Abstract
Investigations into the pathogenesis of type 2 diabetes and islets of Langerhans malfunction 1 have been hampered by the limited availability of type 2 diabetic islets from organ donors2. Here we share our protocol for isolating islets from human pancreatic tissue obtained from type 2 diabetic and non-diabetic patients who have undergone partial pancreatectomy due to different pancreatic diseases (benign or malignant pancreatic tumors, chronic pancreatitis, and common bile duct or duodenal tumors). All patients involved gave their consent to this study, which had also been approved by the local ethics committee. The surgical specimens were immediately delivered to the pathologist who selected soft and healthy appearing pancreatic tissue for islet isolation, retaining the damaged tissue for diagnostic purposes. We found that to isolate more than 1,000 islets, we had to begin with at least 2 g of pancreatic tissue. Also essential to our protocol was to visibly distend the tissue when injecting the enzyme-containing media and subsequently mince it to aid digestion by increasing the surface area.
To extend the applicability of our protocol to include the occasional case in which a large amount (>15g) of human pancreatic tissue is available , we used a Ricordi chamber (50 ml) to digest the tissue. During digestion, we manually shook the Ricordi chamber3 at an intensity that varied by specimen according to its level of tissue fibrosis. A discontinous Ficoll gradient was then used to separate the islets from acinar tissue. We noted that the tissue pellet should be small enough to be homogenously resuspended in Ficoll medium with a density of 1.125 g/ml. After isolation, we cultured the islets under stress free conditions (no shaking or rotation) with 5% CO2 at 37 °C for at least 48 h in order to facilitate their functional recovery. Widespread application of our protocol and its future improvement could enable the timely harvesting of large quantities of human islets from diabetic and clinically matched non-diabetic subjects, greatly advancing type 2 diabetes research.
Keywords: Medicine, Issue 53, human islets, Diabetes mellitus, partial pancreatectomy, human islet isolation
Protocol
1. Pancreatic tissue collection in the operating room
The surgeon performs a partial resection of the pancreas.
After placing the pancreatic specimen in a box on ice, deliver it immediately to the pathologist.
2. Tissue selection for islet isolation
The pathologist selects tissue that appears soft and healthy, retaining the damaged tissue for diagnostic purposes. Fibrotic tissue and specimens offering less than 2 g of usable tissue are excluded from islet isolation.
Immerse the pancreatic tissue in Euro Collins Solution and deliver on ice to the laboratory.
3. Isolation of human islets
Weigh the pancreatic tissue, then place it into a 10 cm dish.
Put 150 ml RPMI media in a 500 ml flask.
In a 250 ml flask, prepare the digestive enzyme solution by combining 130 ml RPMI media with 100 mg/ml DNase and 20 ml of 5mg/ml Liberase RI. Draw 10 ml of this solution into a syringe to inject the pancreatic tissue.
Inject the digestive enzyme solution into the pancreatic tissue, aiming to distend it homogeneously. If this is prevented by fibrosis, the digestion will likely fail. Next, mince the tissue into ~4 mm3 pieces on ice.
4. Human pancreas digestion circuit
Assemble the digestion circuit as shown in Figure 1. The flow direction in the Ricordi chamber is in at the bottom and out at the top of the chamber.
Add the remaining digestive enzyme solution to the 500 ml flask up to a total volume of 300 ml and insert a thermometer.
Transfer the pancreatic tissue into the chamber, insert the mesh (pore diameter: 600 μm) and three Silicon Nitride Marbles (diameter: 15 mm), close the chamber and start the pump with the flow set at 140 ml/min.
When the temperature of the circuit reaches 37 °C, start timing and periodically take samples to determine when to stop the digestion. Staining with dithizone (2 mg/ml) allows microscopic visualization of islets within the digested tissue4.
Once the islets are separated from the surrounding acinar tissue, quickly stop the digestion by placing the heating coil on ice and adding 200 ml of cold wash media (900 ml RPMI 1640 with 5.5 mM glucose and 10% FBS) to the circuit.
Collect the islet solution in 250 ml conical tubes as it comes out of the sample tube. Continue until the circuit is empty.
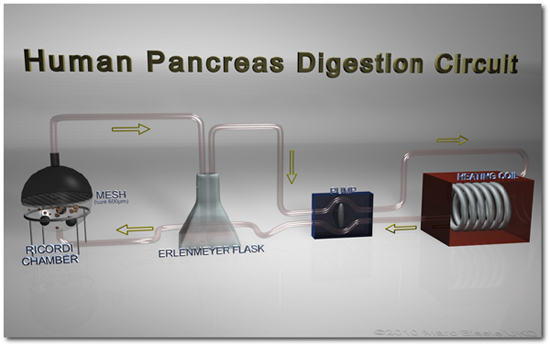 Figure 1. The human pancreas digestion circuit The human pancreas digestion circuit includes a Ricordi chamber containing mesh (pore diameter: 600 μm) and three silicon nitride marbles (diameter: 15 mm). Outflow from the chamber is driven to the tissue collection flask by the peristaltic pump (140 ml/min). Arrows indicate the flow direction. An optimal temperature for enzymatic digestion is maintained by immersing the heating coil in a 37 °C water bath.
Figure 1. The human pancreas digestion circuit The human pancreas digestion circuit includes a Ricordi chamber containing mesh (pore diameter: 600 μm) and three silicon nitride marbles (diameter: 15 mm). Outflow from the chamber is driven to the tissue collection flask by the peristaltic pump (140 ml/min). Arrows indicate the flow direction. An optimal temperature for enzymatic digestion is maintained by immersing the heating coil in a 37 °C water bath.
5. Washing post-digestion
Centrifuge the 250 ml conical tubes containing the islet solution at 1000 rpm, 4 °C for 5 min.
Discard the supernatant, resuspend the islet pellet in wash media (900 ml RPMI 1640 with 5.5 mM glucose and 10% FBS) and distribute it in equal fractions to 50 ml conical tubes. (Optional: Distribute into additional conical tubes to improve washing.) Centrifuge at 1000 rpm, 4 °C for 5 min.
Discard supernatant and gently loosen pellets by manual shaking.
6. Purification on a Ficoll gradient
Resuspend the pellet with Ficoll media at a density of 1.125 g/ml, pH 7.4 and slowly overlay 10 ml aliquots of Ficoll media with densities of 1.080, 1.060 and 1.037 g/ml.
Centrifuge the Ficoll gradients at 2400 rpm, 4°C for 20 min.
7. Islet Collection and Culture
After centrifugation, different tissue components can be distinguished by their partitioning in the gradient.
Discard the upper layer consisting of fat and connective tissue.
Carefully harvest the first layer of islet aggregates at the 1.037-1.060 g/ml interphase. This layer contains the most pure isolated islets. Collect fractions separately for efficient isolation.
Collect the second, less pure fraction of islet aggregates at the 1.060-1.080 g/ml interphase.
Dilute the Ficoll gradient by adding wash media (900 ml RPMI 1640 with 5.5 mM glucose and 10% FBS) to each conical tube up to a total volume of 50 ml. Centrifuge at 1000 rpm, 4°C for 5 min.
Discard the supernatant by suction. Use care as the pellet might be loose due to the Ficoll gradient.
Wash the pellets with wash media (900ml RPMI 1640 with 5.5 mM glucose and 10% FBS) and centrifuge at 1000 rpm, 4°C for 5 min. Repeat using islet culture media
Resuspend the islets in culture media and place them in the incubator with 5% CO2 at 37 °C for 24-48 hours before further processing.
Representative Results
Our protocol yielded an average of ~500 islets per gram of pancreatic tissue, although this greatly varied between preparations due largely to differences in fibrosis and collagenase activity. We achieved > 90% islet purity by first staining with Dithizone during tissue processing, then handpicking them 24 hours after isolation. To determine the quality of the purified islets, we tested for 25 mM glucose-stimulated insulin secretion under static conditions for 2 hours. We found insulin secretion comparable to that of islets obtained from ECIT islet isolation and transplantation centers. As islets isolated from partially pancreatectomized pancreata are not meant for islet transplantation, assessment of the total IEQ was not considered to be a critical factor.
Importantly, our method enabled us to isolate islets for functional studies from 25 partial pancreatectomized patients between 2005 and 20085. These islets were analyzed for glucose-stimulated insulin secretion and specific protein expression by western blotting and immunohistochemistry. Islets isolated from partially pancreatecomized pancreata could also be used to compare gene and protein expression profiles, ultrastructural appearance and functional responses of non-diabetic and diabetic islets. Because there are more patients undergoing partial pancreatectomy than there are organ donors, our protocol could allow enough samples and data to be collected for robust statistical analysis.
Discussion
Using our protocol, human islets can be isolated from pancreatic tissue collected from a partial pancreatectomy. The success of this protocol relies on the care taken during a few critical points. To preserve beta-cell viability, it is essential that the specimen be transported rapidly on ice to the laboratory. Additionally, the duration of tissue digestion must be optimized empirically according to the grade of tissue fibrosis and the enzymatic activity of the media. This is also true for the degree of mechanical force applied manually to the Ricordi chamber. Thus to obtain a good islet yield, the protocol is best performed by a dedicated scientist or technical assistant. Initial failure is the norm unless the team is already experienced in islet isolation.
There are key differences between our islet isolation protocol and the standard human islet isolation method: 1) Although we use pancreatic tissue subjected to several hours of ischemia during the surgical procedure, it is immediately processed on site. This is in contrast to pancreata explanted from brain-dead donors for pancreas/islet transplantation, which remain ischemic for several hours during allocation and delivery to the islet isolation facility. 2) We inject collagenase directly into the pancreatic tissue, whereas the standard protocol is to infuse it into the pancreatic duct. 3) We separate the islets using a discontinuous Ficoll gradient instead of collecting the islets from a continuous Ficoll gradient using a COBE cell processor.
In cases where the surgical specimen is too fibrotic or scarce for isolating an adequate number of islets, tissue can still be retrieved by laser capture microdissection (LCM)10. This allows gene expression data to be recovered from virtually every specimen, even if the islet isolation fails or the yield is very low. Unfortunately, LCM does not produce living cells for functional studies and their amount is typically insufficient for proteomic analysis. Thus, using LCM in parallel with our collagenase digestion protocol to retrieve the islets may be the most effective way to process surgical specimens.
When collecting tissue for islet isolation from partial pancreatectomies, it is important to carefully examine the patient’s clinical history and metabolic state. A partially pancreatectomized patient could be affected by type 3c diabetes, i.e. diabetes secondary to the pancreatic disorder leading to surgery6. Among the 43 participating patients who underwent this surgery in our department in 2010, 32 were non-diabetic, 5 were affected by type 2 diabetes and 6 had type 3c diabetes. These data agree with previous studies pointing to impaired glucose metabolism and diabetes in a sizeable fraction of patients suffering from pancreatic cancer or chronic pancreatitis6. We considered diabetes to be of primary origin if it was diagnosed at least one year prior to the onset of symptoms leading to pancreatic surgery7. The levels of antibodies against islet autoantigens should also be measured to evaluate a potential autoimmune origin of the diabetes8. Because a patient undergoing pancreatectomy could suffer from undiagnosed diabetes or be glucose intolerant, all non-diabetic patients should be given an oral glucose tolerance test prior to the pancreatectomy9.
Disclosures
No conflicts of interest declared.
Acknowledgments
We want to thank our many colleagues who provided help, advice and critical input at various stages of the project. Production of this video article was supported with funds from the German Ministry for Education and Research (BMBF) to the German Centre for Diabetes Research (DZD, http://www.dzd-ev.de), IMIDIA (http://www.imidia.org) and the University Hospital Carl Gustav Carus at the University of Technology Dresden. The research leading to these results has received funding from the European Community's Seventh Framework Programme (FP7/2007-2013) for the Innovative Medicine Initiative under grant agreement n° 115005.
References
- Kahn SE, Zraika S, Utzschneider KM, Hull RL. The beta cell lesion in type 2 diabetes: there has to be a primary functional abnormality. Diabetologia. 2009;52:1003–1012. doi: 10.1007/s00125-009-1321-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deng S, Vatamaniuk M, Huang X, Doliba N, Lian MM, Frank A, Velidedeoglu E, Desai NM, Koeberlein B, Wolf B, Barker CF, Naji A, Matschinsky FM, Markmann JF. Structural and functional abnormalities in the islets isolated from type 2 diabetic subjects. Diabetes. 2004;53:624–632. doi: 10.2337/diabetes.53.3.624. [DOI] [PubMed] [Google Scholar]
- Ricordi C, Lacy PE, Finke EH, Olack BJ, Scharp DW. Automated method for isolation of human pancreatic islets. Diabetes. 1988;37:413–420. doi: 10.2337/diab.37.4.413. [DOI] [PubMed] [Google Scholar]
- Latif ZA, Noel J, Alejandro R. A simple method of staining fresh and cultured islets. Transplantation. 1988;45:827–830. [PubMed] [Google Scholar]
- Ehehalt F, Knoch K, Erdmann K, Krautz C, Jäger M, Steffen A, Wegbrod C, Meisterfeld R, Kersting S, Bergert H, Kuhlisch E, Bornstein S, Bonifacio E, Saeger HD, Solimena M. Impaired insulin turnover in islets from type 2 diabetic patients. Islets. 2010;2:30–36. doi: 10.4161/isl.2.1.10098. [DOI] [PubMed] [Google Scholar]
- Hardt PD, Brendel MD, Kloer HU, Bretzel RG. Is pancreatic diabetes (type 3c diabetes) underdiagnosed and misdiagnosed? Diabetes Care. 2008;31(Suppl 2):S165–S169. doi: 10.2337/dc08-s244. [DOI] [PubMed] [Google Scholar]
- Meisterfeld R, Ehehalt F, Saeger HD, Solimena M. Pancreatic disorders and diabetes mellitus. Exp Clin Endocrinol Diabetes. 2008;116(Suppl 1):S7–S12. doi: 10.1055/s-2008-1080918. [DOI] [PubMed] [Google Scholar]
- Verge CF, Gianani R, Kawasaki E, Yu L, Pietropaolo M, Jackson RA, Chase HP, Eisenbarth GS. Prediction of type I diabetes in first-degree relatives using a combination of insulin, GAD, and ICA512bdc/IA-2 autoantibodies. Diabetes. 1996;45:926–933. doi: 10.2337/diab.45.7.926. [DOI] [PubMed] [Google Scholar]
- Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- Marselli L, Thorne J, Ahn YB, Omer A. Gene Expression of Purified {beta}-Cell Tissue Obtained from Human Pancreas with Laser Capture Microdissection. Journal of Clin. Endocrinol. Metab. 2008;93:1046–1053. doi: 10.1210/jc.2007-0931. [DOI] [PMC free article] [PubMed] [Google Scholar]


