Abstract
Background
Functional ability following nerve transfer for upper brachial plexus injuries relies on both the function and magnitude of force recovery of targeted muscles. Following nerve transfers targeting either the axillary nerve, suprascapular nerve, or both, it is unclear whether functional ability is restored in face of limited muscle force recovery.
Methods
We used a computer model to simulate flexing the elbow while maintaining a functional shoulder posture for 3 nerve transfer scenarios. The minimum restored force capacity necessary to perform the task, associated compensations by neighboring muscles, and the effect of altered muscle coordination on movement effort, were assessed.
Results
The minimum force restored by the axillary, suprascapular, and combined nerve transfers that was required for the model to simulate the desired movement was 25%, 40%, and 15% of the unimpaired muscle force capacity, respectively. When the deltoid was paralyzed, the infraspinatus and subscapularis muscles generated higher shoulder abduction moments to compensate for deltoid weakness. For all scenarios, movement effort increased as restored force capacity decreased.
Conclusions
Combined axillary and suprascapular nerve transfer required the least restored force capacity to perform the desired elbow flexion task, while single suprascapular nerve transfer required the most restored force capacity to perform the same task. Though compensation mechanisms allowed all scenarios to perform the desired movement despite weakened shoulder muscles, compensation increased movement effort. Dynamic simulations allowed independent evaluation of the effect of restored force capacity on functional outcome in a way that is not possible experimentally.
Clinical Relevance
Simultaneous nerve transfer to suprascapular and axillary nerves yields the best simulated biomechanical outcome for lower magnitudes of muscle force recovery in this computer model. Axillary nerve transfer performs nearly as well as the combined transfer, while suprascapular nerve transfer is more sensitive to the magnitude of reinnervation and therefore avoided.
Keywords: Biomechanics, Computer Simulation, Brachial Plexus, Nerve Transfer, Shoulder
Introduction
Brachial plexus injuries commonly result in avulsion of C5 and C6 nerve roots (1) and impair elbow flexion and shoulder function (2, 3). Surgical interventions seek to restore shoulder stability and reanimate elbow flexion to provide patients purposeful arm function. While combined nerve transfers to both suprascapular and axillary nerves are preferred to restore shoulder function, occasionally only single nerve transfer to either the axillary or suprascapular nerve may be possible due to limited donor nerve availability (4-6). Factors that influence functional outcomes after nerve transfers include overall patient health, injury severity, and surgical technique (7). Biomechanically, the magnitude of restored muscle force capacity in reinnervated muscles influences a patient’s postoperative ability to perform tasks.
During functional movement, muscles rotate a joint by generating moment as a function of the magnitude of muscle force and the distance from the joint center of rotation (moment arm). Whether muscles generate sufficient moment to perform a functional task is a measure of strength. From a biomechanical standpoint, joint strength is most effectively restored when muscles that generate relatively large joint moments favorable for performing a functional task are preferentially targeted for nerve transfer. Previous analyses considered biomechanical factors, such as moment arm and isometric joint strength, independently to evaluate the importance of the deltoid and infraspinatus muscles during basic shoulder abduction and external rotation movements (5). However, analyses did not simultaneously consider other determinants of muscle force (e.g. optimal fiber length, pennation angle, and muscle volume), the magnitude of muscle force recovery, or dynamic interactions among muscles and limb segments in the context of multi-joint movement (8, 9).
Computer-generated dynamic musculoskeletal models are a compendium of mathematical representations of experimentally-derived anatomical properties, strength measurements, and joint kinematics. Computational models of movement use fundamental mechanics to describe physiologic musculoskeletal behavior. A benefit of simulation is that muscle model properties can be altered to represent clinical scenarios and evaluate the influence of individual biomechanical factors in isolation on movement. For example, dynamic simulation has been used to assess contributions of shoulder and elbow muscles to wheelchair propulsion (10) and the influence of muscle strength on pinch force following brachioradialis transfer (11).
This study sought to elucidate biomechanical consequences of nerve transfer strategies targeting the axillary nerve, suprascapular nerve, or both using dynamic simulation. The goal was to evaluate (i) the minimum restored force capacity of reinnervated muscles required to perform a characteristic upper limb functional task and (ii) the effect of compensations following nerve transfer on movement effort. Limb strength, movement effort, and muscle coordination were not considered in previous biomechanical analyses of shoulder nerve transfers but may have important clinical implications for upper limb movement following brachial plexus injury. This study hypothesized that task performance following combined shoulder nerve transfer will be more similar to an unimpaired upper limb than single nerve transfer to the axillary or suprascapular nerve and that muscle coordination will change as less muscle force is recovered following transfer in order to compensate for muscle weakness.
Materials and Methods
This study used a three-dimensional computer model of the upper limb musculoskeletal system (12) to simulate movement of the upper extremity following various nerve transfers. The computer model was designed as a platform for a broad range of neuromuscular and clinical simulations, capable of dynamic simulation (10, 13), and implemented in the OpenSim open-source modeling environment (Stanford University, California) (14). Five physiological degrees of freedom at the shoulder and elbow (shoulder abduction, shoulder flexion/extension, shoulder rotation, elbow flexion, and forearm pronation/supination) were represented (Figure 1). The movement of the scapula and clavicle were constrained to account for stabilizing physiological action of the trapezius, serratus anterior, and pectoralis minor during movement of the shoulder girdle (15). The architecture and origin-to-insertion paths of 23 muscles and muscle compartments crossing the elbow and shoulder joints (Table 1) were defined based on anatomical data from previous studies (16-20). Muscle fiber lengths and moment arms for each simulated muscle compartment were calculated as a function of the joint postures. A mathematical model of the muscle-tendon unit was used to calculate the total force a muscle could produce passively when stretched and actively when contracted during neuronal excitation (21). Active forces depending on the cross-sectional area, length, and shortening velocity of the muscle-tendon unit were allowed to vary from inactive to fully active levels according to the coordination pattern needed to produce the movement. Passive forces generated by stretched muscles were independent of muscle activation.
Figure 1. The upper extremity model represented five degrees of freedom at the shoulder and elbow: shoulder abduction, shoulder rotation, shoulder flexion/extension, elbow flexion, and forearm pronation/supination (not shown).
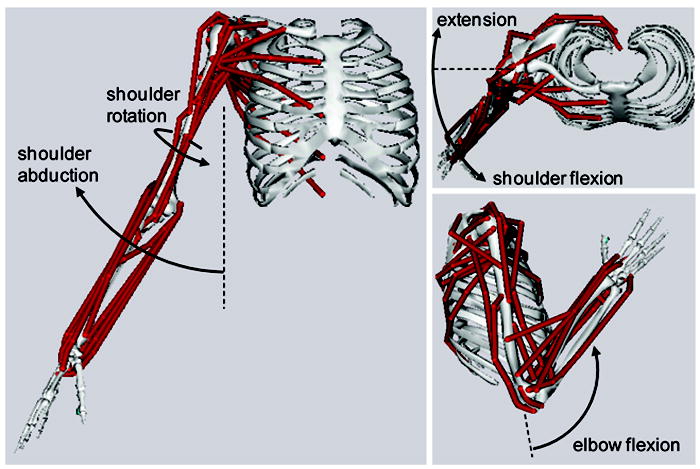
The model is shown with the limb in the initial (left and upper right) and final (lower right) postures of the movement.
TABLE 1.
Muscles Represented in the Upper Extremity Model
| Region | Shoulder | Elbow | Forearm |
|---|---|---|---|
| Muscle | Deltoid | Triceps brachii | Brachioradialis |
| Supraspinatus | Biceps brachii | Extensor carpi radialis longus | |
| Infraspinatus | Brachialis | Extensor carpi radialis brevis | |
| Subscapularis | Anconeus | Extensor carpi ulnaris | |
| Teres major | Supinator | Flexor carpi radialis | |
| Teres minor | Flexor carpi ulnaris | ||
| Latissimus dorsi | Palmaris longus | ||
| Pectoralis major | Pronator teres | ||
| Coracobrachialis | Pronator quadratus |
Three scenarios were generated, each representing a common nerve transfer procedure to the axillary nerve and/or suprascapular nerve for avulsion of the C5 and C6 nerve roots. A fourth scenario representing a normal, unimpaired limb was generated for comparison. Paralyzed muscles and muscles reinnervated by nerve transfer were defined for each scenario based on descriptions of common procedures found in the literature (Table 2).
TABLE 2.
Upper Extremity Clinical Cases
| scenario name | muscles paralyzed | muscles reinnervated |
|---|---|---|
| unimpaired | none | none |
| axillary | SUP, INF, TRIB | DELT, TMIN, BIC, BRA |
| suprascapular | DELT, TMIN | SUP, INF, BIC, BRA |
| combined | TRIB | SUP, INF, DELT, TMIN, BIC, BRA |
SUP = supraspinatus, INF = infraspinatus, DELT = deltoid, TMIN = teres minor, TRIB = triceps brachii, BIC = biceps, BRA = brachialis, BRD = brachioradialis
Brachial plexus avulsion injury of the C5 and C6 nerve roots presents with paralysis of the supraspinatus, infraspinatus, deltoid, teres minor, biceps brachii, brachialis, and brachioradialis (2). In all 3 nerve transfer scenarios, the biceps brachii and brachialis were assumed to be reinnervated by a double musculocutaneous nerve transfer (22). The axillary nerve scenario simulated nerve transfer to the axillary nerve with reinnervation of the deltoid and teres minor using the radial nerve branch to the long head of the triceps. The long head of the triceps is denervated as a consequence of this procedure (Table 2) (3). The suprascapular nerve scenario simulated nerve transfer to the suprascapular nerve with reinnervation of the supraspinatus and infraspinatus using the spinal accessory nerve (Table 2) (5). The combined scenario represented nerve transfers to both the suprascapular and axillary nerves (Table 2).
Functional movement was assessed through simulation of a task that is characteristic of eating, lifting, or reaching. With the shoulder held in a functional posture of 25° of abduction, 25° of flexion, and 20° of internal rotation, the elbow was flexed from 0° to 120° in 1 second (23) (Figure 1). The forearm and wrist were held in the neutral position. Whether the model could perform the desired movement accurately depended on the overall strength of the simulated muscle properties in each nerve transfer scenario. A computed muscle control (CMC) algorithm (24) was used to calculate the muscle activations that allowed the model to perform the desired movement as accurately as possible while minimizing a physiologically-based estimate of the effort (i.e. metabolic cost) that muscles exerted to perform the movement (25). This algorithm permits cocontraction of muscles if that pattern of activation satisfies the movement conditions and minimizes the effort cost.
While the CMC algorithm was used to calculate the actual activation levels of muscles during the movement, there were limits placed on the maximal activation a muscle could experience. This limit was expressed as a percentage of its unimpaired force capacity. Unimpaired muscles were allowed to be fully activated, so these muscles had a force capacity of 100%. Paralyzed muscles were not allowed to be activated and had a force capacity of 0%. Reinnervated muscle activations were varied among simulations to determine the minimum restored force capacity of reinnervated muscles necessary to perform the movement accurately. For each scenario, a set of simulations were performed in which the restored force capacity of reinnervated muscles was decreased from 100% in 5% increments. In a given simulation, all muscles reinnervated by shoulder nerve transfer had the same activation limit. Passive force properties of reinnervated muscles were assumed to be unaffected, while paralyzed muscles could produce passive properties only. To fully represent a typical C5-C6 injury while limiting variability across simulations, muscles reinnervated by the musculocutaneous nerve transfer could generate force up to 20% of their unimpaired capacity in all simulations (26).
The accuracy of a simulated movement was determined by comparing the resulting joint angles of an unimpaired model to the joint angles in nerve transfer scenarios. A simulated movement that resulted in joint angles with less than 1° of average difference was classified as accurate.
Joint moments for each muscle crossing the shoulder were calculated to determine if muscular compensations were needed following nerve transfer. Moment, a measure of joint strength, is the product of muscle force and moment arm. Since the movement was the same for all successful simulations, the net joint moments were also the same. However, individual muscle contributions could vary based on altered coordination strategies. We evaluated the individual muscle moments for the point in the movement at which the net shoulder moments were maximal for the 3 scenarios, with reinnervated muscles permitted fully-restored force capacity (100%) and expressed as a percentage of the net joint moment.
Finally, we evaluated the effort required by each scenario to perform the desired elbow flexion movement while dynamically stabilizing the shoulder, as described earlier. The movement effort was calculated using the effort function that was minimized by the CMC algorithm (25) and expressed as the ratio of the movement effort of the nerve transfer scenarios to the movement effort of the unimpaired scenario.
Results
The minimum restored force capacity required by the axillary, suprascapular, and combined nerve transfer scenarios to perform the desired movement accurately was 25%, 40%, and 15%, respectively. The peak net joint moments occurred when the elbow was flexed to approximately 14°. For the axillary nerve scenario, the ability to perform the task with reduced restored force capacity was limited by the strength of the muscles that contribute to external shoulder rotation moment. That is, below 25% restored force capacity, external rotation moment was not sufficient to maintain the desired posture. In contrast, the suprascapular nerve and combined scenarios were limited by the ability of the muscles to generate sufficient positive shoulder abduction moment.
In the unimpaired scenario, the deltoid, infraspinatus, subscapularis, and supraspinatus were 4 of the primary muscles that generated moments in the same direction as the net shoulder abduction moment. When restored by axillary or combined nerve transfer, the deltoid generated the largest shoulder abduction moment (Figure 2). The moment generated by the deltoid exceeded 100% of the net moment for the unimpaired, axillary, and combined scenarios because of the simultaneous action of antagonist muscles (pectoralis major, latissimus dorsi, triceps long head, and biceps short head) that adduct the shoulder. Additionally in this posture, the restored deltoid generated an internal rotation moment that is consistent with that developed in the unimpaired arm (Figure 3). When the deltoid remained paralyzed in the suprascapular scenario, the infraspinatus and subscapularis were more highly activated and generated shoulder abduction moments that were higher than those in the unimpaired scenario to compensate for deltoid weakness. However, as a consequence, the infraspinatus generated a very large external rotation moment that opposed the net shoulder internal rotation moment and required antagonist action of the subscapularis to maintain the shoulder posture (Figure 3).
Figure 2. Shoulder abduction moment contributions by deltoid, infraspinatus, subscapularis, and supraspinatus at the point in the motion when the net shoulder joint moments were maximal.
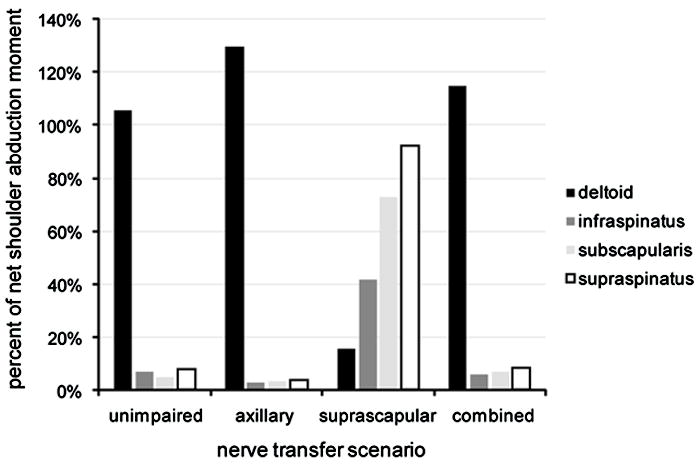
The moments are shown as a percent of the net shoulder abduction moment and can exceed 100% due to the simultaneous action of antagonist muscles. In the unimpaired, axillary, and combined scenarios, the deltoid was the primary contributor to net shoulder abduction moment. When the deltoid remained paralyzed in the suprascapular scenario, the infraspinatus, subscapularis, and supraspinatus muscles were the primary contributors to net shoulder abduction moment.
Figure 3. Shoulder rotation moment contributions by deltoid, infraspinatus, subscapularis, and supraspinatus at the point in the motion when the net shoulder joint moments were maximal.
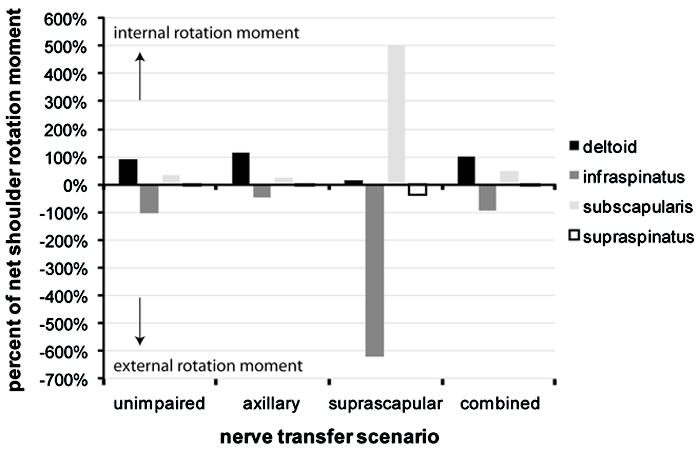
Shoulder rotation moments are shown as a percent of net shoulder rotation moment, respectively. Positive values indicate an internal rotation moment, while negative values indicate an external rotation moment.
The movement effort increased as the restored activation capacity of muscles in each scenario decreased (Figure 4). The combined scenario exhibited the lowest movement effort of the 3 nerve transfer scenarios. The movement effort of the suprascapular scenario was approximately 50% higher than that of the axillary and combined scenarios.
Figure 4. Relationship between restored force capacity and movement effort.
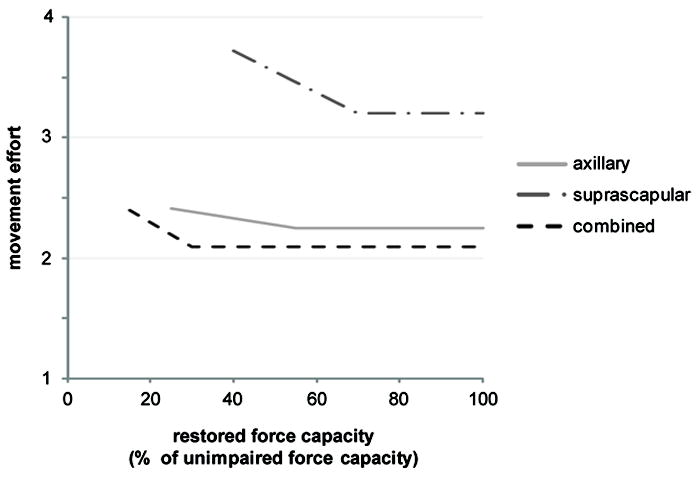
The movement effort was expressed as the ratio of the effort required by the nerve transfer scenario to perform the desired movement to the effort required by the unimpaired scenario to perform the desired movement. The suprascapular scenario exhibited the highest movement effort, while the combined scenario exhibited the lowest movement effort. Movement effort decreased as restored force capacity increased.
Discussion
Three shoulder nerve transfer scenarios were simulated to elucidate how the magnitude of restored force capacity affects performance of a functional task. The minimum restored force capacity required to perform the intended movement correlates to the extent of muscle recovery achieved by nerve transfers and reinnervation of the target muscles. Nerve transfer scenarios that were able to perform the movement with lower restored force capacity required less muscle reinnervation compared to transfer scenarios requiring higher restored force capacity to perform the movement. The combined axillary and suprascapular nerve transfer required the least restored force capacity for adequate functional movement. This finding concurs with clinical observations that combined nerve transfers provides enhanced functional recovery compared to single nerve transfers for brachial plexus injuries (4, 6, 27). Of the single nerve transfer scenarios, the axillary scenario outcome required a lower restored force capacity to perform the elbow flexion movement accurately.
Shoulder joint moments generated by muscles crossing the shoulder were evaluated to identify the biomechanical role of muscles targeted by nerve transfers during functional movement. In the suprascapular scenario, the infraspinatus and subscapularis were required to contribute larger shoulder abduction moments to compensate for deltoid paralysis. Though compensation enabled the suprascapular simulations to perform the desired movement while the deltoid remained paralyzed, the movement was performed less efficiently. The unique musculoskeletal geometry and muscle architecture of the deltoid allowed it to elevate the shoulder without generating axial rotation moments that required antagonist action to overcome. The muscle properties of the infraspinatus and subscapularis were not as well-suited for generating the required shoulder joint moments.
Several limitations of this study should be considered. We used a generic model representing average musculoskeletal properties of an adult male. These properties vary across subjects and with age and gender. Among all simulations, the musculoskeletal properties were held constant while restored force capacity was varied, allowing assessment of the independent effect of restored force capacity on movement ability. Though differences in strength may affect the magnitude of restored force capacity required to accomplish the task, we expect that relative results among nerve transfer scenarios would be consistent.
We assumed that the restored force capacity of muscles reinnervated by a musculocutaneous nerve transfer was 20%, based on a reported average recovered elbow flexion strength of 27% compared to normal contralateral strength following musculocutaneous nerve transfer (26). This was held constant across all scenarios to focus on differences in function associated with different shoulder strategies only. The simulated musculocutaneous transfer was sufficient to flex the elbow, thus shoulder muscle function was the limiting determinant in performing the desired movement.
Muscles that stabilize the clavicle and scapula, including the trapezius, serratus anterior, and pectoralis minor, were not expected to be affected by C5-C6 injury or nerve transfers simulated in this study and were not included in the analysis (2, 5, 6). The physiological action of these muscles was instead accounted for by constraining movement of the clavicle and scapula in the computational model (15). Clinically, the static and dynamic positions of the scapula may be altered due to changes in shoulder muscle function following injury. However, the shoulder maintained a static posture during the entire movement, so any affect of injury on shoulder girdle posture would be consistent across scenarios.
The simulated nerve transfers reduced force capacity of muscles affected by injury; however, other muscle properties not accounted for may also be affected. The formation of contractures (28) following injury cause a decrease in muscle fiber lengths of unimpaired muscles and limit the upper extremity range of motion. Atrophy, fibrosis, and joint stiffness following brachial plexus injury may further limit functional recovery (29, 30). Though passive force adaptations associated with contracture and atrophy were unaccounted for, the reduced functional ability would likely be consistent for all clinical treatment scenarios modeled here. Therefore, while the magnitude of necessary joint moments or effort may increase to account for these additional changes in muscle and joint properties, we expect that the relative performance of the 3 clinical scenarios discussed here would remain.
Muscle activations were calculated using a CMC algorithm, assuming for all scenarios that muscle coordination would minimize the metabolic effort required to perform the desired movement (25). CMC has been used to predict activations of lower limb muscles during unimpaired (24) and pathological ambulation (14). CMC has also been used to predict activations of upper limb muscles during a functional pull and a forward reach (13). In both instances, the CMC results were consistent with electromyograms measured during the movements for which they were calculated. Therefore, the CMC algorithm provided a reasonable and accepted method to evaluate the movement ability of the scenarios.
Results from this computer simulation study indicate that simultaneous nerve transfer to the suprascapular and axillary nerves yields superior simulated biomechanical outcomes for a single functional movement of important upper extremity function (31) (eating, lifting, reaching) for lower magnitudes of muscle reinnervation. Transfer to the axillary nerve performs nearly as well as a combined transfer, while suprascapular nerve transfer is more sensitive to the magnitude of reinnervation. Surgical factors which may affect restored muscle force capacity include the donor nerve, proximity of the implanted donor nerve to the reinnervated muscle, and the number and size of transferred motor neurons (5, 27, 32). Optimization of these factors is limited; therefore knowledge of the functional movements that can be achieved through various nerve transfers based on biomechanical simulations can provide guidance toward surgical treatment. The axillary and suprascapular nerves reinnervate muscles with different biomechanical roles, therefore single nerve transfers may be chosen depending on the dynamic requirements of the intended patient-specific functional tasks. Transfer approaches that are less sensitive to the magnitude of force restored to a reinnervated muscle may provide a more robust functional outcome requiring less compensation and reduced effort. Further studies are needed to examine the outcome of nerve transfers for various important functional movements during activities of daily living. This would allow surgeons to prioritize surgical strategies according to patient needs.
Acknowledgments
This work was supported by the National Institutes of Health (NIH 5R24HD050821-02) and the Wake Forest School of Medicine. We would like to thank Dr. Sandeep Mannava for helpful clinical conversations.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rankine JJ. Adult traumatic brachial plexus injury. Clin Radiol. 2004;59:767–774. doi: 10.1016/j.crad.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 2.Venkatramani H, Bhardwaj P, Faruquee SR, Sabapathy SR. Functional outcome of nerve transfer for restoration of shoulder and elbow function in upper brachial plexus injury. J Brachial Plexus Periph Nerve Inj. 2008;3:15. doi: 10.1186/1749-7221-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bertelli JA, Ghizoni MF. Reconstruction of C5 and C6 Brachial Plexus Avulsion Injury by Multiple Nerve Transfers: Spinal Accessory to Suprascapular, Ulnar Fascicles to Biceps Branch, and Triceps Long or Lateral Head Branch to Axillary Nerve. J Hand Surg. 2004;29A:131–139. doi: 10.1016/j.jhsa.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 4.Merrell GA, Barrie KA, Katz DL, Wolfe SW. Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg. 2001;26:303–314. doi: 10.1053/jhsu.2001.21518. [DOI] [PubMed] [Google Scholar]
- 5.Terzis JK, Kostas I. Suprascapular Nerve Reconstruction in 118 Cases of Adult Posttraumatic Brachial Plexus. Plastic & Reconstr Surg. 2006;117:613–629. doi: 10.1097/01.prs.0000203410.35395.fa. [DOI] [PubMed] [Google Scholar]
- 6.Terzis JK, Barmpitsioti A. Axillary Nerve Reconstruction in 176 Posttraumatic Plexopathy Patients. Plastic & Reconstr Surg. 2010;125:233–247. doi: 10.1097/PRS.0b013e3181c496e4. [DOI] [PubMed] [Google Scholar]
- 7.Terzis JK, Vekris M, Soucacos P. Outcome of Brachial Plexus Reconstruction in 204 Patients with Devastating Paralysis. Plastic & Reconstr Surg. 1999;104:1221–1240. doi: 10.1097/00006534-199910000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Hollerbach JM, Flash T. Dynamic interactions between limb segments during planar arm movement. Biolog Cybernet. 1982;44:67–77. doi: 10.1007/BF00353957. [DOI] [PubMed] [Google Scholar]
- 9.Delp SL, Arnold AS, Piazza SJ. Graphics-based modeling and analysis of gait abnormalities. Biomed Mater Eng. 1998;8:227–240. [PubMed] [Google Scholar]
- 10.Rankin JW, Kwarciak AM, Richter WM, Neptune RR. The influence of altering push force effectiveness on upper extremity demand during wheelchair propulsion. J Biomech. 2010;43:2771–2779. doi: 10.1016/j.jbiomech.2010.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mogk JPM, Johanson ME, Hentz VR, Saul KR, Murray WM. A simulation analysis of the combined effects of muscle strength and surgical tensioning on lateral pinch force following brachioradialis to flexor pollicis longus transfer. J Biomech. 2011;44:669–675. doi: 10.1016/j.jbiomech.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holzbaur KRS, Murray WM, Delp SL. A Model of the Upper Extremity for Simulating Musculoskeletal Surgery and Analyzing Neuromuscular Control. Ann Biomed Eng. 2005;33:829–840. doi: 10.1007/s10439-005-3320-7. [DOI] [PubMed] [Google Scholar]
- 13.Daly M. Ph D dissertation. Wake Forest University Graduate School of Arts and Sciences; Winston-Salem, NC: 2011. Adaptations following upper extremity resistance training in older adults. [Google Scholar]
- 14.Delp SL, Anderson FC, Arnold AS, Loan P, Habib A, John CT, et al. OpenSim: Open-Source Software to Create and Analyze Dynamic Simulations of Movement. IEEE Trans Biomed Eng. 2007;54:1940–1950. doi: 10.1109/TBME.2007.901024. [DOI] [PubMed] [Google Scholar]
- 15.de Groot JH, Brand R. A three-dimensional regression model of the shoulder rhythm. Clin Biomech. 2001;16:735–743. doi: 10.1016/s0268-0033(01)00065-1. [DOI] [PubMed] [Google Scholar]
- 16.Lieber RL, Jacobson MD, Fazeli BM, Abrams RA, Botte MJ. Architecture of selected muscles of the arm and forearm: Anatomy and implications for tendon transfer. J Hand Surg. 1992;17:787–798. doi: 10.1016/0363-5023(92)90444-t. [DOI] [PubMed] [Google Scholar]
- 17.Murray WM, Buchanan TS, Delp SL. The isometric functional capacity of muscles that cross the elbow. J Biomech. 2000;33:943–952. doi: 10.1016/s0021-9290(00)00051-8. [DOI] [PubMed] [Google Scholar]
- 18.An KN, Hui FC, Morrey BF, Linscheid RL, Chao EY. Muscles across the elbow joint: A biomechanical analysis. J Biomech. 1981;14:659–669. doi: 10.1016/0021-9290(81)90048-8. [DOI] [PubMed] [Google Scholar]
- 19.Jacobson MD, Raab R, Fazeli BM, Abrams RA, Botte MJ, Lieber RL. Architectural design of the human intrinsic hand muscles. J Hand Surg. 1992;17:804–809. doi: 10.1016/0363-5023(92)90446-v. [DOI] [PubMed] [Google Scholar]
- 20.Lieber RL, Fazeli BM, Botte MJ. Architecture of selected wrist flexor and extensor muscles. J Hand Surg. 1990;15:244–250. doi: 10.1016/0363-5023(90)90103-x. [DOI] [PubMed] [Google Scholar]
- 21.Zajac FE. Muscle and tendon: properties, models, scaling, and application to biomechanics and motor control. Critical Rev Biomed Eng. 1989;17:359–411. [PubMed] [Google Scholar]
- 22.Goubier J-N, Teboul F. Technique of the Double Nerve Transfer to Recover Elbow Flexion in C5,C6 or C5 to C7 Brachial Plexus Palsy. Tech Hand Upper Extrem Surg. 2007;11:15–17. doi: 10.1097/01.bth.0000248360.14448.6b. [DOI] [PubMed] [Google Scholar]
- 23.Clare DJ, Wirth MA, Groh GI, Rockwood CA. Shoulder Arthrodesis. J Bone Joint Surg. 2001;83-A:593–600. doi: 10.2106/00004623-200104000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Thelen DG, Anderson FC. Using computed muscle control to generate forward dynamic simulations of human walking from experimental data. J Biomech. 2006;39:1107–1115. doi: 10.1016/j.jbiomech.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 25.Happee R. Inverse dynamic optimization including muscular dynamics, a new simulation method applied to goal directed movements. J Biomech. 1994;27:953–960. doi: 10.1016/0021-9290(94)90267-4. [DOI] [PubMed] [Google Scholar]
- 26.Bertelli JA, Ghizoni MF. Nerve Root Grafting and Distal Nerve Transfers for C5-C6 Brachial Plexus Injuries. J Hand Surg. 2010;35A:769–775. doi: 10.1016/j.jhsa.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Midha R. Nerve transfers for severe brachial plexus injuries: a review. Neurosurg Focus. 2004;16:E5. doi: 10.3171/foc.2004.16.5.6. [DOI] [PubMed] [Google Scholar]
- 28.Krishnan KG, Martin KD, Schackert G. Traumatic Lesions of the Brachial Plexus: An Analysis of Outcomes in Primary Brachial Plexus Reconstruction and Secondary Functional Arm Reanimation. Neurosurg. 2008;62 doi: 10.1227/01.neu.0000318173.28461.32. [DOI] [PubMed] [Google Scholar]
- 29.Gu Y-D, Cai P-Q, Xu F, Peng F, Chen L. Clinical application of ipsilateral C7 nerve root transfer for treatment of C5 and C6 avulsion of brachial plexus. Microsurg. 2003;23:105–108. doi: 10.1002/micr.10113. [DOI] [PubMed] [Google Scholar]
- 30.Bentolila V, Nizard R, Bizot P, Sedel L. Complete Traumatic Brachial Plexus Palsy Treatment and Outcome After Repair. J Bone Joint Surg. 1999;81:20–28. doi: 10.2106/00004623-199901000-00004. [DOI] [PubMed] [Google Scholar]
- 31.Magermans DG, Chadwick EKJ, Veeger HEJ, Helm FCTvd. Requirements for upper extremity motions during activities of daily living. Clin Biomech. 2005;20:591–599. doi: 10.1016/j.clinbiomech.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 32.Oberlin C, Durand S, Belheyar Z, Shafi M, David E, Asfazadourian H. Nerve transfers in brachial plexus palsies. Chirurgie de la Main. 2009;28:1–9. doi: 10.1016/j.main.2008.11.010. [DOI] [PubMed] [Google Scholar]


