Abstract
Objectives:
To evaluate appropriateness of prescribing medicines in geriatric patients using both Beers criteria and Phadke's criteria and compare them for validation of Phadke's criteria as a tool to evaluate rationality of prescribing in elderly.
Materials and Methods:
A cross-sectional prospective observational study was conducted and the baseline data were collected from different inpatient and outpatient departments in Shree Krishna Hospital (SKH), Karamsad. A total of 400 patients of geriatric age group (≥65 years) from various inpatient and outpatient departments of SKH were included in the study. Relevant information from patients included in the study was recorded in a structured proforma from their case files. Data were evaluated for appropriateness of prescribing by using both Beers criteria and Phadke's criteria and comparison between the two criteria was also carried out.
Results:
Out of total 400 patients, 291 (72.75%) patients were prescribed appropriately according to Beers criteria. Based on Phadke's criteria, 158 (39.5%) prescriptions were rational, 129 (32.3%) were semirational and 113 (28.3%) were irrational. Mean rationality score on a 30-point semiscientific scale was found to be 18.47 ± 9.66 (mean ± SD). The comparison of outcome by both the criteria showed no significant difference in appropriateness of prescribing (P>0.05).
Conclusions:
Inappropriate prescribing is common in elderly patients. Beers criteria is a well-established method for evaluating appropriateness of prescribing. This study has shown that Phadke's method of evaluating rationality of prescriptions compares equally well and hence can be a valuable objective tool for assessing appropriateness of prescribing in geriatric patients.
Keywords: Beers criteria, geriatrics, Phadke's criteria
INTRODUCTION
Rational (appropriate) prescribing is that which bases the choice of a drug on its effectiveness, safety and convenience relative to other drugs in a particular patient and takes cost into account only when the above criteria for choice have been satisfied.[1]
Evidence indicates that high prevalence of inappropriate prescribing of medicines in elderly people is associated with increased morbidity and mortality, increased cost of treatment and decreased quality of life. Inappropriate prescribing has therefore become a significant public health issue worldwide. Hence effective optimization strategies are needed to improve prescribing of medicines in older patients.[2] Therefore, there is a need for a simple, inexpensive and time-efficient screening tool which can be used routinely to guide prescribing practice and reduce the rate of inappropriate prescribing in older patients. Such a tool should be sensitive, specific, include commonly encountered Adverse Drug Events (ADE) and have good inter-rater reliability. To be clinically relevant, use of such a screening tool must translate into positive clinical outcomes. Specific ADE causality assessment criteria for older people are also needed to measure the result of such interventions.[3]
There are no definite standardized criteria for assessing rationality of doctors’ prescription. Different investigators have analyzed prescriptions with their own different indicators. This suggests that there is a need for uniform criteria for evaluation of appropriateness of prescribing in general and in geriatric patients in particular. This study is an effort to find out objective criteria with scoring system to evaluate rationality of prescribing in elderly by using Phadke's criteria.
MATERIALS AND METHODS
A prospective observational study spread over 2 years and 3-months duration was undertaken from August 2007 to October 2009, in Shree Krishna Hospital (SKH) and medical research centre, a 550 bedded tertiary care rural, teaching hospital attached to Pramukh Swami Medical College, Karamsad, India. The study protocol was approved by Human Research Ethics Committee of the institute.
Sample size
Four hundred patients of geriatric age group (≥65 years), 200 each from various inpatient and outpatient departments of SKH were included in the study.
Criteria for inclusion of participants
Patients of either sex who had completed 65 years of age on 31st July, 2007 or earlier and attended to various outpatient or inpatient departments like Medicine, Surgery, Obstetrics and Gynecology, Orthopedics, Psychiatry, Skin, TB and Chest, Ophthalmology, ENT, Oncology and Dentistry were included in the study.
Criteria for exclusion of participants
Patients unable to communicate i.e., patients on ventilators, seriously ill patients requiring ICU admission or unwilling to participate were excluded from the study.
The study was conducted in both indoor and outdoor patients meeting inclusion criteria. A time period of 2 months each in a sequential manner was spent in departments of General medicine, Surgery, Obstetrics and Gynecology and Orthopedics and 15 days each in the departments of Psychiatry, Skin, TB and chest, Ophthalmology, ENT, Oncology and Dentistry. Patients were recruited in the study on prorata basis in the stipulated time period and all the patients participating in the study were explained clearly about the purpose and nature of the study in the language they could understand. Written informed consent was obtained before including them in the study. All indoor patients from respective departments were visited daily during their hospital stay and interviewed. Every indoor patient was then followed up till he/she was discharged and their case record sheets were reviewed for gathering necessary information in a prestructured case record form. All outdoor patients, new as well as old, meeting the inclusion criteria attending to various departments were interviewed once only and their case sheets were reviewed to gather necessary information -as on that day- to fill-up case record forms. For indoor patients whole therapy was considered as one prescription while for outdoor patients treatment given on that day was considered as one prescription. The gathered data was analyzed for rationality/appropriateness of prescribing by Beers criteria, rationality/appropriateness of prescribing by Phadke's criteria and comparison between the two criteria was carried out.
Appropriateness of prescribing
Appropriateness of prescribing was assessed using Beers criteria and Phadke's criteria both. Beers criteria gives status to every drug as appropriate or inappropriate for the elderly in given conditions while Phadke's criteria is based on a 30-point scale and ultimately assign a prescription the status as rational, semirational or irrational.
Beers criteria[4] are a comprehensive set of explicit criteria for potentially inappropriate drug use in elderly aged 65 years and above. Accordingly inappropriate drugs are categorized as the drugs that generally should be avoided in older adults (Category A), drugs that exceed maximum recommended daily dose (Category B) or drugs to be avoided in combination with specific comorbidity (Category C).
Phadke's criteria[5] is a method to assess a prescription for rationality as a whole and assign the status as rational, semirational or irrational to it. It is based on a 30-point scale comprising of 20 points for main drug/s and 10 points for complementary drug/s. Half of the points (10 and 5 respectively) for each of these two categories are allotted to the drug chosen for the condition and remaining half for the correctness of the dose given, including route and frequency of administration and the duration of therapy. If more than two drugs are needed to be given in a condition, the points allocated are subdivided accordingly. For deciding correctness of selection of a drug, its dose, route, frequency of administration and duration of therapy, evidence base is searched and applied. For computing the final score (out of 30), when necessary, negative points are assigned as under:
-
(a)
Irrational drug or irrational drug combination: 5 for each drug/formulation.
-
(b)
Unnecessary drug or injection: 5 for each drug/formulation
-
(c)
Hazardous drugs: 10 for each drug/formulation.
-
(d)
Unnecessary injection: 5 for each injection.
An irrational drug or irrational drug combination means a drug not recommended in the standard textbook of pharmacology or other evidence-based source, an unnecessary drug or injection is a category of drug or formulation not recommended for that particular condition. However, rational alternatives are not considered unnecessary. A hazardous or banned drug is the one which is listed under the heading ‘Banned and bannable drugs’ of Voluntary Health Association of India, 2003.
Prescription analysis guidelines (Phadke's criteria)
-
Correctness of main drug (Out of 10 points)
- First choice drug used- 100% points
- Second choice drug used- 60% points
- Third choice drug used- 30% points
- Wrong drug used- 0% points.
-
Dose, duration, frequency of administration (Out of 10 points)
- Correct formulation, strength, dose and duration- 100% points
- Inadequate dose/excess dose- 50% points
- Wrong formulation- 50% points
- Totally wrong dose- 0% points
-
Correctness of complementary drug (Out of 5 points)
- First choice drug used- 100% points
- Second choice drug used- 60% points
- Third choice drug used- 30% points
- Wrong drug used instead of proper drug - 0% points.
-
Dose, duration, frequency of administration (Out of 5 points)
- Correct formulation, strength, dose and duration: -100% points
- Inadequate dose/excess dose- 50% points
- Wrong formulation- 50% points
- Totally wrong dose- 0% points
When wrong drug/s was/were used as main drug/s in the prescription, zero point was assigned out of 20, but same drug/s was/were not considered again in the column for unnecessary drug/s. When a complementary drug was not needed and hence not prescribed, full 10 points were assigned to the column of complementary drug/s. Net score for each prescription was computed using these criteria and prescriptions were graded as rational (25-30 points), semirational (15-24 points) or irrational (0-14 points).
Statistical analysis
All data were analyzed with the help of SPSS version 14 software. χ2 test was used for analysis and P-value less than 0.05 was considered as significant.
RESULTS
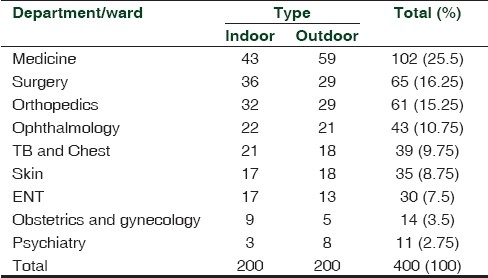
Majority of patients were in age group of 65-74 years, 76% and 68%; followed by age group of 75-84 years, 19% and 23.5% and lowest number of patients was in age group of more than 85 years, 5% and 8.5%; both in indoor and outdoor patients, respectively. Out of total 400 patients, 241 (60.3%) were males and 159 (39.7%) were females [Table 1]. Department-wise distribution of patients is shown in Table 2. Maximum number of patients (102, 25.5%) was from Medicine department followed by Surgery (65, 16.25%), Orthopedics (61, 15.25%) and Ophthalmology (43, 10.75%). The number of patients was small from Obstetrics and Gynecology (14, 3.5%) and Psychiatry (11, 2.75%) departments.
Table 1.
Demographic details of patients
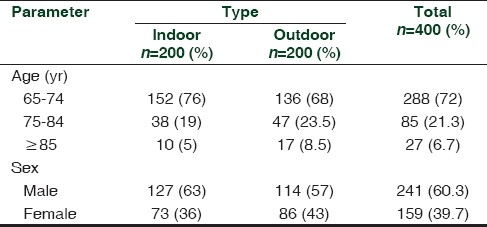
Table 2.
Department/ward-wise distribution of patients
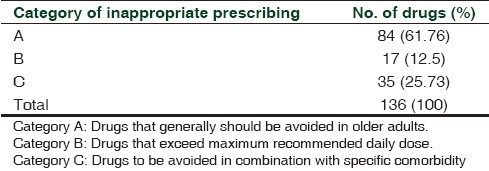
On evaluating appropriateness of prescribing by Beers criteria, out of total 400 patients, 291 (72.75%) patients were prescribed appropriately and 109 (27.25%) were prescribed inappropriately. A total of 2924 formulations were prescribed, of which 2788 (95.34%) were prescribed appropriately and 136 (4.65%) were prescribed inappropriately. According to categories of inappropriate prescribing, majority of drugs (85, 61.76%) fell in category A, followed by 35 drugs (25.73%) in category C. Lowest number of drugs (17, 12.5%) fell in category B [Table 3].
Table 3.
Categories of inappropriate drug use according to Beers criteria
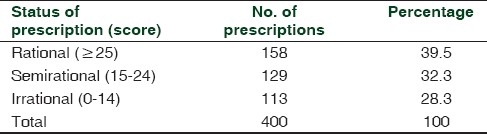
Of the 400 prescriptions analyzed, based on Phadke's criteria, 158 (39.5%), 129 (32.3%) and 113 (28.3%) prescriptions were rated as rational, semirational and irrational, respectively [Table 4]. Average rationality score per prescription was found to be 18.47 ± 9.66 (Mean ± SD) on a 30-point scale.
Table 4.
Status of prescriptions based on Phadke's criteria
When only inappropriately/irrationally prescribed drugs by both Beers criteria (109) and Phadke's criteria (113) were compared, we did not find any significant difference between the two (χ2=0.09, P=0.812).
DISCUSSION
Medicines should always be prescribed rationally in general, and particularly in elderly patients. Elderly population is on the rise worldwide to increased longevity. They suffer from more diseases requiring drug therapy. Drug therapy is the most common and important form of medical treatment in the care of elderly people. The elderly population is a major recipient of drug therapy, using considerably more drugs than the younger population.[6] Most of the drugs used by older people are consumed for many years to control chronic disorders such as diabetes, hypertension, congestive heart failure, asthma, etc. However, drugs may also be used for shorter periods to prevent diseases or relieve common symptoms or to treat infections.
Inappropriate prescribing can be defined as prescribing medications outside the bounds of accepted medical standards.[7] Inappropriate prescribing is more likely to occur in elderly patients since they may receive several drugs simultaneously on account of chronic diseases or/and multiple health problems. Prevalence of inappropriate prescribing is high in general but is variable in different parts of world. A study of potentially inappropriate medication use in elderly done in Georgia, evaluated using the Beers criteria, in a medically managed care population found a prevalence of 23%.[8] As against this, in a study carried out in Singapore,[9] it was found that prevalence of inappropriate use of medicines was around 70% in elderly patients evaluated using explicit criteria developed by a panel of experts in US and adopted by HCFA. This wide variability in inappropriateness of prescribing in elderly could be because of different criteria used for evaluation.
Currently there are a number of medication assessment tools available to clinicians for the purpose of evaluating medication regimens for rationality/appropriateness in elderly.[10] Beers criteria are well established and very frequently used method for evaluating appropriateness of prescribing in elderly. It was developed in 1999 and revised in 2003. Almost at the same time, in 1990s another method namely Phadke's criteria, was evolved to evaluate rationality of prescribing in general and not necessarily in elderly only.
In the present study, on evaluating the appropriateness of prescribing by Beers criteria, it is revealed that 4.65% of total drugs prescribed were inappropriate as compare to an earlier study conducted in south India (4.1%).[11] This is though apparently higher in our study, it is not statistically significant (χ2=0.03, P=0.8). In our study, total 109 patients out of 400 had received inappropriate prescription of at least one drug as evaluated by Beers criteria. This forms 27.25% of total patients, making a sizeable group. However, these findings are not significantly different from those found in the studies from the Netherlands[12] and Japan[13] which showed use of at least one inappropriate medicine in 20% (χ2=1.457, P=0.22) and 21.1% (χ2=1.032, P=0.31) of prescriptions, respectively. According to categories of inappropriate prescribing, majority of drugs (85, 61.76%) fell in category A, followed by 35 drugs (25.73%) in category C in our study. Lowest number of drugs (17, 12.5%) was falling in category B in this study. Almost similar pattern was found in a study from Ahmadabad.[14] This suggests that drugs ‘to be avoided in elderly’ are among the most frequently inappropriately prescribed drugs followed by drugs ‘to be avoided with certain comorbid conditions’ in elderly. Drugs in the category of, ‘drugs exceeded the certain dose limits’ were the least frequently prescribed. Thus it may be prudent to say that geographical differences do not matter in assessing appropriateness of prescribing in elderly when Beers criteria are used.
The present study is perhaps the first effort, to best of our knowledge, wherein Phadke's criteria have been used to evaluate rationality of prescribing exclusively in elderly. On evaluating rationality of prescribing in the present study using Phadke's criteria, we found that 39.5% of prescriptions were rational, 32.3% were semirational and 28.3% were irrational. Average rationality score was 18.47 ± 0.48 (mean ± SEM) per prescription. In an earlier study done by Gajjar BM[15] in 1999 at this institute only using Phadke's criteria reported an average rationality score of 19.23 ± 1.16 (mean ± SEM). However, there is no significant difference in the average rationality score from these two studies (Z=0.607, P>0.05). It may be noted that study done by Gajjar BM was in patients attending ‘General Medicine OPD’ at this institute, not necessarily all geriatric patients. It may be thus derived that Phadke's criteria are equally good for evaluating rationality of prescribing in elderly.
When the inappropriateness of prescribing was compared using both the Beers criteria (27.25%) and Phadke's criteria (28.3%) in the present study, we did not find any significant difference between the two (χ2=0.02, P>0.05). Similarly inappropriate prescribing found by Phadke's criteria (28.3%) in the present study was compared with inappropriate prescribing found in studies from the Netherlands[12] (20%) and Japan[13] (21.1%) using Beers criteria. We found no difference between our study and above two studies from Netherlands (χ2=1.88, P=0.17) and Japan (χ2=1.39, P=0.24). It can be thus inferred that Phadke's criteria can be effectively used to assess rationality of prescribing in geriatrics patients as it compares equally well with Beers criteria.
The advantage of using Beers criteria is that it gives information of each drug formulation prescribed to patient with regard to its appropriateness, but the disadvantage is that it is time consuming. Moreover, it categorizes the formulation as appropriate or inappropriate only. Whereas Phadke's criteria easily differentiates between rational prescribing as a whole at one end and irrational at other, having additional category of semirational prescribing. Rational prescribing is doubtlessly the best and the most desirable. In absence of it, semirational prescribing can be accepted as rational with some reservations. In addition, Phadke's criteria allow the use of an objective scale and the method is less time consuming. The only disadvantage is that it cannot categorize an individual drug formulation as appropriate or inappropriate as in Beers criteria.
In summary, inappropriate prescribing is quite prevalent in general, and also in elderly patients in particular, calling for attention of the health care providers. The present study has shown that though Phadke's criteria for evaluating rationality of prescriptions are used so long in general population, they can be effectively used in geriatric population also for the same purpose. It compares equally well in this regard with Beers criteria, a well established method for evaluating rationality of prescriptions exclusively in geriatric patients. It is recommended that both the methods can be gainfully used to complement each other. Although this may be time consuming, it will prove to be rewarding since their advantages are added and disadvantages are excluded.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Patel VJ, Mansuri SM. Rational drug use. Journal of Academy of Applied-Basic Medical Sciences. 2003;5:98–100. [Google Scholar]
- 2.London: Department of health; 2001. Mar, Medicines and older people: Implementing medications- related aspects of NSF for older people; p. 37. [Google Scholar]
- 3.Hamilton HJ, Gallagher PF, O’Mahony D. Inappropriate prescribing and adverse drug events in older people. BMC Geriatr. 2009;9:5. doi: 10.1186/1471-2318-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163:2716–24. doi: 10.1001/archinte.163.22.2716. [DOI] [PubMed] [Google Scholar]
- 5.Phadke A. 1st ed. New Delhi: Sage publications; 1998. Drug supply and use: Towards rational policy in India; pp. 85–100. [Google Scholar]
- 6.Rumble RH, Morgan K. Longitudinal trends in prescribing for elderly patients: Two surveys four years apart. Br J Gen Pract. 1994;44:571–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Spinewine A, Schmader KE, Barber N, Hughes C, Lapane KL, Swine C, et al. Appropriate prescribing in elderly people: How well can it be measured and optimised? Lancet. 2007;370:173–84. doi: 10.1016/S0140-6736(07)61091-5. [DOI] [PubMed] [Google Scholar]
- 8.Fick DM, Waller JL, Maclean JR, Heuvel RV, Tadlock JG, Gottlieb M, et al. Potentially inappropriate medication use in a medicare management care.Population: Association with higher costs and utilization. J Manag Care Pharm. 2001;7:407–13. [Google Scholar]
- 9.Mamun K, Lien CT, Goh-Tan CY, Ang WS. Polypharmacy and inappropriate medication use in Singapore nursing homes. Ann Acad Med Singapore. 2004;33:49–52. [PubMed] [Google Scholar]
- 10.Shelton PS, Fritsch MA, Scott MA. Assessing medication appropriateness in elderly. Drugs Aging. 2000;16:437–50. doi: 10.2165/00002512-200016060-00004. [DOI] [PubMed] [Google Scholar]
- 11.Shenoy S, Rao J, Sen A, Kumar V. Evaluation of the drug prescribing pattern in elderly patients in tertiary care hospital. Indian J Pharmacol. 2006;38(Suppl):90. [Google Scholar]
- 12.Van der Hooft CS, Jong GW, Dieleman JP, Verhamme KM, van der Cammen TJ, Stricker BH, et al. Inappropriate drug prescribing in older adults: The updated 2002 Beers criteria-a population-based cohort study. Br J Clin Pharmacol. 2005;60:137–44. doi: 10.1111/j.1365-2125.2005.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Niwata S, Yamada Y, Ikegami N. Prevalence of inappropriate medication using Beers criteria in Japanese long term care facilities. BMC Geriatr. 2006;6:1. doi: 10.1186/1471-2318-6-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaveri HG, Mansuri SM, Patel VJ. Use of potentially inappropriate medicines in elderly: A prospective study in medicine out-patient department of a tertiary care teaching hospital. Indian J Pharmacol. 2010;42:95–8. doi: 10.4103/0253-7613.64499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gajjar BM. Karamsad: Sardar Patel University; 1999. Evaluation and comparison of prescribing pattern of physicians from ‘the institute’ and ‘the private’ sectors for rational drug therapy [Msc thesis] [Google Scholar]


