Abstract
Background
The electronic medical record (EMR)/electronic health record (EHR) is becoming an integral component of many primary-care outpatient practices. Before implementing an EMR/EHR system, primary-care practices should have an understanding of the potential benefits and limitations.
Objective
The objective of this study was to systematically review the recent literature around the impact of the EMR/EHR within primary-care outpatient practices.
Materials and methods
Searches of Medline, EMBASE, CINAHL, ABI Inform, and Cochrane Library were conducted to identify articles published between January 1998 and January 2010. The gray literature and reference lists of included articles were also searched. 30 studies met inclusion criteria.
Results and discussion
The EMR/EHR appears to have structural and process benefits, but the impact on clinical outcomes is less clear. Using Donabedian's framework, five articles focused on the impact on healthcare structure, 21 explored healthcare process issues, and four focused on health-related outcomes.
Keywords: Clinical informatics, quality of healthcare, systematic review, machine learning, health data standards, vocabulary, ontology, scientific information and health data policy, consumer health/patient education information, information retrieval, NLP, public health informatics, clinical trials, electronic medical records, primary care, systematic review
Introduction and background
The electronic medical record (EMR)/electronic health record (EHR) is becoming an integral component of many primary-care outpatient practices. Several countries have implemented successful programs to promote the use of the EMR/EHR within primary care, and the financial commitment by governments to support health information technology continues to grow.1–4 The perception is that the EMR/EHR will reduce healthcare costs and improve the quality of healthcare provided.1 5 6 However, studies exploring the impact on care, which included both specialty and primary care, have found that the EMR/EHR has had mixed success at decreasing costs and improving the quality of ambulatory care services.7–10 Reviews that have explored the value of different components of the EMR/EHR have also found only marginal benefits. There is modest evidence that computerized physician order entry (CPOE) decreases prescribing errors.11 However, it appears that it is mostly minor errors that are decreased, and CPOE may actually increase duplicate orders and result in failures to discontinue medications. A review of electronic reminder systems found only a small improvement in adherence to processes of care, with a trend toward larger improvements when clinicians were required to enter a response.12 A review of electronic strategies to improve dosage selection when prescribing found some improved clinical outcomes, such as a decrease in rates of toxic drug levels and a decrease in hospital length of stay.13
Before implementing an EMR/EHR system, primary-care practices should have an understanding of the potential benefits and limitations such systems may have on their practice. To help address this, we sought to systematically review the recent literature around the impact of the EMR/EHR within primary-care outpatient practices. We chose to focus on studies examining the effectiveness or benefits of the EMR/EHR broadly, and considering the impact on healthcare structure, process, and outcomes.
Selection and inclusion criteria
Literature search strategy
Searches of Medline, EMBASE, CINAHL, ABI Inform, and Cochrane Library were completed to identify English-language articles published between January 1998 and January 2010 inclusive, which involved primary-care outpatient practices and EHRs or EMRs. Given how rapidly technology evolves, we choose to only review articles published within the past 10 years, as they were felt to be most relevant. The search strategies included terms such as: electronic or computer or internet, CPOE or EHR or EPR, ambulatory care or outpatient or primary-care or family doctor, and decision-support system. A detailed description of the search strategies used is available from the authors. A search of the gray literature was conducted with the assistance of a research librarian with expertise in systematic reviews. This involved reviewing the websites of 62 related organizations, identified from global government and institute websites and databases, for articles published and posted between January 2009 and April/May 2009. Additional articles were identified from searching the reference lists of retrieved articles.
Study selection
We excluded articles that were published before 1998, were not published in English, did not focus primarily on family doctors or primary-care outpatient practices, did not focus on evaluating the effectiveness or benefits of the EMR/EHR, or focused on only one component of the EMR/EHR. Previous systematic reviews have already focused on various components of the EMR/EHR (eg, CPOE; reminders).11 12 Additionally, when implementing an EMR/EHR system, clinicians are initially interested in the overall impact of the system. The role for specific items, such as electronic clinical decision-support strategies, is often a secondary consideration.
We chose to accept the definition of EMR/EHR supplied by the authors. Given the non-uniformity in the use of terminology, the terms EMR and EHR were used synonymously in this review. The definition of primary care used considered differences in the healthcare structure between countries; specifically studies originating from the USA that included general internists practicing within the community were included. We did not restrict by study design, but quantitative (primary data or appropriate summary statistics) and/or qualitative results had to be available.
Two authors independently reviewed the abstracts to select relevant publications that met the inclusion criteria. Disagreements were resolved by a third reviewer or by retrieving the full text article for review (371/4773 abstracts=8%). Two authors then independently reviewed all full text articles to confirm that inclusion criteria were met. A third reviewer resolved disagreements (52/383 articles=14%).
Data extraction and analysis
Two authors independently extracted data from the included studies using a standardized form that was piloted by the authors on an initial sample of articles. Information was extracted pertaining to study design, study population and size, clinical setting, outcomes, and results. A meta-analysis was not conducted due to the clinical heterogeneity between included articles. Instead, a summary of the data is presented.
Findings
Study characteristics
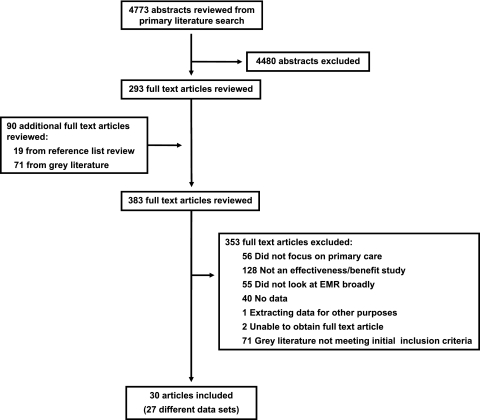
The primary search identified 4773 citations, of which 293 were retrieved for full text review. A further 71 articles were found from searching the gray literature and 19 from searching the reference lists of retrieved articles. Thirty studies met inclusion criteria for data extraction and synthesis (figure 1).
Figure 1.
Literature search results.
We categorized the articles according to Donabedian's framework, considering how the EMR/EHR impacted healthcare structure, process, and outcomes. Among the included studies, five articles focused on the impact on structure,14–18 21 explored process issues,19–39 and four focused on outcomes40–43 (table 1 as an online data supplement at http://www.jamia.org/).
Impact of the EMR/EHR on healthcare-system structure
Four studies compared the EMR/EHR to paper records; three were case–control studies,14–16 and one was a cross-sectional survey.18 These studies involved primary-care practices in the UK and the USA. The fifth study was a chart review from Finland that focused solely on the EMR/EHR.17
A case–control study involving 53 primary-care practitioners (25 with an EMR/EHR and 28 with paper records) in the UK revealed that legibility of the EMR/EHR was not an issue, while 36% of the paper records were at least partially illegible (p<0.0001).15 Although the EMR/EHR contained more words (p<0.0001), there were no differences in terms of the proportion of charts with an entry (p=0.25) or with a documented encounter reason (p=0.56). A similar case–control study involving 18 practices (1396 patients) in the UK also found no significant difference in the number of visits recorded between EMR/EHR and paper-based practices.14
A case–control study conducted among six physicians (238 encounters) in the USA found that the three physicians using an EMR/EHR checked and clarified information (p<0.01), encouraged patient questions (p<0.005), and ensured completeness of the encounter (p<0.005) more often than the three using a paper record.16 There was no significant difference in the mean visit time or number of laboratory tests ordered between the two groups of physicians, but the physicians using an EMR/EHR spent more time with new patients (mean of 35.2 min vs 25.6 min; p<0.05). In both groups, there were often long periods of silence while physicians entered data or checked the chart for information.
A survey of primary-care practices in the mid-Western USA (response rate=42% (628/1482)) found that 143 (23.6%) used an EMR/EHR.18 After adjusting for belonging to a larger organization, EMR/EHR users had greater odds of believing their medical records were up to date (OR=2.12; 95% CI 1.29 to 3.45), modifiable to meet individual needs (OR=1.60; 95% CI 1.03 to 2.49), and accessible (OR=2.49; 95% CI 1.58 to 3.92). EMR/EHR users were also more satisfied with their medical record system (OR=2.36; 95% CI 1.58 to 3.54).
A retrospective chart review involving 50 primary-care physicians (175 patient records) in Finland found that the quality of the EMR/EHR record was rated ‘good’ in only 20% of patient records.17 However, the quality of the record was not associated with the quality of the encounter. Instead, the quality of the record was dependent on the electronic system used.
Impact of the EMR/EHR on healthcare processes
The impact of the EMR/EHR on clinical processes was assessed in 17 articles (14 different data sets)19–23 28–39 (online table 1). These studies involved surveys, focus groups, chart and database reviews, and/or interviews.
Survey data gathered in early 1997 prior to implementation of an EMR/EHR at seven ambulatory clinics in the Eastern USA revealed that overall expectations were positive, with most perceiving that the EMR/EHR would be helpful.29 Although anxiety about computers was low overall, there was a positive relationship between prior computer experience and expected utility. Respondents expressed fears about system downtime and about it depersonalizing the patient encounter. Among the six clinics (22 physicians) involved in postimplementation surveys completed by the end of June 1998 (with matched pre- and postsurvey results from 12 physicians at three sites), following initial EMR/EHR implementation a significant decline was noticed in ratings of time saving (longer to get into the electronic record; support staff tasks transferred to physicians), perceived productivity (less lost charts and easier access but increased time charting), and perceived quality of care (legibility improved but chart accuracy questioned).28
When surveyed serially over the first year of EMR/EHR implementation, 86 primary-care clinicians in the Eastern USA (response rate=82–95%) changed many of their perceptions of the EMR over time.38 Specifically, increasing numbers perceived improvements in quality of care (63–86%; p<0.001), reductions in medication-related errors (72–81%; p=0.03), improvement in communication among clinicians (72–93%; p<0.001), and improved follow-up of test results (62–87%; p<0.001). Similarly, a decreasing number reported a perceived negative impact on the quality (49–33%; p=0.001) and duration of patient encounters (68–51%; p=0.001). Although the EMR/EHR was initially perceived to increase time spent on documentation, this perception decreased over time (78–68%; p=0.006). A retrospective analysis of data from a large health maintenance organization in the USA identified that implementation of an EMR (which included secured email messages and was coupled with scheduled telephone visits) decreased actual annual primary-care office visits from 2.2 per patient to 1.7 per patient over 3 years.39
Provider satisfaction with the EMR/EHR was similarly explored among primary-care physicians in Norway.31–33 This study involved focus groups (24 physicians in three focus groups), observations (11 physicians in 80 observed encounters), and a validated mailed questionnaire conducted in 2003 (response rate=73% (247/338)). Primary-care physicians in Norway felt that, although overall the EMR/EHR saved time compared to paper, many administrative tasks were now carried out by the physicians.32 The EMR/EHR was easy to access but hard to search and efficiently review. The presentation of information within the EMR/EHR was identified as a major issue, including the need to organize notes and results by condition and chronologically, the need for reminders or checklists during the follow-up of chronic conditions, and the need to improve electronic communication between providers.33 Despite this, and that 15% (34/225) reported daily or weekly software or hardware issues, they strongly agreed that the system was worth the time and effort required to use it.31
Similarly, a survey mailed in 2001 to 205 primary-care physicians in Australia (response rate=19% (39/205)) revealed that most believed computers were essential to healthcare (71%), had the potential to improve the quality of care (71%), and improved the way they worked (77%).30 The vast majority surveyed had no university training in computers (95%), and a large number had not received computer training/advice (41%). There were problems with system crashes (97%) and viruses (28%).
Interviews among 13 small primary-care practices in England and Scotland identified that the three most valuable features of an EMR/EHR were e-prescribing, its impact on overall efficiency, and its ability to improve quality.34 Interviews and observations in five primary-care practices (14 physicians) in the Southern USA identified the advantages of an EMR to be the ability of multiple users to access records, record legibility and completeness, improved organization, decreased time for documentation, improved communication within the practice, and improved quality of care.35 The limitations identified included downtime, the inability of the system to capture all data, and the time necessary to develop customized templates.
A US national mail survey of primary-care residents (24 family residency programs; 563 residents; 46% response rate) conducted in 1999 identified many of the same benefits and concerns with the EMR/EHR.36 Specifically, residents perceived the EMR/EHR to improve the legibility and access to records. Concerns with the EMR/EHR included issues around privacy and confidentiality, the time needed to enter data, hardware problems, downtime, training, and decreased patient–physician interaction.
Within the US Indian Health Services, 223 clinicians were surveyed via email or telephone about their perceptions of a recently implemented EMR/EHR (response rate=56% (125/223)).37 The EMR/EHR had been implemented within these health centers between June 2003 and December 2005. The majority used the EMR with every encounter (78%), and 35% agreed it improved the quality of care. Identified barriers to implementation were technical difficulties and lost clinical productivity. However, 66% reported geography was a significant barrier to providing high-quality care to this population, and 87% felt the EMR/EHR could improve the quality of care in rural and underserved areas.
Staff interviews before and after partial implementation of an EMR/EHR at one rural primary-care practice (six physicians) in the Eastern USA revealed that staff perceptions of care errors based on hazard scores decreased in some areas and increased in others.21 Specifically, staff perceived decreased hazard in nurse–physician and physician–chart interactions, but increased hazard in domains of physician–patient interactions and nurse–chart interactions.
Quality-of-care measures based on comparison to nationwide performance percentiles for cervical cancer screening, retinal exams among diabetics, and smoking cessation counseling increased only marginally following EMR/EHR implementation in a retrospective record review that included 48 outpatient practices (477 primary-care practitioners) in Colorado and the Northwest USA.20 There was a significant decrease in service use (p<0.0001) with no increase in emergency-department visits or change in the ratio of primary-care providers to patients. Another retrospective chart review in one practice (six physicians; 3740 patients) in the USA found that after implementation of an EMR/HER, the completion rates for preventive care measures increased among adults (28–64% pre; 47–80% post), and immunization rates of children also increased (30–39% pre; 47–56% post).19
A study combining survey data from 2007 with performance data on 13 measures of primary-care quality among 305 practices in the Eastern USA (response rate=74%) demonstrated a positive association between frequent EMR/EHR use and improved cancer (breast and colon; not cervical) and sexually transmitted disease (Chlamydia) screening and improved diabetes care (eye examinations and nephropathy monitoring; not cholesterol or hemoglobin A1C testing).23 There was no association with EMR/EHR use and depression care (acute-phase contacts, treatment) or heathcare overuse (imaging for low-back pain, avoidance of antibiotics for acute bronchitis). Similarly, a cross-sectional survey from 2001 to 2004 involving 506 physicians in the Eastern USA found no difference in performance between 164 EMR/EHR users and 342 non-users in six clinical categories of quality (asthma care, mental health, cancer screening, diabetes care, well-child visit, and women's health).22 There was also no relationship between duration of EMR/EHR use and physician performance.
Four studies explored the impact of the EMR/EHR on patients' experiences with care processes.24–27 Three studies involved patient surveys,25–27 and one was a cross-sectional observational study.24 Three studies were conducted in the USA,24–26 while the fourth was performed in Australia.27
The EMR/EHR impact on patient-centered care was explored in a cross-sectional observational study comparing high usage of the EMR/EHR (>10% of encounter time) versus low usage.24 The study observed 50 encounters with six physicians in the Southern USA. Although there was no difference between the two groups in the number of physician-initiated questions, high usage of the EMR/EHR was associated with a significant increase in the number of questions initiated by patients (p<0.05). High EMR/EHR usage was also associated with significantly more relevant physician responses to patient questions (p<0.05), and encounters were more patient-centered (p=0.07). However, while using the EMR/EHR, physicians would miss non-verbal patient communications.
Three studies surveyed patients regarding their opinion of the impact computers had on patient–physician relationships.25–27 Two studies were conducted in 2003,25 26 while the third occurred in 2000.27 In none of these surveys did there seem to be a perceived negative impact on the patient–physician relationship. However, there was no consensus between studies in terms of the EMR/EHR having a positive impact on care.
Impact of the EMR/EHR on healthcare-related outcomes
Only one study included clinical outcomes.41 It was a cross-sectional analysis of 11 889 visits across the USA that examined the impact of the EMR/EHR on clinical outcomes (blood pressure control) and processes (receipt of appropriate pharmacological therapies for chronic conditions).41 Of 4433 visits, there was no association between blood-pressure control and EMR/EHR components. However, in patients over 65, there was a 54% increased odds of blood pressure control associated with the presence of an electronic reminder system (OR 1.54; 95% CI 1.03 to 2.29). Among the four pharmacological therapies assessed (ASA for ischemic heart disease or stroke; beta-blockers for ischemic heart disease; ACE inhibitors/angiotension receptor blockers for diabetics with hypertension; inhaled steroids for asthmatics), the use of an EMR/EHR was not associated with receipt of appropriate therapy, with the exception of an association between reminder systems and use of ACE inhibitors/angiotension receptor blockers for diabetics with hypertension (OR 2.58; 95% CI 1.22 to 5.42) and an association between electronic physician notes and inhaled steroid use in asthmatics (OR 2.86; 95% CI 1.1.2 to 7.32).
Three articles, all from the USA, explored the financial costs and benefits of the EMR/EHR.40 42 43 One was a cost–benefit analysis using a hypothetical practice,43 while the other two were case reports.40 42 Compared to paper records, a primary-care practitioner with a panel of 2500 patients (75% under 65 years old and of whom 17% under 65 belonged to capitated plans) who implemented an EMR/EHR would see a hypothetical net benefit of US$86 400 over a 5-year period (based on 2002 USA dollars).43 The data on costs and benefits in this analysis came from primary data collected from the authors' EMR, from published studies and/or expert opinion using a modified Delphi technique. In this model, drug expenditures would make up the majority of the savings (33%). The remainder of savings primarily resulted from decreased radiology utilization (17%), decreased billing errors (15%), and improvement in charge capture (15%). This model, which is not a cost-effectiveness analysis, was most sensitive to changes in the proportion of patients in capitated health plans.
In a case report of a primary-care practice network of 260 physicians in the USA implementing an EMR/EHR system, it was estimated from pilot site data that the system would pay for itself within 8 years of implementation.42 It is not known if this projection was realized. At the pilot sites, savings were seen in the areas of chart preparation, billings, triage-nurse phone time, and transcription costs. A second case report involving five office practices (three primary-care offices) in the USA realized cost savings in the areas of chart pulls, new chart creation, filing time, support staff salary, transcription, patient cycle time, completeness of codes billed, and days in accounts receivable.40 Overall, the initial costs of the EMR/EHR were recaptured within 16 months.
Discussion
The EMR/EHR appears to have both positive and negative impacts on primary-care outpatient practices. There are clear advantages over traditional paper-based records in terms of legibility and accessibility. Fears of computers interfering with the patient–physician relationship do not appear to have been realized in our review of the literature. Although not specifically identified as an issue in this review, previous studies have highlighted concerns around the privacy and confidentiality of the EMR/EHR.10 44
Our review of published studies of EMRs/EHRs as a whole confirms results from previous reviews of published studies of EMR/EHR components in that the EMR/EHR appears to have mixed effects on both process and clinical outcomes.11–13 Overall, based on evidence in the literature, the EMR/EHR appears to contribute only marginally to improved health.
Many primary-care physicians appear to perceive a positive impact on the quality of care. However, the impact an EMR/EHR system has on measured quality indicators within primary care appears to be mixed. This is similar to the impact seen within other clinical care settings.8 12 45 46
When first implementing an EMR/EHR, primary-care providers should consider the potential decrease in productivity resulting from the increased time initially spent on documentation. However, this issue appears to lessen over time. Initial adoption of an EMR/EHR system requires allocation of time for learning and training.44 Primary-care practices need to budget for the upfront costs associated with implementation. However, the identified USA-based cost data appear to suggest that cost savings are realized over time. Further studies are needed to determine if cost savings also exist in countries with national healthcare systems. When choosing an EMR/HER, clinicians should also consider issues around clinical decision support, such as how the CPOE and reminder systems are designed.11–13
Within the identified articles, the study designs utilized were relatively weak and observational in nature. There is a need for a more rigorous evaluation of the EMR/EHR within primary-care outpatient practices, particularly as it relates to the impact of the EMR/EHR on outcomes, using pragmatic randomized control trials. Additionally, the current body of literature comes from developed nations. As access to technology expands, and the associated costs decline, the potential role and impact of the EMR/EHR within developing countries need to be explored.
Limitations
Our search was limited to English-language articles published since 1998. This was done for practical reasons and also to present a review of the most recent and relevant literature within a rapidly evolving field. We chose not to explore the specific impact of various components of the EMR/EHR, such as clinical-decision-support resources, as these have been explored by others. Instead, we focused on the value of the EMR/EHR in its entirety. We accepted the EMR/EHR definitions adopted by studies included in this review. These studies could have defined EMR/EHR differently, and it is possible that these definitions were similar to those used in studies excluded from this review. However, the search strategy and criteria for inclusion were broad, so the probability of excluding important studies is low.
Conclusions
The EMR/EHR appears to have both positive and negative impacts on primary-care outpatient practices. The EMR/EHR has structural and process benefits, but the impact on clinical outcomes is less clear. When implementing an EMR/HER, appropriate resources need to be allocated.
Footnotes
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bates DW. Getting in step: electronic health records and their role in care coordination. J Gen Intern Med 2010;25:174–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Purves IN, Sugden B, Booth N, et al. The PRODIGY project—the iterative development of the release one model. Proc AMIA Symp 1999:359–63 [PMC free article] [PubMed] [Google Scholar]
- 3.Mount CD, Kelman CW, Smith LR, et al. An integrated electronic health record and information system for Australia? Med J Aust 2000;172:25–7 [DOI] [PubMed] [Google Scholar]
- 4.Thakurdas P, Coster G, Gurr E, et al. New Zealand general practice computerisation; attitudes and reported behaviour. N Z Med J 1996;109:419–22 [PubMed] [Google Scholar]
- 5.Bates DW, Ebell M, Gotlieb E, et al. A proposal for electronic medical records in US primary care. J Am Med Inform Assoc 2003;10:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bodenheimer T, Grumbach K. Electronic technology: a spark to revitalize primary care? JAMA 2003;290:259–64 [DOI] [PubMed] [Google Scholar]
- 7.Pham HH, Schrag D, Hargraves JL, et al. Delivery of preventive services to older adults by primary care physicians. JAMA 2005;294:473–81 [DOI] [PubMed] [Google Scholar]
- 8.Linder JA, Ma J, Bates DW, et al. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med 2007;167:1400–5 [DOI] [PubMed] [Google Scholar]
- 9.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52 [DOI] [PubMed] [Google Scholar]
- 10.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med 2008;359:50–60 [DOI] [PubMed] [Google Scholar]
- 11.Reckmann MH, Westbrook JI, Koh Y, et al. Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. J Am Med Inform Assoc 2009;16:613–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shojania KG, Jennings A, Mayhew A, et al. Effect of point-of-care computer reminders on physician behaviour: a systematic review. CMAJ 2010;182:E216–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Durieux P, Trinquart L, Colombet I, et al. Computerized advice on drug dosage to improve prescribing practice. Cochrane Database Syst Rev 2008;(3):CD002894. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton WT, Round AP, Sharp D, et al. The quality of record keeping in primary care: a comparison of computerised, paper and hybrid systems. Br J Gen Pract 2003;53:929–33; discussion 33. [PMC free article] [PubMed] [Google Scholar]
- 15.Hippisley-Cox J, Pringle M, Cater R, et al. The electronic patient record in primary care–regression or progression? A cross sectional study. BMJ 2003;326:1439–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makoul G, Curry RH, Tang PC. The use of electronic medical records: communication patterns in outpatient encounters. J Am Med Inform Assoc 2001;8:610–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vainiomaki S, Kuusela M, Vainiomaki P, et al. The quality of electronic patient records in Finnish primary healthcare needs to be improved. Scand J Prim Health Care 2008;26:117–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karsh BT, Beasley JW, Hagenauer ME. Are electronic medical records associated with improved perceptions of the quality of medical records, working conditions, or quality of working life? Behaviour and Information Technology 2004;23:327–35 [Google Scholar]
- 19.Gill JM, Ewen E, Nsereko M. Impact of an electronic medical record on quality of care in a primary care office. Del Med J 2001;73:187–94 [PubMed] [Google Scholar]
- 20.Garrido T, Jamieson L, Zhou Y, et al. Effect of electronic health records in ambulatory care: retrospective, serial, cross sectional study. BMJ 2005;330:581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh R, Servoss T, Kalsman M, et al. Estimating impacts on safety caused by the introduction of electronic medical records in primary care. Inform Prim Care 2004;12:235–41 [DOI] [PubMed] [Google Scholar]
- 22.Zhou L, Soran CS, Jenter CA, et al. The relationship between electronic health record use and quality of care over time. J Am Med Inform Assoc 2009;16:457–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedberg MW, Coltin KL, Safran DG, et al. Associations between structural capabilities of primary care practices and performance on selected quality measures. Ann Intern Med 2009;151:456–63 [DOI] [PubMed] [Google Scholar]
- 24.Arar N, McGrath J, Rosales J, et al. The role of electronic medical records in improving patient-centred care in outpatient encounters. Journal on Information Technology in Healthcare 2004;2:187–202 [Google Scholar]
- 25.Garrison GM, Bernard ME, Rasmussen NH. 21st-century health care: the effect of computer use by physicians on patient satisfaction at a family medicine clinic. Fam Med 2002;34:362–8 [PubMed] [Google Scholar]
- 26.Rouf E, Whittle J, Lu N, et al. Computers in the exam room: differences in physician-patient interaction may be due to physician experience. J Gen Intern Med 2007;22:43–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Callen JL, Bevis M, McIntosh JH. Patients' perceptions of general practitioners using computers during the patient–doctor consultation. HIM J 2005;34:8–12 [DOI] [PubMed] [Google Scholar]
- 28.Gamm LD, Barsukiewicz CK, Dansky KH, et al. Investigating changes in end-user satisfaction with installation of an electronic medical record in ambulatory care settings. J Healthc Inf Manag 1998;12:53–65 [PubMed] [Google Scholar]
- 29.Gamm LD, Barsukiewicz CK, Dansky KH, et al. Pre- and post-control model research on end-users' satisfaction with an electronic medical record: preliminary results. Proc AMIA Symp 1998:225–9 [PMC free article] [PubMed] [Google Scholar]
- 30.Bomba D. Moving beyond implementation to sustained use of computers in general practice in Australia. International Journal in Healthcare Technology and Management 2004;6:83–90 [Google Scholar]
- 31.Christensen T, Faxvaag A, Loerum H, et al. Norwegians GPs' use of electronic patient record systems. Int J Med Inform 2009;78:808–14 [DOI] [PubMed] [Google Scholar]
- 32.Christensen T, Grimsmo A. Instant availability of patient records, but diminished availability of patient information: a multi-method study of GP's use of electronic patient records. BMC Med Inform Decis Mak 2008;8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Christensen T, Grimsmo A. Expectations for the next generation of electronic patient records in primary care: a triangulated study. Inform Prim Care 2008;16:21–8 [DOI] [PubMed] [Google Scholar]
- 34.Schade CP, Sullivan FM, de Lusignan S, et al. e-Prescribing, efficiency, quality: lessons from the computerization of UK family practice. J Am Med Inform Assoc 2006;13:470–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wager KA, Lee FW, White AW, et al. Impact of an electronic medical record system on community-based primary care practices. J Am Board Fam Pract 2000;13:338–48 [PubMed] [Google Scholar]
- 36.Aaronson JW, Murphy-Cullen CL, Chop WM, et al. Electronic medical records: the family practice resident perspective. Fam Med 2001;33:128–32 [PubMed] [Google Scholar]
- 37.Sequist TD, Cullen T, Hays H, et al. Implementation and use of an electronic health record within the Indian Health Service. J Am Med Inform Assoc 2007;14:191–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.El-Kareh R, Gandhi TK, Poon EG, et al. Trends in primary care clinician perceptions of a new electronic health record. J Gen Intern Med 2009;24:464–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chen C, Garrido T, Chock D, et al. The Kaiser Permanente Electronic Health Record: transforming and streamlining modalities of care. Health Aff (Millwood) 2009;28:323–33 [DOI] [PubMed] [Google Scholar]
- 40.Grieger DL, Cohen SH, Krusch DA. A pilot study to document the return on investment for implementing an ambulatory electronic health record at an academic medical center. J Am Coll Surg 2007;205:89–96 [DOI] [PubMed] [Google Scholar]
- 41.Keyhani S, Hebert PL, Ross JS, et al. Electronic health record components and the quality of care. Med Care 2008;46:1267–72 [DOI] [PubMed] [Google Scholar]
- 42.Pifer EA, Smith S, Keever GW. EMR to the rescue. An ambulatory care pilot project shows that data sharing equals cost shaving. Healthc Inform 2001;18:111–14 [PubMed] [Google Scholar]
- 43.Wang SJ, Middleton B, Prosser LA, et al. A cost–benefit analysis of electronic medical records in primary care. Am J Med 2003;114:397–403 [DOI] [PubMed] [Google Scholar]
- 44.Mitchell E, Sullivan F. A descriptive feast but an evaluative famine: systematic review of published articles on primary care computing during 1980-97. BMJ 2001;322:279–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Longhurst CA, Parast L, Sandborg CI, et al. Decrease in hospital-wide mortality rate after implementation of a commercially sold computerized physician order entry system. Pediatrics 2010;126:14–21 [DOI] [PubMed] [Google Scholar]
- 46.Metzger J, Welebob E, Bates DW, et al. Mixed results in the safety performance of computerized physician order entry. Health Aff (Millwood) 2010;29:655–63 [DOI] [PubMed] [Google Scholar]