Abstract
Objective
To present a partnership-based and community-oriented approach designed to ease provider anxiety and facilitate the implementation of electronic health records (EHR) in resource-limited primary care settings.
Materials and Methods
The approach, referred to as partnership model, was developed and iteratively refined through the research team's previous work on implementing health information technology (HIT) in over 30 safety net practices. This paper uses two case studies to illustrate how the model was applied to help two nurse-managed health centers (NMHC), a particularly vulnerable primary care setting, implement EHR and get prepared to meet the meaningful use criteria.
Results
The strong focus of the model on continuous quality improvement led to eventual implementation success at both sites, despite difficulties encountered during the initial stages of the project.
Discussion
There has been a lack of research, particularly in resource-limited primary care settings, on strategies for abating provider anxiety and preparing them to manage complex changes associated with EHR uptake. The partnership model described in this paper may provide useful insights into the work shepherded by HIT regional extension centers dedicated to supporting resource-limited communities disproportionally affected by EHR adoption barriers.
Conclusion
NMHC, similar to other primary care settings, are often poorly resourced, understaffed, and lack the necessary expertise to deploy EHR and integrate its use into their day-to-day practice. This study demonstrates that implementation of EHR, a prerequisite to meaningful use, can be successfully achieved in this setting, and partnership efforts extending far beyond the initial software deployment stage may be the key.
Keywords: Collaborative technologies, community health care, developing/using clinical decision support (other than diagnostic) and guideline systems, electronic health records (E05.318.308.940.968.625.500), health information technology for economic and clinical health act (N03.706.615.049), human–computer interaction and human-centered computing, improving healthcare workflow and process efficiency, nurse-managed health centers, personal health records and self-care systems, qualitative/ethnographic field study, regional extension centers, social/organizational study, system implementation and management issues, systems supporting patient–provider interaction
Widespread adoption and meaningful use of health information technology (HIT), electronic health records (EHR) in particular, will play a pivotal role in enabling transformative changes in the US healthcare system in order to achieve broader quality improvement and cost containment goals.1–3 Despite the great promise, the rates of EHR adoption remain low in the USA4–6 largely attributable to healthcare practices' lack of technology expertise and their limited ability to manage complex changes.7–9 Even in resource-abundant and technologically competent environments, implementation projects of EHR and HIT systems in general have experienced a high rate of failure,10 and successfully deployed systems often fail to generate anticipated results;11–14 some are even associated with unintended adverse consequences.15–18
The adoption lag and implementation deficiencies disproportionally affect those resource-limited primary care practices serving vulnerable populations, widening the gap in quality of care and access to care.19–21 Recognizing the importance of this issue, the American Recovery and Reinvestment Act of 2009 has placed a prominent focus on incentivizing EHR adoption in smaller and resource-limited primary care settings. This effort is further reinforced by the establishment of a nationwide network of HIT regional extension centers that are dedicated to assisting disadvantaged shareholders in purchasing and implementing EHR systems.22
In this paper, we describe a partnership-based and community-oriented approach, referred to as ‘partnership model’ hereafter, which was developed and iteratively refined over the past few years through the research team's previous work on implementing EHR among over 30 safety net practices, many of which are federally qualified health centers. Through two case studies, we illustrate how we applied the model to facilitate EHR implementation in a particularly vulnerable primary care setting: nurse-managed health centers (NMHC). This work was grounded in an EHR demonstration project supported by the Agency for Healthcare Research and Quality, jointly conducted by the Institute of Nursing Centers at the Michigan Public Health Institute (MPHI) and the Alliance of Chicago Community Health Services (‘Alliance’), collectively referred to as ‘the partnership’. The MPHI and the Alliance are also founding partners of two regional extension centers: the Michigan Center for Effective IT Adoption and the Chicago Health Information Technology Regional Extension Center, respectively.
Background
The partnership model
The partnership model described in this paper emphasizes ‘sharing of benefits, risks, and resources toward a common goal’.23 24 It was developed based on the following three premises: (1) an engaging and sustaining relationship with the technology team is the only way to shield healthcare practices from adoption difficulties and uncertainties (ie, partnership-based); (2) adopting practices should think and act collectively as a community in order to lower purchase and maintenance costs and jointly develop best practices for implementation and use (ie, community-oriented); and (3) it is central to have strong commitments by all parties to managing EHR implementation as a long-term, continuous quality improvement (CQI) process, as opposed to a one-time software installation effort.
The model, as its name suggests, places a prominent focus on building a strong and long-lasting collaborative relationship between EHR implementers and adopting healthcare practices. As a matter of fact, the technology group of the partnership, Alliance, was initially created by a network of federally qualified health centers to plan and establish a shared technology infrastructure to serve their common needs. Such needs include not only implementing electronic systems to support routine clinical data acquisition and management, but also (1) advocating on their behalf to compete for resources from parent organizations, affiliated physician consortiums and extramural funding agencies; (2) negotiating with external partners (eg, affiliated hospitals and outpatient laboratories and pharmacies); and (3) creating a community-wide analytical data warehouse for secondary-use purposes such as quality improvements and research. Over the past few years, Alliance has also evolved into a technology consulting group providing EHR implementation services to new members of the partnership—at a much more affordable price subsidized by both federal grants and cost sharing among all participating centers. In essence, the ‘EHR implementer’ of the partnership grew from the community, supported by the community, and serves the community, rather than being brought in as a temporary, third-party IT contractor.
Furthermore, the partnership model places a particular emphasis on fostering a collaborative culture among all participating healthcare practices to facilitate information and experience sharing. The objective was to leverage the partnership's collective wisdom so as to reduce redundant effort (eg, by the shared use of common disease management templates and decision-support tools), as well to jointly identify solutions to common adoption barriers and post-implementation adaptation difficulties. This peer cooperation has been achieved through periodical leadership teleconferences and an annually convened in-person partnership symposium. The partnership also encourages the community to document and share their EHR implementation knowledge and stories; the present paper is an example.
Finally, CQI serves as a key guiding principle of the partnership model because none of the EHR implementation processes are discrete and can be optimized independently. Furthermore, emerging conditions brought with or magnified by later processes often invalidate previous assumptions, thus requiring an iterative approach. This approach needs to incorporate not only the initial assessments (we used the analysis of strengths, weaknesses, opportunities and threats; SWOT),25 but also CQI methods including formative evaluation, constant performance feedback and timely implementation of corrective actions (based on the Shewhart /Deming cycle of plan, do, check, and act).26 27 Therefore, establishing strong commitments by all parties involved to managing EHR implementation as a long-term project, rather than a one-time software installation effort, is foremost crucial.
The EHR planning and implementation guideline of the partnership model
An important component of the partnership model is an EHR planning and implementation guideline (PM–PIG), which was designed to facilitate consensus development between the technology team and the participating healthcare practices and strategic planning and task execution in each of the key implementation phases. The guideline was largely informed by the notion of mindful innovation with IT proposed by Swanson and Ramiller,28 which conceptualizes that an organization's journey toward mindful adoption of a technological innovation must undergo four essential steps: comprehension, adoption, implementation, and assimilation, with an analysis of common pitfalls caused by ‘mindlessness’ in each step.
The guideline is presented in additional detail in supplementary appendix 1 (available online only). In table 1, we provide an outline of its 19 key components organized into three distinct implementation phases, before (comprehension and adoption), during (implementation) and after (assimilation). Note that while the post-implementation activities usually start 3 months after the initial ‘go-live’ date, there is no definitive time divide between the during and the post phase. The during implementation activities could last as long as it takes if the needs persist, eg, unexpected technical or user acceptance issues that may continue to emerge.
Table 1.
Outline of the EHR planning and implementation guideline of the partnership model
| Phrase | Ref no | Guideline component |
| Pre-implementation | 1.1 | Readiness assessments |
| 1.2 | Technical infrastructure preparation | |
| 1.3 | Culture preparation and change management | |
| 1.4 | Workflow redesign | |
| 1.5 | Guided data preloading | |
| 1.6 | Software tailoring | |
| 1.7 | Integrated and upgraded billing | |
| 1.8 | Data exchange capability | |
| 1.9 | Assistance in negotiation and working with external partners | |
| During-implementation | 2.1 | Shared hosting |
| 2.2 | Training and retraining | |
| 2.3 | Formative evaluation | |
| 2.4 | Regular performance feedback | |
| 2.5 | Corrective actions | |
| Post-implementation | 3.1 | Leadership teleconference |
| 3.2 | Annual partnership symposium | |
| 3.3 | Data integrity | |
| 3.4 | Centralized analytical data warehouse | |
| 3.5 | Research capacity building and summative evaluation |
Full descriptions of each of the guideline components are provided in supplementary appendix 1, available online only.
EHR, electronic health record.
The execution of PM–PIG is supported by a variety of tools and theoretical frameworks informed by the literature, such as a computer literacy survey assessing clinicians' use of, knowledge about and attitudes toward computers29 and the unified theory of acceptance and use of technology that outlines common antecedents to end users' acceptance behavior of technological innovations.30 We describe these two methods in more detail in the Materials and methods section. In the Results section, we illustrate how they were applied to help us formatively evaluate the EHR implementation at the two NMHC study sites. In supplementary appendix 1D (available online only), we provide a complete list of all supporting tools and theoretical frameworks encompassed in the partnership model.
Nurse-managed health centers
Directed and primarily staffed by nurse practitioners and midwives, NMHC are an important supplementary primary care model that performs a critical role in the nation's healthcare safety net.31 NMHC are historically rooted in underserved communities and have embraced many qualities of new care delivery models, such as patient-centered medical homes, to provide holistic patient care services including health promotion, disease prevention and the early detection of common chronic conditions.31 Previous research has shown that the performance of NMHC on managing complex chronic diseases (eg, diabetes, hypertension, depression and asthma) is comparable to, and better than from several aspects, national benchmarks.32
A majority of NMHC, however, are extremely poorly resourced and lack the necessary expertise to deploy EHR and integrate its use into their day-to-day practice. Therefore, the partnership model that offers a guided implementation process is particularly welcomed in this setting. Over the past few years, the Institute for Nursing Centers and MPHI have coordinated the implementation activities among the NMHC of the partnership, and have also made strides in tailoring the model to accommodate the special requirements of nurse-managed facilities such as helping them design customized patient satisfaction survey tools catering to their needs and preferences.
Materials and methods
Empirical setting
In this paper, we describe our recent experiences in applying the partnership model to implement an EHR system at two NMHC. In both case presentations, we focus on key challenges that we encountered through our work in the field rather than making a victory declaration or providing a laundry list of all issues uncovered and all actions undertaken. Table 2 presents the characteristics of the two study sites.
Table 2.
Site characteristics
| Name | Year established | Provider characteristics | Annual patient visit volume | Patent population served |
| The Glide Health Services (Glide) | 1997 | 7.5 FTE advanced NP (average age: 48.1 years; average years in practice: 17 years) in addition to other types of medical professionals and trainees and volunteers | Over 17 000 patient visits by an adult patient population of approximately 3250 | Behavioral health and primary care for homeless, immigrant, and urban poor |
| The University Campus Health Center, Detroit (CHCD) | 2005 | 4.2 FTE advanced NP (average age: 52.9 years; average years in practice: 19 years) | Over 9000 health visits by about 4500 distinct patients | Primarily urban college students |
FTE, full-time equivalent; NP, nurse practitioner.
Evaluation of end user acceptance
We administered a series of end user surveys to formatively evaluate clinicians' experiences with and satisfaction of the EHR system and the implementation processes. All full-time equivalent (FTE) providers at both sites participated in the surveys. Not all of them were available in all study phases, however, due to uncontrollable factors (eg, staff turnover).
As baseline, approximately 1 month before the EHR was implemented, we administered a computer literacy survey to assess clinicians' attitudes toward the use of EHR in clinical care (‘computer optimism’). The survey questionnaire was developed based on a validated instrument developed by Cork et al,29 and measures clinicians' basic levels of computer literacy in addition to their expected impacts of EHR on care quality, efficiency, costs, enjoyment of practice and patient-clinician relationships. These questionnaire items were assessed on a five-point scale: ‘highly detrimental’, ‘detrimental on the whole’, ‘neither detrimental nor beneficial’, ‘beneficial on the whole’ and ‘highly beneficial’, coded as an ordinal variable from 1 to 5 in the data analysis. After the EHR implementation, repeated measurements of the survey were obtained at multiple time points to allow clinicians to provide additional feedback based on their hands-on, personal experiences with the EHR system.
In the post-implementation stage, we introduced an EHR end user evaluation questionnaire (see supplementary appendix 2, available online only) to solicit clinicians' perception of the usefulness and ease of use of the EHR system (‘performance expectancy’ and ‘effort expectancy’), and the quality of the EHR use environment such as the adequacy of training and computer/network performance (‘facilitating conditions’). The questionnaire was developed based on the unified theory of acceptance and use of technology, which postulates that these constructs, in addition to ‘social influence’ (which we were unable to examine in this study due to small sample size), are the most influential factors underlying end users' decision to accept or to reject a technological innovation.30 All unified theory of acceptance and use of technology-based questionnaire items were assessed on a four-point, forced Likert scale stepping from ‘strongly disagree’ to ‘strongly agree’, coded as an ordinal variable from 1 to 4; higher values indicate more positive evaluation.
Results
Case 1: the Glide Health Services
General facts and EHR readiness assessments
Located in the Tenderloin of San Francisco, California, USA, the Glide Health Services (‘Glide’) is a nurse managed federally qualified health center funded through a partnership of the Glide Foundation, the University of California San Francisco's School of Nursing, the Saint Francis Memorial Hospital (a member of the Catholic Healthcare West Corporation) and the Health Resources and Services Administration (HRSA) Division of Nursing. Since its inception in 1997, Glide has been providing a holistic coverage of primary care to an underserved population that has a high rate of homelessness (60%) and poverty (80% under 100% federal poverty level).
Through an earlier participation in California's electronic chronic disease registry initiatives, Glide had long recognized the potential of using HIT to improve the efficiency and quality of its patient care services. The key barriers were the prohibitive cost of purchasing a comprehensive EHR system and the complexity of managing associated changes as a small practice. With a considerable group purchase discount and the technical and community support provided by the partnership, Glide was prepared to embark on the journey toward EHR. The initial step, applying the SWOT analysis to assess its readiness for EHR (PM–PIG 1.1), was conducted in February 2009. The results are presented in table 3.
Table 3.
Results of the SWOT analysis, Glide
| Strengths | Weakness |
|
|
| Opportunities | Threats |
|
|
CQI, continuous quality improvement; EHR, electronic health record; SWOT, strengths, weaknesses, opportunities and threats.
Implementation challenges
Implementation was supported by the partnership particularly in preparing a facilitating practice culture such as fostering an atmosphere of open discussions about this transformative change (PM–PIG 1.3). The partnership led these preparatory activities through in-person and telephone meetings (PM–PIG 1.2, 1.4). As Glide's services include highly integrated primary and behavioral care, creating tailored documentation forms in the EHR and redesigning the existing workflow also represented substantial challenges, which the partnership was instrumental in helping address (PM–PIG 1.6). Not all workflow pitfalls were identified during the planning stage, however. For example, many encounters were not timely released to activate the billing process because staff often missed a few key steps to mark a visit ‘complete’ in electronic documentation. A noticeable decrease in the volume of billing then prompted target training and additional workflow reviews and amendments (PM–PIG 1.7, 2.2–2.5).
As identified by the SWOT analysis, a prominent weakness for Glide to adopt EHR lay in its outdated computer network infrastructure. Even though this weakness was recognized early, resolving it had taken arduous and time-consuming steps given that Glide is homed within a large social service foundation and it must compete for resources with many other units in the organization. After a 6-month delay, Glide decided to launch the EHR system before the network upgrades were fully accomplished in order to realize its benefits sooner. The suboptimal network performance, however, did result in intermittent interruptions of EHR services (eg, response lags and connection drops). All clinicians were accordingly advised to save their work frequently and use alternative documentation methods as needed, such as to avoid using the system during busy office hours. The result of the initial poor experience, or ‘negative effect’,33 led to adoption resistance among some of the clinicians, the effect of which has carried over to date.
Besides providing information on network diagnostics, the partnership has a very limited influence over IT decisions within the Glide Foundation. Representatives from the partnership were keen to resolve the issues and met with the Foundation leadership frequently to explain why the EHR implementation placed additional requirements on the IT infrastructure and the importance of meeting the requirements in order to achieve success (PM–PIG 1.2, 1.9, 2.3–2.5, 3.1). The internal network at Glide has been overhauled with a stimulus grant awarded recently. The network infrastructure has been improved significantly and the performance issues encountered earlier are expected to be fully resolved in the near future.
Another factor significantly restraining the potential of the EHR was the delayed implementation of the data interfaces with Glide's outpatient laboratories. The real-time data exchange was planned to go live within 2 months after the EHR was implemented. With the sudden downturn of the economy in California, however, this work was put on a long hold. The resulting manual tracking processes not only caused a tremendous waste of labor, but also diminished the anticipated value of the EHR in enhancing the practice's longitudinal management of chronic conditions, a key outcomes-oriented motivation for adopting the system. While the partnership had little control over the other parties to accelerate the data interface establishment, it served a critical role as an advocate for Glide, and provided technical expertise throughout the negotiation with Glide's external partners (PM–PIG 1.8, 1.9). In September 2010, the laboratory data interface project was finally completed.
On the positive side, early post-implementation, Glide's staff welcomed the benchmarking data provided by the partnership facilitated by a partnership-wide analytical data warehouse (PM–PIG 2.4, 3.3, 3.4). The benchmarking data, at the granularity of the level of individual clinicians and patients, are particularly helpful to identify areas where practitioners were not providing recommended care and/or not fully utilizing the clinical decision-support functionalities of the EHR. The comparative data from other participating practices of the partnership, made available under a data-sharing agreement, were also welcomed by Glide's CQI committee and were used to inform their various quality improvements initiatives.
Case 2: the Campus Health Center, Detroit
General facts and EHR readiness assessments
The Campus Health Center, Detroit (CHCD) is an NMHC created by the Nursing Practice Corporation, a 501(c)(3) non-profit corporation composed of nursing faculty at Wayne State University, Detroit, Michigan, USA. The center was funded partly through student fees and a recently completed grant received from the HRSA to provide primary and behavioral care to urban university students seeking services related to acute illnesses, sexually transmitted infections, travel health and routine immunizations. Although seemingly healthy, many students delay seeking care due to the lack of insurance: approximately 40% of students serviced by CHCD are uninsured and 20% of residence hall students (generally aged 17–22 years) are uninsured.
Discussions regarding the implementation of an EHR system began within 1 year of the clinic's inception in 2005 while the clinic was still in an early developmental stage. Key goals for adopting EHR included enhanced efficiency, better documentation and improved tracking capability of the quality of the primary care services provided. A SWOT analysis was performed with assistance of the partnership in March 2007. Table 4 presents the findings.
Table 4.
Results of the SWOT analysis, CHCD
| Strengths | Weakness |
|
|
| Opportunities | Threats |
|
|
CHCD, Campus Health Center, Detroit; CQI, continuous quality improvement; SWOT, strengths, weaknesses, opportunities and threats.
Implementation challenges
Even though reliable IT services provided by Wayne State University's College of Nursing were identified as a particular strength, the EHR implementation at CHCD encountered extreme difficulties after the College of Nursing's IT support was withdrawn unexpectedly due to resource allocation reasons shortly after the EHR's go-live. The partnership then provided both onsite and remote IT support and guidance, which was not initially planned because of the optimism based on the SWOT analysis results. The issue finally got resolved with the partnership helping the center contract an off-campus IT support firm (PM–PIG 1.1, 1.9, 2.5) almost 1 year after the EHR system was implemented.
While a predominantly healthy and chronic disease-free population makes use of certain EHR functionalities straightforward, catering to the needs of this population created challenges in developing special templates and decision-support algorithms that are not commonly found in commercially sold vendor systems (eg, those for managing travel health and emergency and routine contraception care). The partnership provided guidance and technical assistance in template development (PM–PIG 1.6), which was also greatly simplified leveraging the partnership's collective resources and experiences (eg, templates previously developed for other centers that have similar needs).
As identified in the SWOT analysis, a known weakness of CHCD was the limited computer literacy among the majority of its staff (mean age of CHCD practitioners 52.9 years). Accordingly, the partnership provided on-site computer literary education before the implementation, which was instrumental in assisting ‘computer-challenged’ staff with hands-on instructions on how to use computers to be prepared for the EHR (PM–PIG 2.2). Approximately 9 months after the system was implemented, the partnership also arranged a follow-up targeted training workshop based on specific issues that had emerged during the EHR's day-to-day use (PM–PIG 2.2–2.5). This allowed CHCD staff to review their past use experience, exchange opinions and ‘tricks’, while simultaneously getting feedback from the partnership's technical team. This workshop was deemed extremely helpful and significantly improved the consistency of EHR use among all CHCD practitioners.
End user acceptance evaluation: a comparison between the two study sites
At the baseline, T0, complete survey responses were obtained from five clinicians from Glide and four clinicians from CHCD, respectively. The follow-up surveys were administered at 3 months (T1, n=9), 6 months (T2, n=10) and 9 months (T3, n=9) post-implementation at Glide, and 3 months (T1, n=3) and 6 months (T2, n=6) post-implementation at CHCD. The sample size is small due to the small staff size of the two NMHC.
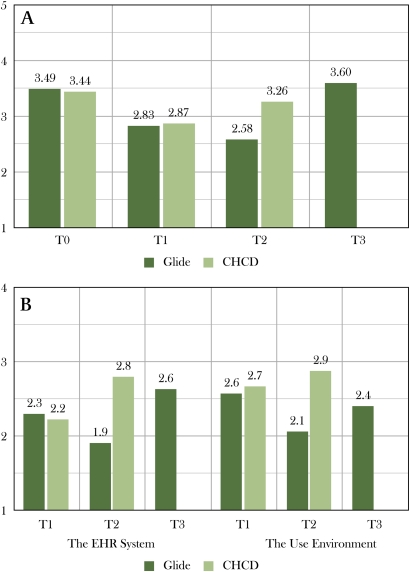
The results revealing the clinicians' attitudes toward EHR are depicted in figure 1A. Before the EHR implementation (T0), the average computer optimism scores at both Glide and CHCD were very similar: from neutral to mildly positive (3.49 and 3.44, respectively, on a 1–5 scale where five represents ‘highly beneficial’). At T1, a considerable decrease was observed at both sites (Glide 2.83; CHCD 2.87). Nonetheless, CHCD's T2 results (3.26) had nearly returned to its pre-implementation levels (3.44).
Figure 1.
End user survey results. (A) Clinicians' attitudes toward the use of electronic health records (EHR) in clinical care (construct mean; 1–5: ‘highly detrimental’, ‘detrimental on the whole’, ‘neither detrimental nor beneficial’, ‘beneficial on the whole’ and ‘highly beneficial’). (B) End user evaluation of the EHR system and the use environment (construct mean; 1–4: higher values indicate more positive evaluation). CHCD, Campus Health Center, Detroit.
At Glide, clinician optimism declined further between T1 and T2 (from 2.83 to 2.58). Nonetheless, at T3, it rebounded to 3.60, which is the highest level observed in this study. This curve-bending result suggests that despite the initial frustrations likely due to the issues described in the case study section, the clinicians at Glide re-established a positive attitude toward EHR 9 months after the implementation. According to the technology acceptance literature, such a positive attitude is a critical, immediate factor determining if a technological innovation will be accepted by its targeted end users.30 34 35
Figure 1B exhibits the results obtained through the EHR end user evaluation questionnaire. At T1, mean response was slightly more positive regarding the EHR use environment than the EHR system itself (2.6 vs 2.3 at Glide and 2.7 vs 2.2 at CHCD, respectively). At T2, the results at the two NMHC sites diverged, with CHCD tending toward the positive side on both measures (2.9 and 2.8) and Glide tending toward the negative side (2.1 and 1.9). Nonetheless, Glide's T3 results improved considerably on both measures (2.6 for the EHR system and 2.4 for the use environment). These results resonate with the findings on the developmental trajectories of the clinician optimism measure. They are also in agreement with the technology acceptance literature: it has been shown that end users' evaluation of a technology (usefulness and ease of use) and their perception of the use environment (facilitating conditions) are key factors driving their attitudes toward the technology, which in turn determines their ultimate acceptance behavior.30 34 35
Discussion
As described in the case study section, the two NMHC were highly motivated to adopt and utilize EHR to improve their operational efficiency and quality of clinical practice. However, due to resource constraints, they had encountered extreme difficulties on the journey toward EHR and in the aftermath of go-live as both practices struggled to use the technology meaningfully to transform the provision of their patient care services.
First, challenges arising from their inadequate computer infrastructure and inability to get cooperation from external entities were particularly prominent. Glide, for example, experienced protracted difficulties in issues related to network connectivity and data interfaces, and clinician satisfaction scores reflect this trajectory. This observation also made it clear that having ancillary data integrated into EHR in a structured format, laboratory test results in particular, is pivotal to achieving user acceptance in a busy primary care practice. Unfortunately, despite best efforts, both sites continued to receive laboratory data on paper forms and faxes for an extended period of time due to numerous practical constraints.
Second, while the initial SWOT analyses were valuable and led to the identification of key barriers to implementation, not all complicating conditions emerged during the readiness assessments and strategic planning phase: certain environmental changes were unpredictable and uncontrollable such as the sudden downturn of the economy in California. Therefore, the partnership's continuous support after go-live played a pivotal role in helping the two centers reach the eventual implementation success. Such support included: (1) ongoing negotiation with the NMHC external partners (eg, outpatient laboratories); (2) ongoing consultation and training on software customization and process optimization and (3) ongoing conversations with the practices' leadership and parent organizations to gain resources to create facilitating conditions such as IT support.
Third and finally, clinicians' overall attitudes toward the use of EHR in clinical care, and their evaluation of the quality of implementation of a particular system, are influential factors determining if they will be self-motivated to fully integrate the system into their day-to-day clinical routines.30 35 This self-motivation is extremely important to the realization of the true value of EHR, considering that the broader objectives of EHR on quality improvements and cost reduction can only be achieved through clinicians' full utilization of the value-added capabilities such as computerized clinical decision support. Such capabilities, however, could be easily circumvented in the absence of end users' self-motivation. The longitudinal survey results suggest that at both study sites unexpected implementation issues and adaptation difficulties adversely affected clinician satisfaction during the early stages. Even though such adverse effects diminished eventually, they lasted for an extended period and could not have been resolved without the partnership's long-term, hands-on assistance. This observation reinforced our belief that a strong and long-lasting collaborative relationship between EHR implementers and adopting healthcare practices (therefore ‘partnership’) is the only way to shield healthcare practices from adoption difficulties and uncertainties during their long journey toward the adoption and meaningful use of EHR.3
As the next step forward, the partnership has also worked with the participating practices, from very early on, to create a collective capability that will enable them to actively participate in clinical, translational and comparative effectiveness research. This objective is being achieved through EHR implementation, emphasis on quality of data and use of standards, and the establishment of a community-wide analytical data warehouse (PM–PIG 3.4, 3.5). On 1 September 2010 the partnership was awarded a HRSA grant in recognition of this effort as a key node of a nationwide community health applied research network to demonstrate that safety net providers and academic institutions can partner together to create an effective infrastructure to support patient-centered outcomes research.
Conclusion
This paper presents a partnership-based and community-oriented approach designed to facilitate EHR implementation in resource-limited primary care settings. We illustrate the model through two case studies based on our recent experience in deploying EHR systems at two NMHC, a particularly vulnerable primary care environment. We show that despite careful initial planning, emerging conditions brought with or magnified by later processes often invalidate previous assumptions, thus necessitating an iterative and continuous approach. This learning is particularly pertinent to resource-limited primary care settings as very few of them will have all facilitating conditions in place before embarking on the journey toward EHR. The partnership model described in this paper, with a prominent focus on CQI, may therefore provide useful insights into the work shepherded by the HIT regional extension centers, which are dedicated to supporting resource-limited communities disproportionally affected by EHR adoption barriers.
Supplementary Material
Footnotes
Funding: This work is supported by grant no 1R18HS017191 received from the Agency for Healthcare Research and Quality (PI: JMP), and in part by funding received from the W.K. Kellogg Foundation.
Competing interests: None.
Ethics approval: The research protocol of this study was reviewed and approved by the Medical School Institutional Review Board at the University of Michigan (IRB no HUM00015728) and the research ethics governing bodies at the respective study sites.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, USA: National Academy Press, 2001 [PubMed] [Google Scholar]
- 2.Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med 2009;360:1477–9 [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med 2010;363:501–4 [DOI] [PubMed] [Google Scholar]
- 4.Furukawa MF, Raghu TS, Spaulding TJ, et al. Adoption of health information technology for medication safety in U.S. Hospitals, 2006. Health Aff (Millwood) 2008;27:865–75 [DOI] [PubMed] [Google Scholar]
- 5.DesRoches CM, Campbell EG, Rao SR, et al. Electronic health records in ambulatory care—a national survey of physicians. N Engl J Med 2008;359:50–60 [DOI] [PubMed] [Google Scholar]
- 6.Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med 2009;360:1628–38 [DOI] [PubMed] [Google Scholar]
- 7.Ash JS, Bates DW. Factors and forces affecting EHR system adoption: report of a 2004 ACMI discussion. J Am Med Inform Assoc 2005;12:8–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berner ES, Detmer DE, Simborg D. Will the wave finally break? A brief view of the adoption of electronic medical records in the United States. J Am Med Inform Assoc 2005;12:3–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ford EW, Menachemi N, Peterson LT, et al. Resistance is futile: but it is slowing the pace of EHR adoption nonetheless. J Am Med Inform Assoc 2009;16:274–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kaplan B, Harris-Salamone KD. Health IT success and failure: recommendations from literature and an AMIA workshop. J Am Med Inform Assoc 2009;16:291–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52 [DOI] [PubMed] [Google Scholar]
- 12.Linder JA, Ma J, Bates DW, et al. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med 2007;167:1400–5 [DOI] [PubMed] [Google Scholar]
- 13.Jones SS, Adams JL, Schneider EC, et al. Electronic health record adoption and quality improvement in US hospitals. Am J Manag Care 2010;16(12 Suppl HIT):SP64–71 [PubMed] [Google Scholar]
- 14.Romano MJ, Stafford RS. Electronic health records and clinical decision support systems: impact on national ambulatory care quality. Arch Intern Med 2011;171:897–903 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293:1197–203 [DOI] [PubMed] [Google Scholar]
- 16.Campbell EM, Sittig DF, Ash JS, et al. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 2006;13:547–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Research Council Computational Technology for Effective Healthcare: Immediate Steps and Strategic Directions. Washington, DC, USA: National Academies Press, 2009 [PubMed] [Google Scholar]
- 18.Kuehn BM. IT vulnerabilities highlighted by errors, malfunctions at veterans' medical centers. JAMA 2009;301:919–20 [DOI] [PubMed] [Google Scholar]
- 19.Miller RH, West CE. The value of electronic health records in community health centers: policy implications. Health Aff (Millwood) 2007;26:206–14 [DOI] [PubMed] [Google Scholar]
- 20.Shields AE, Shin P, Leu MG, et al. Adoption of health information technology in community health centers: results of a national survey. Health Aff (Millwood) 2007;26:1373–83 [DOI] [PubMed] [Google Scholar]
- 21.Jha AK, DesRoches CM, Shields AE, et al. Evidence of an emerging digital divide among hospitals that care for the poor. Health Aff (Millwood) 2009;28:w1160–70 [DOI] [PubMed] [Google Scholar]
- 22.Torda P, Han ES, Scholle SH. Easing the adoption and use of electronic health records in small practices. Health Aff (Millwood) 2010;29:668–75 [DOI] [PubMed] [Google Scholar]
- 23.Linder SH, Quill BE, Aday LA. Academic partnership in public health practice. In: Novick LF, Benjamin GC, Mays GP, eds. Public Health Administration: Principles for Population-Based Management. Gaithersberg, MD, USA: Aspen Publishers, 2001:521–39 [Google Scholar]
- 24.Levin J, Tadelis S. A theory of partnerships. Stanford Law and Economics Olin Working Paper No. 244. In: Stanford Law School, Law and Economics Research Paper Series. Stanford, CA, USA: John M. Olin Program in Law and Economics, 2002 [Google Scholar]
- 25.Ansoff HI. Corporate Strategy. New York City, NY, USA: McGraw-Hill, 1965 [Google Scholar]
- 26.Deming WE. Out of the Crisis. Cambridge, MA, USA: MIT Press, 1982 [Google Scholar]
- 27.Zheng K, McGrath D, Hamilton A, et al. Assessing organizational readiness for adopting electronic health record systems: a case study in ambulatory practices. J Decis Syst 2009;18:117–40 [Google Scholar]
- 28.Swanson B, Ramiller N. Innovating mindfully with information technology. MIS Quarterly 2004;28:553–83 [Google Scholar]
- 29.Cork RD, Detmer WM, Friedman CP. Development and initial validation of an instrument to measure physicians' use of, knowledge about, and attitudes toward computers. J Am Med Inform Assoc 1998;5:164–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: toward a unified view. MIS Quarterly 2003;27:425–78 [Google Scholar]
- 31.Pohl JM, Hanson C, Newland JA, et al. Unleashing nurse practitioners'potential to deliver primary care and lead teams. Health Aff (Millwood) 2010;29:900–5 [DOI] [PubMed] [Google Scholar]
- 32.Barkauskas VH, Pohl JM, Tanner C, et al. Quality of care in nurse-managed health centers. Nurs Adm Q 2011;35:34–43 [DOI] [PubMed] [Google Scholar]
- 33.Sittig DF, Krall M, Kaalaas-Sittig J, et al. Emotional aspects of computer-based provider order entry: a qualitative study. J Am Med Inform Assoc 2005;12:561–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fishbein M, Ajzen I. Beliefs, Attitude, Intention and Behavior: An Introduction to Theory and Research. Reading, MA, USA: Addison-Wesley, 1975 [Google Scholar]
- 35.Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13:319–40 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.