Abstract
Current technologies for tumor imaging, such as ultrasound, MRI, PET and CT, are unable to yield high-resolution images for the assessment of nanoparticle uptake in tumors at the microscopic level1,2,3, highlighting the utility of a suitable xenograft model in which to perform detailed uptake analyses. Here, we use high-resolution intravital imaging to evaluate nanoparticle uptake in human tumor xenografts in a modified, shell-less chicken embryo model. The chicken embryo model is particularly well-suited for these in vivo analyses because it supports the growth of human tumors, is relatively inexpensive and does not require anesthetization or surgery 4,5. Tumor cells form fully vascularized xenografts within 7 days when implanted into the chorioallantoic membrane (CAM) 6. The resulting tumors are visualized by non-invasive real-time, high-resolution imaging that can be maintained for up to 72 hours with little impact on either the host or tumor systems. Nanoparticles with a wide range of sizes and formulations administered distal to the tumor can be visualized and quantified as they flow through the bloodstream, extravasate from leaky tumor vasculature, and accumulate at the tumor site. We describe here the analysis of nanoparticles derived from Cowpea mosaic virus (CPMV) decorated with near-infrared fluorescent dyes and/or polyethylene glycol polymers (PEG) 7, 8, 9,10,11. Upon intravenous administration, these viral nanoparticles are rapidly internalized by endothelial cells, resulting in global labeling of the vasculature both outside and within the tumor7,12. PEGylation of the viral nanoparticles increases their plasma half-life, extends their time in the circulation, and ultimately enhances their accumulation in tumors via the enhanced permeability and retention (EPR) effect 7, 10,11. The rate and extent of accumulation of nanoparticles in a tumor is measured over time using image analysis software. This technique provides a method to both visualize and quantify nanoparticle dynamics in human tumors.
Keywords: Medicine, Issue 52, Nanoparticles, tumors, intravital imaging, avian embryo, confocal microscopy
Protocol
1. Inoculation of tumor into avian embryo CAM
Prepare shell-less fertilized chicken embryos as described8.
On Day 9 of embryonic development, assemble a micro-injector using an 18-gauge needle connected onto 1 mL syringe. Cut a 5-6 inches piece of Tygon tubing (1/32" inner diameter, 3/32" outer diameter,1/32" wall thickness) and carefully insert bevel of needle into the tubing. Approximately 4-5 inches of tubing should extend from the tip of the needle (Figure 1a).
Fill the syringe and tubing with cell suspension. Then, insert a microinjection glass needle at the end of the tubing and carefully remove any air bubbles.
Inject Day 9 embryos (Figure 1b) under a dissection scope with an illuminator with 10,000-100,000 cancer cells as a bolus within the CAM (Figure 1c). Slowly inject cells and carefully ensure that the needle is in the correct place for the cells to form a visible bolus within the CAM. Cells that drip onto the CAM surface can be cleaned using Kimwipe or other applicator.
Return embryos to humidified incubator at 38°C at 60% humidity and allow tumor to grow and vascularize (up to 7 days).
2. Preparation of nanoparticles
To prepare fluorescently labeled CPMV nanoparticles for injection into the chicken embryo; dilute the viral nanoparticles (synthesized as in 8 in PBS, pH 7.4, to a concentration of 100 μg/ml. Vortex mixture well before using and centrifuge for one minute to remove any aggregates. Sonication may also be useful depending on conjugates and degree of aggregation. Stocks of fluorescently labeled CPMVs are stable for at least 1 year when stored at 4°C in the dark. Check stocks periodically by putting a couple drops onto a glass slide and checking for fluorescence. Transmission Electron Microscopy (TEM) can also be used to determine if the particles remained intact after conjugation.
Briefly, one microgram of viral nanoparticles (in a final volume of 2 μl) can be added to copper coated grids. Next, add an equal volume of 2% uranyl acetate for 1 minute at electron microscope (Philips EM 410).
3. Intravenous injection of fluorescently-labeled viral nanoparticles
On Day 16, assemble micro-injector as described above. Draw up desired volume of viral nanoparticle through the tubing into the syringe (> 200 μL). Carefully remove any air bubbles. Insert microinjection glass needle at the end of the tubing. Ensure that the needle is as long and tapered as possible (Figure 2a). If the needle is too blunt, it will not be able to pierce through the ectoderm and will fail to penetrate the vessel. If the needle is too sharp, the tip will collapse when penetrating tissue.
Intravenously inject 100 μl of 1 mg/ml fluorescein dextran (MW 70,000 Da, Invitrogen) into tumor bearing embryo distal from the desired site to be visualized (Figure 3d). Successful cannulation of CAM vein is evident by the clearing of blood in the path of the injection flow (Figure 2b). Assess vascular leak 1 hour after injection.
Intravenously inject 50 μl of 1 mg/ml solution of CPMV-Alexa Fluor 647 (CPMV-AF 647) or PEGylated CPMV-Alexa Fluor 647 (CPMV-PEG-AF 647) into embryos containing tumors with vascular leak distal from the desired site to be visualized.
Image tumors immediately and every hour after injection using a Zeiss Examiner Z1 upright microscope fitted with a Yokogawa spinning disk, Hamamatsu ImagEM 9100-12 EM-CCD camera.
4. Real time intravital imaging
To assemble the embryo imaging unit, apply a thin layer of vacuum grease around the circumference of the imaging port on the underside of the lid of the embryo imaging unit, and fit an 18 mm glass coverslip onto the port.
Position the embryo such that the coverslip will cover the desired area for imaging. Slowly lower the lid until the coverslip just makes contact with the embryo, and then screw the lid onto the unit to hold it in place (Figure 2c).
Add water heated to 37°C into the embryo imaging unit outside of the dish containing the embryo, and then place the entire unit onto the stage of an upright confocal microscope with the inside environmental chamber equilibrated to 37°C.
Position the imaging unit containing the embryo under the Spinning disk confocal fluorescence microscope (Figure 2e). The imaging unit will hold the embryo in place and keep the field of view fixed while capturing images, allowing for both three-dimensional Z stacks and time-lapse images to be captured. We acquire and analyze three-dimensional time-lapse images using Perkin Elmer’s (formerly Improvision) Volocity software package (Figure 3a). Acquire a high-resolution three-dimensional stack of the tumor and surrounding vasculature to visualize detailed structural analyses at specific time-points. Acquire three-dimensional stacks at regular time-points to map detailed structural changes in the tumor vasculature. Image tumors every hour after injection.
Quantitate the uptake of viral nanoparticles by calculating the mean Alexa Fluor (AF) 647 signal within selected regions in the tumor or in the stroma (non-tumor area) using image quantitation software such as Volocity (Perkin Elmer). The tumor to stroma ratio was calculated by dividing the mean AF 647 signal in the tumor over the mean AF 647 signal in the stroma. A tumor/stroma ratio higher than 1 indicates that the nanoparticle is being taken up by the tumor.
5. Representative results:
In the example described here, we injected HT-29 colon cancer cells to form a bolus approximately 1mm in size within the CAM of day 9 chicken embryos (Figure 1b). After inoculation, the embryos were cultured for 7 days in a humidified incubator to permit sufficient tumor growth and vascularization (Figure 1c). Embryos were injected intravenously with a low molecular weight dextran to confirm tumor vascularization, and the tumors were visualized under the Zeiss AxioExaminer Z1 upright microscope (Figure 2d).
After intravenous administration of CPMV-AF 647 or CPMV-PEG-AF 647 nanoparticles (Figure 3a and b), high-resolution real time confocal imaging (Figure 2e) revealed that both CPMV and CPMV-PEG nanoparticles rapidly labeled the entire vasculature, but the uptake of CPMV-PEG by the tumor was approximately 3 times higher than CPMV after 12 hours (Figure 3a). The relative tumor uptake of nanoparticles was determined using image analysis software (Volocity from Perkin Elmer). Regions of interest were selected within and outside the tumor (in the stromal compartment) and the mean fluorescence intensity of each was determined. Data is expressed as tumor/stroma ratio.
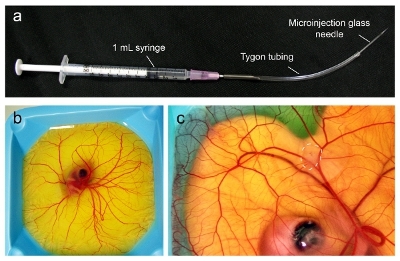 Figure 1.Microinjection of tumors into the CAM of an avian embryo. (a) The microinjection apparatus is assembled from the components as indicated. (b) Avian embryos at day 9 are ready to be inoculated with tumor when the CAM has spread to cover the entire surface. (c) At day 16, the tumor will have grown to up to 1 cm in diameter (dashed line) and is ready for injection with nanoparticles.
Figure 1.Microinjection of tumors into the CAM of an avian embryo. (a) The microinjection apparatus is assembled from the components as indicated. (b) Avian embryos at day 9 are ready to be inoculated with tumor when the CAM has spread to cover the entire surface. (c) At day 16, the tumor will have grown to up to 1 cm in diameter (dashed line) and is ready for injection with nanoparticles.
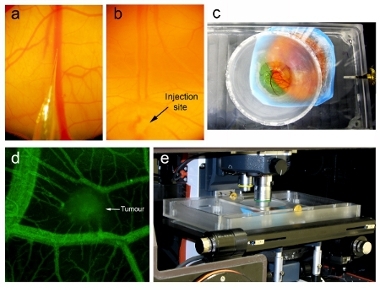 Figure 2.Nanoparticle injection and intravital imaging. Injection under a dissection microscope showing (a) the tip of the microinjector needle ready to be injected into the CAM vein and (b) the microinjector needle inserted into the vein (indicated by arrow) and nanoparticles injected into the blood flow (seen by clearing of blood). (c) Imaging unit containing avian embryo with the coverslip interfaced directly with the CAM. (d) Prior to nanoparticle injection, tumor vascularization is assessed using intravital imaging after injection of fluorescein dextran. (e) Imaging unit containing the embryo positioned on the stage of an upright confocal microscope within a temperature-regulated enclosure set to 37°C.
Figure 2.Nanoparticle injection and intravital imaging. Injection under a dissection microscope showing (a) the tip of the microinjector needle ready to be injected into the CAM vein and (b) the microinjector needle inserted into the vein (indicated by arrow) and nanoparticles injected into the blood flow (seen by clearing of blood). (c) Imaging unit containing avian embryo with the coverslip interfaced directly with the CAM. (d) Prior to nanoparticle injection, tumor vascularization is assessed using intravital imaging after injection of fluorescein dextran. (e) Imaging unit containing the embryo positioned on the stage of an upright confocal microscope within a temperature-regulated enclosure set to 37°C.
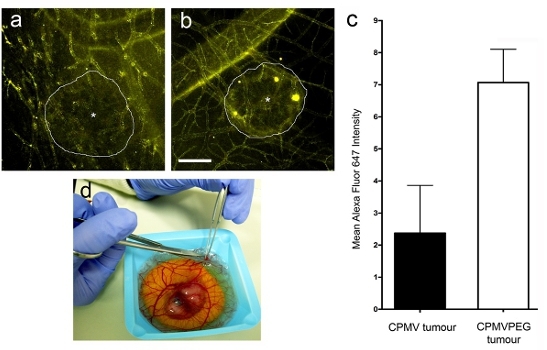 Figure 3.Intravital visualization of nanoparticle uptake in human tumors. Tumors are visualized 7 hours after injection of (a) CPMV-AF647 and (b) CPMV-PEG-AF647. d) Excision of tumor from avian embryo for subsequent analysis.
Figure 3.Intravital visualization of nanoparticle uptake in human tumors. Tumors are visualized 7 hours after injection of (a) CPMV-AF647 and (b) CPMV-PEG-AF647. d) Excision of tumor from avian embryo for subsequent analysis.
Discussion
The chorioallantoic membrane (CAM) of the avian embryo is a useful model to assess the vascular dynamics and pharmacokinetics of human tumors. The structure and position of the CAM allows high quality image acquisition and accommodates of many kinds of cancer xenografts without invasive surgical procedures. Moreover, cancer tumor xenografts implanted into the chorioallantoic membrane become vascularized within 7 days, offering a rapid, inexpensive and semi-high-throughput means to assess the accumulation of nanoparticles in tumor tissue. Since cancer xenografts implanted in the CAM of shell-less chicken embryos are accessible to the high-resolution optics of an upright epifluorescence or confocal microscope, contextual and temporal information regarding nanoparticle uptake in the tumor vasculature can be readily obtained. Cancer xenografts in this model tend to grow laterally across the CAM, resulting in tumors that are large while remaining less than 200 m in depth. This makes them particularly well-suited for intravital imaging because standard epifluorescence microscopes can effectively penetrate the entire tumor mass. In contrast, tumors implanted in either superficial or orthotopic sites within the mouse proliferate in three dimensions, making it difficult to accurately localize nanoparticles deep within these tumors by non-invasive techniques. We have utilized this model to assess the uptake of quantum dots, liposomes, and iron oxide nanoparticles in a number of human tumor xenografts, highlighting the potential for this model to be suitable for the in vivo analysis of a broad range of nanoparticle formulations.
Disclosures
No conflicts of interest declared.
Acknowledgments
This study was supported by CCSRI Grant #700537 and CIHR Grant #84535 to JDL and NIH/NCI grant #CA120711-01A1 and CA120711-01A1 to AZ. All experiments were performed in accordance with the regulations and guidelines of the Institutional Animal Care and Use Committee at the University of California San Diego, Animal Care and Use at the University of Western Ontario.
References
- Halin C, Mora JR, Sumen C, von Andrian UH. In vivo imaging of lymphocyte trafficking. Annu Rev Cell Dev Biol. 2005;21:581–603. doi: 10.1146/annurev.cellbio.21.122303.133159. [DOI] [PubMed] [Google Scholar]
- Judenhofer MS. Simultaneous PET-MRI: a new approach for functional and morphological imaging. Nat Med. 2008;14:459–465. doi: 10.1038/nm1700. [DOI] [PubMed] [Google Scholar]
- Weissleder R, Pittet MJ. Imaging in the era of molecular oncology. Nature. 2008;452:580–589. doi: 10.1038/nature06917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers AF, Ling V. Selection for experimental metastatic ability of heterologous tumor cells in the chick embryo after DNA-mediated transfer. Cancer Res. 1984;44:3970–3975. [PubMed] [Google Scholar]
- Cretu A, Fotos JS, Little BW, Galileo DS. Human and rat glioma growth, invasion, and vascularization in a novel chick embryo brain tumor model. Clin Exp Metastasis. 2005;22:225–236. doi: 10.1007/s10585-005-7889-x. [DOI] [PubMed] [Google Scholar]
- Zijlstra A, Lewis J, Degryse B, Stuhlmann H, Quigley JP. The inhibition of tumor cell intravasation and subsequent metastasis via regulation of in vivo tumor cell motility by the tetraspanin CD151. Cancer cell. 2008;13:221–234. doi: 10.1016/j.ccr.2008.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis JD. Viral nanoparticles as tools for intravital vascular imaging. Nature medicine. 2006;12:354–360. doi: 10.1038/nm1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong HS. Intravital imaging of embryonic and tumor neovasculature using viral nanoparticles. Nature protocols. 2010;5:1406–1417. doi: 10.1038/nprot.2010.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterji A. New addresses on an addressable virus nanoblock; uniquely reactive Lys residues on cowpea mosaic virus. Chemistry & biology. 2004;11:855–863. doi: 10.1016/j.chembiol.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Brunel FM. Hydrazone ligation strategy to assemble multifunctional viral nanoparticles for cell imaging and tumor targeting. Nano letters. 2010;10:1093–1097. doi: 10.1021/nl1002526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmetz NF, Manchester M. PEGylated viral nanoparticles for biomedicine: the impact of PEG chain length on VNP cell interactions in vitro and ex vivo. Biomacromolecules. 2009;10:784–792. doi: 10.1021/bm8012742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmetz NF, Cho CF, Ablack A, Lewis JD, Manchester M. CPMV nanoparticles target surface vimentin on cancer cells. Nanomedicine. 2010. Forthcoming. [DOI] [PMC free article] [PubMed]


