Abstract
Background
There is growing interest in the use of technology to enhance the tracking and quality of clinical information available for patients in disaster settings. This paper describes the design and evaluation of the Wireless Internet Information System for Medical Response in Disasters (WIISARD).
Materials and methods
WIISARD combined advanced networking technology with electronic triage tags that reported victims' position and recorded medical information, with wireless pulse-oximeters that monitored patient vital signs, and a wireless electronic medical record (EMR) for disaster care. The EMR system included WiFi handheld devices with barcode scanners (used by front-line responders) and computer tablets with role-tailored software (used by managers of the triage, treatment, transport and medical communications teams). An additional software system provided situational awareness for the incident commander. The WIISARD system was evaluated in a large-scale simulation exercise designed for training first responders. A randomized trial was overlaid on this exercise with 100 simulated victims, 50 in a control pathway (paper-based), and 50 in completely electronic WIISARD pathway. All patients in the electronic pathway were cared for within the WIISARD system without paper-based workarounds.
Results
WIISARD reduced the rate of the missing and/or duplicated patient identifiers (0% vs 47%, p<0.001). The total time of the field was nearly identical (38:20 vs 38:23, IQR 26:53–1:05:32 vs 18:55–57:22).
Conclusion
Overall, the results of WIISARD show that wireless EMR systems for care of the victims of disasters would be complex to develop but potentially feasible to build and deploy, and likely to improve the quality of information available for the delivery of care during disasters.
Keywords: Electronic Health records, disasters, wireless, mobile computing
Introduction
This paper discusses an application of information technology to enhance the care of patients at a disaster site. Recent events illustrate the wide variety in type and scope of disasters that an information technology (IT) system for disaster care must address: rocket attacks in Israel; suicide bombings in Iraq, Afghanistan, and Pakistan; the coordinated bombings in Madrid1 and London;2 the Tsunami disaster in South East Asia; Hurricane Katrina;3 and the Haitian Earthquake. These events add to the lessons learned from earlier disasters such as the 9-11 attacks, the Bhopal chemical disaster,4 and the Tokyo-subway sarin-gas attack.5 In addition, disaster IT systems must be able to address the other threats our nation prepares for: a dirty bomb (an explosive-dispersed radiation device) or nuclear-bomb detonation,6 or an anthrax ‘sprayer’ attack on a city.7 While no system will be completely functional in all of these settings, the objective of research in disaster informatics is to identify the principles that will maximize the utility of systems across settings.
The accurate tracking of patients and patients' data is a central component in medical management of mass casualty incidents (MCIs).1–5 By tracking the types of symptoms patients are experiencing, responders can more readily determine the nature of the threat and manage the logistics of response on the field.6 The right patients need to get to the right facilities that have the resources for their care. This is made more complex because resources for care in the community in a postdisaster setting are limited and often degraded by the disaster. There is a further need, from a humanitarian perspective, to provide information to the survivors of disasters about which of their relatives are alive and where they are being treated. Unfortunately, problems with patient tracking are common. During the Hurricane Katrina disaster, more than 12 500 adults and 5000 children were registered as missing.8 One place where victims and/or critical medical information are ‘lost’ is in the transition from field care sites to hospital. Johnson and Calkins looked at series of 45 smaller MCIs in the state of New York and found that in only 44% of incidents were all victims appropriate tracked prior to assignment to a treating hospital. Further, in many incidents, the appropriate clinical data were not available at the time of hospital assignment decisions.9 Problems with lost or missing patients, missing clinical data, and/or lost linkages between patients and their clinical data occur even in field exercises.10 11
A number of groups have developed systems designed to improve the management of medical information in mass casualty events. Prior work in this area is summarized in table 1. In general, such systems have two components: victim tracking (often called mass casualty tracking) and field care management. Victim-tracking systems manage records of the severity and disposition of patients to enhance the situational awareness of decision-makers. Field care systems are systems designed for use in mobile environments for initial stabilization of victims with electronic health record (EHR)-like features. Different systems have been developed for different use cases with different technologies. For example, Battlefield Medical Information System Tactical—Joint (BMIST-J) was developed for use by Army medics in the field and avoids radio-frequency identification (RFID) technologies to prevent enemies from targeting wounded soldiers by signal tracking. Other systems, such as the Raytheon system focused on using the capabilities of existing cellular systems and devices for mass casualty tracking. Still other groups have explored the possibilities of using Motes, a type of low-power computer designed for networked sensor applications, for disaster response applications.21 29 Investigators also have studied the use of WiFi (802.11) systems for monitoring of patients' vital signs and other telemetry as part of comprehensive systems for field care.22 30
Table 1.
Features of existing IT systems for field care and mass-casualty tracking
| System | Scope | Network | Patient-tracking device | Sensors | Other devices | Transaction model | References |
| ARTEMIS | Mass casualty tracking and field care | WiFi | Handheld computer | ECG, pulse oximeter | Client push | 12 | |
| Army BMIST-J and MC-4 | Field care | Smart tag or desktop sync | Smart dog tag | None | Handheld computer | Synchronization | 13 |
| Navy Tacmed-cs and Theater Medical | Field care | RFID tag or desktop sync | Passive RFID tag wrist band | None | Handheld computer | Synchronization and client push | 14 15 |
| Raytheon | Mass casualty tracking | Cellular or WiFi | Paper triage tags with barcode | None | Cell phone or handheld computer | Client push | 16 |
| mTriage | Mass casualty tracking | SMS cellular | Passive RFID tag | None | Cell phone with RFID reader/writer | Client push | 17 |
| EMsystems | Mass casualty tracking | WiFi to cellular or satellite | Paper triage tags with barcode | None | Handheld computer | Client push | 18 |
| TACIT | Mass casualty tracking | WiFi with cellular or satellite | None | None | Handheld computer | Client push | 19 |
| iRevive | Field care | Zigbee to WiFi to cellular or satellite | Mote RFID device | Pulse oximeter, blood pressure, and ECG | Handheld computer | Client push | 20 |
| AID-N | Field care and mass casualty tracking | Zigbee to WiFi to cellular or satellite | Mote RFID device | Pulse oximeter, blood pressure, and ECG | Handheld computer | Client push | 21 |
| WIISARD | Field care and mass casualty tracking | WiFi to WiFi mesh network to cellular or satellite | WiFi RFID devices and paper triage tags with bar code | Pulse oximeter | Handheld computer, tablet computer | Publish and subscribe with synchronization | 22–28 |
RFID, radio-frequency identification.
The objective of the Wireless Internet Information System for Medical Response in Disasters (WIISARD) was to develop and evaluate a comprehensive system for status and care of victims of a disaster or terrorist attack. The project used a systems approach focused on enhancing the medical functions of Metropolitan Medical Response System (MMRS) units—one of the first responder units that might be called upon to respond to the disasters described above. This resulted in the creation of a number of purpose built devices and software systems described below.
Background
MMRS supports the integration of local emergency management, health, and medical systems into a coordinated response to MCIs. MMRS units are Department of Homeland Security-sponsored teams that integrate law enforcement and hazardous materials, pre-hospital, medical, and public-health first responders into organized teams designed to respond to chemical, biological, radiological, or even nuclear accidents or terrorism.31 The MMRS is designed to coordinate local response to such an event in the first 48 to 72 h before Federal resources become available. Approximately 120 distinct geographic regions across the country are part of the MMRS. Each region fields a Metropolitan Medical Strike Team. These teams are drawn from groups of local first responders and are regional assets under the control of mayors or county officials coordinated through mutual aid agreements among entities in a region. MMRS operations can augment existing local operations as in the examples below:
joint law enforcement and rescue missions, with the aim of close cooperation between tactical and medical teams, with the goal of getting to victims sooner and getting them out of hazardous areas faster;
advanced training for first responders and pre-hospital personnel with special protective gear to allow early penetration into contaminated areas;
systems for mass field decontamination and treatment of victims at MCIs;
enhance capabilities for stabilization and extended field care of victims if definitive care sites and resources such as hospitals are compromised or overwhelmed with patients.
The San Diego MMRS unit functions in the MCI setting with five teams.
The entry team combines paramedics with special weapons and tactics officers to locate, triage, and retrieve victims from a threat zone.
A decontamination team treats victims to remove toxins such as nerve gas or other exposures.
The medical stabilization team retriages patients, performs a more detailed exam, and administers field care.
The transport team, manages the arrival of ambulances and the loading of victims for transport to definitive care sites.
The Med-Com team works with offsite medical personnel, typically a regional coordinator, to track available hospital resources and allocate victims to hospitals based on their available capacity.
The entire process is managed by the Medical Operations Director, who reports to the Incident Commander.
Patients flow through this system, passing from team to team until the ambulance they are in delivers them to their treating hospital. Individual teams function in an independent manner, doing what is necessary to move patients through the system as quickly as possible. This division of labor provides for the greatest efficiency when first-responder personnel may be limited in the face of overwhelming numbers of casualties. However, this patient flow also creates a system dependent on multiple handoffs of victims to different personnel at the scene, and thus communication becomes critical between providers. Communications are aimed at enhancing global situational awareness (how many victims, what kinds of injuries, what threats are present in the environment) and at improving the quality of handoffs between teams for movement of patients through the system. Current strategies for management of communications for MMRS teams include the use of multiple radio bands to pass information. Team leaders work with team members on one radio channel and then switch to a second channel to report findings to their peer-level team leaders and superiors.
WIISARD attempted to design approaches to enhance the functioning of the entire system, focused on enhancing information flow and the global situational awareness of all teams in the MMRS unit. To that end, we developed both hardware and software systems. Development used agile methods working closely with experts from the San Diego MMRS over a 3-year period. Prototypes were tested in a series of MMRS exercises conducted from 2004 to 2006. Progressively more capable systems were developed over this period. Failure modes were identified, revisions to systems were made, and systems were retested.
Design objectives
The overall objective of WIISARD program was to conduct research that would inform the development of a wireless scalable rapidly deployable electronic medical records (EMRs) system for victim tracking and field care at disaster sites. Design requirements were scenario-based, to meet the demands for the care of victims in incidents such as those involving a terrorist attack inside a public building, potentially involving a nerve-gas agent or a radiation-dispersing (‘dirty’) bomb.
First responders upon arrival at the site would deploy a network that was robust and scalable, particularly with regard to extending coverage areas into structures. The triage and tracking of patients would begin in the ‘hot zone’—the contaminated or threatened area inside the attack site. A medical first responder, potentially in bulky hazardous materials protective gear that would limit their operation of complex devices, would enter the threatened space, immediately following law-enforcement officers who were neutralizing threats from armed terrorists. The responder would place an electronic tag on each victim, enter the victim's triage status on the tag, and then proceed to the next victim. The tag would report the victim's general location and display the victim's triage status in an easily visible way. A transport team would subsequently retrieve patients, in the order of their medical urgency, using the triage tags as beacons. They would decontaminate patients using a spray shower. After decontamination, victims would be handed off to another medical team, retriaged, treated to stabilize their injuries, and transported off the field. The WIISARD system would store all medical data including physical examination findings and treatments administered and distribute those data among members of medical teams caring for patients. The WIISARD system would also monitor the vital signs of the most severely injured patients. Team members would use the system to assign patients to modes of transport and to destinations for definitive care at local hospitals. Because patients might have to travel long distances to treatments sites that had limited connectivity, triage tags would carry the data from field care with the patient off the site. However, the data would need to be easily retrievable by medical personnel at the treating facility without any special equipment. In addition, hospitals and regional coordinators should be able to connect to the on-site WIISARD system over the internet, given that cellular networks were operating or a satellite link was established, and review the types of casualties seen at the site and the casualties en route to their facility.
The WIISARD system would improve the quality of field care by:
enhancing triage decision-making through embedded decision support;
improving the quality of documentation of injuries and of treatments through better management of medical data;
automatic monitoring of patients using wireless physiological sensors;
improving unit situational awareness through automated distribution of information across the team;
improving the safety of care delivery by automated tracking the locations of victims, first responders, and threats.
Technical constraints
WIISARD developers assumed that first responders would need to provide their own wireless data communications network after an event and that, at best, there would be limited external bandwidth for communications. Further, we assumed that there would be very limited technical support available onsite. After deployment, the network would need to be able to configure itself automatically for optimal distribution of data to devices when initially deployed. It would also need to be able to recognize and reconfigure itself when new nodes were added to the network to extend its coverage.
Common computer devices would need to be able to use the network to control costs and support interoperability between units from different jurisdictions. We assumed that most devices on the network would not have built in geolocation capabilities and that networks would also need to support geolocation capabilities for devices that did not have GPS units built in. Further, we assumed communications would be unreliable. Early in our experience, we observed that fire trucks and other rescue equipment often put out large electromagnetic footprints that jammed networks. Simple client server mechanisms that submitted and retrieved information from remote databases would ‘lock up’ for extended periods.
We also observed how simple transactional systems could fail in disaster environments. Mass updating of systems might be needed after periods of network disruption. The identification of a contaminant in the environment or threat might require updating of information on many first-responder devices at same time. Simple transactional models could result in unacceptably high bursts of high demands for transactions and bandwidth in such circumstances. We therefore explored alternatives to this model.
Another design requirement stemmed from the need for the WIISARD system to be able to integrate legacy systems, such as paper triage tags. Victims might stream out from an event and be managed using best available methods such as paper triage by other first responders, prior to the arrival of the MMRS. To obtain accurate victim counts and to manage distribution of patients, WIISARD would need to accept patients who had other kinds of tags, create records for these patients, and manage them.
Implementation
WIISARD was designed as a modular system with a variety of different components. Each is described below.
802.11 networking system
To meet the networking needs of the WIISARD system, we developed the Calmesh network. This network was designed to be scalable, automatically reconfiguring its routing tree to the most efficient distribution system. New nodes could be detected and added to the networks' distribution tree, and the network would reconfigure its distribution appropriately and automatically. A Calmesh network is composed of an arbitrary number of Calmesh Nodes. These devices are one-button-on, purpose-built Linux computers that accept multiple wireless networking cards. The computers are enclosed in water resistant cases and have a long battery life that allows continuous operation of network nodes for up to 18 h without recharging. Calmesh nodes form a self-scaling, self-healing WiFi. Ordinary WiFi devices can connect to any node. Nodes speak with each other via a mesh protocol to form a grid. Network nodes include a GPS unit to relay their position. Systems in WIISARD without GPS units use trilateration of 802.11-signal strength from the Calmesh nodes for geolocation outdoors or node association when indoors. Calmesh nodes have been used to create WiFi bubbles over 1.5 km in diameter24 and can sustain transmission speeds of over 2 mb/s.23 However, the addition of new nodes, at present, results in temporary disruption of the network for reconfiguration.
WIISARD database and objects
To overcome issues related to the unreliability of networks and the need to constantly update all providers with the latest information on casualty counts, in a scalable way, we developed publish/subscribe architecture designed to allow software programs to function independently when disconnected and then rapidly synchronize with the main database. The publish/subscribe service also distributed data throughout the system at regular intervals, updating casualty counts and other critical data. The main database publishes various data objects. Software programs on Mid-Tier and First-Tier devices (described below), when activated, subscribe to data objects from the server. Client devices with subscriptions update the model, with the result being disseminated (pushed) to all other subscribe clients. To enable a client to tolerate its own loss of network, each client held a cached objects abstraction layer (COAL) (in essence, a write-through cache) to store local changes. Should a client become disconnected, the device is still able to update its local copies of the data objects. When reconnected, changes were integrated by a roll-back, roll-forward mechanism, and then relevant updates were distributed throughout the network. Intelligent triage tags (ITTs) and pulse oximeters (see descriptions below) had low-power processors that were not capable of maintaining their own COALs. For these devices, virtual COALs were maintained on the server. Changes in state automatically triggered device state updates when reconnected. The software had self-scaling capabilities that included the ability to allow clients to automatically subscribe to data objects on the server allowing the system to expand as more responders joined the network. The data communications architecture of the WIISARD system is described in detail in Brown et al.25
Intelligent triage tags
When medical care is initiated at a mass casualty event, the first activity is to triage victims, which is classifying victims by the severity of their injuries. For WIISARD, we developed ITTs, an electronic device to coordinate patient field care. ITTs combine the basic functionality of a paper triage tag with a communications device, an EMR, and an RFID tag.22 ITTs were designed for chemical–biological and radiation-threat environments, where spacesuit-like protective gear prevents responders from using personal digital assistants or other computer devices. They are water resistant (to survive decontamination) and have a two-button interface with menu driven configuration. When a victim's triage status is changed by another provider, ITTs also flag these updates with a bright flashing LED. In addition to transmitting and displaying triage information, ITTs also display procedural information and instructions. Their LCD screens are used to display alerts and instructions for care of the patient (eg, ‘load in ambulance 38’). They also flash multiple LEDs for alarms.
The final function of ITTs is to record medical data for later access offsite. All physical exam findings and treatments are stored in the ITTs' (non-volatile) memory. When patients are off site, ITTs can be configured into wireless web servers that deliver an EMR of field care to any laptop with WiFi capability and an installed web browser.
iMOX sensor platform
In a mass-casualty situation, medical personnel at the disaster site and other field treatment settings may need to monitor the vital signs of hundreds of seriously injured patients with minimal staffing. The conditions may be primitive, and personnel may have to improvise infrastructure. As part of our research to enhance medical response to disasters with internet-enabled systems, we developed a prototype wireless blood pulse oximeter system for mass-casualty events designed to operate in WiFi hotspots.22 Pulse oximeter units were designed using low-cost embedded system technologies to operate in integrated or stand-alone environments. Units can report data to a command post-on the scene or any remote location with Internet access. iMOX units are based on a hardware/software platform used in ITTs. iMOX units can be used at ITTs or linked with an ITT to simplify workflow issues.
First-tier device
Medical first responders triage and treat victims throughout a mass-casualty response. The First-Tier system is a wireless handheld device with an EMR that allows these responders to triage and record physical examination findings and treatments. The components of this system, the WIISARD First Responder, include a personal digital assistant (PDA) with 802.11 wireless transmission capabilities, a laser bar-code scanner and EMR software that replicates the rapidity and ease of use of the standard paper triage tag for the Simple Triage and Rapid Treatment system.32 33 It contains additional fields for entering information about physical examination findings and treatments not found on paper triage tags. The WIISARD First-Tier system includes an HP 5555 handheld device with a Linux operating system. The Linux OS was modified to enhance the speed of recognition of WiFI networks and the speed of reassociation from one subnetwork to another. The First-Tier system has a WIISARD COAL client that provides seamless transitions between connected and disconnected operations. The barcode scanner allows providers to integrate victims tagged with paper triage tags with bar codes into the WIISARD system,34 thereby meeting our requirement for integration with pre-existing paper systems.
Mid-tier software system
Mid-tier managers are the supervisors of groups of first responders stationed at triage, treatment, and transport areas as well as other, more ad hoc, areas. Mid-tier managers make higher-level decisions about patients: identifying those most in need of medical care and rapid transport, and coordinating requests for resources needed in their area of supervision (Decontamination, Triage, Treatment, Transport, Med-Com). In the field, they are typically equipped with clipboards, pen and paper forms (sometimes dedicated scribes), and radios. They use their paper forms to track victim numbers, status, and destinations. They collaborate with other mid-tier supervisors by talking face to face, while looking at each other's forms, and when apart they are in frequent radio communication with each other.
The WIISARD system replaces these paper worksheets with tablet computers, and replaces the need for many of the radio calls for information by distributing networked data. The data available to supervisors include all information fields from victim tags, any other data entered using the First-Tier device, as well as data entered about hospital availability and the arrival of ambulances and the current queue. The graphical user interfaces have been designed to provide maximal access to data on patients and resources, while still being tailored to the specific tasks and duties of the scene manager. Triage area managers have access to all logged triage patients and their acuity and decontamination status. Treatment area managers have access to lists of patients in their medical areas, their condition and vital signs. Transport managers can use electronic logs to assign patients to ambulances on scene and designate destination hospitals for disposition.26 Hospitals and regional coordinators can view casualties on the field and manage reported receiving capabilities.35 All users can switch rapidly between the views developed for any other user by clicking on a tab. Managers used barcode readers to identify and record data on individual patients. An attached camera system allowed them to add photographs of victims to aid in identification. The mid-tier system runs on any Windows XP operating system computer but is optimized for computers with pen or touch-screen capabilities.
Command-center software system
The WIISARD command-center system is design to help the Medical Director and the Incident Commander understand the MMRS unit's performance from a systems perspective. The command-center system displays the location of first responders and patients. It also provides graphical displays of data quality (latency in reports from teams) and estimates of system through put. It is a communications platform and has the ability to share diagrams with relevant features (hot zones and other hazards, tactical plans) overlaid on maps27 with the Mid-Tier system. Additional alerting and decision-support capabilities are under development.36
System-evaluation methods
Having conducted formative evaluations of most of the individual components of WIISARD in prior exercises, the evaluation of WIISARD focused on the feasibility of using the clinical portions of the system to care for patients in a mass-casualty setting. We completed development of a full working model of the WIISARD system, including 20 Calmesh nodes, 42 ITTs, five iMOX units, 18 first-tier handheld devices, six Mid-Tier tablets, and a mobile server and command center system that was powered by a generator. We then worked with our partners in the San Diego MMRS to deploy this model system during a large-scale, realistic disaster drill.
The drill was designed by MMRS leaders primarily as a training exercise for first responders. We were allowed to add a technical evaluation of WIISARD to this scenario. The training scenario called for a terrorist takeover of a building with multiple casualties due to gunshot wounds and use of explosive devices. The building contained toxic chemicals that were released during explosions. The terrorists behind the attack took up positions on the top floor of the building with hostages, leaving behind additional explosive devices for MMRS team members to find and disarm. The mission of the MMRS team in the exercise was to secure the lower floors of the building, remove wounded victims, capture the terrorists, and free the hostages. MMRS providers received about 30 min of training in use of the WIISARD system prior to the drill (though some had tested the equipment in a previous exercise). All first responders in the exercise were members of the San Diego Regional Metropolitan Medical Strike Team—an elite organization with quarterly training exercises and annual full-scale drills. Responders were highly familiar with the paper mass casualty management system, having used this method in multiple training exercises during the 3 years preceding the evaluation exercise. Equally experienced responders were assigned to both arms of the study. The responses of both groups to the challenges of adopting relatively unfamiliar workflows in a mass casualty setting were part of the evaluation.
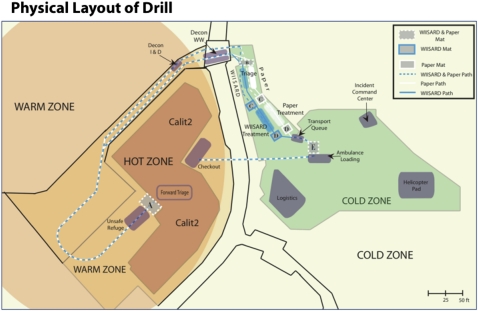
The layout of the training exercise is shown in figure 1. The exercise area was broken down into ‘hot,’ ‘warm,’ and ‘cold’ zones based on the simulated threat level (‘hot’ denoting a high threat; ‘cold’ being a safe zone). The areas inside the building where the terrorists were barricaded was the hot zone, and the immediate surrounding area the ‘warm zone.’ The ‘cold zone’ was in the parking lot outside the building. In this area, two parallel systems were set up, one for WIISARD and one for the paper-based system. The exercise used 100 simulated victims with balanced levels of injuries. We recruited simulated victims from the UCSD student population for the exercise, and 50 victims were randomly assigned to each arm of the study. Each arm also had victims who played deceased or mortally wounded (‘expectant’) victims who were not evacuated and hostages who remained in the building for the entire exercise. Each arm had victims who entered the treatment arms themselves on their own accord (based on their medical scenarios) as well as those who needed to be evacuated from the building by stretcher. A fraction of the victims had progressive scenarios where victims became worse as the exercise evolved. Medical scenarios across arms were carefully balanced across study arms. As shown in figure 1, victims exited the California Institute of Telecommunications and Information Technology (Calit2) Building via one door and were escorted to a common decontamination station, where they went through outdoor showers remove chemicals present as part of the drill script. They were then sent into one of two care systems: the WIISARD care system or the paper-based control field care system.
Figure 1.
Geographical layout of the exercise with the locations of tracking mats and Metropolitan Medical Response System teams for Wireless Internet Information System for Medical Response in Disasters (WIISARD) and control systems. Decon WW is decontamination area Walking Wounded triage category patients. Decon I & D is the decontamination area for Immediate and Delayed triage category patients.
Portions of the networking system were predeployed and optimized for network traffic. The technical feasibility of self-scaling network approaches had been demonstrated in previous exercises. Therefore, this exercise focused only on the feasibility of adding additional nodes to the network inside the building as first responders entered it and cleared sections of suspected terrorists.
The primary outcome measure was the quality of medical data about victims that were generated in each pathway. Are all patients accounted for, or are some lost in the system, or end up in hospitals without any record left on field? How much information about victims is recorded and made available? Do errors of transmission creep in? Are patients correctly identified and continuously linked with their data?
At a population level, we studied the degree to which systems accurately counted the numbers of casualties and the levels of injuries in both pathways. Injuries were divided into four levels of triage status: expectant (who were too severely wounded to recover), immediate (who required early definitive treatment), delayed (who had serious but non-life threatening injuries, and walking wounded (who had moderate injuries but who could both wait for care and transport themselves). We also reviewed the ability to accurately link medical data on individual victims within the pathway. Both pathways had systems to maintain unique victim identification numbers that linked data on injuries, treatment administration, and disposition. The accuracy of victim identification and tracking in both pathways was compared. To track victims independent of the WIISARD system, we gave each victim a numbered and color-coded (control vs WIISARD) football jersey, and set up fixed-location video cameras to record their movements across the field. Videotapes of ongoing care processes and of simulated victims shirt numbers were used to track victims and actual movements, and were compared with data in paper forms used by the Med-Com, Treatment, and Transport supervisors and computer logs. We determined the degree to which each system allowed linkage between the medical data collected on the field for each victim and the disposition of the victim. We also examined the rates of completion and documentation of medical status in each arm (Simple Triage and Rapid Treatment acuity, assessment, decontamination status, disposition). This was evaluated by comparing the WIISARD database with any documentation on either triage tag or paper logs for the conventional pathway.
A second issue examined was the impact of WIISARD on the situational awareness of the treatment teams. To examine this, we recorded all radio communications from first responders in both treatment arms and compared the number of conversations between team members. We hypothesized that WIISARD would reduce the need for radio communications because it distributes information about victims across the care teams and displays that information in an easy-to-read form on-screen.
To further study the effects of WIISARD, the team leads for each area were followed by a cameraman with a mobile video camera. The cameraman recorded interactions with other responders and the state of paper-based documentation materials. All video materials were digitized, time-coded, and indexed. Videotapes from fixed and mobile cameras were reviewed and coded, and the results of analyses abstracted.
Last, we needed to determine if the additional record-keeping required within the WIISARD system excessively slowed the process of caring for and transporting patients off of the field. To time the transit of victims from the hot zone to transport for definitive care, we set up a secondary monitoring system based on the RFID technologies used to track runners in marathons and attached these markers to victims' shoes, manually recording the link between the victims' number on their jersey and the RFID tag at the time of assignment. Victims leaving the building would cross an RFID mat that recorded the initial time of entry onto the field. At each point in the MMRS field care system, victims crossed additional mats that recorded their time of entry into a particular area (decontamination, triage, treatment, and transport). When finally ready for transport, victims were loaded into an ambulance, crossing one last mat that recorded their time of exit from the field. The median time in the field was compared between victims cared for by the WIISARD pathway versus control pathway, excluding expectant victims.
One aspect of the WIISARD system that was not tested in a functional setting was the command center system. While we were able to set up a functional mirror command center staffed by WIISARD personnel, the actual incident command center operated outside of WIISARD and focused on the conducting drill operations and maintaining the safety of drill participants.
Statistical analyses were performed using Fisher exact testing of proportions and Mann–Whitney U for median time intervals (including IQR) with differences and 95% CIs reported where appropriate (SPSS 17.0).
Results
Networking system
The goal of a creating rapidly deployable, scalable, reliable, and high-bandwidth mesh network for data communications based on the WiFi protocol was only partially achieved. New network nodes could be brought rapidly on line, extending the range of the network, and the network distribution tree automatically reconfigured to utilize these nodes was demonstrated during the exercise. However, covering a large area with a high-quality signal required careful positioning of Calmesh units, because of interference from ground level objects such as fire trucks. Devices were occasionally out of contact for brief periods due to moving physical obstructions, electromagnetic interference, and movement of people carrying devices between nodes. Additionally, dynamic reconfiguration of the network when nodes were added to provide indoor networking coverage as first responders entered the building may have disrupted some communications.
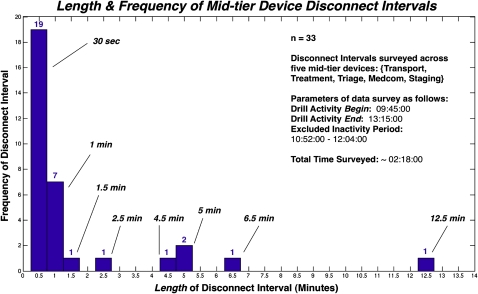
To examine the impacts of disruptions in communications, we tracked the periods of disconnection from the five tablet computers deployed in the exercise. By analyzing the connection logs of the tablet devices in the most recent drill, we built a simple disconnectivity profile for the WIISARD system. Figure 2 shows the 33 occurrences of disconnect periods that were 30 s or more. Several devices had long periods of disconnection. Work-flows were not interrupted because of caching and synchronization systems on each tablet, confirming the value of these systems. However, disconnections did create situations where confusion could have arisen due to different team leaders having different data on their tablets. This did not occur because the software provided feedback on when tablets were disconnected. In the event of disconnections, team leaders conferred with a colleague with an active connection either in person or by radio.
Figure 2.
Distribution of periods of disconnection of mid-tier devices (n=5) from the main Wireless Internet Information System for Medical Response in Disasters database.
Despite periodic network disconnections, the triage tags reliably relayed data across the network. Instructions for triage categories and transport instructions were received and displayed on the tags, and patient medical data were stored. Pulse oximetry data also were accurately relayed without any observed gaps. Pulse oximeters relayed the average heart rate and O2 saturation for 1 min periods, which minimized the impact of short disconnections. They were attached only to victims with immediate triage status in the treatment area. This area had excellent wireless network coverage.
Clinical care systems and data management
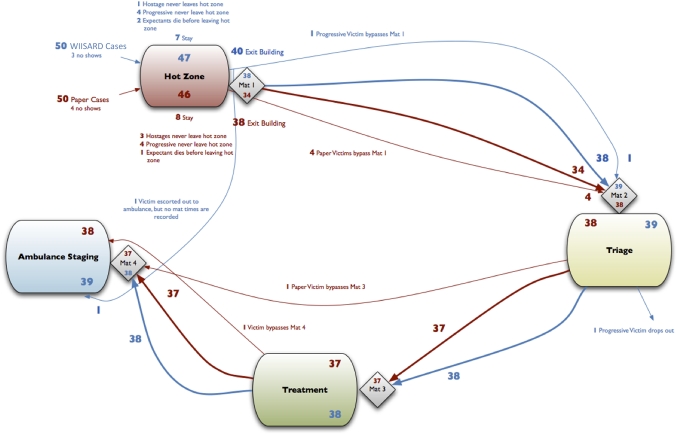
Figure 3 shows the progression of processing of victims by the two care systems. Three victims in the WIISARD group and four victims in the paper group terminated their participation before the exercise began. Additionally one patient in the WIISARD group and three patients in the control group were selected by first responders to become ‘hostages’ of the terrorists and were used in further role-play without regard to their assigned injuries. Other patients expired within the building based on their scenarios and did not enter the exercise field. As a result, the randomization became imbalanced. Thirty-eight of the victims (nine expectant) in the control group and 39 (three expectant) victims in the WIISARD group passed through their respective treatment systems
Figure 3.
Diagram showing how simulated victims actually passed through the Wireless Internet Information System for Medical Response in Disasters (WIISARD) and control treatment system.
Both systems accurately tracked the number of victims and their triage status. The WIISARD system was able to accurately maintain linkages between individual victims and their clinical data as shown in table 2. All 39 victims in the WIISARD group that entered field care had unique patient identifiers and had medical data recorded in the WIISARD electronic database. There were no ambiguous (shared) identifiers or duplicate identifiers. In the conventional pathway, lost tags, ambiguous identification numbers (numbers shared by more than one individual), duplicate identification numbers, and combinations of ambiguously labeled and doubly labeled identifiers (at different points in time) were common in the paper pathway, especially during periods with high victim flows. Overall, 18 of 38 (47%) records had database integrity problems that would have prevented linkage of clinical information with a patient identifier in the paper group. Seven of 38 victims in the control group were dispatched without medical record data from the field due to a lost or missing triage tag.
Table 2.
Victim-tracking accuracy of Wireless Internet Information System for Medical Response in Disasters and paper-based systems
| Wireless Internet Information System for Medical Response in Disasters (N=39) | Paper (N=38) | |
| Lost or missing triage tag | 0 | 7 |
| Non-unique victim identification number | 0 | 8 |
| Multiple identification numbers for same individual | 0 | 7 |
| Both non-unique and multiple identification number errors in the same individual | 0 | 5 |
In addition, more clinical information was captured in the WIISARD group: 73% of required fields were completed on average versus only 30%. Age and gender were almost always recorded in the WIISARD group but only infrequently recorded in the control group (95% vs 26% and 92% vs 24%, respectively). Decontamination status and field treatments were not recorded at all in the control group (0% for both items) but were often recorded in the WIISARD group (59% and 42%, respectively.) A more complete discussion of the impact of WIISARD on the quality of documentation can be found elsewhere.33
Analysis of videotapes revealed why the control system had difficulty maintaining linkages between patient identification numbers and their clinical data. Responders in the control group, when under time pressure, stopped using paper forms as intended, and recorded patient data margins and sometimes on scraps of paper. They subsequently transcribed information to proper forms during breaks in activity but often made errors. In addition, the Med-Com responder changed her work flow under time pressure and assigned patients to facilities based on their triage level, accurately tracking the numbers of patients in groups after significant efforts to reconcile data with other responder teams, but losing distinctions between individuals.
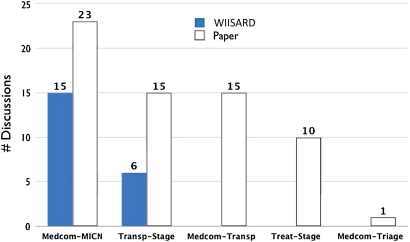
WIISARD appeared to improve first responders' situational awareness resulting in substantial reductions in the number of radio communications between groups to clarify critical issues (figure 4). Qualitative analyses showed that patients could be assigned to ambulances and to receiving hospitals without radio communications in the WIISARD group. Once the nurse coordinating hospital bed availability had mastered the use of WIISARD, there was no longer any need for radio communications with the Med-Com about hospital receiving capacity. When this happened, the role of the Med-Com team became redundant, and the mid-tier responders managing the treatment and transport areas, who had the greater familiarity with victims and their injuries, took over assignment to treating facilities.
Figure 4.
Counts of radio conversations between different first responder groups under Wireless Internet Information System for Medical Response in Disasters (WIISARD) and the control treatment system. MICN (Mobile Intensive Care Nurse); offsite coordinator who tracks available hospital beds at different facilities. Medcom; the team lead for all offsite communications. Transp; transportation area team lead who coordinates the loading of victims into ambulances. Staging; the team lead for the queuing area for ambulances. Treat; the team lead for the victim treatment area. Triage; the team lead for the victim triage area.
The use of a computer system to manage data did not appear to delay transport for definitive care. Among the immediate, delayed, or walking wounded victims processed, 36 WIISARD patients, and 29 control patients (the remainder in each group being expectant), the total time of the field was nearly identical (38:20 vs 38:23, IQR 26:53–1:05:32 vs (18:55–57:22). The times between various stations (triage, treatment, transport) were clinically similar for the two groups (table 3), and there were no statistically significant differences.
Table 3.
Transit times between care stations in Wireless Internet Information System for Medical Response in Disasters and Control groups
| Wireless Internet Information System for Medical Response in Disasters (median) | n | IQR (25–75) | Paper (median) | n | IQR (25–75) | |
| All victims with Mat times (excludes expectant) | ||||||
| Total time (Mat1–4) | 0:38:20 | 36 | (26:53–1:05:32) | 0:38:23 | 29 | (18:55–57:22) |
| Hot-triage (Mat1–2) | 0:04:08 | 36 | (2:15–6:15) | 0:05:26 | 30 | (2:18–6:19) |
| Triage-treatment (Mat2–3) | 0:07:24 | 37 | (0:50–11:54) | 0:04:56 | 33 | (0:51–11:45) |
| Treatment-ambulance (Mat3–4) | 0:30:46 | 37 | (11:37–49:52) | 0:30:12 | 32 | (4:42–40:16) |
| Immediates | ||||||
| Total time (Mat1–4) | 0:27:09 | 17 | (21:04–55:08) | 0:21:36 | 16 | (15:32–46:09) |
| Hot-triage (Mat1–2) | 0:06:16 | 17 | (4:04–12:44) | 0:05:01 | 17 | (4:19–8:18) |
| Triage-treatment (Mat2–3) | 0:03:40 | 18 | (0:39–10:31) | 0:00:55 | 19 | (0:34–9:40) |
| Treatment-ambulance (Mat3–4) | 0:12:55 | 18 | (9:16–36:50) | 0:07:37 | 18 | (3:31–31:22) |
| Delays | ||||||
| Total time (Mat1–4) | 0:39:20 | 9 | (29:51–44:57) | 0:37:19 | 7 | (34:00–58:22) |
| Hot-triage (Mat1–2) | 0:02:08 | 9 | (2:06–3:02) | 0:02:16 | 7 | (2:07–6:19) |
| Triage-treatment (Mat2–3) | 0:06:17 | 9 | (4:40–12:57) | 0:04:31 | 8 | (3:58–11:12) |
| Treatment-ambulance (Mat3–4) | 0:30:50 | 9 | (14:10–37:47) | 0:31:06 | 8 | (19:01–39:50) |
| Minor/WW | ||||||
| Total time (Mat1–4) | 1:06:16 | 10 | (52:59–1:08:01) | 0:58:04 | 6 | (54:39–58:29) |
| Hot-triage (Mat1–2) | 0:04:18 | 10 | (2:17–6:04) | 0:05:44 | 6 | (3:49–6:07) |
| Triage-treatment (Mat2–3) | 0:11:39 | 10 | (4:53–12:00) | 0:11:58 | 6 | (10:33–11:59) |
| Treatment-ambulance (Mat3–4) | 0:50:01 | 10 | (45:02–50:32) | 0:40:21 | 6 | (40:16–40:23) |
Command-center system
The command-center system was the least mature of WIISARD systems, and the results reflect a formative evaluation of this subsystem rather than a comparative one (as the true command center for the exercise operated outside of the scope of WIISARD). The system was able to grossly track the positions of first responders and of patients, but the accuracy of position fixes was limited to access-point association. Trilateration was not an effective tool to improve geolocation. Because of limits in geolocation capability, the system was not able to detect when patients or first responders moved into hazardous areas. Alerting functionalities were tested, and the command center was able to distribute text alerts through the system to ITTs, first-responder handhelds, and mid-tier tablets, as well as sending maps and other notices to tablets.
Discussion
As shown in table 1, at least 10 different systems have been developed that use technology to support mass casualty tracking and field care. These systems have remarkable similarities and notable differences. All systems share a networking component and data-capture tools for tracking, many systems have a personal sensor component, and most have tools for first responders to enter data and managers to view ongoing processes of care. All components need to work in an integrated system. While there is some standardization of work flows in emergency response in terms of triage methods and command structures,37 different response units have different procedures, and some custom tailoring of software and hardware systems is needed.
The WIISARD program illustrates the complexity of developing a comprehensive wireless mass-casualty tracking EHRs system for disaster care. Such systems are at least as complex as EMRs systems for healthcare settings. Multiple types of devices and operating systems were required to create a mass-casualty tracking and field-care system: electronic triage tags, wireless sensors, handheld computers for individual care, tablets for mobile supervisors of care, and command-center-style systems. While general-purpose mobile computers worked well for first-responder applications, systems for victims (electronic triage tags and sensors) appeared to require purpose-built devices. At a software level, the disaster response environment may require alternative software architectures designed for use in unreliable data-communication environments. Most prior systems had relied upon simple query and response methods with periodic updating. WIISARD results show that the use of publish/subscribe systems is feasible and illustrates how low-computation-power devices can be brought into a publish and subscribe network. Further research is needed to ascertain if query and response methods are adequate or whether ‘push’ strategies for information sharing are needed for scalability and resilience.
The WIISARD program had one of the most extensive evaluations of the 10 systems listed in table 1, with over 200 first responders and 100 simulated victims participating in the study and deployment of a full-scale working system. The results showed that it would be feasible to use a wireless medical records system to care for disaster victims, if network connectivity issues can be addressed. Replacing traditional paper-based record systems used in disaster care with an electronic one may improve data quality, affords opportunities for decision support, and does not significantly change the amount of time required for transport off the field. In fact, automated systems may scale better than paper-based methods. In the evaluation study, the time pressure appeared to disrupt the control system's tracking capability. The use of a computer to manage field care appeared to enforce a discipline on maintaining linkages between patient identification numbers and clinical data. Without this discipline linkages were lost between patients' identification numbers, their records of field care, and their receiving facility. The end result is the inability to know how many patients with specific types of injuries have been sent to each receiving hospital or even where specific patients were transported. This could result in overloading of a specific hospital with excessive numbers of patients with one type of injury (eg, multiple victims with head injuries) that would cause delays in definitive treatment. Loss of the linkage would likely make locating victims for family members more difficult. Loss of clinical data on triage tags could delay diagnosis or result in therapeutic errors. These types of errors have been seen in real-world mass-casualty events9 and other exercises.10 11
There appeared to be several other benefits. More data on patient status were collected with the WIISARD system. Some of these data may have immediate practical utility. Documentation of decontamination status of a victim, which was performed much more frequently in the WIISARD system, enhances the safety of providers and allows a patient to bypass decontamination at the treating hospital, thus accelerating definitive care. Collection of more data in the WIISARD system may have been due to Hawthorne-like effects. However, given that an electronic system such as WIISARD would allow supervisors to monitor the completeness of data entry for each patient and track first-tier responders' performance with regard to data recording in real time, it seems likely that any observed effects would translate to working systems.
A further benefit of the use of computer systems for field care is the potential to integrate decision-support tools. We were able to integrate a simple triage decision-support system in WIISARD. Data from the London bombings suggest that improved triage on the field may save lives.38 Handheld computers make it easier to provide decision support for triage; this may be important, as more complex algorithms for triage are introduced,39–41 and algorithms tailored to the types of events42 are developed. Decision support could be enhanced by access to patient records from Health Information Exchanges or through the Nationwide Health Information Network.
Finally, our results illustrate that disaster care systems can enhance workflow by distributing information across the response team, thereby enhancing situation awareness without causing information overflow. In our study, the WIISARD group had much less need for radio communications. There were fewer requests for information and fewer responses. In particular, the onscreen availability of data on hospital bed availability allowed the providers who were caring for victims to take over decision-making on the hospital destinations for those victims, potentially improving the process and freeing up valuable personnel resources.
Research on any one component of WIISARD might have been conducted with more limited resources than afforded by the Broad Area Announcement contract that supports the program. However, it would have been difficult to develop individual components of the system fully without testing a working system in a realistic environment or to understand the potential impact of the system on processes of care without a fully working model of WIISARD.
Technological evolution since the WIISARD evaluation
Overall, the results from WIISARD's program and its evaluation study suggest that deployment of wireless EHRs for MCI and disaster field care is feasible. Advances in technology in the time since completion of this project make such systems more practical. These include improved cellular networks (G4), inexpensive routers, smart phones, and electronic tablets that switch between cellular data and WiFi networks. There have also been significant advances in wireless sensor technology for patients who have expanded the range of sensors available and have lowered their costs.43 While currently designed for disease-management purposes, new wireless sensor technologies could be adapted to first responder use and could provide significant enhancements of field-care capabilities.
Summary
The WIISARD project illustrates how the principles underlying the use of EHRs can be applied to the care of victims of mass-casualty events and disasters. Systems that support mass-casualty tracking and field care have complex design requirements that rival those of EHRs. Networking and geolocation technologies were a challenge within WIISARD and require further development. Electronic triage tags appeared to be a practical technology that could have important secondary benefits such as being a repository for patient data. The software systems for field care developed in WIISARD appeared to improve the quality of information collected and enhance the dissemination of information across the response team. The use of WIISARD did not appear to increase the amount of time required to process patients through a model field-care system.
Acknowledgments
We express profound thanks to the firefighters, police, and other professionals of the San Diego Metropolitan Medical Response team who allowed us to work with them to evaluate WIISARD. We also thank the numerous other members of the WIISARD team not named in this publication but who played critical roles in development of systems, assembly of devices, preparation for exercises, and administration of the project. Finally, we would like to thank our advisory board for their invaluable advice and contributions to the project's direction and scope.
Footnotes
Funding: This work was supported by Award Number R01LM009522 from the National Library Of Medicine.
Competing interests: None.
Ethics approval: University of California, San Diego.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Frykberg ER. Terrorist bombings in Madrid. Crit Care 2005;9:20–2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lockey DJ, Mackenzie R, Redhead J, et al. London bombings July 2005: the immediate pre-hospital medical response. Resuscitation 2005;66:ix–xii [DOI] [PubMed] [Google Scholar]
- 3.Leitl E. Information technology issues during and after Katrina and usefulness of the Internet: how we mobilized and utilized digital communications systems. Crit Care 2005;10:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crabb C. Revisiting the Bhopal tragedy. Science 2004;306:1670–1 [DOI] [PubMed] [Google Scholar]
- 5.Okumura T, Suzuki K, Fukuda A, et al. The Tokyo subway sarin attack: disaster management, Part 1: community emergency response. Acad Emerg Med 1998;5:613–17 [DOI] [PubMed] [Google Scholar]
- 6.Mettler FA, Jr, Voelz GL. Major radiation exposure—what to expect and how to respond. N Engl J Med 2002;346:1554–61 [DOI] [PubMed] [Google Scholar]
- 7.Webb GF. Being prepared: modeling the response to an anthrax attack. Ann Intern Med 2005;142:667–8 [DOI] [PubMed] [Google Scholar]
- 8.Pate BL. Identifying and tracking disaster victims. Fam Community Health 2008;31:23–34 [DOI] [PubMed] [Google Scholar]
- 9.Johnson GA, Calkins A. Prehospital triage and communication. Performance in small mass casualty incidents: a gauge for disaster preparedness. Am J Emerg Med 1999;17:148–50 [DOI] [PubMed] [Google Scholar]
- 10.Hoskins JD, Graham RF, Robinson DR, et al. Mass casualty tracking with air traffic control methodologies. J Am Coll Surg 2009;2008:1001–8 [DOI] [PubMed] [Google Scholar]
- 11.Noordergraaf GJ, Bouman JH, Van Den Brink EJ, et al. Development of computer assisted patient control for use in the hospital mass casualty setting. Am J Emerg Med 1996;14:257–61 [DOI] [PubMed] [Google Scholar]
- 12.McGrath SP, Grigg E, Wendelk S, et al. ARTEMIS. Hanover, NH: Institute for Security, Technology and Society, 2004 [Google Scholar]
- 13.Morris TJ, Pajak J, Havlik F, et al. Battlefield Medical Information System-Tactical (BMIST): the application of mobile computing technologies to support health surveillance in the Department of Defense. Telemed J E Health 2006;12:409–16 [DOI] [PubMed] [Google Scholar]
- 14.Fry EA, Lenert L. MASCAL: RFID tracking of patients, staff, and equipment to enhance hospital response to mass casualty events. AMIA Annu Symp Proc 2005:261–5 [PMC free article] [PubMed] [Google Scholar]
- 15.Navy. http://www.namrl.navy.mil/clinical/projects/tacmedcs.htm
- 16.Raytheon. http://www.raytheon.com/products/epts/index.html
- 17.Jokela J, Simons T, Kuronen P, et al. Implementing RFID technology in a novel triage system during a simulated mass casualty situation. Int J Electron Healthc 2008;4:105–18 [DOI] [PubMed] [Google Scholar]
- 18.EMsystems http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.128.4959&rep=rep1&type=pdf (accessed 16 Jun 2011).
- 19.Zhao X, Rafiq A, Hummel R, et al. Integration of information technology, wireless networks, and personal digital assistants for triage and casualty. Telemed J E Health 2006;12:466–74 [DOI] [PubMed] [Google Scholar]
- 20.Tollefsen WW, Gaynor M, Pepe M, et al. iRevive: a prehospital database system for emergency medical services. Int J Healthc Technol Manage 2005;6:454–69 [Google Scholar]
- 21.Gao T, Massey T, Selavo L, et al. The advanced health and disaster aid network: a light-weight wireless medical system for triage. IEEE Trans Biomed Circuits Syst 2007;1:203–16 [DOI] [PubMed] [Google Scholar]
- 22.Lenert L, Palmer DA, Chan TC, et al. An intelligent 802.11 triage tag for medical response to disasters. AMIA Annu Symp Proc 2005:440–4 [PMC free article] [PubMed] [Google Scholar]
- 23.Arisylu M, Mishra R, Rao R, et al. Wireless infrastructure to enhance medical response to disasters. AMIA Annu Symp Proc 2005:1–5 [PMC free article] [PubMed] [Google Scholar]
- 24.Brauntein B, Trimble T, Mishra R, et al. Feasibility of using distributed wireless mesh networks for medical emergency response. AMIA Annu Symp Proc 2006:86–90 [PMC free article] [PubMed] [Google Scholar]
- 25.Brown SW, Griswold WG, Demchak B, et al., eds. Middleware for reliable mobile medical workflow support in disaster settings. Proceeding 2006 AMIA Fall Symposium. Washington, DC: American Medical Informatics Association, 2006:309–13 [PMC free article] [PubMed] [Google Scholar]
- 26.Buono C, Chan TC, Brown SW, et al. Role-tailored software systems for coordinating care at disaster sites: enhancing the capabilities of ‘mid-tier’ responders. AMIA Annu Symp Proc 2005:908. [PMC free article] [PubMed] [Google Scholar]
- 27.Demchak B, Griswold WG, Lenert LA. Data quality for situational awareness during mass-casualty events. AMIA Annu Symp Proc 2006:176–80 [PMC free article] [PubMed] [Google Scholar]
- 28.Kirsh D, Dabrowski D, Lenert L. Evaluation wireless medical technology for disaster response. AMIA Annu Symp Proc 2006 [Google Scholar]
- 29.Lorincz K, Malan DJ, Fulford-Jones TRF, et al. Sensor networks for emergency response: challenges and opportunities. Pervasive Computing, IEEE 2004;3:16–23 [Google Scholar]
- 30.Curtis DW, Pino EJ, Bailey JM, et al. SMART—an integrated wireless system for monitoring unattended patients. J Am Med Inform Assoc 2008;15:44–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flowers LK, Mothershead JL, Blackwell TH. Bioterrorism preparedness. II: The community and emergency medical services systems. Emerg Med Clin North Am 2002;20:457–76 [DOI] [PubMed] [Google Scholar]
- 32.Cone DC, MacMillan DS. Mass casualty triage systems: a hit of science. Acad Emerg Med 2005;12:740–1 [DOI] [PubMed] [Google Scholar]
- 33.Frykberg ER. Principles of mass casualty management following terrorist disasters. Ann Surg 2004;239:319–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Killeen JP, Chan TC, Buono C, et al., eds. A wireless first responder handheld device for rapid triage, patient assessment and documentation during mass casualty events. Proceedings 2006 AMIA Fall Symposium. Washington, DC: American Medical Informatics Association, 2006:429–33 [PMC free article] [PubMed] [Google Scholar]
- 35.Buono C, Chan TC, Killeen J, et al. Role tailored software systems for coordinating care at disaster sites: enhancing collaboration between base hospitals and the field. AMIA Annu Symp Proc 2006:867. [PMC free article] [PubMed] [Google Scholar]
- 36.Calvitti A, Lenert L, eds. A dynamic model of alert and alarm management in clinical medicine and disaster response. Proceedings of the 2006 AMIA Fall Symposium. Washington, DC: American Medical Informatics Association, 2006 [Google Scholar]
- 37.O'Neill PA. The ABC's of disaster response. Scand J Surg 2005;94:259–66 [DOI] [PubMed] [Google Scholar]
- 38.Aylwin CJ, Konig TC, Brennan NW, et al. Reduction in critical mortality in urban mass casualty incidents: analysis of triage, surge, and resource use after the London bombings on July 7, 2005. Lancet 2006;368:2219–25 [DOI] [PubMed] [Google Scholar]
- 39.Cone DC, Serra J, Burns K, et al. Pilot test of the SALT mass casualty triage system. Prehosp Emerg Care 2009;13:536–40 [DOI] [PubMed] [Google Scholar]
- 40.Jenkins JL, McCarthy ML, Sauer LM, et al. Mass-casualty triage: time for an evidence-based approach. Prehosp Disaster Med 2008;23:3–8 [DOI] [PubMed] [Google Scholar]
- 41.Lerner EB, Schwartz RB, Coule PL, et al. Mass casualty triage: an evaluation of the data and development of a proposed national guideline. Disaster Med Public Health Prep 2008;2(Suppl 1):S25–34 [DOI] [PubMed] [Google Scholar]
- 42.Cone DC, MacMillan DS, Parwani V, et al. Pilot test of a proposed chemical/biological/radiation/ nuclear-capable mass casualty triage system. Prehosp Emerg Care 2008;12:236–40 [DOI] [PubMed] [Google Scholar]
- 43.Topol E. Transforming medicine via digital innovation. Sci Transl Med 2010;2:16cm4. [DOI] [PMC free article] [PubMed] [Google Scholar]