Abstract
Capsaicin is a pungent ingredient in chili red peppers and has been linked to suppression of growth in various cancer cells. However, the underlying mechanism(s) by which capsaicin induces growth arrest and apoptosis of cancer cells is not completely understood. In the present study, we investigated whether capsaicin alters β-catenin-dependent signaling in human colorectal cancer cells in vitro. Exposure of SW480, LoVo, and HCT-116 cells to capsaicin suppressed cell proliferation. Transient transfection with a β-catenin/T-cell factor (TCF)-responsive reporter indicated that capsaicin suppressed the transcriptional activity of β-catenin/TCF. Capsaicin treatment resulted in a decrease of intracellular β-catenin levels and a reduction of transcripts from the β-catenin gene (CTNNB1). These results were confirmed by a reduced luciferase reporter activity driven by promoter-reporter construct containing the promoter region of the Catnb gene. In addition, capsaicin destabilized β-catenin through enhancement of proteosomal-dependent degradation. Western blot and immunoprecipitation studies indicated that capsaicin treatment suppressed TCF-4 expression and disrupted the interaction of TCF-4 and β-catenin. This study identifies a role for the β-catenin/TCF-dependent pathway that potentially contributes to the anti-cancer activity of capsaicin in human colorectal cancer cells.
Keywords: Capsaicin, β-catenin, TCF-4, Colorectal cancer
1. INTRODUCTION
Colorectal cancer is an important public health problem in the Western world and the third leading cause of cancer-related death in the United States [1]. A total of 142,570 new colorectal cancer cases and 51,370 colon cancer-related deaths are expected in the United States in 2010 [2].
A number of case-control and cohort studies have demonstrated an inverse relationship between the consumption of vegetables and colorectal cancer [3]. Among common vegetables selected on the basis of consumption per capita data in the United States, red chili pepper showed very high anti-proliferative and anti-oxidant activity [4], and Americans' consumption of chili peppers has doubled to almost 6 pounds per capita per year since 1980 [5].
Capsaicin is a major ingredient in hot chili pepper, and recent studies demonstrated anti-cancer activities of capsaicin in various types of cancer models [6–13]. However, capsaicin also acts as a co-carcinogen or tumor promoter in some cancer models, including skin [14] and stomach [15]. Previously, we and others reported that capsaicin inhibits growth of colorectal cancer and tumor formation [6, 7, 16–19], and capsaicin-induced apoptosis is mediated by various mechanisms including AMPK, caspase-3, PPARγ, ROS, p53, TRPV6, EGFR/HER-2 and E2F [7–13, 18–22].
A high incidence of human colorectal cancer has been associated with genetic alteration of either the β-catenin gene (CTNNB1) or the adenomatous polyposis coli (APC) gene, the products of which interact with casein kinase 1α, glycogen synthase kinase-3β (GSK-3β), and axin [23]. In the absence of Wnt stimulation, β-catenin is destabilized by phosphorylation and subsequent proteasomal degradation through active GSK-3β. Free β-catenin accumulates in the cytoplasm and translocates into the nucleus, where it binds to the members of the T-cell factor (TCF) / lymphoid enhancer factor (LEF) family and transactivates several target genes, including cyclin D1 [24], cmyc [25], and PPAR-δ [26]. In particular, the formation of the β-catenin/TCF-4 complex results in a master switch that controls proliferation in malignant intestinal epithelial cells [27]. Therefore b-catenin signaling is a significant target of chemoprevention by dietary compounds [28–30].
The current study was performed to elucidate the mechanism by which capsaicin might prevent the growth of human colorectal cancer cells. Here, we report that capsaicin suppresses b-catenin/TCF-dependent pathways through multiple mechanisms, including suppression of β-catenin transcription, activation of proteosomal degradation of β-catenin, and disruption of β-catenin/TCF-4 interactions in human colorectal cancer cells.
2. MATERIALS AND METHODS
2.1. Materials
Capsaicin was purchased from BIOMOL (Plymouth Meeting, PA) and dissolved in absolute ethanol. Polyclonal antibody for β-catenin (#9562) and monoclonal antibody for TCF-4 (#2953) were purchased from Cell Signaling (Beverly, MA). Antibodies for cyclin D1 (sc-718), C/EBPα (sc-9315), ubiquitin (sc-8017) and actin (sc-1615) were purchased from Santa Cruz (Santa Cruz, CA). Antibody for GFP (130-091-833) was obtained from Miltenyi Biotec (Auburn, CA). MG-132, puromycin and cycloheximide were purchased from Calbiochem (San Diego, CA). The GFP-β-catenin expression vector, TOP/FOP FLASH luciferase constructs and cyclin D1 promoter were described previously [31, 32]. Cell culture media were purchased from Invitrogen (Carlsbad, CA). All chemicals were purchased from Fisher Scientific, unless otherwise specified.
2.2. Cell culture and treatment
Human colorectal carcinoma cells (SW480, LoVo, and HCT-116) were purchased from American Type Culture Collection (Manassas, VA) and were grown at 37°C under a humidified atmosphere of 5% CO2. SW480, LoVo and HCT-116 cells were maintained in RPMI1640, Ham's F-12 and McCoy 5A media, respectively. All media were supplemented with 10% fetal bovine serum (FBS) and a mixture of penicillin (100 U/mL) and streptomycin (100 μg/mL). The cells were grown in 12-well plates (for luciferase analysis of TOP/FOP reporter gene, β-catenin or cyclin D1 promoter), 6-well plates (for overexpression of GFP-β-catenin) or 10 cm plates (for immunoprecipitation) at a concentration of 2×105 cells/mL and then treated with capsaicin at concentrations or time points indicated in figure legends.
2.3. Analysis of cell proliferation and cell viability
Cell proliferation assay was performed using the Cell Proliferation Assay system (Promega, Madison, WI). Briefly, SW480 (3000 cells/well), LoVo (3000 cells/well) and HCT-116 (1000 cells/well) cells were plated in 96-well culture plates and incubated overnight. Next day, the cells were treated with 0, 50, or 100 μM of capsaicin in media containing 1% FBS for 0, 1, 2, or 3 d. The cells were incubated with CellTiter96 Aqueous One solution (20 μL) for 1 h at 37°C and absorbance (A490) was recorded in an ELISA plate reader (Bio-Tek Instruments Inc, Winooski, VT). Cell viability was measured using Cell Titer-Glo Luminescent Cell Viability Assay system (Promega). SW480 cells were plated in 96-well culture plates and incubated with 0, 50, or 100 μM of capsaicin for 48 h. Then the cells were lysed by Cell Titer-Glo solution for 2 m with shaking and luminescence signal was stabilized for 10 m at room temperature. The luciferase activity was measured using a luminometer TD-20/20 (Turner Design, Sunnyvale, CA).
2.4. Transient transfections
Transient transfections were performed using the Lipofectamin 2000 (Invitrogen) or PolyJet DNA transfection reagent (SignaGen Laboratories, Ijamsville, MD) according to the manufacturer's instruction. The cells were transiently transfected with expression vectors (GFP-β-catenin) or luciferase constructs (TOP/FOP Flash, β-catenin or cyclin D1 promoter) for 24 h. For luciferase assay, the cells were harvested in 1× luciferase lysis buffer, and luciferase activity was determined and normalized to the pRL-null luciferase activity using a dual luciferase assay system (Promega) as we described previously [16, 33].
2.5. Western blotting
After three washes with ice-cold PBS, cells were scraped into an eppendorf tube and lysed with radioimmunoprecipitation assay (RIPA) buffer containing a protease/phosphatase inhibitors cocktail (Pierce). After centrifugation at 10,000×g for 10 min at 4°C, the supernatant was collected, and protein concentration was determined by the BCA protein assay (Pierce) using bovine serum albumin as a standard. The proteins were separated on SDS-PAGE and transferred to nitrocellulose membranes. The membranes were incubated with a specific primary antiserum in TBS containing 0.05% Tween 20 (TSB-T) and 5% nonfat dry milk at 4°C overnight. After four washes with TBS-T, the blots were incubated with horse radish peroxidase-conjugated IgG for 1 h at room temperature and visualized using ECL (Amersham Biosciences, Piscataway, NJ).
2.6. Immunoprecipitation
Cells were lysed using M-PER mammalian protein extraction reagent (Thermo Scientific, Rockford, IL) for 30 m and then centrifuged for 5 m at 10,000×g at 4°C. The supernatants were incubated with polyclonal anti- β-catenin antibody (1:100) overnight at 4°C, followed by incubation with protein A/G beads (Santa Cruz) for 2 h at 4°C. After washing four times in ice-cold PBS, the protein complex was boiled in an equal volume of 2× SDS-sample buffer and used for immunoblotting using monoclonal anti-ubiquitin or monoclonal anti-TCF-4 antibody.
2.7. Preparation of nuclear extracts
The cells were plated onto a 10 cm culture dish and treated with capsaicin. Nuclear extracts were harvested using the Nuclear Extract Kit (Active Motif, Carlsbad, CA), according to the manufacturers' protocol.
2.8. Isolation and analysis of RNA
Total RNA was prepared using an RNA isolation kit (Eppendorf, Hamburg, Germany), according to the manufacturer's instructions. One μg of total RNA was reverse-transcribed with an iScript cDNA kit (BioRad, Hercules, CA), according to the manufacturer's instruction. PCR was carried out for 25 cycles at 94°C for 30 s, 55°C for 30 s, and 72°C for 1 min using ReadyMix Taq polymerase (Sigma, St.Louis, MO) with human PCR primers as follows: β-catenin (CTNNB1): forward 5'-cccactaatgtccagcgttt-3', and reverse 5'-aatccactggtgaaccaagc-3', GAPDH: forward 5'-gggctgcttttaactctggt-3', and reverse 5'-tggcaggtttttctagacgg-3'.
2.9. Statistical analysis
Statistical analysis was performed with the Student t test, with statistical significance set at *, P < 0.05; **, P < 0.01; ***, P < 0.001.
3. RESULTS
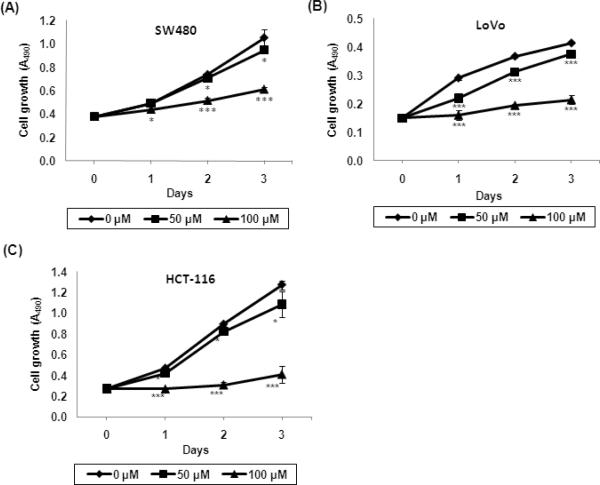
3.1. Inhibitory effects of capsaicin on growth of colorectal cancer cells
To investigate whether capsaicin possessed anti-proliferative activity in APC mutant human colorectal cancer cells, SW480 and LoVo cells (APC mutant, β-catenin wild type) were exposed to 0, 50 and 100 μM of capsaicin for 0, 1, 2, or 3 d, and cell proliferation was performed as described in Materials and Methods. We also measured anti-proliferative activity of capsaicin in HCT-116 cells (APC wild type, β-catenin mutant). As shown in Fig. 1, growth of all three human colorectal cancer cell lines was inhibited by capsaicin treatment in a dose- and time-dependent manner. Although 50 μM capsaicin treatment decreased cell growth to some extent, significantly retarded cell growth was observed in cells treated with 100 μM of capsaicin. In addition, these data indicated that cell growth arrest by capsaicin exposure was mediated in an APC-independent manner.
Fig. 1.
Inhibitory effect of capsaicin on proliferation of colorectal cancer cells. Human colorectal cancer cells SW480 (A), LoVo (B) and HCT-116 (C) were treated with 0, 50 or 100 μM of capsaicin in 1% serum containing media for 0, 1, 2, and 3 days. Cell growth was measured using CellTiter96 Aqueous One Solution Cell Proliferation Assay and expressed as absorbance (A490). *, P<0.05; ***, P < 0.001 versus vehicle (ethanol)-treated cells.
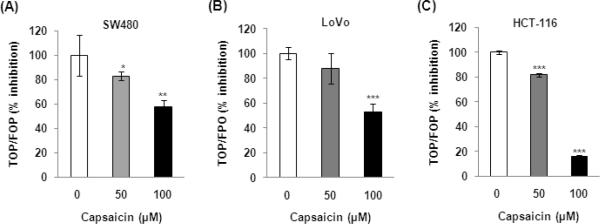
3.2. Decreased transcriptional activity of β-catenin by capsaicin treatment
Alteration of β-catenin signaling caused by mutation in the APC or CTNNB1 gene is associated with colorectal tumorigenesis [34]. In order to determine whether capsaicin modulated b-catenin/TCF-dependent activity, a luciferase reporter assay was performed using TOP-FLASH or FOP-FLASH constructs containing six copies of wild type or mutated TCF binding sites, respectively. Capsaicin treatment significantly inhibited the TOP/FOP ratio in a dose-dependent manner, in cells treated with 50 and 100 μM of capsaicin for 48 h (Fig. 2). These findings indicated that capsaicin suppressed β-catenin/TCF-dependent signaling in human colorectal cancer cells.
Fig. 2.
Decreased transcriptional activity of β-catenin by capsaicin treatment. Human colorectal cancer cells SW480 (A), LoVo (B) and HCT-116 (C) were co-transfected with TOP-FLASH or FOP-FLASH constructs containing six copies of wild type or mutated TCF binding sites and pRL-null. Then, the cells were treated with 0, 50, and 100 μM of capsaicin for 48 h. Luciferase activity for TOP-FLASH and FOP-FLASH was measured as a ratio of firefly luciferase signal/renilla luciferase signal using a dual luciferase assay kit (Promega). A ratio of TOP-FLASH over FOP-FLASH was calculated and expressed as % inhibition over vehicle-treated cells. *, P<0.05; ** < 0.01; ***, P < 0.001 versus vehicle (ethanol)-treated cells. The data represent mean ± SD from three replicates.
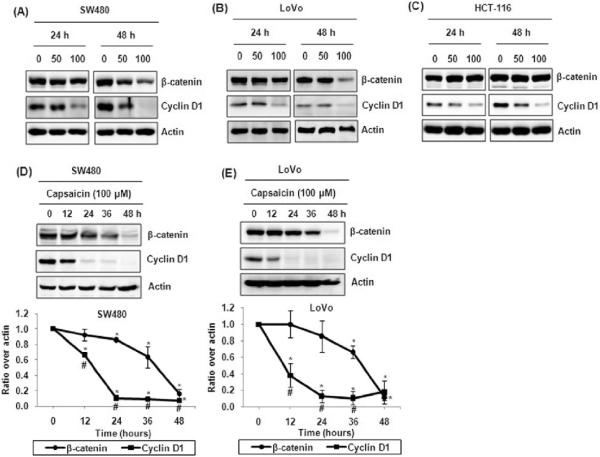
3.3. Decreased expression of β-catenin by capsaicin treatment
Increased expression or nuclear translocation of β-catenin allows interaction with the TCF/LEF transcription factors and stimulates transcription of downstream β-catenin target genes. To test whether capsaicin affects expression of β-catenin, we performed Western blot in the colorectal cancer cells treated with 0, 50, or 100 μM capsaicin. As shown in Fig. 3A, capsaicin treatment resulted in the inhibition of β-catenin expression in SW480 cells, compared with untreated cells. In addition, incubation with 100 μM of capsaicin was associated with a significant decrease in β-catenin levels in LoVo cells (Fig. 3B). Interestingly, capsaicin treatment did not affect expression of β-catenin protein in HCT-116 cells (Fig. 3C). Time course experiments showed that β-catenin began to decrease at 24 h, and markedly decreased at 48 h in SW480 and LoVo cells, respectively (Fig. 3D, E). Expression of cyclin D1 decreased in the cells treated with capsaicin, but the decrease of cyclin D1 expression was much more pronounced than that of β-catenin in the cells, and occurred at an earlier time (12 h).
Fig. 3.
Decreased expression of β-catenin by capsaicin treatment (A, B, C). Human colorectal cancer cells SW480 (A), LoVo (B) or HCT-116 (C) were treated with 0, 50 or 100 μM of capsaicin for 24 or 48 h. (D, E) SW480 (D) or LoVo (E) cells were treated with 100 μM of capsaicin for indicated times. Cell lysates were harvested and subjected to SDS-PAGE. Western blot was performed using antibodies against β-catenin, cyclin D1, and actin. Data from three independent experiments were densitometrically analyzed using Scion Image (Scion Corporation, Frederick, MD) (lower panel). *, P<0.05 between 0 h and each time; #, P<0.05 between β-catenin and cyclin D1 at each time point.
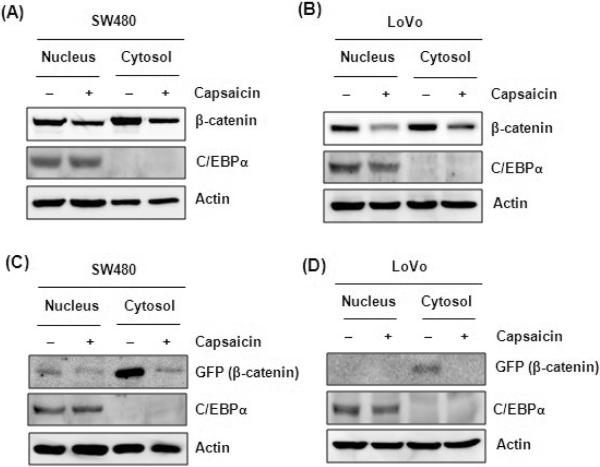
It is also expected that nuclear translocation of β-catenin is positively associated with transcriptional activity of β-catenin. To define whether capsaicin alters nuclear localization, we performed Western blot from fractionated nuclear or cytosolic lysates after 48 h capsaicin treatment. The result shows that capsaicin treatment in SW480 cells did not alter nuclear translocation of endogenous (Fig. 4A) and ectopically transfected β-catenin (Fig. 4C). Instead, capsaicin treatment decreased β-catenin protein level in both fractions (nucleus and cytosol). This trend was also observed in LoVo cells (Fig. 4B, D). Isolation of nuclear and cytosol proteins was validated by the expression of C/EBPα, which is expressed only in the nucleus. It is notable that ectopically expressed β-catenin was mainly localized in the cytosol fraction (Fig. 4C, D). The results indicated that capsaicin treatment simultaneously decreased the accumulation of β-catenin in the nucleus as well as in the cytosol. However, consistent with results of Fig. 3C, Western blot with endogenous or ectopically expressed GFP-labeled β-catenin was not altered by capsaicin treatment in HCT-116 cells (data not shown).
Fig. 4.
Decreased expression of nuclear and cytosol β-catenin by capsaicin treatment. (A, B) SW480 cells (A) or LoVo cells (B) were plated onto 10 cm culture dish and then treated with capsaicin for 48 h. The nuclear and cytosol fractions were isolated and Western blot was performed against β-catenin, C/EBPα and actin antibodies. (C, D) SW480 cells (C) or LoVo cells (D) were transfected with GFP-tagged β-catenin expression vector (GFP-β-catenin) and then treated with 100 μM of capsaicin for 48 h. Nuclear and cytosol fractions were isolated and Western blot was performed using GFP, C/EBPα and actin antibodies.
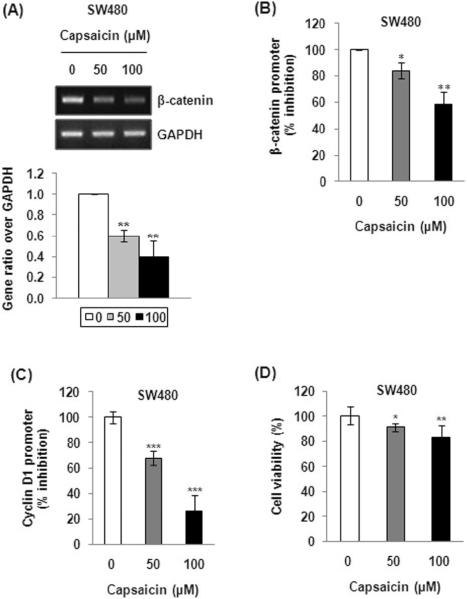
3.4. Transcriptional down-regulation of the β-catenin gene by capsaicin in SW480 cells
To investigate the possible molecular mechanism of capsaicin in down-regulation of β-catenin, SW480 cells were incubated with 0, 50, or 100 μM of capsaicin, and mRNA levels of β-catenin were measured using RT-PCR. The result revealed a dose-dependent decrease in transcript levels of β-catenin after capsaicin treatment (Fig. 5A). We also observed a significant decrease of cyclin D1 mRNA in the cells treated with 100 μM of capsaicin (data not shown). To investigate whether a decrease of β-catenin mRNA is associated with transcriptional regulation of a gene encoding the β-catenin protein, mouse Catnb promoter (spanning −2153 to +18) was transfected into cells, and luciferase activity was measured after 48 h treatment of capsaicin. As shown in Fig. 5B, capsaicin treatment resulted in the suppression of promoter-reporter activity by 16% and 41% in the cells treated with 50 and 100 μM of capsaicin, respectively.
Fig. 5.
Transcriptional down-regulation of β-catenin by capsaicin. (A) SW480 cells were treated with 0, 50, and 100 μM of capsaicin for 48 h, and semi-quantatitive RTPCR was performed as described in Materials and Methods. Data from three independent experiments were densitometrically analyzed using Scion Image and β-catenin versus GAPDH was quantified and expressed as fold induction (Lower panel). **, P < 0.01 versus vehicle-treated cells. (B) SW480 cells were transfected with β-catenin promoter and pRL-null, and then treated with 0, 50 and 100 μM of capsaicin for 48 h. Luciferase activity was determined and normalized to the pRL-null luciferase activity using a dual luciferase assay kit (Promega) and presented as % inhibition versus vehicle-treated group. *, P < 0.05; **, P < 0.01 versus vehicle-treated cells. The data represent mean ± SEM from three independent experiments. (C) SW480 cells were transfected with a reporter gene containing −163/+130 cyclin D1 promoter, and then the cells were treated with 0, 50 and 100 μM capsaicin for 48 h. Luciferase activity was measured as a ratio of firefly luciferase signal/renilla luciferase signal and is presented as % inhibition versus vehicle-treated group. ***, P < 0.001 versus vehicle-treated cells. (D) SW480 cells were treated with 0, 50, or 100 μM of capsaicin for 48 h and then cell viability was measured using Cell Titer-Glo Luminescent Cell Viability Assay system (Promega) as described in Materials and Methods. *, P < 0.05; **, P < 0.01 versus vehicle-treated cells.
Down-regulation of β-catenin inhibits interaction of β-catenin with the TCF/LEF family of transcription factors and deactivates transcription of downstream genes such as cyclin D1 [24]. Thus, to test whether capsaicin affects transcriptional activity of the cyclin D1 gene, we measured luciferase activities of cyclin D1 promoter containing −163 and +130, which contains the TCF binding site [35]. Capsaicin treatment resulted in a dose-dependent decrease of cyclin D1 promoter activity, greater than that seen for Catnb (Fig. 5C). Together with results of Fig. 3(D, E), these data imply that down-regulation of cyclin D1 transcription is independent of β-catenin down-regulation.
We also compared cell viability to see whether decreased promoter activity is a result of cell death. As shown in Fig. 5D, cell viability decreased 9% and 17% in the cells treated with 50 and 100 μM of capsaicin, respectively. The decreased cell viability seems to be a result of activated apoptosis because we and others observed that capsaicin induces apoptosis in human colorectal cancer cells [7–13, 16, 18–22]. However, decreased rate of cell viability (9 and 17%) is much less than those of promoter activities of β-catenin (16 and 41%) or cyclin D1 promoter (32 and 74%), implying that decreased promoter activity represents transcriptional down-regulation of β-catenin and cyclin D1.
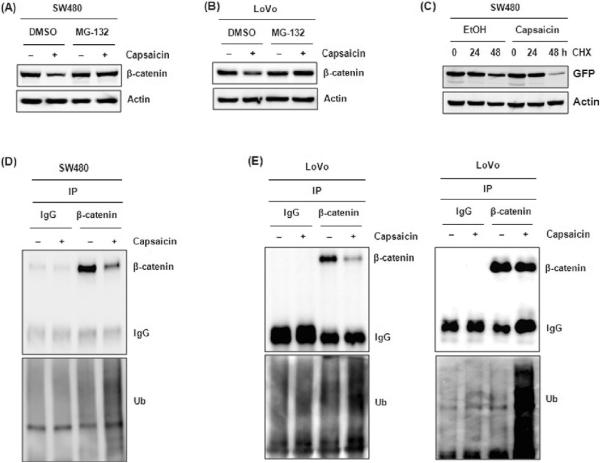
3.5. Proteosomal degradation of β-catenin by capsaicin
β-catenin becomes stabilized when proteasome-mediated proteolysis is inhibited, and this leads to the accumulation of multi-ubiquitinated forms of β-catenin [36]. Thus, we tested whether proteasomal degradation contributes to the decrease of β-catenin protein levels using the proteasome inhibitor MG-132. Pre-treatment with MG-132 diminished capsaicin-mediated down-regulation of β-catenin in SW480 and LoVo cells (Fig. 6A, B). Next, to confirm this data, we compared β-catenin protein levels after capsaicin treatment in the presence of the protein synthesis inhibitor cycloheximide (CHX). GFP-tagged β-catenin expression vector was transfected into SW480 cells and the cells were co-treated with CHX and capsaicin for indicated times. As shown in Fig. 6C, degradation of β-catenin occurred more rapidly in the presence of capsaicin. This more rapid degradation of β-catenin by capsaicin treatment was also observed in LoVo cells (data not shown). These results suggest that capsaicin suppresses β-catenin expression at both transcriptional and post-translational levels.
Fig. 6.
Increased proteosomal degradation and ubiquitination of β-catenin by capsaicin. (A, B) SW480 cells (A) or LoVo cells (B) were pretreated with DMSO or MG-132 (10 μM) for 30 min and then co-treated with ethanol or capsaicin for 48 h. Western analysis was performed for β-catenin and actin antibodies. (C) SW480 cells were transfected with GFP-tagged β-catenin expression vector. Then the cells were pretreated with vehicle (ethanol) or capsaicin for 1 h and then co-treated with 10 μg/mL of cycloheximide (CHX) for the indicated time points. Western blot was performed for using antibodies against GFP and actin. (D, E) SW480 cells (D) or LoVo cells (E) were treated with 100 μM of capsaicin for 48 h, and then immunoprecipitation (IP) was performed by pull down of cellular protein with β-catenin antibody and subsequent immunoblotting with ubiquitin (Ub) antibody. Right panel indicates results after normalizing amounts of immunoprecipitated β-catenin in IP step.
It is well established that β-catenin is degraded by the 26S proteasome after the covalent binding with ubiquitin [23]. To confirm that the reductions in β-catenin levels by capsaicin treatment are indeed caused by this mechanism, we tested whether capsaicin treatment results in an increase of ubiquitinated β-catenin levels. The results show that appearance of an ubiquitin immunoreactive β-catenin band is increased by the addition of capsaicin (Fig. 6D and E). In reflecting decreased immunoprecipitated β-catenin in response to capsaicin, it seems likely that the β-catenin-conjugated ubiquitination was increased significantly by capsaicin treatment. As shown in Fig. 6E (right panel) normalizing amounts of immunoprecipitated β-catenin in immunoprecipitation step revealed a more dramatic increase in ubiquitinated bands on the immunoblots.
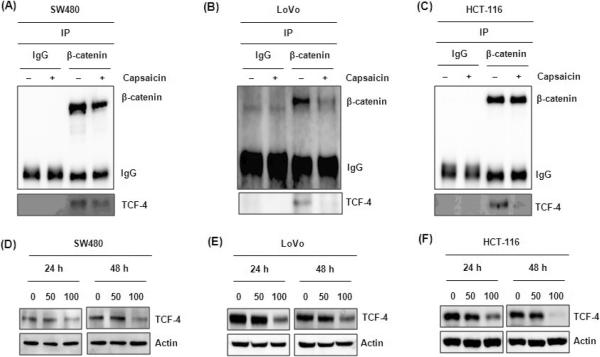
3.6. Capsaicin decreased TCF-4 expression and binding of β-catenin to TCF-4
Another possible mechanism regulating transcriptional activity of β-catenin is integrity of the β-catenin/TCF complex, which is required for normal transcriptional activity. Because cellular levels of β-catenin protein expression remained unchanged in HCT-116 cells (Fig. 3C), despite suppressed transcriptional activity of β-catenin (Fig. 2C), we examined the possibility that capsaicin disrupts the association of β-catenin with TCF-4. For this, cell lysates were pulled down with β-catenin and immunoblotted with anti-TCF-4 antibody. As a result, a substantial level of β-catenin is associated with TCF-4 in vehicle-treated cells: however, capsaicin treatment abolished the association between β-catenin and TCF-4 in all three human colorectal cancer cells (Fig. 7A, B, C).
Fig. 7.
Decreased expression of TCF-4 by capsaicin treatment. (A, B, C) Human colorectal cancer cells SW480 (A), LoVo (B) and HCT-116 (C) were treated with 0 or 100 μM of capsaicin for 48 h and then cellular protein was pulled down with β-catenin antibody and immunoblot was performed for TCF-4 antibody. (D, E, F) Human colorectal cancer cells SW480 (D), LoVo (E) and HCT-116 (F) were treated with 0, 50 or 100 μM of capsaicin for 24 or 48 h. Cell lysates were harvested and subjected to SDS-PAGE. Western blot was performed using antibodies against TCF-4 and actin.
We also sought to determine the changes of TCF-4 expression after capsaicin treatment. As shown in Fig. 7(D, E, F), TCF4 expression was decreased by capsaicin treatment in human colorectal cancer cells. This result indicates that the capsaicin-mediated decrease of TCF-4 expression blocks the β-catenin-TCF4 interaction.
4. DISCUSSION
Hot chili red peppers are among the most heavily and frequently consumed spices. Capsaicin found in these peppers has been subjected to extensive experimental and clinical investigations due to its prominent pharmacologic and toxicological properties [37]. In a previous study, we observed that capsaicin treatment significantly induced growth arrest and apoptosis of human colorectal cancer cells [16]. However, the underlying mechanisms by which capsaicin affects human colorectal carcinoma have been only partially determined.
Deregulation of β-catenin/TCF-dependent signaling is an important event in the development of various malignancies, including colorectal and other types of cancer. In most colorectal cancer cells, the β-catenin/TCF pathway is constitutively active at a high level due to defective APC or β-catenin genes and plays a crucial role in the progression of a subset of these cancers, suggesting an important target in the control of cellular proliferation or cell death. Therefore, we focused on β-catenin expression as an anti-proliferative target of capsaicin. For the first time, our data reveal that expression of β-catenin is suppressed by capsaicin treatment in APC mutant human colorectal cancer cells in which the β-catenin pathway is active.
In this study, we observed that capsaicin down-regulates β-catenin transcription as well as protein stability. Simultaneous transcriptional and post-translational modulation of β-catenin has been reported previously by other research groups. Treatment with indomethacin or activation of cGMP-dependent protein kinase in human colorectal cancer cells suppressed β-catenin expression via transcriptional as well as post-translational modification [38, 39]. Although marked increases in the levels of mRNA and promoter activity of the CTNNB1 gene were found in the carcinomas compared with the non-neoplastic mucosa [40–42], very little data looks at the regulation of β-catenin expression at the transcriptional level. In this report, we found that capsaicin reduced β-catenin expression through down-regulation of β-catenin mRNA expression in SW480 cells (Fig. 5). The promoter region of the gene encoding the b-catenin protein contains binding sites for several important transcription factors, in human, rat, and mouse [43]. Protein/DNA array analyses identified several of these transcription factors for the rat Ctnnb1 promoter, including E2F1, NFkB, MEF1, Smad3/4, and GATA [43]. So, mechanistic studies for transcriptional down-regulation of the β-catenin gene by capsaicin are required in the future. β-catenin mRNA was decreased by 40% and 60% whereas promoter activity was decreased by 16% and 41% in 50 and 100 μM capsaicin-treated cells, respectively (Fig. 5A, B). The reason of discrepancy between mRNA and promoter activity is probably that capsaicin affects β-catenin mRNA stability or that the promoter used in this study may not contain all the necessary regulatory elements for β-catenin transcription.
In addition to transcriptional down-regulation, we observed that capsaicin treatment enhanced β-catenin degradation, which is associated with increased ubiquitination of β-catenin (Fig. 6). Since SW480 and LoVo cells contain a mutated APC gene that encodes for a truncated APC protein [44], it is likely that suppression of β-catenin by capsaicin is accomplished via APC-independent, proteasome-mediated pathways [38, 45, 46].
Interestingly, in HCT-116 cells (APC wild type, β-catenin mutant) we observed significant suppression of β-catenin transcriptional activity (Fig. 2C) without reduction of the β-catenin level (Fig. 3C) or alteration of β-catenin distribution between the nucleus and cytosol (data not shown) upon treatment with capsaicin. This rules out the possibility that the capsaicin interference with b-catenin/TCF-dependent transcription is mediated by regulating the total amount of β-catenin and/or its cellular distribution. Thus, we tested the possibility that other molecules associated with regulation of β-catenin transcriptional activity may be altered under the influence of capsaicin. As a result, we observed that capsaicin suppressed TCF-4 expression and disrupted protein-protein interaction between β-catenin and TCF-4 in HCT-116 cells (Fig. 7). Thus, the possible explanation for discrepancy between impaired transcriptional activity and no alteration of β-catenin is that capsaicin directly inhibits TCF-4 expression and interferes with the formation of a transcriptionally active complex between β-catenin and TCF-4. Because TCF-4 has been shown to be constitutively activated by mutated β-catenin and induction of the pro-apoptotic pathway directly leads to the reduction of TCF-4 mRNA and protein levels [47], TCF-4 could be a therapeutic target for anti-cancer drugs. One aspect remaining unresolved in this study is the detailed mechanism of how capsaicin down regulates TCF-4 expression. This needs to be elucidated in a future study.
We do not yet know the precise reason(s) as to why HCT-116 cells are resistant to a decrease of β-catenin protein in response to capsaicin treatment. One speculation could be that mutation of β-catenin in HCT-116 cells causes resistance of β-catenin degradation to capsaicin. It has been known that HCT-116 cells possess loss of conserved serine residue (Ser45), which leads to activating mutations of β-catenin [44, 48]. Because phosphorylation of β-catenin in Ser45 residue by CK1 primes β-catenin for subsequent phosphorylation by GSK-3 [49], we speculate that deficiency of β-catenin phosphorylation at Ser45 in HCT-116 cells causes resistance to β-catenin degradation.
The effect of capsaicin on β-catenin/TCF-dependent gene transcription can be important for capsaicin-induced anti-tumorigenesis. One established downstream target of β-catenin/TCF transcription is cyclin D1, an important cell-cycle regulator. However, our results indicate that reduction in cyclin D1 protein levels is independent of downregulation of b-catenin because loss of cyclin D1 protein occurred 12 h prior to the loss of β-catenin in time-course studies (Fig 3D,E). In this study, we also observed that TCF-4 was decreased at 24 h after capsaicin treatment, earlier than β-catenin (Fig. 7DF) and transcriptional activity of β-catenin is suppressed in the cells treated with 100 μM of capsaicin for 24 h (data not shown). Taken together, these data indicate that the decrease of TCF-4 by capsaicin treatment is more likely responsible than β-catenin loss for suppression of transcriptional activity of β-catenin/TCF-driven gene expression such as cyclin D1. However, we do not exclude the possibility that reduction of cyclin D1 could be a consequence of multiple mechanisms including proteasome degradation because cyclin D1 is a target of proteasomal degration by various compounds including 6-gingerol [32][32], curcumin [50], retinoic acid [51], and troglitazone [52]. Although we did not compare cell cycles in this study, it has been reported that capsaicin results in sustained suppression of cyclin D1 levels and consequently the inhibition of G1 to S transitions [10‒12].
The concentration used in this study (100 μM) is equivalent to those used in several other studies using human colorectal cancer cells in vitro [7, 17, 18]. We do not know the exact physiological concentration of capsaicin and effective in vivo dose to suppress colon cancer in humans. There is much concern that concentration used in in vitro are relevant in vivo. Thus, prediction of relevant in vitro doses should be considered with couples of factors including bioavailability, potential active metabolites and local concentration.
Vanilloid receptor-1 (VR-1) is a well known receptor of capsaicin and mediates capsaicin's biological roles including anti-cancer activity [53]. Capsaicin is also known to mediate apoptosis through a PPARγ-dependent pathway [19], which also down-regulates cyclin D1 expression [54]. Because we observed that human colorectal cancer cells express VR-1 and capsaicin is a ligand of PPARγ (data not shown), we tested whether capsaicin-mediated β-catenin suppression is mediated by these two pathways by treatment of cells with selective inhibitors against VR-1 (capsazepine;CPZ) or PPARγ (GW9662). The result indicated that capsaicin down-regulates β-catenin and cyclin D1 via a VR-1- and PPARγ-independent pathway (data not shown), consistent with other studies reporting no association between VR-1 or PPARγ and capsaicin-mediated carcinogenesis [14, 19, 55]. However, Kim et al. (2004) claimed that capsaicin-induced apoptotic cell death is mediated by the PPARγ pathway in HT-29 human colorectal cancer cells [19]. Discrepancy between PPARγ-dependent apoptosis and independent β-catenin suppression is not clearly demonstrated, but it is likely due to differences of cell type and study context.
In conclusion, we identified β-catenin/TCF-4 mediated transcription as a target of capsaicin. Capsaicin-mediated suppression of β-catenin transcriptional activity is associated with multiple mechanisms including transcriptional down-regulation of the β-catenin gene and enhanced protein degradation in APC-mutant, β-catenin wild type human cancer cells and suppression of TCF4 in APC-wild type and β-catenin mutant human colorectal cancer cells. The current study will help to explain some features of capsaicin-mediated chemoprevention in human colorectal cancer.
ACKNOWLEDGEMENT
We thank Misty Bailey for her critical reading of manuscript. This work was supported by grant from the National Institutes of Health (R03CA137755) to S-HL. This work was also partially supported by grant from National Institutes of Health (R01CA108975) to SJB and grant from National Institutes of Health (CA122959, CA090890) to RHD.
Grant Source: This work was supported by an NCI/NIH grant (R03CA137755) to S-HL.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108. doi: 10.3322/canjclin.55.2.74. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 3.COMA: Nutritional Aspects of the Development of Cancer. Health Education Authority; London: 1998. [Google Scholar]
- 4.Chu YF, Sun J, Wu X, Liu RH. Antioxidant and antiproliferative activities of common vegetables. J Agric Food Chem. 2002;50:6910–6916. doi: 10.1021/jf020665f. [DOI] [PubMed] [Google Scholar]
- 5.Lucier G, Jerardo A. Vegetables and melons outlook. US Department of Agriculture Economic Research Service; Washington, DC: 2007. Publication VGS-313. [Google Scholar]
- 6.Yoshitani SI, Tanaka T, Kohno H, Takashima S. Chemoprevention of azoxymethane-induced rat colon carcinogenesis by dietary capsaicin and rotenone. Int J Oncol. 2001;19:929–939. doi: 10.3892/ijo.19.5.929. [DOI] [PubMed] [Google Scholar]
- 7.Kim YM, Hwang JT, Kwak DW, Lee YK, Park OJ. Involvement of AMPK signaling cascade in capsaicin-induced apoptosis of HT-29 colon cancer cells. Ann N Y Acad Sci. 2007;1095:496–503. doi: 10.1196/annals.1397.053. [DOI] [PubMed] [Google Scholar]
- 8.Wu CC, Lin JP, Yang JS, Chou ST, Chen SC, Lin YT, et al. Capsaicin induced cell cycle arrest and apoptosis in human esophagus epidermoid carcinoma CE 81T/VGH cells through the elevation of intracellular reactive oxygen species and Ca2+ productions and caspase-3 activation. Mutat Res. 2006;601:71–82. doi: 10.1016/j.mrfmmm.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Ito K, Nakazato T, Yamato K, Miyakawa Y, Yamada T, Hozumi N, et al. Induction of apoptosis in leukemic cells by homovanillic acid derivative, capsaicin, through oxidative stress: implication of phosphorylation of p53 at Ser-15 residue by reactive oxygen species. Cancer Res. 2004;64:1071–1078. doi: 10.1158/0008-5472.can-03-1670. [DOI] [PubMed] [Google Scholar]
- 10.Mori A, Lehmann S, O'Kelly J, Kumagai T, Desmond JC, Pervan M, et al. Capsaicin, a component of red peppers, inhibits the growth of androgen-independent, p53 mutant prostate cancer cells. Cancer Res. 2006;66:3222–3229. doi: 10.1158/0008-5472.CAN-05-0087. [DOI] [PubMed] [Google Scholar]
- 11.Brown KC, Witte TR, Hardman WE, Luo H, Chen YC, Carpenter AB, et al. Capsaicin displays anti-proliferative activity against human small cell lung cancer in cell culture and nude mice models via the E2F pathway. PLoS One. 2010;5:e10243. doi: 10.1371/journal.pone.0010243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thoennissen NH, O'Kelly J, Lu D, Iwanski GB, La DT, Abbassi S, et al. Capsaicin causes cell-cycle arrest and apoptosis in ER-positive and -negative breast cancer cells by modulating the EGFR/HER-2 pathway. Oncogene. 2010;29:285–296. doi: 10.1038/onc.2009.335. [DOI] [PubMed] [Google Scholar]
- 13.Zhang R, Humphreys I, Sahu RP, Shi Y, Srivastava SK. In vitro and in vivo induction of apoptosis by capsaicin in pancreatic cancer cells is mediated through ROS generation and mitochondrial death pathway. Apoptosis. 2008;13:1465–1478. doi: 10.1007/s10495-008-0278-6. [DOI] [PubMed] [Google Scholar]
- 14.Hwang MK, Bode AM, Byun S, Song NR, Lee HJ, Lee KW, et al. Cocarcinogenic effect of capsaicin involves activation of EGFR signaling but not TRPV1. Cancer Res. 2010;70:6859–6869. doi: 10.1158/0008-5472.CAN-09-4393. [DOI] [PubMed] [Google Scholar]
- 15.Agrawal RC, Wiessler M, Hecker E, Bhide SV. Tumour-promoting effect of chilli extract in BALB/c mice. Int J Cancer. 1986;38:689–695. doi: 10.1002/ijc.2910380512. [DOI] [PubMed] [Google Scholar]
- 16.Lee SH, Krisanapun C, Baek SJ. NSAID-activated gene-1 as a molecular target for capsaicin-induced apoptosis through a novel molecular mechanism involving GSK3{beta}, C/EBP{beta}, and ATF3. Carcinogenesis. 2010;31:719–728. doi: 10.1093/carcin/bgq016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang KM, Pyo JO, Kim GY, Yu R, Han IS, Ju SA, et al. Capsaicin induces apoptosis by generating reactive oxygen species and disrupting mitochondrial transmembrane potential in human colon cancer cell lines. Cell Mol Biol Lett. 2009;14:497–510. doi: 10.2478/s11658-009-0016-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim MY, Trudel LJ, Wogan GN. Apoptosis induced by capsaicin and resveratrol in colon carcinoma cells requires nitric oxide production and caspase activation. Anticancer Res. 2009;29:3733–3740. [PubMed] [Google Scholar]
- 19.Kim CS, Park WH, Park JY, Kang JH, Kim MO, Kawada T, et al. Capsaicin, a spicy component of hot pepper, induces apoptosis by activation of the peroxisome proliferator-activated receptor gamma in HT-29 human colon cancer cells. J Med Food. 2004;7:267–273. doi: 10.1089/jmf.2004.7.267. [DOI] [PubMed] [Google Scholar]
- 20.Min JK, Han KY, Kim EC, Kim YM, Lee SW, Kim OH, et al. Capsaicin inhibits in vitro and in vivo angiogenesis. Cancer Res. 2004;64:644–651. doi: 10.1158/0008-5472.can-03-3250. [DOI] [PubMed] [Google Scholar]
- 21.Chow J, Norng M, Zhang J, Chai J. TRPV6 mediates capsaicin-induced apoptosis in gastric cancer cells--Mechanisms behind a possible new “hot” cancer treatment. Biochim Biophys Acta. 2007;1773:565–576. doi: 10.1016/j.bbamcr.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 22.Maity R, Sharma J, Jana NR. Capsaicin induces apoptosis through ubiquitinproteasome system dysfunction. J Cell Biochem. 2010;109:933–942. doi: 10.1002/jcb.22469. [DOI] [PubMed] [Google Scholar]
- 23.Bienz M. APC: the plot thickens. Curr Opin Genet Dev. 1999;9:595–603. doi: 10.1016/s0959-437x(99)00016-7. [DOI] [PubMed] [Google Scholar]
- 24.Tetsu O, McCormick F. Beta-catenin regulates expression of cyclin D1 in colon carcinoma cells. Nature. 1999;398:422–426. doi: 10.1038/18884. [DOI] [PubMed] [Google Scholar]
- 25.He TC, Sparks AB, Rago C, Hermeking H, Zawel L, da Costa LT, et al. Identification of c-MYC as a target of the APC pathway. Science. 1998;281:1509–1512. doi: 10.1126/science.281.5382.1509. [DOI] [PubMed] [Google Scholar]
- 26.He TC, Chan TA, Vogelstein B, Kinzler KW. PPARdelta is an APC-regulated target of nonsteroidal anti-inflammatory drugs. Cell. 1999;99:335–345. doi: 10.1016/s0092-8674(00)81664-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van de Wetering M, Sancho E, Verweij C, de Lau W, Oving I, Hurlstone A, et al. The beta-catenin/TCF-4 complex imposes a crypt progenitor phenotype on colorectal cancer cells. Cell. 2002;111:241–250. doi: 10.1016/s0092-8674(02)01014-0. [DOI] [PubMed] [Google Scholar]
- 28.Jaiswal AS, Marlow BP, Gupta N, Narayan S. Beta-catenin-mediated transactivation and cell-cell adhesion pathways are important in curcumin (diferuylmethane)-induced growth arrest and apoptosis in colon cancer cells. Oncogene. 2002;21:8414–8427. doi: 10.1038/sj.onc.1205947. [DOI] [PubMed] [Google Scholar]
- 29.Bocca C, Bozzo F, Francica S, Colombatto S, Miglietta A. Involvement of PPARgamma and E-cadherin/beta-catenin pathway in the antiproliferative effect of conjugated linoleic acid in MCF-7 cells. Int J Cancer. 2007;121:248–256. doi: 10.1002/ijc.22646. [DOI] [PubMed] [Google Scholar]
- 30.Dashwood WM, Orner GA, Dashwood RH. Inhibition of beta-catenin/Tcf activity by white tea, green tea, and epigallocatechin-3-gallate (EGCG): minor contribution of H(2)O(2) at physiologically relevant EGCG concentrations. Biochem Biophys Res Commun. 2002;296:584–588. doi: 10.1016/s0006-291x(02)00914-2. [DOI] [PubMed] [Google Scholar]
- 31.Lee SH, Yamaguchi K, Kim JS, Eling TE, Safe S, Park Y, et al. Conjugated linoleic acid stimulates an anti-tumorigenic protein NAG-1 in an isomer specific manner. Carcinogenesis. 2006;27:972–981. doi: 10.1093/carcin/bgi268. [DOI] [PubMed] [Google Scholar]
- 32.Lee S-H, Cekanova M, Baek SJ. Multiple mechanisms are involved in 6-gingerol-induced cell growth arrest and apoptosis in human colorectal cancer cells. Molecular Carcinogenesis. 2008;47:197–208. doi: 10.1002/mc.20374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee SH, Bahn JH, Whitlock NC, Baek SJ. Activating transcription factor 2 (ATF2) controls tolfenamic acid-induced ATF3 expression via MAP kinase pathways. Oncogene. 2010;29:5182–5192. doi: 10.1038/onc.2010.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nelson WJ, Nusse R. Convergence of Wnt, beta-catenin, and cadherin pathways. Science. 2004;303:1483–1487. doi: 10.1126/science.1094291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shtutman M, Zhurinsky J, Simcha I, Albanese C, D'Amico M, Pestell R, et al. The cyclin D1 gene is a target of the beta-catenin/LEF-1 pathway. Proc Natl Acad Sci USA. 1999;96:5522–5527. doi: 10.1073/pnas.96.10.5522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aberle H, Bauer A, Stappert J, Kispert A, Kemler R. beta-catenin is a target for the ubiquitin-proteasome pathway. EMBO J. 1997;16:3797–3804. doi: 10.1093/emboj/16.13.3797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Surh YJ. More than spice: capsaicin in hot chili peppers makes tumor cells commit suicide. J Natl Cancer Inst. 2002;94:1263–1265. doi: 10.1093/jnci/94.17.1263. [DOI] [PubMed] [Google Scholar]
- 38.Hawcroft G, D'Amico M, Albanese C, Markham AF, Pestell RG, Hull MA. Indomethacin induces differential expression of beta-catenin, gamma-catenin and T-cell factor target genes in human colorectal cancer cells. Carcinogenesis. 2002;23:107–114. doi: 10.1093/carcin/23.1.107. [DOI] [PubMed] [Google Scholar]
- 39.Kwon IK, Wang R, Thangaraju M, Shuang H, Liu K, Dashwood R, et al. PKG inhibits TCF signaling in colon cancer cells by blocking beta-catenin expression and activating FOXO4. Oncogene. 2010;29:3423–3434. doi: 10.1038/onc.2010.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.El-Bahrawy MA, Poulsom R, Jeffery R, Talbot I, Alison MR. The expression of E-cadherin and catenins in sporadic colorectal carcinoma. Hum Pathol. 2001;32:1216–1224. doi: 10.1053/hupa.2001.28948. [DOI] [PubMed] [Google Scholar]
- 41.El-Bahrawy MA, Talbot IC, Poulsom R, Jeffery R, Alison MR. The expression of E-cadherin and catenins in colorectal tumours from familial adenomatous polyposis patients. J Pathol. 2002;198:69–76. doi: 10.1002/path.1168. [DOI] [PubMed] [Google Scholar]
- 42.Wang R, Dashwood WM, Lohr CV, Fischer KA, Pereira CB, Louderback M, et al. Protective versus promotional effects of white tea and caffeine on PhIP-induced tumorigenesis and beta-catenin expression in the rat. Carcinogenesis. 2008;29:834–839. doi: 10.1093/carcin/bgn051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li Q, Dashwood WM, Zhong X, Al-Fageeh M, Dashwood RH. Cloning of the rat beta-catenin gene (Ctnnb1) promoter and its functional analysis compared with the Catnb and CTNNB1 promoters. Genomics. 2004;83:231–242. doi: 10.1016/j.ygeno.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 44.Morin PJ, Sparks AB, Korinek V, Barker N, Clevers H, Vogelstein B, et al. Activation of beta-catenin-Tcf signaling in colon cancer by mutations in beta-catenin or APC. Science. 1997;275:1787–1790. doi: 10.1126/science.275.5307.1787. [DOI] [PubMed] [Google Scholar]
- 45.Sharma C, Pradeep A, Wong L, Rana A, Rana B. Peroxisome proliferator-activated receptor gamma activation can regulate beta-catenin levels via a proteasome-mediated and adenomatous polyposis coli-independent pathway. J Biol Chem. 2004;279:35583–35594. doi: 10.1074/jbc.M403143200. [DOI] [PubMed] [Google Scholar]
- 46.Xiao JH, Ghosn C, Hinchman C, Forbes C, Wang J, Snider N, et al. Adenomatous polyposis coli (APC)-independent regulation of beta-catenin degradation via a retinoid X receptor-mediated pathway. J Biol Chem. 2003;278:29954–29962. doi: 10.1074/jbc.M304761200. [DOI] [PubMed] [Google Scholar]
- 47.Rother K, Johne C, Spiesbach K, Haugwitz U, Tschop K, Wasner M, et al. Identification of Tcf-4 as a transcriptional target of p53 signalling. Oncogene. 2004;23:3376–3384. doi: 10.1038/sj.onc.1207464. [DOI] [PubMed] [Google Scholar]
- 48.Sparks AB, Morin PJ, Vogelstein B, Kinzler KW. Mutational analysis of the APC/beta-catenin/Tcf pathway in colorectal cancer. Cancer Res. 1998;58:1130–1134. [PubMed] [Google Scholar]
- 49.Liu C, Li Y, Semenov M, Han C, Baeg GH, Tan Y, et al. Control of beta-catenin phosphorylation/degradation by a dual-kinase mechanism. Cell. 2002;108:837–847. doi: 10.1016/s0092-8674(02)00685-2. [DOI] [PubMed] [Google Scholar]
- 50.Mukhopadhyay A, Banerjee S, Stafford LJ, Xia C, Liu M, Aggarwal BB. Curcumin-induced suppression of cell proliferation correlates with down-regulation of cyclin D1 expression and CDK4-mediated retinoblastoma protein phosphorylation. Oncogene. 2002;21:8852–8861. doi: 10.1038/sj.onc.1206048. [DOI] [PubMed] [Google Scholar]
- 51.Spinella MJ, Freemantle SJ, Sekula D, Chang JH, Christie AJ, Dmitrovsky E. Retinoic acid promotes ubiquitination and proteolysis of cyclin D1 during induced tumor cell differentiation. J Biol Chem. 1999;274:22013–22018. doi: 10.1074/jbc.274.31.22013. [DOI] [PubMed] [Google Scholar]
- 52.Huang JW, Shiau CW, Yang YT, Kulp SK, Chen KF, Brueggemeier RW, et al. Peroxisome proliferator-activated receptor gamma-independent ablation of cyclin D1 by thiazolidinediones and their derivatives in breast cancer cells. Mol Pharmacol. 2005;67:1342–1348. doi: 10.1124/mol.104.007732. [DOI] [PubMed] [Google Scholar]
- 53.Amantini C, Ballarini P, Caprodossi S, Nabissi M, Morelli MB, Lucciarini R, et al. Triggering of transient receptor potential vanilloid type 1 (TRPV1) by capsaicin induces Fas/CD95-mediated apoptosis of urothelial cancer cells in an ATM-dependent manner. Carcinogenesis. 2009;30:1320–1329. doi: 10.1093/carcin/bgp138. [DOI] [PubMed] [Google Scholar]
- 54.Qin C, Burghardt R, Smith R, Wormke M, Stewart J, Safe S. Peroxisome proliferator-activated receptor gamma agonists induce proteasome-dependent degradation of cyclin D1 and estrogen receptor alpha in MCF-7 breast cancer cells. Cancer Res. 2003;63:958–964. [PubMed] [Google Scholar]
- 55.Athanasiou A, Smith PA, Vakilpour S, Kumaran NM, Turner AE, Bagiokou D, et al. Vanilloid receptor agonists and antagonists are mitochondrial inhibitors: how vanilloids cause non-vanilloid receptor mediated cell death. Biochem Biophys Res Commun. 2007;354:50–55. doi: 10.1016/j.bbrc.2006.12.179. [DOI] [PubMed] [Google Scholar]