Abstract
Background
Atrial fibrillation (AF) is the most common cardiac arrhythmia. Magnesium has been reported to be effective in reducing the incidence or prophylaxis of AF. Magnesium is also an essential constituent of many enzyme systems and plays a physiological role in coagulation regulation. The aim of the present study was to examine the effects of magnesium, whether magnesium infusion might decrease the incidence of AF and induce hypocoagulable state in patients with AF, who were undergoing mitral valve annuloplasty.
Methods
This prospective laboratory study was performed using blood from patients with AF undergoing mitral valve annuloplasty. The radial artery was punctured with a 20 gauge catheter and used for monitoring continuous arterial pressure and blood sampling. After anesthesia induction, 4 g of magnesium was mixed with 100 ml normal saline and infused for 5 minutes. Magnesium, calcium, activated clotting time (ACT) and thromboelastographic parameters were checked before and 60 minutes after the magnesium infusion. The electrocardiography changes after magnesium infusion were also checked before commencing cardiopulmonary bypass.
Results
After magnesium infusion, the serum level of magnesium increased significantly but serum calcium did not change significantly. ACT did not change significantly before or after magnesium infusion. The thromboelastographic parameters showed no significant changes before or after magnesium infusion. None of the patients converted to sinus rhythm from AF after the magnesium infusion.
Conclusions
A magnesium infusion did not influence the course of AF and coagulation in patients during prebypass period with AF undergoing mitral valve annuloplasty.
Keywords: Atrial fibrillation, Magnesium, Mitral valve annuloplasty, Thromboelastography
Introduction
Atrial fibrillation (AF) is the most common cardiac arrhythmia. The association between AF and the risk of thromboembolic complications has long been recognized. The pathogenesis of thromboembolic complications is multifactorial but may be attributed to a hypercoagulable state with hemostatic abnormalities and endothelial dysfunction in AF [1].
Several meta-analyses showed that intravenous magnesium is effective for decreasing the incidence or prophylaxis of AF [2-4]. Miller et al. [2] reported the effectiveness of magnesium on post-cardiac surgeries AF. Onalan et al. [3] reported effectiveness of magnesium on rapid AF in patients without surgeries. Ho et al. [4] that magnesium could be considered as a safe adjunct to digoxin in controlling the ventricular response in acute AF. Magnesium is also an essential constituent of many enzyme systems and plays a physiological role in the regulation of coagulation. Magnesium is thought to prevent the coagulation process but the effects of magnesium on coagulation, as evaluated by thromboelastography, are inconsistent. In situation of rapid intravenous fluid infusion, maintaining magnesium at the upper limit of normal value attenuates rapid hemodilution-induced coagulation change (clot formation rate prolongation) due to decreased magnesium level in healthy volunteers [5]. Magnesium significantly improves the hypocoagulable state toward normal in patients undergoing liver transplantation [6]. However, James and Neil [7] reported that magnesium has minimal effects on coagulation (small prolongation of r time and k time and r + k time at thromboelastography) and Ames et al. [8] reported that magnesium levels remained unchanged except for an increase of the α angle at thromboelastography in healthy volunteers. Additionally, there was one report that magnesium has no effect on the overall coagulation index in women with pre-eclampsia [9]. On the other hand, there were some investigations that magnesium interrupted platelet aggregation and adhesion so magnesium sulphate administration induced hypocoagulation state in vitro and in vivo studies [10,11].
We hypothesized that magnesium infusion might decrease the incidence of AF and induce platelet dysfunction and induce hypocoagulable state because it can affect platelet function and it is essential factor for coagulation. The aim of the present study was to determine the effects of magnesium to the course of AF and coagulation status in mitral valve disease patients with AF.
Materials and Methods
Study population
This prospective laboratory study was performed using blood from patients with AF undergoing mitral valve annuloplasty after obtaining institutional review board approval and informed consent from the patients. Patients were excluded if any of the following criteria were present: 1) urgent or emergent case, 2) reduced left ventricular function (ejection fraction < 40%), 3) significant concomitant other valvular heart disease, 4) intra-cardiac shunt, 5) myocardial infarction or clinical angina for 14 days, 6) severe renal disease (serum creatinine > 2.0 mg/dl) or 7) severe hepatic disease.
Anesthetic regimen
After establishing routine invasive (invasive radial arterial blood pressure) and non-invasive patient monitoring (pulse oximetry, electrocardiography, bispectral index and near infrared spectroscopy), anesthesia was induced and maintained using target-controlled infusion (Orchestra®Base Primea, Fresenius Vial, Brezins, France) of propofol (target concentration, 1.0-1.5 µg/ml) and remifentanil (target concentration, 10-20 ng/ml). Muscle relaxation was obtained with a bolus of rocuronium under the guidance of peripheral neuromuscular transmission monitoring. Tracheal intubation and central venous catheterization on an internal jugular vein were performed, and a transesophageal echocardiography probe (6T probe, GE Healthcare, Piscataway, NJ, USA) was inserted.
Definition of AF and disappearance of AF
AF was defined as an irregular narrow complex rhythm (in the absence of a bundle branch block) with absence of discrete P waves for at least 10 minutes in the general ward and upon arrival at the operating room [12]. The disappearance of AF was defined as at least 10 minutes of sustained sinus rhythm after magnesium infusion. Changes in electrocardiography after the magnesium infusion were checked before commencing cardiopulmonary bypass.
Blood sample and thromboelastography (ROTEM®, Pentapharm GmbH, München, Germany)
The radial artery was punctured with a 20 gauge catheter after a modified Allen's test and an arterial tubing Luerlock connector was secured to the intra-arterial catheter. The pressure-tubing-transducer system was flushed with heparinized saline (heparin 5,000 U mixed in 1,000 ml normal saline). A blood sample was obtained after 10 ml of blood and heparinized saline were discarded from the radial artery. A 1 ml arterial blood sample was obtained and arterial blood gas analysis for measuring magnesium and calcium was performed. A 2.5 ml arterial blood sample was obtained and activated clotting time (ACT) was measured by Hemochron Response® (ITC, Edison, NJ, USA) with celite activator. A 1 ml blood sample was obtained and collected in a tube containing sodium citrate (Vacuette®, Greiner Bio-One GmbH, Kremsmünster, Austria) thromboelastography. Before sample analysis, the thromboelstography instrument was calibrated and underwent daily quality control testing. Samples were collected and analysed simultaneously at 37℃ on a four-channel thromboelstography machine with HepTEM® (Pentapharm GmbH, München, Germany). All reagents were purchased from Pentapharm. Just after induction of anesthesia, magnesium, calcium, ACT and the thromboelstographic parameters were measured as baseline values.
Magnesium (4 g mixed in 100 ml normal saline) was infused for 5 minutes before anesthesia induction. After 60 minutes of magnesium infusion, magnesium, calcium, ACT and the thromboelstographic parameters were measured.
Thromboelstographic parameters
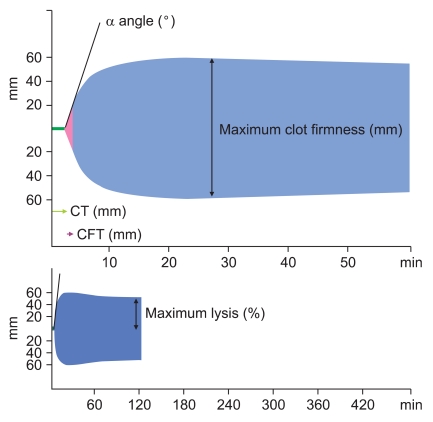
Clotting time (CT), clot formation time (CFT), α angle, maximum clot firmness (MCF) and maximum lysis (ML) were measured.
CT was the time until the initiation of clotting. CFT was the time from the initiation of clotting until the clot reached 20 mm, which represented the speed of clot formation. The α angle was the tangent of the curve made as 20 mm of firmness was reached and describes the kinetics of clot formation. MCF described the maximum amplitude of thromboelastogram and reflected clot strength. ML was the reduction in clot firmness in relation to MCF and represented maximum fibrinolysis detected during analysis (Fig. 1).
Fig. 1.
Rotational thromboelastometry parameters. clotting time (CT), clot formation time (CFT), α angle, maximum clot firmness (MCF) and maximum lysis (ML).
Statistics
The primary outcome variables were the thromboelstographic parameters. Reference values, from a pilot study of 10 patients with AF undergoing mitral valve annuloplasty, were: CT, 172 ± 18 seconds; CFT, 81 ± 16 seconds; α angle, 75 ± 3°; MCF, 60 ± 5 mm; ML, 18 ± 3%. A difference of 10% or more detected between baseline and after magnesium infusion was deemed clinically significant. For a power of 0.8 and an α value of 0.05, sample sizes of 11, 35, 4, 9 and 23 for CT, CFT, α angle, MCF and ML, respectively, were calculated to be appropriate.
The data were analysed using the Statistical Package for the Social Sciences (SPSS for Windows, ver. 12.0; SPSS Inc, Chicago, IL, USA). Changes in magnesium, calcium, ACT, CT, CFT, α angle, MCF and ML were compared between baseline and after magnesium infusion value using a paired t-test. All data are expressed as number of patients or the mean ± SD. A P < 0.05 was deemed to be statistically significant.
Results
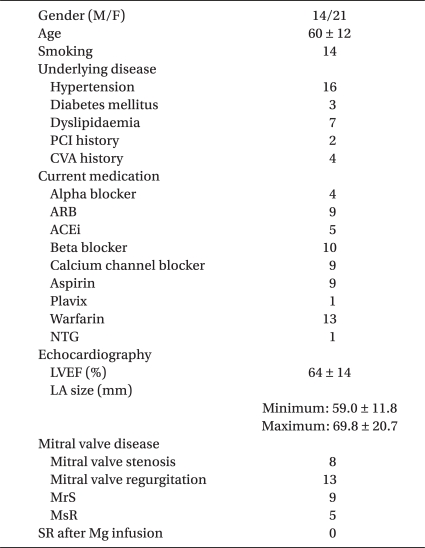
Thirty-nine patients with AF undergoing mitral valve annuloplasty were studied but four patients were excluded because of simultaneous tricuspid valve annuloplasty. Thus, 35 patients were included in the final analysis (Table 1).
Table 1.
Patient Characteristics
Data are expressed as numbers of patients or mean ± SD. PCI: percutaneous coronary intervention, CVA: cerebrovascular accident, ARB: angiotensin receptor blocker, ACEi: angiotensin converting enzyme inhibitor, NTG: nitroglycerin, LVEF: left ventricular ejection LA: left atrium, MrS: combined mitral stenosis and regurgitation but mainly stenosis, MsR: combined mitral stenosis and regurgitation but mainly regurgitation, SR after Mg infusion: sinus rhythm after magnesium infusion.
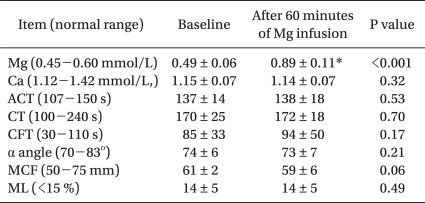
After magnesium infusion, serum levels of magnesium increased significantly (0.46 ± 0.06 mmol/L vs. 0.89 ± 0.11 mmol/L; P < 0.001) but the serum calcium level did not change significantly (1.15 ± 0.06 mmol/L vs. 1.14 ± 0.07 mmol/L; P = 0.32) (Table 2). ACT did not change significantly before or after the magnesium infusion (137 ± 14 seconds vs. 138 ± 18 seconds; P = 0.53) (Table 2).
Table 2.
Effects of Magnesium on Rotational Thromboelastometry with HepTEM®
Data are expressed as mean ± SD. Mg: magnesium, Ca: calcium, ACT: activated clotting time, CT: clotting time, CFT: clot formation time, MCF: maximum clot firmness, ML: maximum lysis. *P < 0.05.
The thromboelstography parameters did not change significantly before or after the magnesium infusion: CT, 170 ± 24 seconds vs. 172 ± 18 seconds (P = 0.70); CFT, 85 ± 33 seconds vs. 94 ± 50 seconds (P = 0.17); α angle, 74 ± 6° vs. 73 ± 7° (P = 0.21); MCF, 61 ± 6 mm vs. 59 ± 6 mm (P = 0.06); ML, 14 ± 5% vs. 14 ± 5% (P = 0.49) (Table 2).
None of the patients converted to sinus rhythm from AF after the magnesium infusion.
Discussion
Wang et al. [13] reported that the maintenance of low LA wall tension and near normal size of LA was important factors to maintain normal sinus rhythm after mitral or tricuspid valve surgeries and Maze procedure. Wachtell et al. [14] also reported that LA size is strong predictor to the development of AF. Mitral valvular heart disease, increased left atrial pressure and volume overload, which lead to left atrial enlargement (LAE), is frequently associated with AF. The incidence of AF is known as 30-40% in patients presenting mitral valve surgery [15]. Most studies about correlation between prophylactic magnesium and the incidence of AF have focused on coronary artery bypass grafting surgery (CABG) with cardiopulmonary bypass in cardiac surgeries [2,16]. A meta-analysis by Miller et al. [2] included, in the main, patients undergoing CABG (only CABG, 1794 patients; CABG and valve surgery, 523 patients; only valve surgery, 70 patients) and did not fully clarify valve surgery, especially only mitral valve surgery. Therefore, the present study focused on mitral valve disease patients with AF before surgical correction.
The patients with AF, who were undergoing mitral valve annuloplasty, frequently underwent concomitant maze procedure and received postoperative amiodarone for AF. Preoperative magnesium infusion was more effective in prevention of postoperative AF, comparing with intra- or postoperative magnesium infusion in a meta-analysis by Miller et al. [2] and postoperative AF usually has a self limited course [17,18]. Therefore, pre- and intra-operative AF was focused in the present study.
Hypomagnesemia is a common disorder after cardiac surgeries and has a higher frequency in patients with AF [2,19]. Therefore, a magnesium infusion is highly effective prophylactic therapy for reducing the incidence of AF after cardiac surgery [2,16]. The mechanism of prevention of AF by magnesium infusion is not entirely known, but depletion of magnesium is associated with proarrhythmic and magnesium infusion significantly increases atrial refractoriness [20,21]. DiCarlo et al. [22] showed magnesium infusion increased refractoriness in 10 patients with normal range of magnesium. We had performed pilot study before the present study and had got the results, showing 20% reduction of AF with changing from lower normal limit of magnesium to upper limit. Therefore, we thought that magnesium infusion could decrease the incidence of AF with normal range of magnesium in patients with AF undergoing mitral valve annuloplasty.
As mentioned above, AF in mitral valvular heart disease is a structural problem of left atrial size and an effort to decrease the occurrences of AF with prophylactic magnesium infusion might have the limitations without a reduction in left atrial size. Preoperative echocardiography also showed LAE (59.0 ± 11.8-69.8 ± 20.7 mm) in the present study. As the results of structural changes of left atrium (LA) with AF, blood stasis on LA easily occurs and contributes to thrombus formation in LA in mitral valvular heart disease with AF. Black et al. [23] reported that a left atrial spontaneous echo contrast in AF, representing a hypercoagulable state, is related to left atrial dimensions, increased hematocrit and fibrinogen but is not related to platelet count and coagulation factor. This result indicates that AF coagulant properties are related to the interaction between the structural problem and hematologic change, and magnesium infusion might fail to change the coagulant properties.
The total dosage of magnesium has also been considered. Several studies investigating the effect of magnesium on the incidence of AF used from 2 to 25 g for from 30 minutes to 96 hours [2-4], although Abraham et al. [24] reported that a single dose of 2.4 g magnesium sulphate is effective and the lower limit of normal serum magnesium before magnesium infusion changed into a higher limit after the magnesium infusion in the present study.
Magnesium is well known as a calcium (it was known as an essential ion for coagulation) antagonist and is believed to have anticoagulant effects. Magnesium induces a significant prolongation of bleeding time, mediated neither by changes in platelet count or aggregation pattern nor by changing the level or ratios of serum arachidonic acid metabolites in preeclampsia [25]. In contrast, magnesium is a crucial constituent of coagulation. It activates platelet aggregation in healthy volunteers [26] and all processes related to factor XI [27], and promotes coagulation. These different effects on coagulation suggest that magnesium may have different actions under various circumstances. The effect of magnesium on coagulation, evaluated by thromboelastography, also shows variable results according to coagulation state and pregnancy [5-9].
Lip et al. [28] reported that plasma levels of fibrinogen, fibrin D-dimer and vWF are increased in patients with chronic AF, comparing with sinus rhythm. These factors are predictive of cardiovascular events hence may be markers of prothrombin state in patients with AF. Li-Saw-Hee et al. [29] reported that there was no significant variation in indexes of thrombogensis, platelet activation and endothelial dysfunction between LA and peripheral artery or vein. Therefore, we thought that the thromboelastographic parameters at baseline in the present study would show hypercoagulabe state but it showed normal ranges. Because antiplatelet and anticoagulation medications made weakness of clot strength or induced prolongation of initiation of clotting in thromboelastography results [30], medications such as aspirin, plavix and warfarin in patients with AF might be associated with normal ranges for the thromboelastographic parameters. If these medications were not used to the patients in this study, the possibility seemed to tend to the hypercoagulation by thromboelastography parameters. However, according to the results of our study, the change of coagulation profile might not be significant. Further investigation for the effects of magnesium on coagulation of the patients without antiplatelet or anticoagulation medication would help to support the present study.
One limitation should be considered. The sample size of the present study was calculated from thromboelastographic parameters in the pilot study. If the sample sizes were calculated from reduction rate of AF, 108 for 10%, 42 for 5% and 30 for 3%, respectively were obtained. However, the sample sizes from meta-analysis by Ho et al. [4] were various (15, 18, 20, 34, 35 and so on) and the sample size of 35 patients in the present study was not thought to be insufficient.
In conclusion, magnesium infusion did not influence the course of AF or coagulation during prebypass period in mitral valve disease patients with AF undergoing mitral valve annuloplasty.
Footnotes
The English in this document has been checked by at least two professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/PecI59
References
- 1.Lip GY. Does atrial fibrillation confer a hypercoagulable state? Lancet. 1995;346:1313–1314. doi: 10.1016/s0140-6736(95)92339-x. [DOI] [PubMed] [Google Scholar]
- 2.Miller S, Crystal E, Garfinkle M, Lau C, Lashevsky I, Connolly SJ. Effects of magnesium on atrial fibrillation after cardiac surgery: a meta-analysis. Heart. 2005;91:618–623. doi: 10.1136/hrt.2004.033811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onalan O, Crystal E, Daoulah A, Lau C, Crystal A, Lashevsky I. Meta-analysis of magnesium therapy for the acute management of rapid atrial fibrillation. Am J Cardiol. 2007;99:1726–1732. doi: 10.1016/j.amjcard.2007.01.057. [DOI] [PubMed] [Google Scholar]
- 4.Ho KM, Sheridan DJ, Paterson T. Use of intravenous magnesium to treat acute onset atrial fibrillation: a meta-analysis. Heart. 2007;93:1433–1440. doi: 10.1136/hrt.2006.111492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruttmann TG, Montoya-Pelaez LF, James MF. The coagulation changes induced by rapid in vivo crystalloid infusion are attenuated when magnesium is kept at the upper limit of normal. Anesth Analg. 2007;104:1475–1480. doi: 10.1213/01.ane.0000261256.88414.e4. [DOI] [PubMed] [Google Scholar]
- 6.Choi JH, Lee J, Park CM. Magnesium therapy improves thromboelastographic findings before liver transplantation: a preliminary study. Can J Anaesth. 2005;52:156–159. doi: 10.1007/BF03027721. [DOI] [PubMed] [Google Scholar]
- 7.James MF, Neil G. Effect of magnesium on coagulation as measured by thrombelastography. Br J Anaesth. 1995;74:92–94. doi: 10.1093/bja/74.1.92. [DOI] [PubMed] [Google Scholar]
- 8.Ames WA, McDonnell N, Potter D. The effect of ionised magnesium on coagulation using thromboelastography. Anaesthesia. 1999;54:999–1001. doi: 10.1046/j.1365-2044.1999.00647.x. [DOI] [PubMed] [Google Scholar]
- 9.Harnett MJ, Datta S, Bhavani-Shankar K. The effect of magnesium on coagulation in parturients with preeclampsia. Anesth Analg. 2001;92:1257–1260. doi: 10.1097/00000539-200105000-00033. [DOI] [PubMed] [Google Scholar]
- 10.Gries A, Bode C, Gross S, Peter K, Bohrer H, Martin E. The effect of intravenously administered magnesium on platelet function in patients after cardiac surgery. Anesth Analg. 1999;88:1213–1219. doi: 10.1097/00000539-199906000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Gawaz M, Ott I, Reininger AJ, Neumann FJ. Effects of magnesium on platelet aggregation and adhesion. Magnesium modulates surface expression of glycoproteins on platelets in vitro and ex vivo. Thromb Haemost. 1994;72:912–918. [PubMed] [Google Scholar]
- 12.Toraman F, Karabulut EH, Alhan HC, Dagdelen S, Tarcan S. Magnesium infusion dramatically decreases the incidence of atrial fibrillation after coronary artery bypass grafting. Ann Thorac Surg. 2001;72:1256–1261. doi: 10.1016/s0003-4975(01)02898-3. [DOI] [PubMed] [Google Scholar]
- 13.Wang W, Buehler D, Martland AM, Feng XD, Wang YJ. Left atrial wall tension directly affects the restoration of sinus rhythm after Maze procedure. Eur J Cardiothorac Surg. 2011;40:77–82. doi: 10.1016/j.ejcts.2010.10.022. [DOI] [PubMed] [Google Scholar]
- 14.Wachtell K, Gerdts E, Aurigemma GP, Boman K, Dahlof B, Nieminen MS, et al. In-treatment reduced left atrial diameter during antihypertensive treatment is associated with reduced new-onset atrial fibrillation in hypertensive patients with left ventricular hypertrophy: The LIFE Study. Blood Press. 2010;19:169–175. doi: 10.3109/08037051.2010.481811. [DOI] [PubMed] [Google Scholar]
- 15.Jovin A, Oprea DA, Jovin IS, Hashim SW, Clancy JF. Atrial fibrillation and mitral valve repair. Pacing Clin Electrophysiol. 2008;31:1057–1063. doi: 10.1111/j.1540-8159.2008.01135.x. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan M, Kut MS, Icer UA, Demirtas MM. Intravenous magnesium sulfate prophylaxis for atrial fibrillation after coronary artery bypass surgery. J Thorac Cardiovasc Surg. 2003;125:344–352. doi: 10.1067/mtc.2003.108. [DOI] [PubMed] [Google Scholar]
- 17.Maisel WH, Rawn JD, Stevenson WG. Atrial fibrillation after cardiac surgery. Ann Intern Med. 2001;135:1061–1073. doi: 10.7326/0003-4819-135-12-200112180-00010. [DOI] [PubMed] [Google Scholar]
- 18.Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–1729. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 19.Aglio LS, Stanford GG, Maddi R, Boyd JL, 3rd, Nussbaum S, Chernow B. Hypomagnesemia is common following cardiac surgery. J Cardiothorac Vasc Anesth. 1991;5:201–208. doi: 10.1016/1053-0770(91)90274-w. [DOI] [PubMed] [Google Scholar]
- 20.Roden DM, Iansmith DH. Effects of low potassium or magnesium concentrations on isolated cardiac tissue. Am J Med. 1987;82:18–23. doi: 10.1016/0002-9343(87)90128-8. [DOI] [PubMed] [Google Scholar]
- 21.Rasmussen HS, Thomsen PE. The electrophysiological effects of intravenous magnesium on human sinus node, atrioventricular node, atrium, and ventricle. Clin Cardiol. 1989;12:85–90. doi: 10.1002/clc.4960120204. [DOI] [PubMed] [Google Scholar]
- 22.DiCarlo LA, Jr, Morady F, de Buitleir M, Krol RB, Schurig L, Annesley TM. Effects of magnesium sulfate on cardiac conduction and refractoriness in humans. J Am Coll Cardiol. 1986;7:1356–1362. doi: 10.1016/s0735-1097(86)80157-7. [DOI] [PubMed] [Google Scholar]
- 23.Black IW, Chesterman CN, Hopkins AP, Lee LC, Chong BH, Walsh WF. Hematologic correlates of left atrial spontaneous echo contrast and thromboembolism in nonvalvular atrial fibrillation. J Am Coll Cardiol. 1993;21:451–457. doi: 10.1016/0735-1097(93)90688-w. [DOI] [PubMed] [Google Scholar]
- 24.Abraham AS, Rosenmann D, Kramer M, Balkin J, Zion MM, Farbstien H, et al. Magnesium in the prevention of lethal arrhythmias in acute myocardial infarction. Arch Intern Med. 1987;147:753–755. [PubMed] [Google Scholar]
- 25.Assaley J, Baron JM, Cibils LA. Effects of magnesium sulfate infusion upon clotting parameters in patients with pre-eclampsia. J Perinat Med. 1998;26:115–119. doi: 10.1515/jpme.1998.26.2.115. [DOI] [PubMed] [Google Scholar]
- 26.Serebruany VL, Herzog WR, Schlossberg ML, Gurbel PA. Bolus magnesium infusion in humans is associated with predominantly unfavourable changes in platelet aggregation and certain haemostatic factors. Pharmacol Res. 1997;36:17–22. doi: 10.1006/phrs.1997.0212. [DOI] [PubMed] [Google Scholar]
- 27.Sekiya F, Yoshida M, Yamashita T, Morita T. Magnesium (II) is a crucial constituent of the blood coagulation cascade. Potentiation of coagulant activities of factor IX by Mg2+ ions. J Biol Chem. 1996;271:8541–8544. doi: 10.1074/jbc.271.15.8541. [DOI] [PubMed] [Google Scholar]
- 28.Lip GY, Lowe GD, Rumley A, Dunn FG. Increased markers of thrombogenesis in chronic atrial fibrillation: effects of warfarin treatment. Br Heart J. 1995;73:527–533. doi: 10.1136/hrt.73.6.527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li-Saw-Hee FL, Blann AD, Goldsmith I, Lip GY. Indexes of hypercoagulability measured in peripheral blood reflect levels in intracardiac blood in patients with atrial fibrillation secondary to mitral stenosis. Am J Cardiol. 1999;83:1206–1209. doi: 10.1016/s0002-9149(99)00060-0. [DOI] [PubMed] [Google Scholar]
- 30.Swallow RA, Agarwala RA, Dawkins KD, Curzen NP. Thromboelastography: potential bedside tool to assess the effects of antiplatelet therapy? Platelets. 2006;17:385–392. doi: 10.1080/09537100600757521. [DOI] [PubMed] [Google Scholar]