Abstract
Background
The electronic exchange of health information among healthcare providers has the potential to produce enormous clinical benefits and financial savings, although realizing that potential will be challenging. The American Recovery and Reinvestment Act of 2009 will reward providers for ‘meaningful use’ of electronic health records, including participation in clinical data exchange, but the best ways to do so remain uncertain.
Methods
We analyzed patient visits in one community in which a high proportion of providers were using an electronic health record and participating in data exchange. Using claims data from one large private payer for individuals under age 65 years, we computed the number of visits to a provider which involved transitions in care from other providers as a percentage of total visits. We calculated this ‘transition percentage’ for individual providers and medical groups.
Results
On average, excluding radiology and pathology, approximately 51% of visits involved care transitions between individual providers in the community and 36%–41% involved transitions between medical groups. There was substantial variation in transition percentage across medical specialties, within specialties and across medical groups. Specialists tended to have higher transition percentages and smaller ranges within specialty than primary care physicians, who ranged from 32% to 95% (including transitions involving radiology and pathology). The transition percentages of pediatric practices were similar to those of adult primary care, except that many transitions occurred among pediatric physicians within a single medical group.
Conclusions
Care transition patterns differed substantially by type of practice and should be considered in designing incentives to foster providers' meaningful use of health data exchange services.
Keywords: Health information policy, decision support, machine learning, confidentiality, Patient Safety, decision support, data exchange, editorial Office, health data standards, vocabulary, ontology, scientific information and health data policy, consumer health/patient education information, information retrieval, NLP, public health informatics, clinical trials, health information exchange, health information technology, meaningful use, care coordination
Introduction
Health information exchange (HIE)—the sharing of health-related data across the boundaries of healthcare institutions—is widely expected to be of tremendous value by improving the quality of healthcare and reducing the unnecessary costs of redundant diagnostic tests, among other benefits.1 2
A central function of HIE is facilitating data exchange among healthcare providers working in different locations. Studies suggest a significant need for this type of data exchange.3–6 For example, the typical Medicare beneficiary between 2000 and 2002 saw a median of seven different physicians in four different offices each year, and patients with chronic conditions saw even greater numbers of physicians.3 Within individual episodes of care for many common clinical conditions, multiple physicians are often involved: a median of eight physicians were involved in episodes of acute myocardial infarction for Medicare patients.6
Studies have also demonstrated that the current practices of information exchange could be much better. Primary care physicians reported missing clinical data in 13% of patient visits in one study.4 In another study, focusing on referrals, 28% of primary care physicians and 49% of specialists were dissatisfied with the quality of the information they received from each other.7 Another group of investigators asked physicians if information from specific previous visits was available at the time of a visit and found that information was available for only 22% of previous visits.8 By automating such information pathways, HIE has the potential to facilitate care transitions and improve the care of all patients who visit more than one healthcare provider, which includes the vast majority of patients.
Unfortunately, few HIE organizations currently offer provider-to-provider data exchange functionality. So far, most have focused on more basic forms of HIE such as the delivery of laboratory results.9 A recent study of one of the few HIEs that do offer provider-to-provider exchange for patients in a community found that many factors prevent or inhibit clinicians' HIE usage, suggesting that important areas of HIE functionality may be underutilized and the movement to establish widespread HIE may fall short of realizing its full value.10
The American Recovery and Reinvestment Act of 2009 has the potential to help foster HIE usage by providing incentive payments to eligible healthcare providers for ‘meaningful use’ of health information technology, including HIE. The criteria for receiving the first of three stages of meaningful use payments have already been specified but include minimal HIE requirements.11 Criteria for the remaining stages, to be applied in 2013 and 2015, will likely involve substantial HIE usage requirements, but few studies suggest how meaningful use of HIE should be defined and measured to inform these criteria.10–12
For the final stage of the meaningful use payments, policymakers are interested in promoting ‘access to comprehensive patient data.’11 This may be realized in the form of regional HIEs that offer aggregate patient records: patient-indexed, longitudinal records of electronic health data, integrated from multiple clinical sources. Determining a suitable level of meaningful use of this form of HIE may be challenging because visits that do not involve care transitions—that is, repeat visits to the same provider—would not be opportunities for HIE usage: the HIE would not contain any new clinical information for those visits. This may partly explain why usage may be lower than expected in some operational HIEs.13 14 We investigate the opportunities for using this form of HIE and suggest a simple method of computing the number of visits to a provider in which an aggregate patient record would contain clinical data that the provider had not yet seen, based on whether or not a visit involved a care transition. We propose that some fraction of the number of visits which involve care transitions may serve as a reasonable target for the number of times a clinician might be expected to access an aggregate record HIE. This in turn could be considered in the meaningful use criteria, or related policies, aimed at fostering HIE. To better understand the nature of care transitions in which an aggregate patient record may be used, we explored patient visit patterns in one geographic community and compute descriptive statistics related to care transitions in that community.
Methods
Data sources
We analyzed claims data for members of a large private payer in a small community in New England, data which accounted for approximately 33% of all visits in the community.15 The community had an established HIE with most of its medical groups participating. The data set included all claims, paid and unpaid, from January 1, 2005 through June 20, 2009, which were submitted to the payer by providers who practiced within the six zip codes of the community, as well as claims from providers outside the community that were ascribed to any patient who had at least one claim from a community provider. Additionally, the data set included certain demographic information describing members and community providers, current as of the end of the study period.
Community providers
Providers were represented by unique provider identification numbers, which were assigned to either individual clinicians or medical groups. We assembled a list of all provider numbers within the community's six zip codes which had at least one claim ascribed to them during the study period. We included all community providers regardless of whether or not they participated in the actual HIE. In most cases, the specialty and medical group of the provider were supplied in the data. In addition, we used the name and address of the medical group given in the data and internet searches to determine or verify specialty and to assign the provider to a medical group (eg, one physician was labeled ‘emergency medicine’ but also had an orthopedic surgery practice). We excluded anesthesiologists because they typically work only with other physicians and may not require a separate data exchange.
We excluded providers who had the fewest visits in the data set because the results related to those providers were unstable. We selected a cut-off of <300 visits during the study period for excluding providers and tested the findings with the threshold set at 200 and 400 visits. Providers may have had low visit volumes for a number of reasons, because, for example, they worked part time, had practiced in the community for only a short while, or primarily cared for older patients who were not in the data set.
Community patients
We included all patients enrolled in the health plan who had one or more claims to a community provider in the data set. We excluded patients over 65 years of age because many of them may have also filed claims through Medicare, and we did not have access to that information. To assess the completeness of our data, for each patient, we calculated their active time span in the data set by counting the number of days between their earliest and latest claim.
Individual visits
From the claims data, we derived provider visits. Multiple claims that contained the same date, provider, and patient were considered part of the same visit. We excluded all facilities fees and other claims not labeled ‘professional.’ For the main analysis, we included only claims assigned to individual providers. We also carried out an additional sensitivity test of our findings that included claims assigned to medical groups. For inpatient claims, any claim submitted between the admit and discharge dates was considered part of the inpatient visit.
Care transitions
For the primary analyses, we estimated care transitions to providers based on the visit patterns of each provider's patients. A visit was counted as a care transition if the patient's preceding medical visit in the community was to a different provider (table 1). This measure is similar to the ‘sequence’ metric used by researchers to estimate continuity of care.16 We defined the transition percentage as the percentage of a provider's visits that involved care transitions.
Table 1.
Example patient visit patterns with computed care transitions and transition percentages
| Patient visit pattern to provider A, B, and C | Provider A: no. of care transitions/total visits (transition percentage) | Provider B: no. of care transitions/total visits (transition percentage) | Provider C: no. of care transitions/total visits (transition percentage) |
| Patient 1: AAAAAAAAAA | 0/9 | 0/0 | 0/0 |
| Patient 2: ABABABABAB | 4/4 | 5/5 | 0/0 |
| Patient 3: AAAAABBBBB | 0/4 | 1/5 | 0/0 |
| Patient 4: ABCAACABBA | 3/4 | 2/3 | 2/2 |
| Total for patients 1, 2, 3, and 4 | 7/21 (33%) | 8/13 (62%) | 2/2 (100%) |
Transition percentage is defined as the percentage of a provider's total visits in which the patient's previous visit was to a different provider. Each patient's first visit in the study period with any provider would not count as part of their total visits for this provider because there was no way to determine if this first visit involved a care transition.
We computed these and related metrics under the following scenarios:
Individual clinicians. We computed the clinicians' transition percentage, ignoring the clinicians' medical group membership. We computed average transition percentages by medical specialty to allow comparisons across specialties, and we also report variation within specialties.
Medical groups. We computed the transition percentages of medical groups. A visit was counted as a care transition only if the patient's preceding visit in the community was to a different medical group. We assumed providers remained in the same groups throughout the study period.
We did not assign inpatient and emergency department visits to individual providers because they tended to involve multiple clinicians and it was not clear which providers would have been most likely to use HIE for the visit. We combined inpatient and emergency department visits into one category because there was only one hospital in the community and the emergency department was attached to that hospital.
For both individual clinician and medical group scenarios, we computed the transition percentage for the community as a whole, and we tested the sensitivity of these estimates when including only those clinical specialties which we believed would be the primary users of an HIE (‘core’ specialties) and also when excluding radiology and pathology. All groups in this community included clinicians who were either core or non-core specialties, never both. We used only claims assigned to individual clinicians, but also tested the sensitivity of the results when including claims assigned to medical groups for the group scenario. We also computed the percentage of visits to all community providers for which the previous visit took place outside of the community.
Results
We found notable variation in transition percentages across specialty, within specialty, and across medical groups even in this small community. Primary care physicians had a transition percentage of 54%, while in comparison, specialists tended to have higher percentages, averaging 79% for core specialties. Among primary care physicians, pediatricians had similar transition percentages compared to internists when considered as individual providers, but a pediatric medical group showed only 24%, reflecting a higher number of transitions internal to the group. Within specialties, primary care physicians showed the greatest range of transition percentage, varying from 32% to 95%. Medical groups had a wide range, and in particular the large group practice had about half the transition percentage of several smaller practices. For the community as a whole, excluding radiology and pathology, the transition percentage was 51% for individual clinicians and 41% for medical groups.
Provider characteristics
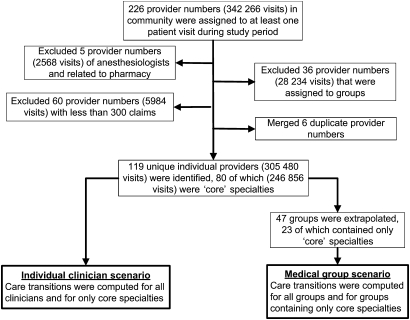
We identified 226 provider identification numbers in the community with at least one patient visit, 119 of which were assigned to unique individuals with more than 300 visits (figure 1). Of those 119 providers, 80 were in core specialties (table 2). A wide range of specialties was represented in the community, including 34 providers who were considered to be supplying primary care.
Figure 1.
Community providers included in the study.
Table 2.
Specialties of community providers
| Providers in core specialties (N=80) | Providers in non-core specialties (N=39) |
| Primary care (34) | Chiropractic (6) |
| Family practice (5) | Clinical psychology (7) |
| Internal medicine (18) | Dentistry (8) |
| Nurse practitioner (2) | Dietician nutritionist (1) |
| Pediatrics (9) | Mental health counselor (3) |
| Specialties | Optometry (3) |
| Cardiovascular disease (2) | Physical therapy (6) |
| Dermatology (3) | Social worker (5) |
| Gastroenterology (1) | |
| General surgery (2) | |
| Hematology/oncology (1) | |
| Midwife (2) | |
| Neurology (2) | |
| Obstetrics and gynecology | |
| Ophthalmology (4) | |
| Oral and maxillofacial surgery (3) | |
| Orthopedic surgery (4) | |
| Otolaryngology (1) | |
| Pathology (4) | |
| Podiatry (2) | |
| Psychiatry (2) | |
| Pulmonary disease (1) | |
| Radiology (5) | |
| Urology (2) |
Patient characteristics
The sample included 18 831 patients who were less than 65 years of age and had visited a community provider for more than one visit. Slightly more than half of the patients (55%) were female and average age was 36. The average active time span among patients was 826 days (median 832, IQR 269–1402) of a total possible 1641 days. The mean number of visits per patient during the study period was 19 (median 11, IQR 4–25).
Care transitions—individual community clinicians
We found notable variation in the transition percentage by clinical specialty (table 3). Radiologists and pathologists had the greatest transition percentages, as might be expected, averaging >95%. Providers with low transition percentages included physical therapists and chiropractors with 22% and 25%, respectively. Specialties with relatively high transition percentages included ophthalmology and obstetrics/gynecology with transitions occurring in 84% and 79% of visits on average, respectively. Primary care specialties fell in the middle range, with 54%.
Table 3.
Transition percentages for individual clinicians, grouped by specialty
| Specialty | No. of clinicians | No. of visits | Weighted average transition percentage (weighted SD) (low–high) |
| Primary care | |||
| Family practice | 5 | 16 569 | 44.3 (7.3) (32.4–67.6) |
| Internal medicine | 18 | 66 411 | 54.6 (10.3) (35.0–95.2) |
| Nurse practitioner | 2 | 783 | 91.0 (88.1–93.3) |
| Pediatrics | 9 | 41 008 | 56.2 (11.1) (45.1–93.2) |
| All primary care | 34 | 124 771 | 54.0 (11.3) (32.4–95.2) |
| Core specialties | |||
| Cardiovascular disease | 2 | 2220 | 81.4 (60.9–85.3) |
| Dermatology | 3 | 9862 | 59.3 (49.7–62.5) |
| Gastroenterology | 1 | 4517 | 68.4 |
| General surgery | 2 | 2551 | 78.1 (77.4–82.9) |
| Hematology/oncology | 1 | 2009 | 50.9 |
| Midwife | 2 | 783 | 91.1 (88.1–93.3) |
| Neurology | 2 | 4430 | 61.7 (58.1–80.4) |
| Obstetrics and gynecology | 5 | 13 972 | 79.3 (6.9) (65.0–84.1) |
| Ophthalmology | 4 | 6166 | 83.9 (79.2–87.3) |
| Oral and maxillofacial surgery | 3 | 2035 | 57.5 (51.9–70.1) |
| Orthopedic surgery | 4 | 10 051 | 71.6 (70.8–73.7) |
| Otolaryngology | 1 | 740 | 73.9 |
| Pathology | 4 | 5938 | 98.7 (98.7–99.0) |
| Podiatry | 2 | 2725 | 71.5 (55.4–77.4) |
| Psychiatry | 2 | 2219 | 47.2 (36.5–49.1) |
| Pulmonary disease | 1 | 665 | 87.4 |
| Radiology | 5 | 29 524 | 95.2 (0.9) (94.2–97.6) |
| Urology | 2 | 2571 | 72.1 (68.1–75.4) |
| Non-core specialties | |||
| Chiropractic | 6 | 12 165 | 25.3 (9.1) (12.1–47.0) |
| Clinical psychology | 7 | 3573 | 32.2 (14.3) (7.4–57.5) |
| Dentistry | 8 | 12 861 | 59.3 (5.1) (51.3–70.9) |
| Dietician nutritionist | 1 | 357 | 82.6 |
| Mental health counselor | 2* | 2039 | 23.9 (9.3–23.7) |
| Optometry | 2* | 5885 | 87.4 (85.5–89.0) |
| Physical therapy | 6 | 16 570 | 22.1 (2.7) (19.1–28.4) |
| Social worker | 5 | 2282 | 31.9 (4.6) (27.4–40.1) |
Averages of each specialty are weighted by visit totals and so are equivalent to the portion of total visits to clinicians in each particular specialty that are care transitions. Standard deviations are also weighted by total visits and are computed as the square root of the weighted unbiased variance. We only report standard deviations for specialties for which the data contain five or more providers, and low–high for two or more. The number of visits excludes patients' first visits in the data set.
One mental health counselor and one optometrist showed zero care transitions and, as such, were considered outliers and excluded.
We found that the transition percentage also varied to some extent within medical specialties. For example, internists and pediatricians showed notable variation. Transition percentages for both of these specialties ranged more than 45 percentage points with a standard deviation (weighted by number of visits) of >10. Most specialties seemed more consistent, although there were fewer practitioners of these specialties in the community. The transition percentages of obstetrics and gynecology physicians varied by <20%, with four out of five having transition percentages between 79% and 85%. The transition percentages of orthopedic surgeons ranged from 71% to 74%.
Care transitions—medical group scenario
We also found notable variation in transition percentage among medical groups (table 4). The hospital had the greatest transition percentage in the community on account of the radiologists and pathologists practicing there. Several group practices were single-specialty and had transition percentages comparable to those of similar specialists in the individual scenario. The pediatric practice, however, showed a transition percentage of 24%, which was considerably smaller than any pediatrician's percentage in the individual scenario, indicating a large number of transitions within the group. The community's largest group also had a smaller transition percentage compared with most other practices.
Table 4.
Care transitions between medical groups
| Medical group description | No. of clinicians | Specialties represented in group | Transition percentage (of total visits) |
| Group 1: hospital | 8* | Radiology (2), pathology (4), internal medicine (1), otolaryngology (1) | 86.4% (of 18 403)† |
| Group 2: large group practice | 21 | Multiple specialties‡ | 36.8% (of 75 246) |
| Group 3: medium-size group practice | 6 | Cardiology (2), urology (2), obstetrics/gynecology (2) | 70.8% (of 10 343) |
| Group 4: medium-size group practice | 4 | Orthopedic surgery | 69.5% (of 9993) |
| Group 5: medium-size group practice | 5 | Internal medicine | 41.2% (of 14 248) |
| Group 6: medium-size group practice | 5 | Pediatrics | 23.9% (of 20 890) |
| Group 7: medium-size group practice | 4 | Ophthalmology | 81.7% (of 6164) |
| Group 8: medium-size group practice | 6 | Family practice (3), nurse practitioner (1), obstetrics/gynecology (2) | 62.2% (of 14 039) |
| Group 9: medium-size group practice | 5 | Physical therapy | 20.1% (of 14 542) |
| Group 10: small group practice | 1 | Family practice | 43.1% (of 8725) |
Only groups with >6000 visits in the data set are shown (except for one radiology group which is not shown). Care transitions between providers within the same group are not counted in the transition percentages.
Clinicians who treat patients for inpatient and emergency department visits are not counted in the number of clinicians.
The hospital's transition percentage includes inpatient and emergency department visits. If these visits are excluded, the transition percentage is slightly higher at 88.5%. Most hospital visits are for radiology or pathology.
This group included: general surgery (2), internal medicine (11), nurse practitioner (1), neurology (1), obstetrics and gynecology (1), pediatrics (3), pulmonary disease (1), and podiatry (1).
Community results
For the community in total, we found that the overall transition percentage ranged between 36% and 62% depending on various assumptions (table 5). When providers are considered in their medical groups, their transition percentages are up to 15% lower than when they are considered as individuals, because of the care transitions that occur within medical groups. Transition percentages among core specialties were similar to those among all provider types. When radiology and pathology visits were removed, the community transition percentage decreased by approximately 10%.
Table 5.
Community care transitions per patient visit
| Scenario | Transition percentages (of patient visits) | Transition percentages (of patient visits), excluding radiology and pathology |
| Individual clinician: all providers | 60.2% (of 283 613) | 51.2% (of 247 105) |
| Individual clinician: core specialties only | 62.2% (of 226 381) | 51.5% (of 190 015) |
| Medical group: all providers | 50.2% (of 284 597) | 40.6% (of 247 793) |
| Medical group: core specialties only | 48.8% (of 226 346) | 35.7% (of 189 929) |
Inpatient and emergency visits were included in group scenarios and excluded from the individual scenarios. Differences in visits between individual and group scenarios are because we consider same day visits to the same group as part of the same visit in the group scenario.
We performed several sensitivity tests on these results and found them to be reasonably robust. Removing inpatient and emergency department visits from the group scenario resulted in negligible change in the community transition percentage, reflecting the fact that these types of visits represented a small portion of the total community visits. We changed the provider exclusion threshold to 200 visits and 400 visits, which involved adding 3211 visits and excluding 4448 visits, respectively, for the individual provider scenario. We found negligible changes in transition percentages resulting from these changes. We included 28 234 visits which were assigned to medical groups in the group scenario for all clinicians. The total community transition percentage rose from 50% to 52% as a result of the group claims, with most groups having changes of only one or two percentage points and the largest change occurring in the pediatric practice which showed a 4% increase in transition percentage from 24% to 28%.
Even though we did not have complete knowledge of the clinicians who worked outside of the community, we did estimate the total proportion of community visits which involved transitions from outside of the community, and assessed this proportion to be 14.5% of all visits to community providers.
Discussion
We found that transitions in care constituted a substantial proportion of patient visits in one community. These visits represent opportunities where an aggregate patient record form of HIE could provide useful information. We found a notable range of transition percentages across specialties, within specialties, and across medical groups even among the modest number of clinicians in the data set.
We identified a few other reports that studied the frequency of care transitions for patients in a community, although most involved narrower clinical samples. For example, one study that investigated the frequency with which an HIE was accessed was restricted to emergency departments.13 Another study evaluated the number of patients who visited more than one emergency department within a geographic region.14 A study of the United Kingdom's effort to share clinical records was also restricted to emergency or unscheduled care settings.17 Other studies that report HIE usage numbers did not focus on appropriate levels of usage based on patient visit patterns.18
If variation in transition percentage among clinicians is common in many communities, meaningful use payments and related policy incentives should consider patient visit patterns, in addition to visit volumes, in estimates of target HIE usage.
Many providers may not access an aggregate record HIE for every care transition for good reason. Some patients' problems may be routine and data in the HIE may be unrelated to the patient's current problem or clinical episode. However, providers will often not be able to determine the relevance of the data without first reviewing them. We suggest that if providers—primary care especially—are to be responsible for coordination of patient care and comprehensive treatment of medical conditions, some fraction of the number of care transitions a provider encounters will represent a reasonable meaningful use target for a provider accessing an aggregate patient record HIE. What that fraction is should be addressed empirically. Which specific data types providers should be expected to view is also an open question and likely varies by clinician's specialty and the setting in which they are seeing the patient, as well as the specific circumstances of the patient's visit. In many clinical scenarios, providers may be expected to check for recent laboratory results, changes in problem lists and medications, or consultation notes.
Some providers may access an HIE even for repeat visits because information from the HIE had not been imported into the provider's electronic health record (EHR) during the previous visit, or because the provider had no way of knowing whether or not new data were present in the HIE. HIE vendors may reduce the need for these accesses, which could be a burden on the provider, by providing functionality that allows automatic importing of HIE data into an EHR and by implementing a visual cue that indicates whether or not new data have been added to the HIE since the patient's previous visit.
Aggregate records in HIEs may not always be comprehensive and include up-to-date information from all providers in the community because some providers may not participate and some may not always contribute data immediately following every patient visit.10 Also, some providers may not have easy access to the HIE. Therefore, realistic usage targets will likely be lower than the estimates in this study but will still be computable from the patient visit patterns of providers who participate in HIEs.
In addition to assessing HIE accesses, meaningful use payments might also consider including accesses to medical groups' EHRs for care transitions within medical groups, which accounted for 10%–15% of visits in the community we studied and may be more or less in other communities, although data exchange is much easier within a group that shares an EHR. This may be especially important for large medical groups in which many patients receive most of their care, because many care transitions will likely occur between providers within those groups and incentives may be needed to ensure care within the group is coordinated.
If measures of HIE accesses are to be used in connection with incentive payments, HIE and EHR vendor companies must offer the capability to report these metrics. It is unlikely that vendors will develop functionalities to report metrics that can be compared across HIEs without some change in their incentives offered. We recommend that vendors should be required to support these metrics as a condition of certification.19 Vendors would likely be able to calculate counts of actual HIE accesses as well as the volume of care transitions from data they already capture in audit trails, although they should not be expected to develop their own algorithms for doing this—development of a single algorithm might be helpful and also could diminish the risk of ‘gaming’ or manipulation of the system.
Gaming is a serious concern; in particular, direct incentives to providers simply to access HIE may not be a judicious approach to encourage meaningful use.20 The risk of gaming should be studied empirically. In addition to being used to assess providers' usage, care transition metrics may also be applied to evaluate and compare the effectiveness of HIE organizations and regional extension centers in engaging clinical users. One option might be to incentivize HIEs in particular to have higher clinician usage rates. We have observed when evaluating a working HIE that the doctors would have benefitted from some simple office training, but the HIE did not have an incentive to provide such training.10
This study has several important limitations. It focused on only one small community and thus may not be generalizable to other care settings. Visit patterns may be different in different types of communities, such as urban settings, and may have more or less variation in transition percentage. In addition, our claims data were limited to the claims submitted to one private payer, so the results may not be generalizable to other payers. Also, visits from patients over 65 years of age or from patients or providers not covered by the payer were not included. We also did not account for providers who changed medical groups during the study period.
In conclusion, in this study within one community, we found that a substantial percentage of patient visits involved care transitions. This finding supports previous studies that identified significant potential use for HIE, especially for aggregate patient records. We also found substantial differences in care transition patterns by type of practice in this community, which suggests that patient visit patterns should be considered when incentives to foster providers' meaningful use of health data exchange functionality are being designed.
Footnotes
Funding: This work was funded by NLM grant number LM007092.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Walker J, Pan E, Johnston D, et al. The value of health care information exchange and interoperability. Health Aff (Millwood) 2005;Suppl Web Exclusives:W5–10–W5–18. http://dx.doi.org/10.1377/hlthaff.w5.10 [DOI] [PubMed] [Google Scholar]
- 2.AHRQ Health Information Exchange, 2009. http://www.healthit.ahrq.gov/hie (accessed Jul 2010).
- 3.Pham HH, Schrag D, O'Malley AS, et al. Care patterns in Medicare and their implications for pay for performance. N Engl J Med 2007;356:1130–9 http://dx.doi.org/10.1056/NEJMsa063979 [DOI] [PubMed] [Google Scholar]
- 4.Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA 2005;293:565–71 http://dx.doi.org/10.1001/jama.293.5.565 [DOI] [PubMed] [Google Scholar]
- 5.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med 2006;145:488–96 [DOI] [PubMed] [Google Scholar]
- 6.Hussey PS, Sorbero ME, Mehrotra A, et al. Episode-based performance measurement and payment: making it a reality. Health Aff (Millwood) 2009;28:1406–17 http://dx.doi.org/10.1377/hlthaff.28.5.1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gandhi TK, Sittig DF, Franklin M, et al. Communication breakdown in the outpatient referral process. J Gen Intern Med 2000;15:626–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Walraven C, Taljaard M, Bell CM, et al. Information exchange among physicians caring for the same patient in the community. CMAJ 2008;179:1013–18 http://dx.doi.org/10.1503/cmaj.080430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adler-Milstein J, Bates DW, Jha AK. U.S. Regional health information organizations: progress and challenges. Health Aff (Millwood) 2009;28:483–92 http://dx.doi.org/10.1377/hlthaff.28.2.483 [DOI] [PubMed] [Google Scholar]
- 10.Rudin RS, Volk LA, Simon SR, et al. What affects clinicians' usage of health information exchange? Applied Clinical Informatics 2011;2:250–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Department of Health and Human Services Final Rule, 2010. http://www.ofr.gov/OFRUpload/OFRData/2010-17207_PI.pdf (accessed Jul 2010).
- 12.Vest JR, Jasperson J. What should we measure? Conceptualizing usage in health information exchange. J Am Med Inform Assoc 2010;17:302–7 http://dx.doi.org/10.1136/jamia.2009.000471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson KB, Gadd CS, Aronsky D, et al. The MidSouth eHealth Alliance: use and impact in the first year. AMIA Annu Symp Proc 2008:333–7 [PMC free article] [PubMed] [Google Scholar]
- 14.Finnell JT, Overhage JM, Dexter PR, et al. Community clinical data exchange for emergency medicine patients. AMIA Annu Symp Proc 2003:235–8 [PMC free article] [PubMed] [Google Scholar]
- 15.Correspondence with largest medical group in community; October, 2010 [Google Scholar]
- 16.Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev 2006;63:158–88 http://dx.doi.org/10.1177/1077558705285294 [DOI] [PubMed] [Google Scholar]
- 17.Greenhalgh T, Stramer K, Bratan T, et al. Adoption and non-adoption of a shared electronic summary record in England: a mixed-method case study. BMJ 2010;340:c3111. [DOI] [PubMed] [Google Scholar]
- 18.Vest JR. Health information exchange and healthcare utilization. J Med Syst 2009;33:223–31 [DOI] [PubMed] [Google Scholar]
- 19.Certification Commission for Health Information Technology. http://www.cchit.org/
- 20.Doran T, Fullwood C, Reeves D, et al. Exclusion of patients from pay-for-performance targets by English physicians. N Engl J Med 2008;359:274–84 http://dx.doi.org/10.1056/NEJMsa0800310 [DOI] [PubMed] [Google Scholar]