Abstract
Background:
Decisions about CPR in the medical ICU (MICU) are important. However, discussions about CPR (code status discussions) can be challenging and may be incomplete if they do not address goals of care.
Methods:
We interviewed 100 patients, or their surrogates, and their physicians in an MICU. We queried the patients/surrogates on their knowledge of CPR, code status preferences, and goals of care; we queried MICU physicians about goals of care and treatment plans. Medical records were reviewed for clinical information and code status orders.
Results:
Fifty patients/surrogates recalled discussing CPR preferences with a physician, and 51 recalled discussing goals of care. Eighty-three patients/surrogates preferred full code status, but only four could identify the three main components of in-hospital CPR (defibrillation, chest compressions, intubation). There were 16 discrepancies between code status preferences expressed during the interview and code status orders in the medical record. Respondents’ average prediction of survival following in-hospital cardiac arrest with CPR was 71.8%, and the higher the prediction of survival, the greater the frequency of preference for full code status (P = .012). Of six possible goals of care, approximately five were affirmed by each patient/surrogate and physician, but 67.7% of patients/surrogates differed with their physicians about the most important goal of care.
Conclusions:
Patients in the MICU and their surrogates have inadequate knowledge about in-hospital CPR and its likelihood of success, patients’ code status preferences may not always be reflected in code status orders, and assessments may differ between patients/surrogates and physicians about what goal of care is most important.
Code status orders refer to decisions to perform or not perform CPR in the event of cardiopulmonary arrest. In making decisions about code status orders it is essential that physicians and patients communicate effectively so that patients can receive informed, compassionate care that respects their treatment preferences. However, communication between physicians and patients (or their surrogates) about code status orders is difficult,1 and misunderstandings about code status preferences may lead to unwanted medical interventions2,3 or withholding of desired interventions. The need for effective and respectful communication about resuscitation preferences is heightened in the setting of the ICU where the pace of decision making is often rapid, the burdens of medical technology are typically significant, diagnoses and prognoses may be uncertain,4 surrogate decision making is common,5 and the threat of death or disability understandably causes fear and anxiety. These conditions make clear communication in the ICU both challenging and necessary.6
In light of these communication challenges, authors have increasingly emphasized the importance of goals of care in discussions about medical interventions, especially toward the end of life.1,7‐11 Goals of care are also significant in the ICU, where there is particular interest in guiding, when appropriate, the transition from the goal of cure to the goal of palliation.6 Goals of care are important because they provide a basic orientation for decision making and can guard against tendencies to isolate interventions from the larger clinical realities that surround them.12
We are not aware of prior studies that have deliberately queried patients in the ICU about their preferences regarding goals of care. However, there is empirical evidence from a general medical setting that most patients find it helpful to discuss goals of care,13 and a recent structured literature review has identified six goals of care that summarize the range of goals that are commonly mentioned in the literature.11 Less is known about how the discussion of goals may influence code status orders, although it is believed that the accuracy of code status decisions may be compromised when physicians and patients have differing goals of care in mind14,15 or when patients have an inadequate understanding of outcome probabilities.16‐19
To improve our understanding of code status orders and goals of care in the ICU setting, we interviewed adult patients (or their surrogates) in a medical ICU (MICU) to: (1) assess the concordance between patients’ code status preferences and their actual code status orders, (2) assess patients’/surrogates’ understanding of outcome probabilities after in-hospital cardiac arrest and CPR, (3) describe patients’ goals of care during their hospitalization, and (4) compare patients/surrogates and their physicians regarding their respective assessments of most important goals of care.
Materials and Methods
Setting and Participants
We interviewed adult patients (or their legally authorized surrogate decision makers) who were in the MICU of a large Midwestern academic medical center between December 2008 and December 2009. We then interviewed the MICU physicians (faculty or postgraduate fellows) caring for each patient on the same or (occasionally) next day.
Enrollment, Informed Consent, and Interviews
After Institutional Review Board approval (University of Iowa IRB-01 Biomedical, study # 200809732), a physician-investigator (T. G. G.), who is a pulmonary and critical care postgraduate fellow, enrolled subjects, obtained informed consent, and conducted interviews. For patients lacking ability to provide consent, a legally authorized surrogate was invited to provide consent and serve as the interviewee. Patients were excluded for any of the following criteria: (1) unable to speak English or incapacitated without an available English-speaking surrogate; (2) imprisoned; (3) admitted after attempted suicide or for pharmacologic desensitization; (4) hospitalized in the MICU for less than 48 h; or (5) unavailable for interview on a weekday.
A randomized list of potential participants was created each day of the study using a random sequence generator to order the 26 beds in the MICU; the interviewer then approached as many patients/surrogates as possible on a given day following the order of listed bed numbers generated from that day. Patients were not approached if doing so appeared inappropriate (eg, because of clinical instability requiring active interventions, severe emotional stress, or withdrawal of life support). Interviews were conducted at the patient’s bedside, in a private location in the MICU, or (for some surrogates) by phone. Responses were recorded in writing by the interviewer in real time. The interviewer deemed patients/surrogates capable of providing consent if they were alert, able to communicate, and able to understand what would be expected of them during the interview, what they would do if they no longer wanted to participate in the study, and what they would do if they experienced distress or discomfort during the interview. MICU physicians were notified by e-mail about the study before enrollment began, and members of the research team were excluded from participation.
Survey Instrument
A previously developed survey instrument13 was modified for use in the ICU setting and underwent minor revisions after the first few interviews to increase clarity (a copy is available from the corresponding author). The survey instrument provided a verbatim guide for the interviewer and consisted of closed-ended and open-ended questions. In-hospital CPR was understood as having three components: defibrillation, chest compressions, and intubation with mechanical ventilation (“full code” consists of a decision to receive, in case of arrest, all three components; “do not resuscitate” refers to a decision to receive none of these components). We queried patients/surrogates about their goals of care, first in open-ended fashion and then in closed-ended fashion. A structured literature review11 provided the six (closed-ended) goals of care that were queried: be cured; live longer; improve/maintain current health (or quality of life and independence); be comfortable; achieve life goals (such as accomplishing something particular in life); and provide support for family/caregivers. Patients/surrogates were also given the opportunity to specify an “other” goal beyond these six options.
Regarding outcome probabilities, the interviewer asked, “On a scale from 0 to 100%, what do you think are the chances of someone surviving a cardiac arrest in the hospital if they receive CPR?” Based on published data,20 the interviewer then said, “Research has shown that if someone has a cardiac arrest in the hospital and is treated with CPR, their chance of surviving long enough to leave the hospital is approximately 18% (18 out of 100). Amongst patients in the ICU who experience a cardiac arrest and are treated with CPR, the chance of surviving long enough to leave the hospital is approximately 16% (16 out of 100),” and added, “While these data may not predict your (or your loved one’s) chance of surviving CPR, does this information make you want to change your preferences (for him/her) about receiving CPR while you (he/she) are (is) in the hospital?” The interviewer then said, “Research has also shown that if someone has a cardiac arrest in the hospital and is treated with CPR, their chance of leaving the hospital with good brain function is approximately 14% (14 out of 100),” and added, “Does this information make you want to change your preferences (for him/her) about receiving CPR while you (he/she) are (is) in the hospital?”
Physicians were asked which goals of care they believed were medically appropriate for the patient, which goal was most important, and how much they agreed or disagreed with the patient’s current treatment plan. Physicians were not informed of patients’/surrogates’ responses to questions about their goals of care. (Questions about goals of care were added to the physician interviews after the first six interviews had already been conducted.)
Medical Record Review
Patients’ medical records were reviewed immediately after each interview. If a discrepancy was found between a patient’s code status order in the medical record and the patient’s code status preferences expressed during the interview, the patient’s faculty physician was notified.
Statistical Analysis
Data were double-entered into an Access data file and uploaded into SAS (SAS Institute Inc; Cary, North Carolina). Frequency, χ2, and Kruskal Wallis tests of significance were used for analysis. Differences were considered statistically significant at level of P < .05. There were some missing values in the χ2 analyses (range 0-5, except for one case of 8).
Results
Demographic and Hospitalization Data
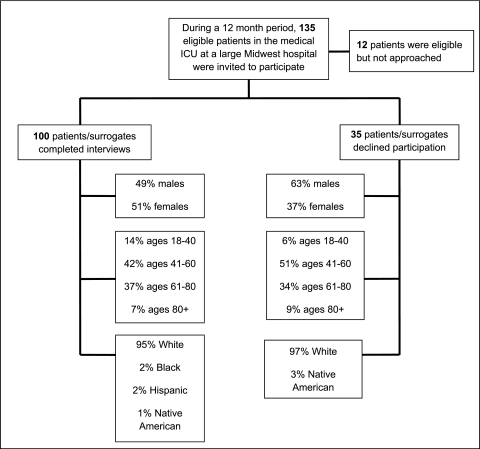
Figure 1 compares the 100 participating patients with the 35 patients who declined (or whose surrogates declined) participation. Table 1 shows the interviewee descriptions and demographic data for patients.
Figure 1.
Flowchart of patients included in the study.
Table 1.
—Participant Descriptions and Patient Demographic Data
| Participant Variable | Result |
| Patients/surrogates, total, No. | 100 |
| Patients | 20 |
| Surrogates | 80 |
| Surrogates, type, No. | |
| Spouse | 39 |
| Adult child | 18 |
| Parent | 9 |
| Sibling | 8 |
| Legal guardian | 2 |
| Durable power of attorney for health care (no other description) | 2 |
| Nephew | 1 |
| Friend | 1 |
| Physician interviews, total, No. | 99 |
| Faculty | 32 |
| Fellow | 67 |
| Physician participants, total, No. | 15 |
| Faculty | 7 |
| Fellow | 8 |
| Patient age, mean, y | 58.1 |
| Patient gender, No. | |
| Women | 51 |
| Men | 49 |
| Patient race/ethnicity, No. | |
| White | 95 |
| Black | 2 |
| Hispanic | 2 |
| Native American | 1 |
| Patient APACHE II score for hospital mortality, mean | 22.5 |
| Patient length of stay in MICU, mean/median/range, d | 10.3/9/3-38 |
| Day number of MICU hospitalization when interview occurred, mean/median/range, d | 5.3/3/3-28 |
| Patient primary admitting diagnoses, No. | |
| Respiratory | 45 |
| Infectious diseases | 15 |
| Gastroenterologic | 12 |
| Neurologic | 11 |
| Cardiac | 7 |
| Other | 10 |
| Possession of a living will, by patient/surrogate report, No. | 40 |
| Possession of a durable power of attorney for health care, by patient/surrogate report, No. | 47 |
| Patient or surrogate religious service attendance, No. | |
| At least once a week | 32 |
| At least once a month | 13 |
| Once a year or a few times a year | 35 |
| Never | 20 |
| Patients’/surrogates’ religious or spiritual beliefs provide comfort when thinking about death or dying, No. | |
| Yes | 84 |
| No | 15 |
| Unsure | 1 |
APACHE = Acute Physiology and Chronic Health Evaluation; MICU = medical ICU.
CPR and Code Status: Knowledge, Preferences, Orders, and Discussions
Table 2 shows respondents’ knowledge and attitudes regarding CPR and goals-of-care discussions. Only four participants were able to identify all three components of in-hospital CPR; 83 participants preferred administration of all three, and nine preferred none. Respondents’ prediction of a patient’s survival following in-hospital cardiac arrest with CPR was, on average, 71.8% (range 10%-100%). After learning the evidence-based likelihood of survival after CPR, four respondents were less interested in receiving CPR. After learning the likelihood of a good neurologic outcome following CPR, eight respondents (inclusive of the four just mentioned) were less interested in receiving CPR. Factors associated with a preference for full code status are shown in Table 3. There was a linear relationship between predicted likelihood of survival after CPR and preference for CPR: the higher the predicted survival, the more frequent the preference for full code status.
Table 2.
—Patient or Surrogate Knowledge and Attitudes Regarding CPR, Code Status Preferences, and Goals-of-Care Discussions
| Knowledge or Attitude Measured | No. |
| Knowledge of what “CPR” stands for | |
| Perceived knowledge | 65 |
| Actual knowledge | 17 |
| Knowledge of what treatments doctors use during CPR | |
| Perceived knowledge | 95 |
| Actual knowledge of the three main components of CPR | |
| Cardiac defibrillation | 32 |
| Chest compressions | 71 |
| Intubation with mechanical ventilation | 7 |
| Preferences regarding code status (verbatim text shown) | |
| “In case your (your loved one’s) heart stopped beating or your (his/her) lungs stopped breathing, which would mean that you (he/she) were (was) dying, would you want your (his/her) physicians…” | |
| “… to use defibrillation (that is, electricity) on your (his/her) chest to shock your (his/her) heart to make it start beating again?” [yes] | 84 |
| “… to use chest compressions (that is, to push up and down on your [his/her] chest) to try to keep the blood moving through your (his/her) body?” [yes] | 83 |
| “… to use intubation (that is, to have a tube placed through your [his/her] mouth and into your [his/her] windpipe) so that a breathing machine can then move air in and out of your (his/her) lungs?” [yes] | 90 |
| Patient code status as documented in medical record | |
| Full code | 85 |
| Do not resuscitate | 13 |
| No documentation | 2 |
| Discussions with physician during current hospitalization, by patient/surrogate report | |
| Discussion about CPR preferences | 50 |
| Discussion about at least one goal of care | 51 |
| Discussion about CPR preferences and at least one goal of care | 28 |
| No discussion about CPR preferences or at least one goal of care | 27 |
| Participant attitudes at end of interview | |
| Believed it was helpful to talk about chances of surviving cardiac arrest after CPR | 80 |
| Believed it was helpful to talk about goals of care | 71 |
Table 3.
—Factors Associated With Patient/Surrogate Preference for Full Code Status
| Factor | Percentage Desiring Full Code Status | P Value |
| Age, y | .025 | |
| 18-49 | 93.3 | |
| 50-64 | 88.2 | |
| 65-74 | 77.8 | |
| 75-89 | 61.1 | |
| APACHE II score | .062 | |
| 7-22 | 90.0 | |
| 23-43 | 76.0 | |
| Religious service attendance | .042 | |
| Less than once weekly | 88.2 | |
| At least weekly | 71.8 | |
| Most important goal | .046 | |
| Cure | 96.0 | |
| All other goals | 78.7 | |
| Living will | .005 | |
| Absent or uncertain | 91.7 | |
| Present | 70.0 | |
| Durable power of attorney for health care | .032 | |
| Absent or uncertain | 90.6 | |
| Present | 74.5 | |
| Goals-of-care discussion with physician | .076 | |
| No | 89.8 | |
| Yes | 76.5 | |
| Physician agreement with patient’s treatment plan | .029 | |
| “Strongly agree” or “agree” | 86.1 | |
| “Neutral,” “disagree,” or “strongly disagree” | 61.5 | |
| Estimated chance of survival following CPR, % | .012 | |
| 0-25 | 33.3 | |
| 26-50 | 64.7 | |
| 51-75 | 82.9 | |
| 76-100 | 92.7 |
See Table 1 legend for expansion of abbreviation.
Code Status Discrepancies
Ninety-eight patients had documentation of code status in the medical record (85 full code, 13 do not resuscitate). For 16 patients there was a discrepancy between code status preferences expressed during the interview and the code status order in the medical record. In 10 cases, the patient/surrogate desired less treatment than documentation reflected, and in six instances the patient/surrogate desired more treatment. Patients were less likely to have a code status discrepancy if: (1) their most important goal of care was cure, as compared with all other goals (4.0% vs 20.0%, P = .058); (2) they preferred full code status, as compared with not full code status (7.2% vs 58.8%, P < .001); and (3) the physician agreed or strongly agreed that the patient’s treatment plan was medically appropriate (12.8% vs 38.5%, P = .019). Discrepancies were more likely among respondents who reported having discussed goals of care with their physicians (23.5% vs 8.2%, P = .036).
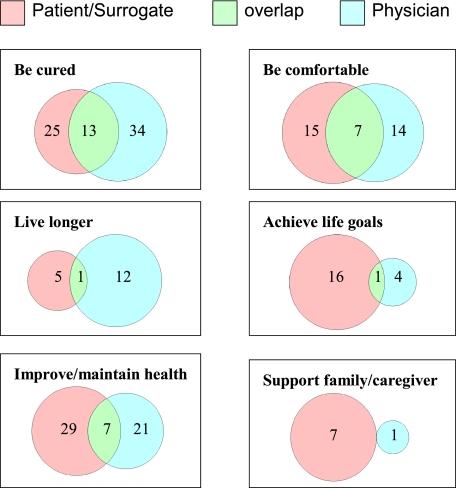
Goals of Care
Most patients/surrogates (88%) were able to answer the open-ended question, “Please tell me what your goals of care are for your (your loved one’s) treatment in the hospital,” and the 12% who did not seem to understand this question were able to answer the follow-up question, “What are you expecting will be accomplished by your (your loved one’s) treatment in the hospital?” Of six possible (closed-ended) goals of care, approximately five goals of care were affirmed by each patient/surrogate (5.2) and physician (5.1), and Table 4 shows the frequencies with which patients/surrogates and physicians affirmed specific goals of care and the most important goal of care. In 67.7% (63/92) of cases, the most important goal of care identified by patients/surrogates differed from the one identified by physicians, and the overlap between their most important goals of care is shown in Figure 2.
Table 4.
—Frequencies of Goals of Care Affirmed by Patients/Surrogates and Physicians
| Goal of Care | Patients/Surrogates, No. (%) | Physicians,a No. (%) |
| Goals of care affirmed (participants were asked to select as many goals as pertained) | ||
| Be cured | 84 (84.0) | 74 (79.6) |
| Live longer | 95 (95.0) | 86 (92.5) |
| Improve or maintain health/quality of life/independence | 95 (95.0) | 86 (92.5) |
| Be comfortable | 100 (100.0) | 87 (93.5) |
| Achieve life goals | 72 (72.0) | 67 (72.0) |
| Provide support for family/caregivers | 73 (73.0) | 71 (78.0) |
| Other | 2 (2.0) | 1 (1.1) |
| Most important goal of care (participants were asked to select the one most important goal) | ||
| Be cured | 25 (25.0) | 34 (37.0) |
| Live longer | 5 (5.0) | 12 (13.0) |
| Improve or maintain health/quality of life/independence | 29 (29.0) | 21 (22.8) |
| Be comfortable | 15 (15.0) | 14 (15.2) |
| Achieve life goals | 16 (16.0) | 4 (4.3) |
| Provide support for family/caregivers | 7 (7.0) | 1 (1.1) |
| Could not select one most important goal of care | 3 (3.0) | 5 (5.4) |
| Other | n/a | 1 (1.1) |
n/a = not applicable.
Ninety-three physicians provided responses to questions about each of the six goals of care, and 92 physicians provided responses regarding the most important goal of care.
Figure 2.
Venn diagrams of the selections by patients/surrogates and physicians selections of the most important goals of care.
Physician Assessment of Patient’s Treatment Plan
When asked to respond to the statement “The patient’s current treatment plan is medically appropriate,” 86.9% of physicians agreed or strongly agreed, 6.1% were neutral, and 7.1% disagreed or strongly disagreed; two physicians who disagreed had considered excusing themselves from the patient’s care or transferring the patient’s care to another provider.
Discussion
To our knowledge, this is the first study to address code status preferences and goals of care in a population of critically ill patients hospitalized in a MICU. Our data suggest that patients in the MICU and their surrogates have a poor understanding of CPR as it is administered in hospitals and an excessively positive estimation of its likelihood of success. Our results also suggest that in a substantial minority of cases, there may be a discrepancy between code status preferences patients/surrogates express and code status orders in the medical record. Our findings also show that goals of care in the MICU are diverse and that patients/surrogates may differ with their physicians about which goal should be given the highest priority.
Participants in our study had inadequate knowledge of CPR and its outcomes in the hospital setting. Only 4% of respondents were able to identify the three main components of in-hospital CPR, and respondents grossly overestimated the likelihood of survival following CPR. Moreover, the beliefs of patients/surrogates about CPR outcome probabilities appeared to guide their CPR preferences: the higher the overestimate of survival, the greater the likelihood of a preference for CPR. Such knowledge deficits regarding CPR are consistent with studies of other populations,13,18,21‐23 and the correlation between increased understanding of CPR survival probabilities and decreased preference for CPR has been noted among nonhospitalized persons.17,24 There is also evidence that physicians rarely discuss with their patients the likelihood of survival following CPR.25 Taken together, available data argue for the need for more dialogue about CPR and its outcome probabilities during code status discussions, with the acknowledgment that it may be challenging to say how a given patient’s prospects compare with the 18% mean likelihood of survival to discharge after in-hospital CPR documented in large studies.20,26
Discrepancies between patients’ preferences regarding resuscitation and their actual code status orders were found in 16% of the patients we studied, and this occurred despite the perception by patients/surrogates that code status discussions occurred 50% of the time, which is higher than in other inpatient studies.2,23,27‐29 The possible causes of such discrepancies include lack of communication, miscommunication, and a failure to revisit code status preferences as the course of illness worsens or improves, but our findings also suggest discrepancies may be more likely when a patient’s most important goal of care is not cure or when a physician does not believe that a patient’s treatment plan is medically appropriate.
Our data include new findings about goals of care in the setting of the MICU. Patients/surrogates affirmed as many as five goals of care simultaneously and were almost always able to identify one goal that is most important; a strong majority (71%) believes it is helpful to talk about goals of care. However, we also observed a paradoxical association between code status discrepancies and goals-of-care discussions (as perceived by patients/surrogates). We do not know what prompted these discussions or what they contained. One possibility is that a goals-of-care discussion may be a marker for challenging circumstances that required more communication to reach consensus about a treatment decision. Furthermore, such circumstances may be sufficiently resistant to consensus that goals discussions may not necessarily prevent the uncertainties or confusions that lead to code status discrepancies. This latter possibility is all the more concerning if patients/surrogates differ with physicians about which goal of care should be given highest priority, a phenomenon that was common in our study population (67.7% of cases).
Our study had limitations. Although our patient population represented a broad range of adults with critical illness admitted to a MICU, some disease categories were underrepresented (postoperative complications, cardiovascular disease, and trauma). Data were gathered from a single MICU with limited racial and ethnic diversity among patients, and the number of physician participants was small. Although 80% of participants were surrogates, rather than patients, this distribution reflects the reality of ICU practice in which physicians routinely rely upon surrogates to assist decision making for patients who lack decision-making capacity.5 The clustering of patients and surrogates within physicians may have confounded our results, and the small size of our sample limited our ability to adjust for this clustering. Finally, the CPR outcome probabilities we provided to patients/surrogates were based on statistical means rather than patient-specific estimates; therefore, the statistical figures we provided to patients may not reflect the individualized outcomes that might be predicted on the basis of each patient’s particular medical circumstances.
Expert consensus has noted the importance of goals of care for navigating conflicts and guiding the transition from curative to palliative care,6 and there are good reasons to place code status discussions within a framework of goals.30 Nevertheless, it remains uncertain whether discussing goals of care can improve shared decision making and decrease the frequency of discrepancies between resuscitation preferences and code status orders. Prospective studies are needed to determine the content that goals-of-care discussions should include, how these discussions should be conducted, and what their impact on treatment decisions, including code status orders, may be.
Acknowledgments
Author contributions: Dr Kaldjian had full access to the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Gehlbach: contributed to study concept and design; acquisition, analysis, and interpretation of data; drafting the manuscript; critical revision of the manuscript for important intellectual content; obtaining funding; and administrative, technical, or material support.
Ms Shinkunas: contributed to study concept and design; critical revision of the manuscript for important intellectual content; and administrative, technical, or material support.
Dr Forman-Hoffman: contributed to statistical analysis and critical revision of the manuscript for important intellectual content.
Dr Thomas: contributed to study concept and design and critical revision of the manuscript for important intellectual content.
Dr Schmidt: contributed to study concept and design and critical revision of the manuscript for important intellectual content.
Dr Kaldjian: contributed to study concept and design; analysis and interpretation of data; drafting the manuscript; critical revision of the manuscript for important intellectual content; administrative, technical, or material support; and study supervision.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsor: The sponsor had no role in design or conduct of the study or in the analysis or reporting of the data.
Abbreviations
- MICU
medical ICU
Footnotes
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (http://www.chestpubs.org/site/misc/reprints.xhtml).
Funding/Support: Dr Gehlbach was supported by a Ruth L. Kirschstein National Research Service Award [5 T32 HL 07638-22].
References
- 1.von Gunten CF, Ferris FD, Emanuel LL. The patient-physician relationship. Ensuring competency in end-of-life care: communication and relational skills. JAMA. 2000;284(23):3051–3057. doi: 10.1001/jama.284.23.3051. [DOI] [PubMed] [Google Scholar]
- 2.Hofmann JC, Wenger NS, Davis RB, et al. SUPPORT Investigators. Study to Understand Prognoses and Preference for Outcomes and Risks of Treatment Patient preferences for communication with physicians about end-of-life decisions. Ann Intern Med. 1997;127(1):1–12. doi: 10.7326/0003-4819-127-1-199707010-00001. [DOI] [PubMed] [Google Scholar]
- 3.Wenger NS, Phillips RS, Teno JM, et al. Physician understanding of patient resuscitation preferences: insights and clinical implications. J Am Geriatr Soc. 2000;48(5) Suppl:S44–S51. doi: 10.1111/j.1532-5415.2000.tb03140.x. [DOI] [PubMed] [Google Scholar]
- 4.Evans LR, Boyd EA, Malvar G, et al. Surrogate decision-makers’ perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med. 2009;179(1):48–53. doi: 10.1164/rccm.200806-969OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White DB, Braddock CH, III, Bereknyei S, Curtis JR. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med. 2007;167(5):461–467. doi: 10.1001/archinte.167.5.461. [DOI] [PubMed] [Google Scholar]
- 6.Truog RD, Campbell ML, Curtis JR, et al. American Academy of Critical Care Medicine Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008;36(3):953–963. doi: 10.1097/CCM.0B013E3181659096. [DOI] [PubMed] [Google Scholar]
- 7.Balaban RB. A physician’s guide to talking about end-of-life care. J Gen Intern Med. 2000;15(3):195–200. doi: 10.1046/j.1525-1497.2000.07228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Emanuel LL. Structured deliberation to improve decisionmaking for the seriously ill. Hastings Cent Rep. 1995;25(6):S14–S18. [PubMed] [Google Scholar]
- 9.Emanuel LL, von Gunten CF, Ferris FF, editors. The Education in Palliative and End-of-Life Care (EPEC) curriculum: The EPEC Project. Chicago, IL: The Robert Wood Johnson Foundation; 1999. Module 7: goals of care. [Google Scholar]
- 10.Lesage P, Portenoy RK. Ethical challenges in the care of patients with serious illness. Pain Med. 2001;2(2):121–130. doi: 10.1046/j.1526-4637.2001.002002121.x. [DOI] [PubMed] [Google Scholar]
- 11.Kaldjian LC, Curtis AE, Shinkunas LA, Cannon KT. Goals of care toward the end of life: a structured literature review. Am J Hosp Palliat Care. 2008;25(6):501–511. doi: 10.1177/1049909108328256. [DOI] [PubMed] [Google Scholar]
- 12.Kaldjian LC, Weir RF, Duffy TP. A clinician’s approach to clinical ethical reasoning. J Gen Intern Med. 2005;20(3):306–311. doi: 10.1111/j.1525-1497.2005.40204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaldjian LC, Erekson ZD, Haberle TH, et al. Code status discussions and goals of care among hospitalised adults. J Med Ethics. 2009;35(6):338–342. doi: 10.1136/jme.2008.027854. [DOI] [PubMed] [Google Scholar]
- 14.Bradley EH, Bogardus ST, Jr, Tinetti ME, Inouye SK. Goal-setting in clinical medicine. Soc Sci Med. 1999;49(2):267–278. doi: 10.1016/s0277-9536(99)00107-0. [DOI] [PubMed] [Google Scholar]
- 15.Rosenfeld KE, Wenger NS, Kagawa-Singer M. End-of-life decision making: a qualitative study of elderly individuals. J Gen Intern Med. 2000;15(9):620–625. doi: 10.1046/j.1525-1497.2000.06289.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schneiderman LJ, Kaplan RM, Pearlman RA, Teetzel H. Do physicians’ own preferences for life-sustaining treatment influence their perceptions of patients’ preferences? J Clin Ethics. 1993;4(1):28–33. [PubMed] [Google Scholar]
- 17.Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330(8):545–549. doi: 10.1056/NEJM199402243300807. [DOI] [PubMed] [Google Scholar]
- 18.Fischer GS, Tulsky JA, Rose MR, Siminoff LA, Arnold RM. Patient knowledge and physician predictions of treatment preferences after discussion of advance directives. J Gen Intern Med. 1998;13(7):447–454. doi: 10.1046/j.1525-1497.1998.00133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fried TR, Van Ness PH, Byers AL, Towle VR, O’Leary JR, Dubin JA. Changes in preferences for life-sustaining treatment among older persons with advanced illness. J Gen Intern Med. 2007;22(4):495–501. doi: 10.1007/s11606-007-0104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peberdy MA, Ornato JP, Larkin GL, et al. National Registry of Cardiopulmonary Resuscitation Investigators Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 21.Shmerling RH, Bedell SE, Lilienfeld A, Delbanco TL. Discussing cardiopulmonary resuscitation: a study of elderly outpatients. J Gen Intern Med. 1988;3(4):317–321. doi: 10.1007/BF02595786. [DOI] [PubMed] [Google Scholar]
- 22.Miller DL, Jahnigen DW, Gorbien MJ, Simbartl L. Cardiopulmonary resuscitation: how useful? Attitudes and knowledge of an elderly population. Arch Intern Med. 1992;152(3):578–582. doi: 10.1001/archinte.152.3.578. [DOI] [PubMed] [Google Scholar]
- 23.Heyland DK, Frank C, Groll D, et al. Understanding cardiopulmonary resuscitation decision making: perspectives of seriously ill hospitalized patients and family members. Chest. 2006;130(2):419–428. doi: 10.1378/chest.130.2.419. [DOI] [PubMed] [Google Scholar]
- 24.Schonwetter RS, Walker RM, Kramer DR, Robinson BE. Resuscitation decision making in the elderly: the value of outcome data. J Gen Intern Med. 1993;8(6):295–300. doi: 10.1007/BF02600139. [DOI] [PubMed] [Google Scholar]
- 25.Tulsky JA, Chesney MA, Lo B. How do medical residents discuss resuscitation with patients? J Gen Intern Med. 1995;10(8):436–442. doi: 10.1007/BF02599915. [DOI] [PubMed] [Google Scholar]
- 26.Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med. 2009;361(1):22–31. doi: 10.1056/NEJMoa0810245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Covinsky KE, Fuller JD, Yaffe K, et al. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments Communication and decision-making in seriously ill patients: findings of the SUPPORT project. J Am Geriatr Soc. 2000;48(5) suppl:S187–S193. doi: 10.1111/j.1532-5415.2000.tb03131.x. [DOI] [PubMed] [Google Scholar]
- 28.Reilly BM, Magnussen CR, Ross J, Ash J, Papa L, Wagner M. Can we talk? Inpatient discussions about advance directives in a community hospital. Attending physicians’ attitudes, their inpatients’ wishes, and reported experience. Arch Intern Med. 1994;154(20):2299–2308. [PubMed] [Google Scholar]
- 29.Frankl D, Oye RK, Bellamy PE. Attitudes of hospitalized patients toward life support: a survey of 200 medical inpatients. Am J Med. 1989;86(6 pt 1):645–648. [PubMed] [Google Scholar]
- 30.Kaldjian LC, Broderick A. Developing a policy for do not resuscitate orders within a framework of goals of care. Jt Comm J Qual Patient Saf. 2011;37(1):11–19. doi: 10.1016/s1553-7250(11)37002-x. [DOI] [PubMed] [Google Scholar]