAL ANALYSIS
Body mass index (BMI) was calculated as weight (kg)/height (m)2 and percentage free and glucuronidated cannabinoids as (free/hydrolyzed) × 100 and (hydrolyzed – free/hydrolyzed) × 100, respectively. Percentage free THC increase from baseline (before first 20-mg dose) to maximum concentration (Cmax) was calculated as [(Cmax – baseline)/baseline] × 100; percentage THC decrease from admission to predosing baseline as [(admission – baseline)/admission] × 100; and percentage hydrolysis increase as [(hydrolyzed – free)/free] × 100. Using paired t-tests, we compared within-subject free and glucuronidated cannabinoids (n = 264 specimens), percentage free self-administered cannabinoids (n = 18 specimens) and after steady-state oral THC (n = 18, day 7 specimens), and 11-OH-THC/THC and THCCOOH/THC ratios after cannabis self-administration (n = 18) and during steady-state administration (n = 18, day 7 specimens). Association between oral dosing day and mean concentration was obtained by least-squares linear regression analysis. A 2-tailed α = 0.05 was used for all comparisons. Statistical calculations used SPSS 13.0 for Windows.
Results
GLUCURONIDE HYDROLYSIS EVALUATION
We verified THC- and THCCOOH-glucuronide calibrator concentrations and activity of the E. coli β-glucuronidase by fortifying 5 replicates each of pH 6.8 phosphate buffer and blank urine and plasma to 75 μg/L and determining recovery after our standard analysis procedure. Mean THC yields after hydrolysis in buffer, urine, and plasma were 108.7% (1.7%), 90.4% (1.9%), and 21.3% (0.1%), respectively. THCCOOH yields were 50.1% (0.5%) in buffer, 47.9% (0.3%) in urine, and 37.3% (0.2%) in plasma. Evaluation of plasma cannabinoid glucuronide hydrolysis in 5 different plasma pools yielded mean (SD) (median, range) yields of 17.9% (1.5%) (17.3%, 15.8%–21.2%) and 43.9% (4.4%) (43.6%, 38.3%–49.6%) for THC- and THCCOOH-glucuronides, respectively. Intraplasma pool imprecisions (%CV) were 0.9%–6.2% and 0.4%–2% and interplasma pool imprecisions 8.6% and 10.1%, respectively.
Spontaneous and/or extraction-induced THC-glucuronide conversion to free THC was not measurable up to 75 μg/L and only 0.2% at 200 μg/L. Conversion to free THCCOOH was less than the limit of quantification (LOQ) up to 20 μg/L and <0.8% up to 200 μg/L in nonhydrolyzed plasma samples. Urine containing 75 μg/L THC-glucuronide yielded no measurable THC in nonhydrolyzed samples, but the same concentration in buffer produced 1.6% free THC. Up to 2.2% THCCOOH was produced from 75 μg/L THCCOOH-glucuronide in buffer.
We also evaluated the potential for hydrolysis of glucuronidated THC and THCCOOH up to 200 μg/L during derivatization and found conversion rates of 2.8% and 25%, respectively, in neat glucuronide samples simply evaporated and derivatized. As described above, however, processing samples fortified only with THC- and THCCOOH-glucuronides by our method, but without enzymatic hydrolysis, yielded low free drug concentrations.
We attempted to improve the recovery of cannabinoids by hydrolyzing samples with Glusulase®, which potentially could free both glucuronide and sulfate conjugates; the results were not statistically different from those with E. coli β-glucuronidase (data not shown). These data suggested little or no sulfate conjugation, although 11-OH-THC could not be measured owing to poor chromatography. In addition, we attempted to hydrolyze plasma with our published tandem enzymatic and alkaline hydrolysis procedure for freeing urine cannabinoid conjugates (19), but the chromatography was too poor to accurately quantify analytes of interest. Furthermore, THC and 11-OH-THC could not be measured after alkaline hydrolysis alone, although THCCOOH concentrations were approximately twice as high as after β-glucuronidase or Glusulase hydrolysis. Only the E. coli β-glucuronidase hydrolysis yielded acceptable chromatography at the method’s LOQ for THC and 11-OH-THC.
PLASMA CANNABINOID DISPOSITION AFTER MULTIPLE ORAL THC DOSES
Participant demographics and drug use characteristics are reported in Table 1. One individual was underweight (BMI <18.5), 3 were at normal weight (BMI 18.5–24.9), and 2 were overweight (BMI 25–29.9).
Table 1.
Demographic and self-reported drug use characteristics of 6 adult cannabis smokers at the time of study qualification.
| Participant | Mean | SE | Median | ||||||
|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | F | ||||
| Age, years | 20 | 32 | 26 | 18 | 23 | 21 | 23.9 | 2.1 | 22.5 |
| BMI, kg/m2 | 17.8 | 29.8 | 25.1 | 23.7 | 21.1 | 22.9 | 23.4 | 1.6 | 23.3 |
| Cannabis joints smoked per day | 6 | 3 | 24 | 3 | 6 | 1 | 7.2 | 3.5 | 4.5 |
| No. days used cannabis in past 14 | 13 | 13 | 14 | 12 | 14 | 14 | 13.3 | 0.3 | 13.5 |
| Days since last cannabis use | 1 | 1 | 1 | 0 | 1 | 1 | 0.8 | 0.2 | 1 |
| Lifetime cannabis use, years | 4 | 18 | 13 | 4 | 10 | 4 | 9.4 | 2.4 | 7.5 |
| Age at first cannabis use, years | 16 | 14 | 13 | 14 | 13 | 17 | 14.5 | 0.7 | 14 |
| No. alcoholic drinks per occasion | 2 | 2 | 4 | 1.5 | 6 | 10 | 4.3 | 1.3 | 4 |
| No. alcohol drinking occasions per week | 0.5 | 0.08 | 1 | 0.25 | 2 | 3 | 1.1 | 0.5 | 1 |
| No. tobacco smoking occasions per week | 70 | 3 | 76 | 10.5 | 0 | 21 | 30.1 | 13.9 | 21 |
| Other drugs | |||||||||
| Substance | NAa | NA | A | O | O | O,C,T,H | |||
| Frequency | NA | NA | Once past 3 months | Once past 3 months | 1.5 years ago | Each once in past 2 years | |||
NA, none admitted; A, amphetamines; O, opiates; C, cocaine; T, tranquilizers; H, hallucinogens.
The mean (SE) (range) free plasma concentrations (n = 6) on admission for THC, 11-OH-THC, and THCCOOH were 9.6 (4.8) (2.4–33.3), 3.6 (1.7) (1.3–11.7), and 59.2 (16.7) (24.8–136.6) μg/L, respectively, representing cannabis self-administered before admission (Fig. 1). After 19.5 h, THC, 11-OH-THC, and THCCOOH concentrations were 4.3 (1.1) (1.9–9.6), 1.3 (0.5) (0.7–3.7), and 34.0 (8.4) (13.3–73.2) μg/L, respectively, decreasing by 37.0% (8.8%), 54.8% (6.4%), and 39.0% (6.2%) since admission.
Fig. 1. Free plasma THC, 11-OH-THC, and THCCOOH concentrations in 6 daily cannabis users before and after first 20-mg oral THC dose (day 1) (panel A) and up to 22.5 h after 7 days of continuous oral dosing (days 8 and 9) (panel B).
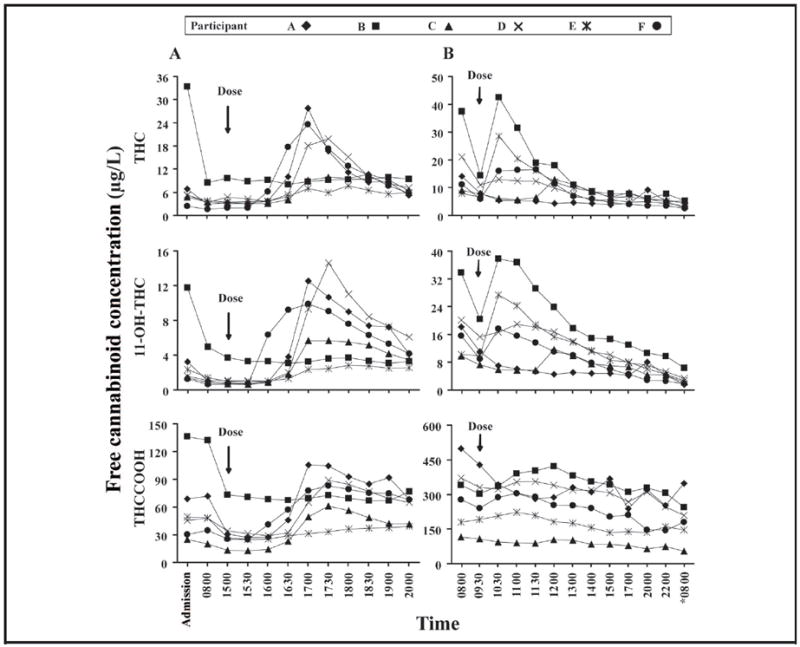
Blood was collected on admission, 12.5 and 19.5 h later, and multiple times after first and last dose. *, day 9.
After the first dose (Fig. 1), mean (SE) free Cmax and time to maximum concentration (Tmax) (n = 6) were 16.5 (3.4) μg/L at 2.8 (0.33) h for THC, 8.2 (2.0) μg/L at 2.5 (0.18) h for 11-OH-THC, and 75.8 (9.4) μg/L at 3.3 (0.56) h for THCCOOH. The mean (SE) (range) free THC, 11-OH-THC, and THCCOOH (n = 6) increases from baseline to Cmax were 421.6% (174.2%) (2.5%–1227.2%), 825.4% (254.6%) (0%– 1443.2%), and 172.8% (53.6%) (4.7%–357.8%), respectively. Mean (SE) Cmax and Tmax during continuous dosing were 47.7 (8.1) μg/L on day 5 [98.1 (9.6) h after first dose] for free THC, 23.9 (3.1) μg/L on day 7 [142.8 (12.7) h after first dose] for free 11-OH-THC, and 327.2 (53.1) μg/L on day 9 [153.1 (9.9) h after first dose] for free THCCOOH. Table 2 provides mean (SE) plasma cannabinoid concentrations during continuous dosing. Fig. 2 represents mean free cannabinoid concentrations at 2200 or 2230 on days 1–7 with dosing 2 h before specimen collection. Significant positive linear correlations between day of continuous dosing and concentrations were observed for 11-OH-THC (P = 0.007) and THCCOOH (P < 0.001), but not THC (P = 0.46). Free 11-OH-THC/THC and THCCOOH/THC ratios (Fig. 3) significantly increased (P < 0.001) during 7 days of continuous dosing (n = 18). After last dose, mean peak free plasma THC [18.5 (5.9), range 5.3– 42.4 μg/L] and 11-OH-THC [18.7 (5.0), range 5.8–37.8 μg/L] concentrations occurred within 1 h; mean peak free THCCOOH [277.9 (44.1), range 90.4–390.8 μg/L] concentration was 0.5 h later, gradually decreasing over time. Mean (SE) (range) free THC, 11-OH-THC, and THCCOOH concentrations 22.5 h after last dose were 3.8 (0.5) (2.4–5.2), 3.0 (0.7) (1.6–6.3), and 196.9 (39.9) (55.0–347.3) μg/L, respectively (Fig. 1).
Table 2.
Free and hydrolyzed plasma THC, 11-OH-THC, and THCCOOH concentrations (μg/L) from the second dose (day 1, 2000) to 2.5 h after last dose (day 8), during oral THC dosing.
| Specimen collection | No. doses before blood collection | Hours since last dose before blood collection | Free THC, μg/L | Hydrolyzed THC, μg/L | Free 11-OH-THC, μg/L | Hydrolyzed 11-OH-THC, μg/L | Free THCCOOH, μg/L | Hydrolyzed THCCOOH, μg/L | |
|---|---|---|---|---|---|---|---|---|---|
| Day | Time | ||||||||
| 1 | 2000 | 1 | 5 | 6.6 (0.6) | 6.7 (0.5) | 3.9 (0.5) | 9.7 (1.3) | 59.7 (6.3) | 194.3 (33.2) |
| 1 | 2200 | 2 | 2 | 14.4 (7.7) | 14.8 (7.9) | 5.5 (2.0) | 14.5 (4.1) | 63.1 (8.1) | 185.2 (34.3) |
| 2 | 0800 | 3 | 6 | 10.2 (2.6) | 11.4 (2.8) | 5.9 (0.6) | 21.1 (3.3) | 109.0 (11.3) | 330.2 (72.6) |
| 2 | 2000 | 5 | 6 | 8.0 (0.9) | 8.4 (0.8) | 6.4 (0.4) | 17.6 (3.1) | 109.5 (14.3) | 305.3 (46.5) |
| 2 | 2200 | 6 | 2 | 16.4 (4.7) | 17.1 (4.9) | 9.2 (2.2) | 26.0 (5.7) | 131.0 (31.0) | 341.2 (71.5) |
| 3 | 1000 | 8 | 4 | 8.7 (1.0) | 9.8 (1.0) | 8.5 (1.0) | 25.8 (4.5) | 156.2 (19.8) | 410.0 (68.2) |
| 3 | 2000 | 10 | 5 | 9.4 (2.7) | 10.0 (3.0) | 7.0 (1.1) | 18.3 (3.6) | 130.0 (19.5) | 366.6 (64.6) |
| 3 | 2200 | 11 | 2 | 23.7 (6.6) | 24.3 (6.5) | 12.1 (2.8) | 32.8 (9.6) | 161.8 (21.9) | 383.2 (81.4) |
| 4 | 1000 | 13 | 4 | 14.7 (4.0) | 16.2 (4.3) | 11.7 (1.8) | 42.8 (9.5) | 204.1 (38.6) | 493.7 (112.2) |
| 4 | 2000 | 15 | 5 | 11.7 (3.3) | 12.1 (3.5) | 9.0 (1.7) | 24.7 (3.5) | 168.2 (36.3) | 423.8 (98.1) |
| 4 | 2200 | 16 | 2 | 16.1 (2.2) | 17.3 (2.6) | 9.3 (1.5) | 30.8 (6.3) | 155.1 (29.9) | 381.7 (78.4) |
| 5 | 1000 | 18 | 4 | 7.9 (0.8) | 8.8 (0.7) | 8.2 (0.9) | 31.0 (7.7) | 200.0 (27.1) | 507.3 (99.0) |
| 5 | 2030 | 21 | 3.5 | 17.7 (4.0) | 18.8 (3.9) | 13.1 (2.4) | 41.0 (9.3) | 201.7 (41.4) | 495.7 (116.3) |
| 5 | 2230 | 22 | 2 | 42.9 (10.6) | 44.9 (11.4) | 20.3 (3.8) | 71.8 (19.7) | 227.8 (28.4) | 543.5 (102.3) |
| 6 | 1000 | 24 | 4 | 9.7 (2.4) | 10.9 (2.2) | 12.0 (2.9) | 47.4 (15.8) | 243.8 (36.1) | 581.8 (88.1) |
| 6 | 2030 | 27 | 3.5 | 15.5 (3.1) | 16.1 (3.0) | 12.3 (1.2) | 40.7 (9.3) | 211.2 (29.2) | 491.6 (81.5) |
| 6 | 2230 | 28 | 2 | 17.2 (4.2) | 18.8 (4.0) | 13.9 (3.2) | 50.9 (17.5) | 226.7 (46.1) | 511.7 (107.9) |
| 7 | 1000 | 30 | 4 | 8.2 (1.4) | 9.1 (1.3) | 11.1 (2.2) | 38.9 (12.9) | 253.6 (39.9) | 619.6 (110.9) |
| 7 | 2030 | 33 | 3.5 | 29.3 (7.4) | 31.4 (8.0) | 17.1 (3.0) | 53.7 (10.4) | 237.9 (35.3) | 566.3 (83.9) |
| 7 | 2230 | 34 | 2 | 16.6 (2.5) | 17.7 (2.9) | 13.4 (1.5) | 45.0 (6.5) | 227.8 (43.3) | 563.7 (91.6) |
| 8 | 0800 | 36 | 2 | 16.7 (4.6) | 17.5 (4.0) | 18.0 (3.6) | 74.0 (21.6) | 296.9 (56.2) | 619.4 (114.7) |
| 8 | 0930 | 36 | 3.5 | 8.8 (1.3) | 9.7 (1.2) | 12.2 (2.0) | 48.1 (15.8) | 267.0 (45.6) | 621.0 (116.4) |
| 8 | 1030 | 37 | 1 | 18.5 (5.9) | 20.4 (6.2) | 18.7 (5.0) | 59.5 (18.4) | 264.6 (39.9) | 594.2 (117.1) |
| 8 | 1100 | 37 | 1.5 | 15.2 (4.0) | 16.7 (4.3) | 17.9 (4.8) | 66.6 (24.5) | 277.9 (44.1) | 599.9 (115.7) |
| 8 | 1130 | 37 | 2 | 12.5 (2.3) | 13.5 (2.4) | 15.1 (3.7) | 57.6 (21.1) | 271.1 (45.5) | 618.8 (136.4) |
| 8 | 1200 | 37 | 2.5 | 11.3 (1.8) | 12.4 (1.8) | 13.9 (2.6) | 50.2 (17.6) | 264.9 (46.2) | 634.5 (150.2) |
Data are mean (SE). Oral THC (20-mg dronabinol) was administered to 6 daily cannabis users throughout the day and night for 7 days.
Fig. 2. Mean (SE) free plasma THC (■), 11-OH-THC (▲), and THCCOOH (●) accumulation during continuous oral THC.
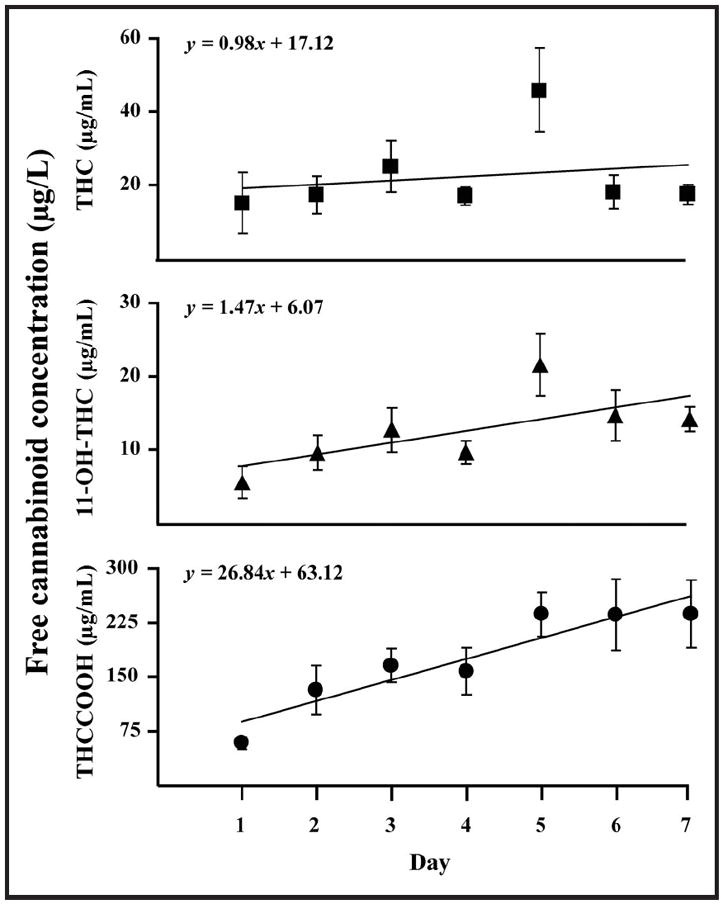
Dronabinol (20 mg) was administered to 6 daily cannabis users continuously for 7 days. Data points (n = 6) represent only blood collected at 2200 or 2230 from the second dose (day 1, 2000) to the 34th dose (day 7, 2030).
Fig. 3.
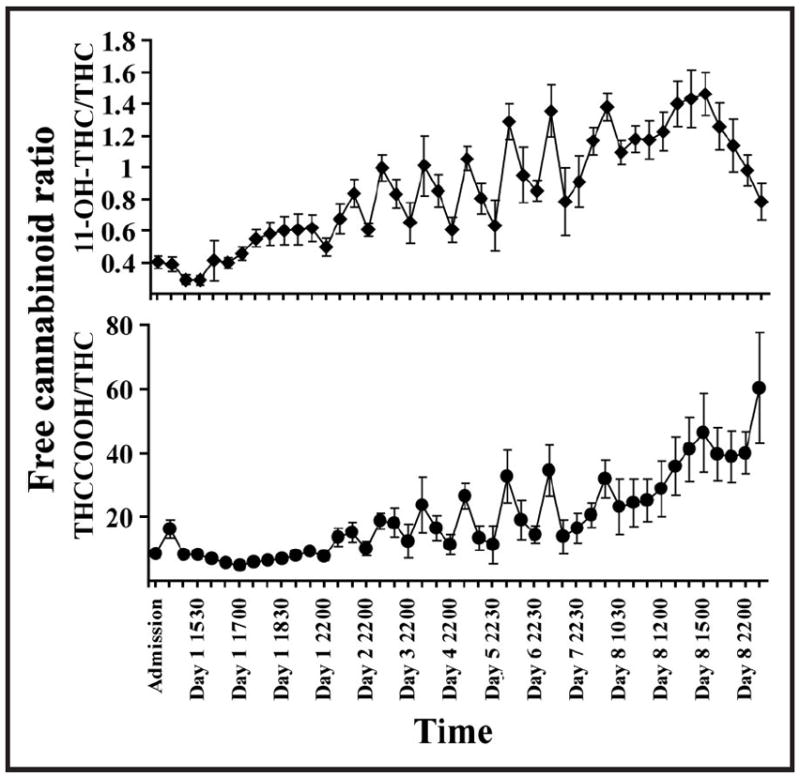
Mean (SE) free 11-OH-THC/THC and THCCOOH/THC ratios in 6 daily cannabis users before and after first 20-mg oral THC dose (day 1, 1500), during 7 days of continuous oral dosing, and up to 22.5 h after last oral dose (day 8, 0930).
Significant increases over free concentrations occurred after hydrolysis with β-glucuronidase: 9.5% (14.1%) for THC (n = 264, P < 0.001), 198.8% (135.2%) for 11-OH-THC (n = 264, P < 0.001), and 166.8% (80.1%) for THCCOOH (n = 264, P < 0.001). Fig. 4 shows mean % free cannabinoids (n = 6). After 7 days of continuous dosing, mean % free 11-OH-THC was significantly lower (P < 0.001) and mean % free THCCOOH was significantly higher (P < 0.001) than after smoked cannabis. A nonsignificant decreasing trend was observed in % free THC (P = 0.08).
Fig. 4. Mean (SE) % free THC (■), 11-OH-THC (▲), and THCCOOH (●) in 6 daily cannabis users before and after first 20-mg oral THC dose (day 1, 1500), during 7 days of continuous oral dosing, and up to 22.5 h after last oral dose (day 8, 0930).
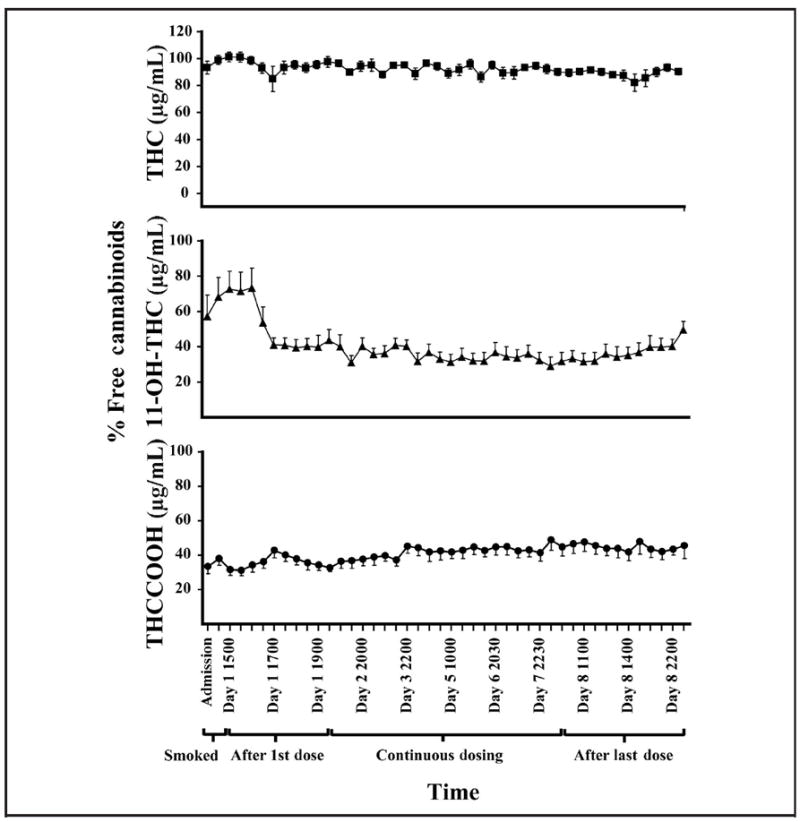
Percentage free cannabinoids were calculated as (free/hydrolyzed) × 100.
Discussion
In this study, we characterized for the first time free THC, 11-OH-THC, and THCCOOH and their glucuronides in plasma during and after frequent oral THC administration. Our data indicate that total cannabinoid concentrations are not currently measurable due to the lack of cannabinoid sulfate and 11-OH-THC glucuronide standards. Total concentrations cannot be estimated by GC-MS analysis because enzymatic and/or alkaline hydrolysis fails to fully cleave cannabinoid conjugates and/or produces poor chromatography for accurate cannabinoid measurement. A third problem is that stability of THC-, 11-OH-THC-, and THCCOOH-glucuronides and sulfates at refrigerated and frozen storage temperatures has not been adequately characterized in authentic plasma specimens. Thus, limitations of current research methods are underestimation of cannabinoid glucuronide conjugates owing to incomplete hydrolysis by E. coli β-glucuronidase and instability when stored at 4 °C for approximately 2 weeks.
Despite these limitations, these unique data characterize cannabinoid disposition after multiple oral THC doses, demonstrate differences in free cannabinoid concentrations after cannabis smoking and oral THC, and document differences in E. coli β-glucuronidase hydrolysis efficiency in 3 different matrices, i.e., buffer, urine, and plasma. Furthermore, for the first time cannabinoid concentrations were quantified in authentic plasma specimens collected after controlled oral THC administration and analyzed after only refrigerated storage for about 2 weeks, to minimize conjugate instability.
Cannabinoid concentrations before first dose reflected self-administered smoked cannabis, providing a valuable comparison to those after frequent oral THC. Mean (SE) plasma free THC after 19.5 h monitored abstinence was 4.3 (1.1) μ/L. Prolonged THC excretion in frequent cannabis users (10, 11) suggests that low free or hydrolyzed plasma THC concentrations, such as 1–2 μg/L (per se THC concentrations), may not reflect recent cannabis exposure. Prolonged daily cannabis use may extend detection times due to THC tissue accumulation and slow release into blood. After 1 33.8-mg THC cigarette, the highest THC concentration 12 h later was 0.7 μg/L (9), considerably less than the 1.9–9.6 μg/L free THC concentrations observed 19.5 h after admission and the >2 μg/L concentration observed 22.5 h after 7 days of continuous dosing in 6 heavy cannabis users in this study.
Pharmacokinetics after first dose were similar to peak plasma free THC concentrations (4.4–11.0 μg/L) reported within 90 min (15), although we found Tmax values of 4 and 5 h in 2 subjects. In another study, after 20-mg oral dronabinol (16), mean (SE) plasma free THC was 0.8 (0.4) μg/L at 45 min, peaking at 7.9 (3.6) μg/L at 135 min. A second peak [9.3 (3.5) μg/L] occurred at 6 h; THC was detected above 1 μg/L for 24 h. Free 11-OH-THC and THC concentrations were equivalent at these times, whereas THCCOOH steadily increased from 6 (4) μg/L at 45 min to 65 (16) μg/L at 165 min, returning to 21 (8) μg/L at 24 h. Subtracting mean baseline free THC of 4.1 μg/L from mean Cmax [16.5 (3.4) μg/L] reported here yielded 12.4 μg/L, similar to Cmax noted after a single dose.
Concentrations during continuous dosing were variable due to erratic absorption, enterohepatic recirculation, and differential timing of specimen collection after dosing, and generally were higher than after a single dose (15, 16). 11-OH-THC and THCCOOH increased over time, indicating accumulation, whereas THC did not. Lack of accumulation of THC could be explained by induced gastrointestinal (GI) metabolism. Frytak et al. (30) found only THCCOOH accumulation after 3 15-mg oral THC doses within 10 h. Frequent cannabis smoking was reported to induce THC metabolism (31); however, this was not replicated (32, 33). If hepatic metabolism could be induced, it likely would have occurred during chronic cannabis smoking, before study entry.
Our data also suggest that THC distribution and elimination are approximately equal to GI absorption during chronic dosing. 11-OH-THC and THCCOOH accumulation may be explained by more rapid THC oxidation than metabolite excretion. Plasma 11-OH-THC elimination half-life in 3 infrequent cannabis users was 19–24 h (14); THCCOOH elimination half-lives were 5.2 (0.08) and 6.2 (6.7) days in frequent and infrequent users, respectively (21). After 5-mg intravenous THCCOOH to 10 non–cannabis users, terminal serum THCCOOH elimination half-life was 17.6 (5.5) h; however, monitoring was for only 4 days, potentially underestimating this parameter (34). Considering our continuous THC dosing and long plasma metabolite excretion half-lives, 11-OH-THC and THCCOOH accumulation was expected. Mean 11-OH-THC/THC and THCCOOH/THC ratios on day 7 were significantly higher than after self-administered cannabis (P < 0.001), consistent with constant plasma THC with increasing metabolite concentrations (Fig. 3).
E. coli β-glucuronidase hydrolysis yielded significant (P < 0.001) increases for all cannabinoid analytes, despite incomplete hydrolysis efficiencies. We previously reported nonsignificant THC increases [18% (17%), n = 4] and significant 11-OH-THC [40% (25%), n = 7] and THCCOOH [42% (12%), n = 9] increases after low-dose (4.9 mg) oral THC administration and E. coli β-glucuronidase hydrolysis (22). THC increases after hydrolysis in this study were similar (approximately 10%), but n = 264 specimens yielded improved statistical power and significance. 11-OH-THC and THCCOOH increases were much higher, 200% and 170%, respectively, possibly owing to higher doses and/or increased metabolic capability in frequent users.
Mean percentage THC-glucuronide was low on admission and before first oral dose after chronic cannabis smoking, but increased over 1 week of oral THC dosing, possibly owing to increased conjugation in the gut and facilitated transport into portal circulation (Fig. 4). Glucuronidation occurs predominantly in the liver (35); however, uridine diphosphate-glucuronosyltransferase was found in human colon (36) and jejunum (37). Although GI conjugation may be possible, to our knowledge, facilitated THC-glucuronide transport has not been reported.
Mean 11-OH-THC-glucuronide increased from approximately 30% after self-administered smoked use to approximately 60% 2 h after first oral dose, remained increased during continuous oral dosing, and decreased to pre-oral THC dosing concentrations 22.5 h after last dose (Fig. 4). There was a significant decrease in % free 11-OH-THC during continuous oral dosing as compared to self-administered smoked cannabis (P < 0.001). Greater amounts of glucuronidated 11-OH-THC may be formed in liver when THC is subject to first-pass metabolism after oral administration.
Mean % THCCOOH-glucuronide exceeded mean % free THCCOOH throughout, but a significant difference (P < 0.001) was noted between % free THCCOOH after 7 days of oral THC and after self-administered smoked cannabis (Fig. 4). This could indicate glucuronidation saturation, yielding higher free THCCOOH concentrations. E. coli β-glucuronidase inefficiently cleaves ester-glucuronides, although free drug increases occur after cleavage of ether-glucuronide linkages. Approximately 50% yield was achieved in buffer, urine, and plasma, suggesting that plasma matrix components do not inhibit THCCOOH-glucuronide hydrolysis.
Specimens were analyzed twice to obtain free and glucuronidated cannabinoid concentrations, after only refrigeration (except subject A’s specimens). Fortified plasma THCCOOH-glucuronide decreased <20% after 10 days storage at 4 °C, with corresponding increases in THCCOOH (38, 39). It is unknown whether similar instability would occur in authentic specimens and whether THC or 11-OH-THC-glucuronides would demonstrate similar stability. The etherglucuronide bonds in THC and 11-OH-THC are believed to be more stable than the ester-glucuronide bond in THCCOOH.
These data improve our knowledge of chronic oral THC plasma pharmacokinetics and will aid interpretation of plasma cannabinoid concentrations after THC pharmacotherapy and in clinical and forensic investigations. Low plasma THC concentrations do not necessarily reflect recent cannabis exposure in daily cannabis users, as indicated by low plasma free THC concentrations 19.5 h after admission and 22.5 h after last oral dose. Positive correlations between time and concentration during frequent oral THC administration indicate 11-OH-THC and THCCOOH, but not THC, accumulation in plasma. Clinicians and investigators may now rely on multiple instead of single-dose pharmacokinetic data for interpretation of plasma concentrations during and after repeated oral THC administration.
Supplementary Material
Acknowledgments
We acknowledge Allan Barnes, Tsadik Abraham, Karl Scheidweiler, and Teresa Gray for technical assistance in manuscript preparation and the National Institute on Drug Abuse (NIDA), Intramural Research Program, and Maryland Psychiatric Research Center clinical research teams for clinical support.
Employment or Leadership: R.H. Lowe, National Institute on Drug Abuse, Intramural Research Program.
Consultant or Advisory Role: None declared.
Stock Ownership: None declared.
Honoraria: None declared.
Research Funding: Intramural Research Program, NIH, NIDA, and NIDA Residential Research Support Services Contract (HHSN271200599091CADB contract no. N01Da-5-9909). R.H. Lowe, National Institute on Drug Abuse, Intramural Research Program.
Expert Testimony: None declared.
Role of Sponsor: The funding organizations played a direct role in the design of study.
Footnotes
Author Contributions: All authors confirmed they have contributed to the intellectual content of this paper and have met the following 3 requirements: (a) significant contributions to the conception and design, acquisition of data, or analysis and interpretation of data; (b) drafting or revising the article for intellectual content; and (c) final approval of the published article.
Nonstandard abbreviations: THC, Δ9-tetrahydrocannabinol; THCCOOH, 11-nor-9-carboxy-THC; 11-OH-THC, 11-hydroxy-THC; 2D, 2-dimensional; BMI, body mass index; Cmax, maximum concentration; LOQ, limit of quantification; Tmax, time to maximum concentration; GI, gastrointestinal.
Authors’ Disclosures of Potential Conflicts of Interest: Upon manuscript submission, all authors completed the Disclosures of Potential Conflict of Interest form. Potential conflicts of interest:
References
- 1.Hall W, Degenhardt L. Prevalence and correlates of cannabis use in developed and developing countries. Curr Opin Psychiatry. 2007;20:393–7. doi: 10.1097/YCO.0b013e32812144cc. [DOI] [PubMed] [Google Scholar]
- 2.Ashton JC, Milligan ED. Cannabinoids for the treatment of neuropathic pain: clinical evidence. Curr Opin Invest Drugs. 2008;9:65–75. [PubMed] [Google Scholar]
- 3.Haney M, Hart CL, Vosburg SK, Comer SD, Reed SC, Foltin RW. Effects of THC and lofexidine in a human laboratory model of marijuana withdrawal and relapse. Psychopharmacology (Berl) 2008;197:157–68. doi: 10.1007/s00213-007-1020-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Levin FR, Kleber HD. Use of dronabinol for cannabis dependence: two case reports and review. Am J Addict. 2008;17:161–4. doi: 10.1080/10550490701861177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walsh JM, de Gier JJ, Christopherson AS, Verstraete AG. Drugs and driving. Traffic Inj Prev. 2004;5:241–53. doi: 10.1080/15389580490465292. [DOI] [PubMed] [Google Scholar]
- 6.Ramaekers JG, Moeller MR, van Ruitenbeek P, Theunissen EL, Schneider E, Kauert G. Cognition and motor control as a function of delta9-THC concentration in serum and oral fluid: limits of impairment. Drug Alcohol Depend. 2006;85:114–22. doi: 10.1016/j.drugalcdep.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Drummer OH, Gerostamoulos J, Batziris H, Chu M, Caplehorn J, Robertson MD, Swann P. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36:239–48. doi: 10.1016/s0001-4575(02)00153-7. [DOI] [PubMed] [Google Scholar]
- 8.Menetrey A, Augsburger M, Favrat B, Pin MA, Rothuizen LE, Appenzeller M, et al. Assessment of driving capability through the use of clinical and psychomotor tests in relation to blood cannabinoids levels following oral administration of 20 mg dronabinol or of a cannabis decoction made with 20 or 60 mg delta9-THC. J Anal Toxicol. 2005;29:327–38. doi: 10.1093/jat/29.5.327. [DOI] [PubMed] [Google Scholar]
- 9.Huestis MA, Henningfield JE, Cone EJ. Blood cannabinoids. I. Absorption of THC and formation of 11-OH-THC and THCCOOH during and after smoking marijuana. J Anal Toxicol. 1992;16:276–82. doi: 10.1093/jat/16.5.276. [DOI] [PubMed] [Google Scholar]
- 10.Karschner EL, Schwilke EW, Lowe RH, Darwin WD, Pope HG, Jr, Herning R, et al. Do Δ9-tetrahydrocannabinol concentrations indicate recent use in chronic cannabis users? Addiction. doi: 10.1111/j.1360-0443.2009.02705.x. Epub ahead of print 2009 Oct 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skopp G, Potsch L. Cannabinoid concentrations in spot serum samples 24–48 hours after discontinuation of cannabis smoking. J Anal Toxicol. 2008;32:160–4. doi: 10.1093/jat/32.2.160. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Reyes M, Lipton MA, Timmons MC, Wall ME, Brine DR, Davis KH. Pharmacology of orally administered delta-9-tetrahydrocannabinol. Clin Pharmacol Ther. 1973;14:48–55. doi: 10.1002/cpt197314148. [DOI] [PubMed] [Google Scholar]
- 13.Huestis MA. Human cannabinoid pharmacokinetics. Chem Biodivers. 2007;4:1770–804. doi: 10.1002/cbdv.200790152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lemberger L, Crabtree RE, Rowe HM. 11-Hydroxy-delta-9-tetrahydrocannabinol: pharmacology, disposition, and metabolism of a major metabolite of marijuana in man. Science (Wash DC) 1972;177:62–4. doi: 10.1126/science.177.4043.62. [DOI] [PubMed] [Google Scholar]
- 15.Ohlsson A, Lindgren JE, Wahlen A, Agurell S, Hollister LE, Gillespie HK. Plasma delta-9-tetrahydrocannabinol concentrations and clinical effects after oral and intravenous administration and smoking. Clin Pharmacol Ther. 1980;28:409–16. doi: 10.1038/clpt.1980.181. [DOI] [PubMed] [Google Scholar]
- 16.Wall ME, Perez-Reyes M. The metabolism of delta-9-tetrahydrocannabinol and related cannabinoids in man. J Clin Pharmacol. 1981;21:178S–89S. doi: 10.1002/j.1552-4604.1981.tb02594.x. [DOI] [PubMed] [Google Scholar]
- 17.Goodwin RS, Gustafson RA, Barnes A, Nebro W, Moolchan ET, Huestis MA. Delta(9)-tetrahydrocannabinol, 11-hydroxy-delta(9)-tetrahydrocannabinol and 11-nor-9-carboxy-delta(9)-tetrahydrocannabinol in human plasma after controlled oral administration of cannabinoids. Ther Drug Monit. 2006;28:545–51. doi: 10.1097/00007691-200608000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Kemp PM, Abukhalaf IK, Manno JE, Manno BR, Alford DD, McWilliams ME, et al. Cannabinoids in humans. II. The influence of three methods of hydrolysis on the concentration of THC and two metabolites in urine. J Anal Toxicol. 1995;19:292–8. doi: 10.1093/jat/19.5.292. [DOI] [PubMed] [Google Scholar]
- 19.Abraham TT, Lowe RH, Pirnay SO, Darwin WD, Huestis MA. Simultaneous GC-EI-MS determination of delta9-tetrahydrocannabinol, 11-hydroxy-delta9-tetrahydrocannabinol, and 11-nor-9-carboxy-delta9-tetrahydrocannabinol in human urine following tandem enzyme-alkaline hydrolysis. J Anal Toxicol. 2007;31:477–85. doi: 10.1093/jat/31.8.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kemp PM, Abukhalaf IK, Manno JE, Manno BR, Alford DD, Abusada GA. Cannabinoids in humans. I. Analysis of delta-9-tetrahydrocannabinol and six metabolites in plasma and urine using GC-MS. J Anal Toxicol. 1995;19:285–91. doi: 10.1093/jat/19.5.285. [DOI] [PubMed] [Google Scholar]
- 21.Kelly P, Jones RT. Metabolism of tetrahydrocannabinol in frequent and infrequent marijuana users. J Anal Toxicol. 1992;16:228–35. doi: 10.1093/jat/16.4.228. [DOI] [PubMed] [Google Scholar]
- 22.Gustafson RA, Moolchan ET, Barnes A, Levine B, Huestis MA. Validated method for the simultaneous determination of delta-9-tetrahydrocannabinol (THC), 11-hydroxy-THC and 11-nor-9-carboxy-THC in human plasma using solid phase extraction and gas chromatographymass spectrometry with positive chemical ionization. J Chromatogr B. 2003;798:145–54. doi: 10.1016/j.jchromb.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 23.Wall ME, Taylor HL. Conjugation of acidic metabolites of delta-8 and delta-9-THC in man. In: Harvey DJ, Paton SW, Nahas GG, editors. Marihuana 84 Proceedings of the Oxford Symposium on Cannabis. Oxford: IRL Press Ltd; 1984. pp. 69–76. [Google Scholar]
- 24.Law B, Mason PA, Moffat AC, Gleadle RI, King LJ. Forensic aspects of the metabolism and excretion of cannabinoids following oral ingestion of cannabis resin. J Pharm Pharmacol. 1984;36:289–94. doi: 10.1111/j.2042-7158.1984.tb04376.x. [DOI] [PubMed] [Google Scholar]
- 25.Jones RT, Benowitz NL, Herning RI. Clinical relevance of cannabis tolerance and dependence. J Clin Pharmacol. 1981;21:143S–52S. doi: 10.1002/j.1552-4604.1981.tb02589.x. [DOI] [PubMed] [Google Scholar]
- 26.Haney M, Ward AS, Comer SD, Foltin RW, Fischman MW. Abstinence symptoms following oral THC administration to humans. Psychopharmacology (Berl) 1999;141:385–94. doi: 10.1007/s002130050848. [DOI] [PubMed] [Google Scholar]
- 27.Hunt CA, Jones RT. Tolerance and disposition of tetrahydrocannabinol in man. J Pharmacol Exp Ther. 1980;215:35–44. [PubMed] [Google Scholar]
- 28.Lowe RH, Karschner EL, Schwilke EW, Barnes AJ, Huestis MA. Simultaneous quantification of delta-9-tetrahydrocannabinol (THC), 11-hydroxy-delta-9-tetrahydrocannabinol (11-OH-THC), and 11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (THCCOOH) in human plasma using two-dimensional gas chromatography, cryofocusing, and electron impact-mass spectrometry. J Chromatogr A. 2007;1163:318–27. doi: 10.1016/j.chroma.2007.06.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.ElSohly M, Feng S. Delta-9-THC metabolites in meconium: identification of 11-OH-delta-9-THC, 8 beta, 11-diOH-delta-9-THC, and 11-nor-delta-9-THC-9-COOH as major metabolites of delta-9-THC. J Anal Toxicol. 1998;22:329–35. doi: 10.1093/jat/22.4.329. [DOI] [PubMed] [Google Scholar]
- 30.Frytak S, Moertel CG, Rubin J. Metabolic studies of delta-9-tetrahydrocannabinol in cancer patients. Cancer Treat Rep. 1984;68:1427–31. [PubMed] [Google Scholar]
- 31.Lemberger L, Tamarkin NR, Axelrod J. Delta-9-tetrahydrocannabinol: metabolism and disposition in long-term marihuana smokers. Science (Wash DC) 1971;173:72–4. doi: 10.1126/science.173.3991.72. [DOI] [PubMed] [Google Scholar]
- 32.Agurell S, Halldin M, Lindgren JE, Ohlsson A, Widman M, Gillespie H, Hollister L. Pharmaco-kinetics and metabolism of delta-tetrahydrocannabinol and other cannabinoids with emphasis on man. Pharmacol Rev. 1986;38:21–43. [PubMed] [Google Scholar]
- 33.Harvey DJ, Paton WDM. Metabolism of the cannabinoids. Rev Biochem Toxicol. 1986;6:221–64. [Google Scholar]
- 34.Glaz-Sandberg A, Dietz L, Nguyen H, Oberwittler H, Aderjan R, Mikus G. Pharmacokinetics of 11-nor-9-carboxy-delta(9)-tetrahydrocannabinol (CTHC) after intravenous administration of CTHC in healthy human subjects. Clin Pharmacol Ther. 2007;82:63–9. doi: 10.1038/sj.clpt.6100199. [DOI] [PubMed] [Google Scholar]
- 35.Sallustio BC, Sabordo L, Evans AM, Nation RL. Hepatic disposition of electrophilic acyl glucuronide conjugates. Curr Drug Metab. 2000;1:163–80. doi: 10.2174/1389200003339153. [DOI] [PubMed] [Google Scholar]
- 36.Strassburg CP, Manns MP, Tukey RH. Expression of the UDP-glucuronosyltransferase 1A locus in human colon: identification and characterization of the novel extrahepatic UGT1A8. J Biol Chem. 1998;273:8719–26. doi: 10.1074/jbc.273.15.8719. [DOI] [PubMed] [Google Scholar]
- 37.Yamanaka H, Nakajima M, Katoh M, Yokoi T. Glucuronidation of thyroxine in human liver, jejunum, and kidney microsomes. Drug Metab Dispos. 2007;35:1642–8. doi: 10.1124/dmd.107.016097. [DOI] [PubMed] [Google Scholar]
- 38.Skopp G, Potsch L, Mauden M, Richter B. Partition coefficient, blood to plasma ratio, protein binding and short-term stability of 11-nor-delta-9-carboxy tetrahydrocannabinol glucuronide. Forensic Sci Int. 2002;126:17–23. doi: 10.1016/s0379-0738(02)00023-3. [DOI] [PubMed] [Google Scholar]
- 39.Skopp G, Potsch L. Stability of 11-nor-delta(9)-carboxy-tetrahydrocannabinol glucuronide in plasma and urine assessed by liquid chromatography-tandem mass spectrometry. Clin Chem. 2002;48:301–6. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


