Abstract
This report describes four diverse programs of community‐engaged research, all of which demonstrated positive health outcomes. Three of the programs were focused on communities of people with diabetes, and one program targeted at‐risk young families raising infants and young children. Brief descriptions of each research study and outcomes are presented as well as a discussion of the processes and lessons that were learned from each model of successful interdisciplinary community‐university health research partnerships. Clin Trans Sci 2011; Volume 4: 285–297
Keywords: community health research, community‐based participatory research, community health partnerships
Introduction
To meet the healthcare demands of the 21st century, the National Institutes of Health (NIH) Roadmap calls for reengineering the nation’s Clinical Research Enterprise to accelerate advancement of medical discoveries to improve human health. 1 , 2 The advancement of promising medical discoveries into clinical practice is inefficient, with estimates suggesting an average 17‐year time lag for 14% of research to be translated into clinical practice, thereby requiring new approaches to clinical validation of research findings. 3 In 2006, to accelerate scientific advancement, while appreciating its tremendous complexities, the NIH launched the growing Clinical and Translational Science Awards (CTSA) Consortium to foster the growth of a new multi‐ and interdisciplinary science, the Discipline of Clinical and Translational Science, with a scope and depth exceeding that of the traditional, separate domains of translational and clinical research. 1 , 2
In May of 2010, the National Center for Research Resources (NCRR) sponsored a conference, Partnering to Improve Health: The Science of Community Engagement, with the purpose of examining and discussing the science of community‐engaged research. This paper originated from the conference panel sessions in which four nurse scientists, all working at CTSA‐funded sites, presented their research programs as exemplars of community‐engaged research demonstrating important health outcomes.
The discipline of Clinical and Translational Science is rooted in translational research. According to the NIH, translational research refers to a bidirectional, incremental process wherein scientific discoveries generated at the “bench” are transferred to the “bedside” or clinical level with practical applications to optimize or improve human health. 2 Following this model, the process of advancing translational research is complex with two vitally important broad steps necessary for its success. The two translational steps may be conceptualized as bridging upstream‐to‐midstream and midstream‐to‐downstream junctures of knowledge development and uptake to advance the flow and transfer of knowledge from basic science, to human clinical research, and ultimately to clinical practice, respectively. While each translational step or bridge engages bidirectionally with respective junctures in the flow of research knowledge, the overall movement of the current is one aimed at step‐wise progression toward downstream translation of science to improve human health. 4
The first translational step or T1 originates at the “bench” with the generation of molecular or cellular discoveries. From this juncture, T1 involves case series and both Phase I and Phase II Clinical Trials to move upstream or cutting‐edge “bench” discoveries midstream for application at the “bedside” with human clinical research or efficacy trials, which involves Phase III Clinical Trials in ideal, controlled settings. The second translational step or T2 follows, bridging knowledge transfer from clinical research to practice or from midstream‐to‐downstream in uncontrolled settings. T2 traditionally involves effectiveness trials and dissemination research with related research dissemination through professional journals, education, meetings, and clinical guidelines. 4 , 5 , 6 However, effective translation downstream has been limited with only modest uptake or adoption to benefit clinic and other community‐based populations, suggesting standard T2 translational methods may be lacking. This has prompted increased recognition that T2 efforts require greater commitment with incorporation of diverse methods while others contend a third translational step or T3 is necessary with a focus on community‐based participatory research (CBPR), for example, to foster successful adoption of scientific knowledge or interventions in “real world settings.” 4 , 5 , 7 CBPR is an approach to health‐related research, as opposed to a specific methodology, that aims to develop, foster, and sustain collaborative partnerships between researchers and communities, including members most affected by the problem, to improve or ameliorate local public health problems. 8 Following this orientation, researchers bring scientific knowledge and skills to the partnership while communities bring local or often cultural expertise, knowledge, skills, and resources. This partnership approach contrasts with traditional research study designs for clinical trials in which researchers direct the study, operate in a unilateral mode, and have much less participant input into the design and conduct of the study protocol. The two contrasting approaches each have costs and benefits. Traditional clinical trials have much less flexibility and produce findings under more controlled conditions with the expectation of generalizability of the findings. 9 , 10 Within CBPR, through power sharing, bidirectional communication and joint decision making throughout the research process, researchers and communities ensure research is conducted with rather than for a community, fostering an equitable partnership. The power‐sharing process fosters mutual learning and trust with scientifically grounded, locally relevant research results. The codeveloped knowledge, both acceptable and applicable to the community, is thereby well poised for local adoption or uptake. 11 Hence, the CBPR approach, engaging communities throughout the research process, serves as a promising orientation to effectively advance the downstream adoption of midstream scientific advances or interventions that may otherwise get lost in translation, as well as to increase the potential for sustainability of the advances or interventions over time. 12 The term, community, may include both structured groups that have internal structures, evidence of leadership roles, and are sustained over time such as geopolitical communities, community social service agencies or religious groups, as well as unstructured groups that are defined by shared traits or characteristics, such as people with a shared ethnic or racial background or people who experience a common chronic illness or condition. 13 , 14 , 15
Research that takes place in community settings often reflects a spectrum of collaboration and participation, that is broadly referred to by NIH as community‐engaged research. 2 , 10 , 13 The spectrum varies from research that simply includes samples of subjects recruited from various community settings, to various formal and informal research partnerships that evolve between researchers and community members, to the use of the specific principles of CBPR. 8 , 9 , 10 , 16 Community‐engaged research, with attention to CBPR, is recognized as critical to the success of the CTSA’s culture of translational healthcare research. 17 Within each CTSA program, there is a Community Engagement and Research Core, which focuses on establishing productive and collaborative health research relationships among university researchers, community agency partners, and community leaders, members, and consumers for the development and implementation of community‐engaged translational health research. Principles of CBPR inform this work, and strengthen the reciprocal nature of discovery and application of evidence‐based practice to healthcare.
Academic nurse scientists and nursing educators share a history of integrating community‐based teaching, service, and research, working toward improvements in community health and elimination of health disparities. 18 , 19 Academic researchers and community health agencies and partners represent institutions with different missions reflecting a primary emphasis on science or service, which can present challenges to collaborative partnerships. 20 , 21 Nurse scientists may have an advantage in helping to understand and bridge these two different but overlapping agendas since nurses have been practicing public health nursing and working to improve the health of communities, since the time of Florence Nightingale. 22 , 23 Nurses, as well as other healthcare professionals such as pharmacists, social workers, primary care physicians, and health educators, often practice and work within community settings, building relationships, establishing trust, and providing clinical service. 10 , 24 The clinical principles and approaches for working within and across communities inform research teams as they establish community‐engaged health research partnerships that are reciprocal and able to be sustained beyond the completion of one or two studies.
Exemplar Studies
The following studies are presented as exemplars of interdisciplinary community‐engaged health research, demonstrating positive health outcomes. Within the exemplar studies, the nurse scientists collaborated with interdisciplinary teams including community members and healthcare agencies, as well as medical, clergy, social work, nutritionist, pharmacist, and psychology colleagues. Each exemplar study had a unique study design and used specific engagement and recruitment methods that were developed to match the preference of the communities and settings. The research settings were varied and included differing degrees of community involvement and creative methods of problem identification and problem solving.
Kelley Newlin, DNSc, ARNP‐C, CDE—Diabetes: Faith‐Based Partnerships to Foster Community Intervention Translation. This program of research represents three related studies in which the researcher employed mixed methods research designs, and engaged faith‐based African American and Latino communities in Nicaragua, Florida, and New York for assessment and development of community‐specific translation of diabetes self‐care management strategies.
The three studies assessing and designing community‐specific strategies to improve self‐management among individuals with type 2 diabetes (T2D) addressed the issue of community engagement through creative approaches with local mass media and involvement of faith‐based communities. These approaches included key elements of pastor endorsement of the studies and centering the work within church‐based study locations. The research team identified the larger problem of diabetes with qualitative findings identifying community needs, preferences, and strategies for partnering in the development and implementation of faith‐based, diabetes self‐management programs. Furthermore, quantitative findings included healthcare patterns, diabetes knowledge, physical activity and nutritional practices, and physiological outcomes, such as glycemic and blood pressure control.
Collaborating with faith‐based communities, including distant sites in Nicaragua, is facilitated by partnering with church‐based nurses, who play a critical role in designing the intervention components to match the needs of the local parishioners and Ministry of Health. Partnering with Nicaraguan church‐based nurses, the principal investigator and team provide ongoing training in research ethics and evidence‐based diabetes care and education through site visits, weekly e‐mail, and more recently, Skype. Program goals are mutually identified, with strategies refined and translated into community settings by the church‐based nurses, including feedback from parishioners and the Ministry of Health. Collaborating with church‐based communities is maximized by identification of unique strengths across the partnership to inform research program responsibilities. Challenges with international collaborative program planning and implementation include consultation for emergent issues that is limited to telephone or electronic communication as opposed to on‐site or face‐to‐face collective problem solving.
Lois S. Sadler, PhD, PNP‐BC, FAAN—Community‐University Partnerships in Community‐Engaged Health Research: The Minding the Baby Home Visiting Program. This ongoing research is located in New Haven, Connecticut and involves the development and evaluation of a preventive home visiting intervention for young at‐risk urban families as they prepare and learn to care for a first‐born child. The study is conducted in close collaboration with two Community Health Centers (CHC). In the Minding the Baby program, research was built into the practice model from the very beginning of the project. The clinical problem identification primarily originated with a key group of CHC midwifery and pediatric clinicians who determined that their usual methods of providing prenatal, pediatric, and primary healthcare needed supplementation for many of the very young and at‐risk families they served in their lowincome community. The study used a CBPR model and adhered to ethical principles of community‐engaged research that were developed for use within university‐community partnerships (http://ycci.yale.edu/resources/docs/PrinciplesforU‐CPs_001.pdf). The primary community partners initially included the CHC clinicians who identified the problem, and also eventually included (downstream) the families who lived in the community served by the CHC. “Graduated families” of the program serve as consultants by providing their evaluation and suggestions to program staff.
The study included an innovative home visiting intervention compared with the usual standard of healthcare provided to the community by the CHC clinicians. The issue of conducting a randomized clinical trial (RCT) for testing this home visiting approach was introduced in discussions among researchers and community partners early in the planning stages. The relative benefits of using an RCT model were presented: testing to see what works and what does not; future funding opportunities; ongoing development; and strengthening of the approaches. In contrast were the community clinicians’ perceptions of the difficulties with the RCT model: the desire to have every eligible family receive the innovative intervention; the additional work of explaining the control condition to CHC staff and clinicians; the additional work in following a randomization scheme for recruitment of families into the project. Ultimately, the benefits were seen to outweigh the problems. However, ongoing explanations and support for the RCT model were provided by the research team as CHC staff changed.
The support of the approach by the executive director and key leadership members of the CHC staff was essential to the success of implementing the RCT approach. Relationship building and mutual respect was established from the first meeting. The measurable health outcomes shared with the CHC clinicians, as well as their anecdotal reports of the benefits that they saw in intervention families helped to continue the positive relationships. A measure of the trust and respectful partnership that has been established, is seen in the “process outcome” of clinicians continuing to support the work, be enthusiastic about the program with colleagues and patients, and participate in the research over several years. Research findings are shared with CHC staff through regular posters and presentations, and with graduated families through newsletters and reunion outings.
Ida J. Spruill, PhD, RN, LISW—Project SuGar (Sea Islands Genetic African‐American Registry). This study was conducted among African‐American families residing on the Sea Islands of South Carolina and interested in the genetic basis of T2D among Gullah families. The study created a registry and DNA bank of 650 African‐American families affected with T2D with guidance from the Citizen Advisory Committee, which was organized at the inception of the project and continues to meet quarterly. A core value of the project was the provision of tangible benefits to the community.
The cultural and genetic characteristics of the Gullah population of South Carolina provided a unique opportunity to conduct a genetic study with a community of people where mutual trust and respect needed to be established among scientists and community members. The Gullahs are direct descendants of enslaved Africans brought to this country to work on plantations. As a community‐based genetic research study, the researchers were interested in locating and isolating genes responsible for the expression of diabetes and obesity among the Sea Islanders of South Carolina.
An important element realized in the success of this project, is that an appreciation of cultural elements (beliefs, attitudes, and life experiences) should be a prerequisite to understanding patterns of behaviors for effective recruitment. African American families can be successfully recruited and do participate in genetic research as evidenced by Project SuGar recruitment success among the Gullah population of South Carolina. Strategies included the organization of a community advisory committee, matching the ethnicity of the study population with the research team, providing a tangible benefit to the community and approaching the community in a slow, kind, and respectful manner. The research team also assisted the communities to identify priorities for learning about diabetes and prevention of complications not only for the participant but also for future generations.
Over the course of the project, the research team recognized several key elements of the work within the community that shaped the conduct and success of the study. These included recognizing that: (1) cultural heterogeneity exists within the African American population, and beliefs are shaped by geographical/ancestral origins; (2) the church has multiple roles including providing social support and education, acting as a community resource and linkage to other resources, and promoting social justice; (3) nonbiological family members or “fictive kin” are ascribed social roles and accepted as members of the biological family; therefore the influence of their role should not be excluded when providing education; (4) the need to understand the importance of nontraditional family styles in decision making as families share more than genes; (5) continued, ongoing community engagement is critical for long‐term relationships; and (6) the formation of a community advisory council (CAC) or community advisory board is fundamental and must include broad community representation.
This understanding was essential to the success as the study unfolded, especially when the community‐based data collection identified diabetes quality of care and self‐management as suboptimal among the Gullah population. However, the mobile SuGar bus allowed the study personnel to work within the community to address some of the diabetes management needs across multiple community recruitment sites. To encourage participation in the research with optimal enrollment, the research team and CAC developed the Community, Plan, and Reward Recruitment Model (CPR). The core value within this model was “coordinated research (work within existing community structure/organizations).” The CPR model is composed of three components: (1) community engagement, (2) flexible recruitment plan and protocol, and (3) tangible benefits to the community.
Carolyn Jenkins, DrPH, APRN‐BC, LD, RD, FAAN—REACH Charleston and Georgetown Diabetes Coalition: Decreasing Disparities in Diabetes‐Related Amputations in African Americans. This program of research, focused on decreasing disparities, is located in two counties in coastal South Carolina, includes three coalitions composed of many community groups and healthcare systems, and is focused on integrating findings into public health practice. The emphasis of this study and public health program was to assess, plan, intervene, and evaluate a community‐wide effort to improve diabetes‐related health disparities. One of the foci was to reduce lower limb amputations among African‐American individuals with diabetes living in the two counties. Diabetes‐related amputations were identified as one of the health disparities by members of the community coalitions. Funding for the program came primarily from Centers for Disease Control and Prevention (CDC) as well as funding for community member interviews from NIH‐National Institute of Nursing Research (NINR).
The REACH project was based on coalition theory, 18 which brought researchers, healthcare organizations, diverse community leaders and organizations, as well as grassroots community activists to work together to address diabetes disparities in African‐American communities within two counties (one rural and one urban) in South Carolina. 25 Intersectoral actions fostered successful assessment of community assets, needs and recruitment where people live, worship, work, and seek healthcare. 26 In collaboration with the researchers, the Coalition leaders recruited, interviewed, and recommended hiring of the community health workers, who preferred to be called Community Health Advocates (CHAs). The CHAs and the research team developed and implemented community interventions for more than 11,000 persons with diabetes. The interventions were guided by the Charleston and Georgetown Diabetes Coalition. The research focused on diabetes management issues including: prevention of complications, identifying and activating community assets for addressing disparities, improving the standards of care and management, and on measuring the effectiveness of broad‐based interventions at the community, health systems, and coalition levels that influenced or were associated with system and community‐wide changes. Both the qualitative and quantitative findings revealed the context and degree of specific diabetes‐related problems affecting the community; in particular, the many devastating outcomes, including lower limb amputation. This study was unique by translating the local findings to community and state policy levels and addressing health policy changes specific to diabetes care leading to the significant reduction of amputations among African Americans living within the communities. The program is now working with 10 community coalitions across the Southeastern United States to decrease diabetes disparities in African American communities.
Table 1 contains brief descriptions of the six exemplar studies including a summary of their health outcomes.
Table 1.
Overview of study designs.
| Study, funding source, and PI | Study design | Theoretical framework(s) | Specific aims/objectives | Population, participants, and health issue | Interventions | Health outcomes |
|---|---|---|---|---|---|---|
| PI: L. Sadler Minding the Baby: A Home Visiting Program for Young Families 38 , 39 | Experimental—Phase II pilot study with cluster randomization by prenatal care groups from local community health centers (CHC) | Attachment & reflective functioning theories; social ecology theory | 1. Test effects of MTB home visiting versus control condition with respect to maternal health & life course outcomes (delaying rapid subsequent childbearing); maternal reflective functioning; child health & attachment outcomes; rates of child abuse/neglect | Eligibility criteria: women attending group‐based prenatal care at CHC; having first child; English speaking; no drug use (CHC screens all prenatal pts.) or major psychosis or terminal illness; ages 14–26 | MTB home visiting program based on: (a) evidence‐based home visiting models 40 & (b) emerging neuroscience of early parenting 41 with innovative additions including home‐based mental health treatment & focus on reflective parenting 38 , 42 | Preliminary pilot study outcomes in MTB families compared with control families: |
| Funded by NINR, NICHD, & following foundations: Harris, AE Casey, Donaghue, Pritzker, Seedlings, Schneider, Edlow, & FAR Fund. | Intervention group—usual prenatal, pediatric, and primary healthcare at CHCs & weekly home visits 3rd trimester of pregnancy through 1st birthday‐weekly visits with NP & SW; biweekly visits during 2nd year. Control group—usual healthcare at CHCs & monthly educational materials, & holiday cards | Framework for community engagement—CBPR & Ethical Principles and Guidelines for Community‐University Research Partnerships | 2. Monitor fidelity of intervention | Control group = 43 mother‐child dyads | Joint training & supervision of NPs & SWs. Manualized treatment flexible & individualized including supplemental curricula. Program maximizes interdisciplinary team & expertise of NPs & SWs | ‐fewer child abuse referrals; |
| Intervention group = 64 dyads | ‐better compliance with pediatric immunizations & visits; | |||||
| 60% of sample = adolescent mothers | ‐less rapid subsequent childbearing; | |||||
| ‐children with more secure attachment & less disorganized attachment | ||||||
| Additional data analysis in process | ||||||
| PI: K. Newlin | Longitudinal, qualitative focus group interviewing with inquiry group method 43 | National Black Nurses’ Association Community Collaboration Model 44 | Explore faith community values, disease threat, benefits & barriers to self‐care health behavior, & community‐based actions about diabetes among Black American faith community stakeholders | Population: Faith communities with or at‐risk for T2D including diverse Black American ethnicities (Nicaraguan, Haitian, & African American) Eligibility criteria: Church member, leader, or nurse; English‐speaking; aged ≥21 years; with or at‐risk T2D. Sample size: N= 96 in 5 churches | Based on findings, community diabetes programs were developed & implemented in coordination with church nurses &/or young professionals | Analysis ongoing |
| 1. Study Title: Faith Communities & Black Women with Type 2 Diabetes | Unit of analyses: (1) church; (2) individual | |||||
| Funding period: 2006–2009. Funding: NIH F32 | ||||||
| 2. Study Title: Church‐Based Diabetes Education in Nicaragua | 4‐Stage Study | CBPR model augmented by work of Springer 45 , 46 | Stage 4: | Population: Creole & Miskito Indian adults with or at‐risk T2D | Stage 1: Public service announcements, church‐based screening, & standard diabetes education provided as service to communities | Stage 1 & 2 |
| Funding period: | Stage 1: Community dialogues | (1) Test the efficacy of church‐based diabetes prevention & self‐management care & education in adults with or at‐risk for T2D | Stage 1 Eligibility criteria: Community members, leaders, & health professionals | Stage 2 &3: Same as stage 1 | Barriers to care: Limited access to healthy foods, medications, & blood glucose testing supplies. | |
| Health beliefs about use of medications | ||||||
| 2008–2011 | Stage 2: Qualitative—focus groups | (2) Examine feasibility of implementation of intensive lifestyle intervention in faith‐based setting | Sample N= 106 community members from 3 Nicaraguan coastal towns | Stage 4: | Facilitators of care: Free access to primary care, committed physicians, nurses, & church leaders. Positive spiritual beliefs supporting daily self‐care. | |
| Funding: Private donations; NIH T32; NYU College of Nursing‐Sponsored Research Award; NYU Global Health Challenge Grant | Stage 3: Quantitative—cross‐sectional, survey | Stage 2 Eligibility criteria: English‐speaking, aged ≥21 years, local nurse or physician, church leader, or lay community member self‐identified with or at‐risk T2D | (1) Intervention translates evidence‐based standards of diabetes self‐management education & components of Diabetes Prevention Program for low‐income Nicaraguan communities | Community goals: | ||
| Stage 4: One‐group pretest‐posttest design | Sample N= 39 (participants); N= 4 (churches) | (2) Training church‐based nurses in intervention, data collection, & management & ethical conduct of research | Church‐based diabetes prevention & education led by nurses & community health workers under direction of physicians 47 , 48 | |||
| Stage 3 Eligibility criteria: English‐speaking, aged ≥21 years, self‐identified with or at‐risk T2D | (3) (a) Manualized intervention delivered by church‐based nurses tailored to individual & contextual factors and (b) Church‐based intervention delivered in one‐to‐one and group formats with weekly coaching visits and case management | Stage 3: | ||||
| Sample: N= 112 (participants); N= 4 (churches) | 62.5% subjects with T2D: Poor glycemic control, obesity, hypertension 37.5% subjects at‐risk for T2D: Obesity & elevated body mass index (BMI) 47 | |||||
| Stage 4 Eligibility criteria: English‐speaking, aged ≥21 years, self‐identified with or at‐risk T2D | Stage 4: | |||||
| Sample size (projected power analysis): N= 40 (participants); N= 1 (church) | Physiological outcomes: A1c, lipid, & blood pressure (BP) levels; psychosocial outcomes: depression & quality of life; process outcomes; | |||||
| Analysis in process | ||||||
| 3. Study Title: Translating the Diabetes Prevention Program and Diabetes Self‐Management Education into aBlack American Faith‐Based Setting | One‐group pretest‐posttest design | RE‐AIM 49 | (1) Examine the effect of a diabetes lifestyle intervention on physiological (blood glucose, HbA1c, & lipid levels in addition to BMI & BP), diabetes knowledge, & psychosocial (quality of life, depression, & diabetes risk perception) outcomes in Black women at‐risk or with T2D; (2) Examine feasibility of implementation of intensive lifestyle intervention in faith‐based setting on participation, attrition, satisfaction, & intervention fidelity | Population: Black American women with or at‐risk for T2D (church nurses requested study be limited to female adults with or at‐risk for T2D) | Intervention same as described in stage 4 above but tailored to specific individuals & community contexts | (1) Physiological outcomes: A1c, lipid, & BP levels; (2) Psychosocial outcomes: depression & quality of life; and (3) Process outcomes |
| Funding period: 2010–2012 | Eligibility criteria: church member; female; English‐speaking; aged ≥21 years; self‐identified as with or at‐risk T2D (e.g., family history, ethnicity, obesity, advancing age) | Analysis in process | ||||
| Funding: NIH KL2 | Sample size projected, based on power analysis: N= 40 (participants); N= 1 (church) | |||||
| PI: T. Garvey | Mixed methods | Community empowerment | Goal: Create a registry of 400 African American families affected with T2D, | African American families born or raised on the Sea Islands with T2D. | First 12 months—conducted community assessment, hired & trained staff/ volunteers, obtained formalized agreements with Federal Qualified CHC | Results from linkage analysis—novel T2D locus in an African‐American population on 14q that appears to reduce age of disease onset; confirmed two loci on chromosome. 7 53 |
| Coinvestigator: I. Spruill | Nonexperiential design | Community‐based—Participatory Model | Aims | Enrolled 672 African American families | Identified formal & informal leaders & organized CAC, which has met quarterly since inception | Created registry & DNA bank of 652 African American families affected with T2DM |
| Project SuGar Sea Islands of South Carolina 50 | Genetic linkage analysis | CBPR | 1) Ascertain sib‐pairs and pedigrees with T2DM, obesity, | Sea Island families received suboptimal diabetes care 51 , 52 | Project Sugar mobile health unit provided free diabetes screenings & education to over 7,000 residents of the Low Country | Implications for personalized medicine, and cultural specific educational interventions. Documented that Gullah families participating in study received suboptimal diabetes care 51 . Genome‐wide Association study (GWAS) not yet completed. |
| Funded by NIH/NIDDK, ADA,W.M. Keck Foundation | GWAS | “Coordinated research” | 2) Study genes contributing to diabetes and obesity | Quarterly Newsletter to research participants | ||
| Recruitment model used principles from CBPR with input from CAC and was called, CPR, community, plan, rewards (community involvement, flexible protocol plan, and rewards to the community) | 3) Community engagement strategies, provide tangible benefits, organize a Citizen Advisory Committee | |||||
| PI: C. Jenkins | Longitudinal case study of 2 counties’ efforts to decrease disparities 54 | Expanded Chronic Care Model for interventions 55 | Improve diabetes and foot care by 3% annually for African Americans with diabetes across 5 health systems | African Americans with diagnosed diabetes (and significant others) living in 2 counties | Community‐driven educational activities & creation of healthy learning environments where people live, work, worship, play, & seek healthcare 56 | County‐wide reduction of diabetes‐related amputations by 44% 57 |
| REACH Charleston and Georgetown Diabetes Coalition: Reducing Diabetes‐Related Amputations | CBPR for methods | Decrease disparities in amputations in African Americans by 3% annually in 2 county areas | (n≥ 45,000 participants) | Evidence‐based health systems changes using CQI teams 57 | Improved diabetes care for African Americans receiving care in 5 health systems 54 | |
| Funded by CDC | Healthcare providers in 2 county area (n= 39 physicians, >250 RNs, 5 pharmacists, 6 podiatrists) | Coalition interventions focused on collaboration, trust, sound business planning for systems, community & policy changes | ||||
| Coalition members including community members and leaders, people with diabetes, and healthcare professionals |
Similarities among the Programs of Research
The exemplar studies illustrated several overarching similarities as well as some unique characteristics. NIH and/or CDC, as well as private foundations, funded all studies and included an interdisciplinary research team, including community members, professionals, and community organizations’ representatives led or coled by nurse scientists. All studies relied upon the CBPR approach and targeted ethnic minority populations. Five studies focused on diabetes, a particularly serious health concern among minority and low‐income populations. All researchers engaged the community by partnering with community health clinics and/or health professionals with minority backgrounds. Gaps in services were identified with varying strategies to coordinate a collaborative response to the identified health problem. In three of the studies presented, there was approximately a 1‐year planning process prior to the delivery of the intervention. All studies used partnership committees or coalitions to provide guidance related to effective methods for community engagement, problem solving, and oversight related to the intervention(s) and monitoring of study progress and outcomes.
Most studies trained health professionals in standards and/or innovative methods developed within the programs for care delivery. Two of the studies included training of lay health workers in the community. Several of the researchers found that training communities and community members in research methods and the ethical conduct of research posed challenges. Time needed for training, scheduling of training sessions, and the ongoing need for IRB approvals and inclusion of community members on the IRB protocols and amendments were addressed. Additionally, several of the studies included opportunities for the community members to train the research team. This colearning facilitated program success.
All studies had translational research components, with the Newlin and Jenkins studies focusing on translation of evidence‐based diabetes self‐management strategies to community settings, while integrating community‐based evidence for application of the strategies. All studies had an initial stage in the research designed for community assessment to identify the community’s needs, and to use this information to guide and shape program development. In three of the studies, there was collaboration with churches or ministries. Several of the studies, Project REACH, Project SuGar, and the Faith‐Based Partnership studies, used fund‐raising strategies for initial work in the community and to generate funds for some community activities that were not covered by the federal grants (i.e., food for community meetings, supplies, and medications). Project SuGar obtained funding from private, public, and NIH sources. The Minding the Baby (MTB) home visiting study initially relied on an NINR P30 Center pilot grant and several foundation grants for bridge funding as the intervention was being initially developed and tested for feasibility. Each of the studies used a variety of media, including face‐to‐face presentations in the community, to communicate study‐related policies, opportunities, health messages, and findings. These dissemination venues included Web pages, newsletters, public service announcements in community meetings and on public buses, radio/TV advertisements with minority media, and dissemination of study reports and health messages.
Challenges and Strategies
The exemplar studies demonstrated successful approaches, ongoing challenges, lessons learned regarding community engagement and CBPR, and influenced community relationships and positive health outcomes. These themes are evident in both the context of the exemplar studies and the emerging literature on community engagement in health research. 20 , 21 , 27 , 28 , 29 The research challenges and strategies, as well as the lessons learned from the exemplar studies are presented in Table 2 .
Table 2.
Summary of community engagement challenges and lessons learned.
| Challenges | Strategies |
|---|---|
| Structural: | Community engagement: |
| • Social cultural access to care | • Formation of CAC and/or coalition |
| • Cultural memory | • Respect for culture and community; practice cultural humility, especially if an “outsider” who may not understand cultural diversity and nuances of community groups |
| • Patient provider concordance | • Find trusted community member to guide and educate research team |
| • Nontraditional family styles | • Provide service to community |
| 1. Professionalism by research team | |
| 2. Match linguistics and ethnicity of research team and study population; however, if ethnicity is different, make sure linkage to the community is demonstrated through participation in community events when appropriate | |
| • Recruitment & data collection through “family gatekeeper” | |
| 1. Distinguish between functional versus biological family members | |
| 2. Consider “fictive kin” (defined as important family members not related by blood or marriage) | |
| Study design/plan: | Flexible protocol: |
| • Protocol | • Research plan amended to increase recruitment options |
| • Fear of study questionnaire | 1. Establish trust with face‐to‐face interviews |
| • Literacy | 2. Acknowledge literacy level with nurse or other research staff completing and recording information, if needed or preferred by the participant |
| • Time | Partnership model for research |
| • Inclusion criteria | • Follow Principles and Guidelines for Community‐University Research Partnerships |
| • Formal policies & agreements | • Memorandum of understanding between community group or clinical agency and the university |
| • Ethical & research training for community partners | • Community group or clinical agency review of IRB protocols—suggest changes when needed |
| Research training | |
| • Consider group or individual face‐to‐face training for community members, or support/guide community members in online training | |
| Economic barriers: | Compensation and reward participant/community: |
| • Burden of research | • Schedule home visits |
| • Having to miss work to participate | • Tangible benefit to community with Project SuGar, mobile health unit, and REACH CHAs |
| • Lack of transportation | • Ancillary service by students |
| • Availability of healthcare | • Clarity on time required for research activities, budgets, and reimbursement (amount and time) for research efforts |
| Time and timelines | • Realistic funding and planning stages to allow for 6–12 months planning meetings with community members to inform and answer questions, build the working relationships, mutually build the intervention and evaluation models, and complete any required research training or IRB certification |
| • Clearly identify funded time for research so community aware of timelines | |
| Integration of research and service into complex health and community systems | • Work with partners to evolve clinical and research approaches acceptable to community members and systems |
| • Focus on community health outcomes as starting point for collaborative teams to “work back” in developing or refining intervention | |
| • Tailor clinical intervention to meet the community’s defined health needs, culture, and beliefs | |
| • Discuss costs and benefits of possible research designs (quasi‐experimental, randomized trials, etc) to test intervention and lead to improved healthcare and future funding opportunities for researchers and community agencies | |
| • Share success stories from other communities to illustrate potential research methods | |
| • Provide tangible benefits such as clinical service, consultations, in‐service education programs, community health screenings, or referrals during planning stages to build credibility and help meet clinical needs of partner agency and community members | |
| • Intervention staff attend clinical or departmental meetings at agency when invited to gain knowledge of system and become integrated into system | |
| • Explore ways to share responsibilities, funding, and completion of paperwork such as Federal Wide Assurances | |
| • Identify sustainability commitments and processes as partnerships are developed | |
| Relationship and trust building | • Explore partnership readiness for research—evidence‐based assessment: http://academicdepartments.musc.edu/nursing/cchp/cchp_products) |
| Dissemination of findings | • Face‐to‐face meetings located in community sites whenever possible. Initial planning meetings followed by ongoing collaborative problem solving and update meetings |
| • Schedule meetings to accommodate community members work schedules and respect for community members’ time | |
| • Provide snacks or light meals at meetings | |
| • Begin planning work early to allow community members to have input into design and make decisions about project | |
| • Continue regular meetings beyond the planning stage to insure communication and consistency | |
| • Build upon past clinical and/or successful research relationships with research team members and community | |
| • Provide regular updates of findings to community members through meetings, posters, newsletters, media reports, etc. | |
| • Inclusion and recognition of partners in publications | |
| Working with communities in distant sites | • Power sharing with shared input into budgets, intervention development and implementation, sharing community‐friendly data, and sustainability planning |
| • Consultation for emergent issues even if limited to telephone or electronic communication | |
| • Provision of intensive trainings and problem‐solving sessions during site visits | |
| • Adequate budget for travel and use of distance technologies |
Summary: Overarching Themes and Conceptual Foundation across the Studies
The following section highlights the overarching themes across the studies as well as the implied but unstated theoretical or conceptual foundation for all of the studies.
Among the six exemplar studies, there were many common and overarching themes that reflected the CDC Principles of Community Engagement and contributed to the success of these programs. 30 These themes included the following points.
-
1
Defining and understanding the community perceptions and preferences was a basic starting point for all the studies. The definitions were guided by both “insider and outsider” perceptions and definitions of community characteristics, history, important groups within the community, and relationships/dynamics among the smaller and larger systems within the community (Social Ecological Model [SEM]).
-
2
This work takes time; that cannot be overstated. Time for working with community leaders, gate keepers, and community partners should be built into the research plan, and funding strategies, to allow for a true working knowledge of the community to emerge within the research team and for a working relationship to develop between community members and researchers.
-
3
This work requires much face‐to‐face involvement and community visibility from the research team in partnership with the community leaders, members, and clinicians who will become part of the research and intervention programs. Respect, trust, and a true partnership model needs to permeate every aspect and phase of the work.
-
4
Research and intervention programs need to maintain a balance between fidelity and flexibility. Research protocols and programs need to be flexible enough to accommodate the multiple perspectives and needs of diverse members of the community. What makes sense theoretically, does not always work well within specific community settings. Community members are the experts in helping to modify approaches for the unique needs and characteristics of the community.
-
5
Building trust and fostering empowerment for community partners are essential elements of the work. Often there is community “history” or myths within the community about research and participation in research. These must be acknowledged and a sense of trust built with the research team and community members.
-
6
This type of research needs to acknowledge and accommodate the many social determinants of health and illness that are often present in racial and ethnic communities and low‐income communities, which are the focus of much CBPR health research. Understanding of issues such as social inequalities that contribute to health disparities, poor health outcomes, and poor participation in research by different racial and ethnic groups helps this process move forward. Social inequalities are rooted in social injustices. Social injustices and poor access to care can lead to bad or negative experiences with research, academic institutions and researchers, as well as healthcare systems. Negative past research experiences and cultural memory can impede participation in research by individuals or families.
-
7
Diverse family forms and styles may often be present and need to be understood and acknowledged. Identifying who the central family members are, blood relations, fictive kin, and family gate keepers, aids in establishing trust and credibility for the research team and in targeting the intervention toward the most appropriate individuals and groups, as indicated by the culture of the family and/or community.
-
8
The community needs short‐term and longer‐term tangible benefits from the research. However, clinical care, services, educational programs, and ongoing sharing of the benefits of the research are important ways to demonstrate the collaboration and mutual respect between research and community partners. Research staff may be able to be hired and trained from within the community settings, to help bridge gaps in background characteristics between researchers and community members. These community members can also act as ambassadors for the study within the community.
-
9
Long‐term commitment is essential to community‐engaged research. This is demonstrated by the Faith‐Based T2D Self‐Management studies since 2006, the Minding the Baby project in development and testing since 2002, and Project SuGar being in place since 1996. The REACH US Charleston and Georgetown Diabetes Coalition has been successfully operating since 1999, although the principal investigator had worked on diabetes‐related projects within segments of the community since 1979.
-
10
Reciprocity of relationships over time is an important consideration for academic‐community partnerships. The researcher and the community work together to improve a health‐related issue over several years; however, the cultures of the academic and community partners are usually distinctively different. The community members are focused on ways to improve health based on their culture, while the academic partners are focused on the culture of scientific processes of research and their theoretical foundations. Reciprocal interchanges and discussions can help to bridge these cultures, while identifying ways of working together to accomplish goals.
Jones and Wells sum up many of the principles by defining community engagement as referring to “values, strategies, and actions that support authentic partnerships, including mutual respect and active, inclusive participation; power sharing and equity; mutual benefit or finding the ‘win‐win’ possibility; and flexibility in pursuing goals, methods, and time frames to fit the priorities, needs, and capacities of communities” (p. 408). 31 They also acknowledge that some health professionals find that it is challenging to learn “what respect means in a community context,” as well as the meanings of “sharing planning authority, and understanding the time frame and flexibility required to accommodate the course of events and to build trust” (p. 408). 31
Conceptual Models Guiding the Research
Although each of the projects has identified theoretical framework(s) for the studies, we all recognize the social determinants of health within our communities, and the social inequities and disparities related to health in our respective communities. We also seek to create health equity and improve health outcomes related to our community and researcher‐identified priorities. We have collaboratively identified two models for further understanding the implications of social inequalities for health. These emphasize the interplay of social processes with features of the physical environment and illustrate the complexities influencing the health of our communities: Social Determinants of Health, developed by Schulz and colleagues; and the SEM. 32 , 33 , 34 The Institute of Medicine (IOM) model is shown in Figure 1 , and illustrates the potential interactions influencing individual and population health.
Figure 1.
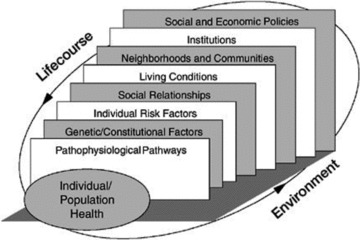
IOM promoting health. 32
In selecting the models, we focused on relationships between social inequalities and population health, as well as many other factors affecting health. Specifically, each of us adapted our research model for understanding racial disparities in diabetes or maternal and infant health. This facilitated the identification of multiple and dynamic pathways through which underlying social, political, and economic conditions influence aspects of the environment, thereby affecting Individuals, the health of the population, and the overall well‐being of the community. 33 , 34 , 35 As shown in Figure 2 , Healthy People 2010 also recognized that “Individual biology and behaviors influence health through their interaction with each other and with the individual’s social and physical environments. It is important to recognize the role of policies and interventions in improving health by targeting factors related to individuals and their environments, including access to quality healthcare. 36
Figure 2.
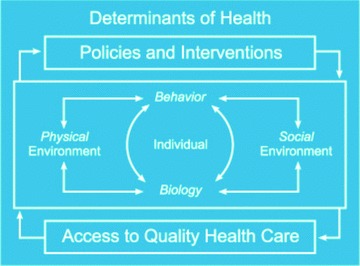
Healthy people 2010 determinants of health. 36
All of the exemplars acknowledge that our research projects are influenced by personal attributes, behavioral patterns, organizations, the larger environment, and that the dynamic interplay is greater than the sum of all. 37 Thus, the studies described in this paper integrated the Social Determinants of Health (SDOH) and the SEM as applied to health promotion, disease prevention, and health outcomes and we recognized the many social factors influencing the health of individuals and families as we engaged the communities in research.
In summary, the exemplar studies illustrated the following essential elements of community‐engaged health research:
-
1
All studies included multiple levels of prevention.
-
2
All delivered interventions to individuals in their social environments, and worked collaboratively with multiple organizations within the community to deliver the interventions and build community capacity for sustainable activities.
-
3
All recognized and addressed that individual behaviors were influenced by the biological, physical, and social environments, as well as the acceptability and access to quality healthcare. Although all recognized the role of policy changes on the individual and their communities, REACH Charleston and Georgetown Diabetes Coalition was the only one that specifically identified policy change as one of their aims. However, all of the diabetes projects focused on improving policies and systems of care while working with individuals and organizations in African American and Hispanic‐Latino communities to improve diabetes management and control. Minding the Baby exemplar focused on improving health for young first‐time parents living in a low‐SES urban community, as well as their social, family, and community networks.
-
4
All of the exemplar projects were led or coled by a nurse scientist. A transdisciplinary team worked together to bring about positive changes in health at the individual, family, organizational, and community levels, integrate the multiple social determinants of health and work to eliminate health disparities and create health equity. The programs were built based on community input, and the protocols included some flexibility as new issues emerged. The relationships were built slowly, over periods of time and emphasized the importance of face‐to‐face working together to building trust. And, finally, the message to remember from the community—“we want to know how much you care, before we care how much you know.”
Conflict of Interest
The authors have declared that no competing interests exist.
Acknowledgments
The authors express their appreciation to the study participants, the members of the communities, the staffs, and the community partners for their collaboration and contributions to these projects. Our work could not have been possible without their wisdom and support. We also thank and acknowledge the following colleagues who provided reviews of this manuscript: Sandra K. Hanneman, Donna. J. McClosky, and Barbara E. Moquin.
L. Sadler acknowledges the following support: NIH/NCRR CTSA (UL1 RR024139), The Irving B. Harris Foundation, The FAR Fund, The Annie E. Casey Foundation, The Patrick and Catherine Weldon Donaghue Foundation, NIH/NINR (P30NR08999), NIH/NICHD (R21HD048591), NIH/NICHD (RO1HD057947).
K. Newlin acknowledges the following support: NYU Global Health
Challenge Research Grant; NIH/NCRR CTSA (UL1 RR029893) and NIH/NINR F32 (NR010043).
I. Johnson‐Spruill acknowledges the following support: W.M. Keck Foundation, NIH/NIDDK (DK4761), ADA‐GENNID. This publication was supported by the South Carolina Clinical & Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, NIH/NCRR CTSA (UL 1RR029882).
C. Jenkins acknowledges the following support: The REACH Charleston and Georgetown Diabetes Coalition, CDC Grant/Cooperative Agreements (U50/CCU422184–01) through 05 and (1U58DP001015–01) through 02 from the US CDC, NIH, NINR (1 R15 NR009486–01A1), the Medical University of South Carolina College of Nursing, and the Diabetes Initiative of South Carolina. This publication was supported by the SCTR Institute, with an academic home at the Medical University of South Carolina, NIH/NCRR CTSA (UL 1RR029882).
This project has been funded in whole or in part with Federal funds from the NCRR, NIH, through the CTSA Program, part of the Roadmap Initiative, Reengineering the Clinical Research Enterprise. The manuscript was approved by the CTSA Consortium Publications Committee.
References
- 1. NIH . NIH Clinical and Translational Science Awards. National Institutes of Health; 2009. Available at: http://www.ncrr.nih.gov/clinical_research_resources/clinical_and_translational_science_awards/index.asp. Accessed September 26, 2010. [Google Scholar]
- 2. NIH . Overview of NIH Roadmap. National Institutes of Health; 2008. Available at: http://report.nih.gov/biennialreport/ViewSection.aspx?sid=4&cid=1. Accessed September 24, 2010. [Google Scholar]
- 3. Balas EA. From appropriate care to evidence‐based medicine. Pediatr Ann. 1998; 27: 581–584. [DOI] [PubMed] [Google Scholar]
- 4. Westfall JM, Mold J, Fagnan L. Practice‐based research‐ “Blue Highways” on the NIH roadmap. JAMA. 2007; 297(4): 403–406. [DOI] [PubMed] [Google Scholar]
- 5. Chesla CA. Translational research: essential contributions from interpretive nursing science. Res Nurs Health. 2008; 31(4): 109–117. [DOI] [PubMed] [Google Scholar]
- 6. Whittemore R, Grey M. The systematic development of nursing interventions. J Nurs Scholarsh. 2002; 34(2): 115–120. [DOI] [PubMed] [Google Scholar]
- 7. Woolf SH. The power of prevention and what it requires. JAMA. 2008; 299(2): 2437–2439. [DOI] [PubMed] [Google Scholar]
- 8. Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community‐based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998; 19: 173–202. [DOI] [PubMed] [Google Scholar]
- 9. Cornwall A, Jewkes R. What is participatory research? Soc Sci Med. 1995; 41(12): 1667–1676. [DOI] [PubMed] [Google Scholar]
- 10. DuBois JM, Bailey‐Burch B, Bustillos D, Campbell J, Cottler L, Fisher CB, Hadley WB, Hoop JG, Roberts L, Salter EK, et al Ethical issues in mental health research: the case for community engagement. Curr Opin Psychiatry. 2011; 24: 208–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Macaulay AC, Commanda LE, Freeman WL, Gibson N, McCabe M, Robbins C, Twohig P. Participatory research maximises community and lay involvement. Br Med J. 1999; 319: 774–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Horowitz CR, Robinson M, Seifer S. Community‐based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009; 119(19): 2633–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ross LF, Loup A, Nelson R, Botkin J, Kost R, Smith GR, Gehlert S. Human subjects protections in community‐engaged research: a research ethics framework. J Emp Res Human Res Ethics. 2010; 5(1): 5–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Olsen D, vanderArend A, Drought T, Eby M, Fasting U, Gastmans C, Leino‐Kilpi H, Lutzen K, Nojima S, Pang S, et al Ethical considerations in international nursing research: a report from the International Centre for Nursing Ethics. Nurs Ethics. 2003; 10(2): 122–137. [DOI] [PubMed] [Google Scholar]
- 15. Sadler LS, Updegrove S, Bouregy S, Breny‐Bontempi J, DAgostino G, Dickey‐Saucier L, LaPaglia D, Larson J, McCaslin C, Minor L, et al Principles and Guidelines for Community‐University Research Partnerships. New Haven , CT : Yale Center for Clinical Investigation; 2009. [Google Scholar]
- 16. Stanton T. New times demand new scholarship: opportunities and challenges for civic engagement at research universities. Education, Citizenship and Social Justice. 2008; 3(19): 19–42. [Google Scholar]
- 17. RFA NIH.: Institutional Clinical and Translational Science Award (U54). http://grants.nih.gov/grants/guide/rfa‐files/rfa‐rm‐08–002.html. Accessed January 24, 2011.
- 18. Francis‐Baldesari C, Williamson D. Integration of nursing education, practice and research through community partnerships. Adv Nurs Sci. 2008; 31(4): E1–E10. [DOI] [PubMed] [Google Scholar]
- 19. Knafl K, Grey M. Clinical and translational science awards: opportunities and challenges for nurse scientists. Nurs Outlook. 2008; 56(3): 132–137. [DOI] [PubMed] [Google Scholar]
- 20. Bilodeau R, Gilmore J, Jones L, Palmisano G, Banks T, Tinney B, Lucas G. Putting the “community” into community‐based participatory research. Am J Prev Med. 2009; 37: S192–S194. [DOI] [PubMed] [Google Scholar]
- 21. Norris KC, Brusuelas R, Jones L, Miranda J, Duru OK, Mangione C. Partnering with community‐based organizations: an academic institution’s evolving perspective. Ethn Dis. 2007; 17: SI27–SI32. [PubMed] [Google Scholar]
- 22. Davey CJ. Lady with a Lamp. New York : Lutterworth Press; 1958. [Google Scholar]
- 23. Nelson S, Rafferty A. Notes on Nightingale: The Influence and Legacy of a Nursing Icon. Ithaca , NY : Cornell University Press; 2010. [Google Scholar]
- 24. Cleary M, Hunt GE. Building community engagement in nursing. J Contin Educ Nurs. 2010; 41(8): 344–345. [DOI] [PubMed] [Google Scholar]
- 25. O’Neill M, Lemieux V, Groleau G, Fortin JP, Lamarche PA. Coalition theory as a framework for understanding and implementing intersectoral health‐related intervention. Health Promot Int. 1997; 12(1): 79–86. [Google Scholar]
- 26. Delaney F. Muddling through the middle ground: theoretical concerns in intersectoral collaboration and health promotion. Health Promot Int. 1994; 9(3): 217–225. [Google Scholar]
- 27. CTSA . Researchers and their communities: the challenge of meaningful community engagement Clinical and Translational Science Awards Community Engagement Key Function Committee. 2009. Available at: http://www.ctsaweb.org/index.cfm?fuseaction=committee.viewCommittee&com_ID=3&abbr=CEKFC. Accessed November 2, 2010. [Google Scholar]
- 28. Silka L, Cleghorn GD, Grullon M, Tellez T. Creating community‐based participatory research in a diverse community: a case study. J Emp Res Human Res Ethics. 2008; 3(2): 5–16. [DOI] [PubMed] [Google Scholar]
- 29. Berwick D. Disseminating innovations in health care. JAMA. 2003; 289(15): 1969–1975. [DOI] [PubMed] [Google Scholar]
- 30. CDC . Principles of community engagement Centers for Disease Control and Prevention Committee on Community Engagement. 1997. Washington , DC : US Government Printing Office; 1997. [Google Scholar]
- 31. Jones L, Wells K. Strategies for academic and clinician engagement in community‐participatory partnered research. JAMA. 2007; 297(4): 407–410. [DOI] [PubMed] [Google Scholar]
- 32. Warner KE. The need for and value of a multilevel approach to disease prevention In: Smedley BD, Syme SL, eds. Promoting Health: Intervention Strategies from Social and Behavioral Research. Washington , DC : National Academy Press; 2000: 40–53. [PubMed] [Google Scholar]
- 33. Schulz AJ, Northridge ME. Social determinants of health: implications for environmental health promotion. Health Educ Behav. 2004; 31(4): 455–471. [DOI] [PubMed] [Google Scholar]
- 34. Schulz AJ, Williams D, Israel BA, Lempert LB. Racial and spatial relations as fundamental determinants of health in Detroit. Milbank Quart. 2002; 80(4): 677–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Schulz AJ, Krieger J, Galea S. Addressing social determinants of health: community‐based participatory approaches to research and practice. Health Educ Behav. 2002; 29(3): 287–295. [DOI] [PubMed] [Google Scholar]
- 36. USDHHS . Healthy People 2010 Office of Disease Prevention and Health Promotion. U.S. Department of Health and Human Services; 2000. Available at: http://www.healthypeople.gov/document/html/uih/uih_2.htm. Accessed November 16, 2010. [Google Scholar]
- 37. Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promot. 1996; 10: 283–298. [DOI] [PubMed] [Google Scholar]
- 38. Sadler LS, Slade A, Mayes L. Minding the baby: a mentalization‐based parenting program In: Allen JG, Fonagy P, eds. Handbook of Mentalization‐Based Treatment. Chichester , UK : Wiley; 2006: 271–288. [Google Scholar]
- 39. Slade A, Sadler LS, de Dios‐Kenn C, Webb D, Ezepchick J, Mayes LC. Minding the baby: a reflective parenting program. Psychoanal Study Child. 2005; 60: 74–100. [DOI] [PubMed] [Google Scholar]
- 40. Olds D, Sadler L, Kitzman H. Programs for parents of infants and toddlers: recent evidence from randomized trials. J Child Psychol Psychiatry. 2007; 48: 355–391. [DOI] [PubMed] [Google Scholar]
- 41. Mayes LC, Swain JE, Leckman J. Parental attachment systems: neural circuits, genes and experiential contributions to parental engagement. Clin Neurosci Res. 2005; 4: 301–313. [Google Scholar]
- 42. Slade A. Parental reflective functioning: an introduction. Attachment and Human Development. 2005; 7(3): 269–281. [DOI] [PubMed] [Google Scholar]
- 43. Parker M, Barry C, King B. Use of inquiry method for assessment and evaluation in a school‐based community nursing project. Fam Community Health. 2000; 23(2): 54–61. [Google Scholar]
- 44. Bolton LB, Georges CA. National black nurses association community collaboration model. J Natl Black Nurses Assoc. 1996; 8(2): 48–67. [PubMed] [Google Scholar]
- 45. Horowitz CR, Goldfinger JZ, Muller SE, Pulichino RS, Vance TL, Arniella G, Lancaster KJ. A model for using community‐based participatory research to address the diabetes epidemic in East Harlem. Mt Sinai J Med. 2008; 75(1): 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Springer ET. Action Research. London : Sage; 1999. [Google Scholar]
- 47. Newlin K, Melkus GD, Mclean Y, Dekker T, Wick A, Chyun D. Nicaraguan Creole and Miskito adults with or at‐risk for type 2 diabetes: exploration of quality of life, A1c, and receipt of diabetes‐related education/advice. Diabetes. 2010; 59(Suppl. 1): A282–A283. [Google Scholar]
- 48. Newlin K, Melkus GD, Mclean Y, Dekker T, Wick A, Chyun D. Mixed‐methods results to inform church‐based diabetes education in Nicaragua. Diabetes. 2010; 59(Suppl. 1): A282. [Google Scholar]
- 49. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE‐AIM framework. Am J Public Health. 1999; 89(9): 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Spruill I. Project Sugar: a recruitment model for successful African‐American participation in health research. J Natl Black Nurses Assoc. 2004; 15(2): 48–53. [PubMed] [Google Scholar]
- 51. Johnson‐Spruill I, Riegel B. The quality of diabetes care to Gullah families of South Carolina. J Natl Black Nurses Assoc. 2008; 19(2): 20–27. [PMC free article] [PubMed] [Google Scholar]
- 52. Spruill I, Hammond P, Davis B, McGee Z, Louden D. Health of Gullah families in South Carolina with type 2 diabetes: diabetes self‐management analysis from Project SuGAR. Diab Educator. 2009; 35(1): 117–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sale M, Lu L, Spruill I, Fernandes J, Lok K, Divers J, Langerfeld C, Garvey T. Genome‐wide linkage scan in Gullah‐speaking African American families with type 2 diabetes. Diabetes. 2009; 58: 260–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jenkins C, McNary S, Carlson BA, King MG, Hossler CL, Magwood GM, Zheng D, Hendrix K, Beck LS, Linnen F, et al Reducing disparities for African Americans with diabetes: progress made by the REACH 2010 Charleston and Georgetown Diabetes Coalition. Public Health Rep. 2004; 119: 323–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Jenkins C, Pope CA, Magwood G, Vandemark L, Thomas V, Hill K, Linnen F, Beck LS, Zapka J. An evolving expanded chronic care framework to improve diabetes management – the REACH case study. Prog Community Health Partnersh. 2010; 4(1): 65–79. [DOI] [PubMed] [Google Scholar]
- 56. Jenkins C, Magwood G, Thomas V, Linnen F. REACH Charleston and Georgetown Diabetes Coalition: improving outcomes for African Americans with diabetes In: Liburd L, ed. Diabetes and Health Disparities Community‐Based Approaches for Racial and Ethnic Populations. Philadelphia : Springer; 2009: 237–256. [Google Scholar]
- 57. Jenkins C, Myers P, Heidari K, Kelechi T, Buckner‐Brown J. Efforts to decrease diabetes‐related amputations in African Americans by the racial and ethnic approaches to community health Charleston and Georgetown Diabetes Coalition. Fam Community Health. 2010; 34(15): S63–S78. [DOI] [PubMed] [Google Scholar]


