Abstract
Introduction:
To study the effects of heparin and low-molecular weight heparin (LMWH) on potassium and sodium levels in patients with cardiovascular diseases (CVDs) and stroke.
Materials and Methods:
Sixty patients were recruited with 30 patients each receiving heparin and enoxaparin. Patients with CVD and stroke receiving heparin and LMWH were compared for their demographic profile and laboratory data, and this was analyzed by descriptive statistics. Risk factors associated with the development of hyperkalemia were analyzed using multiple logistic regression model.
Results:
There was an increase in potassium levels and decrease in sodium levels compared with baseline in both the groups. The difference between the groups with respect to sodium and potassium levels was not statistically significant. On analysis, the risk factors for development of hyperkalemia were baseline potassium levels, serum creatinine, and creatinine clearance. The change in sodium and potassium levels on the fifth day of therapy was increased with LMWH compared with heparin, although not statistically significant.
Conclusions:
The clinician should anticipate hyperkalemia especially in patients with renal impairment receiving these drugs.
Keywords: Enoxaparin, hyperkalemia, heparin, risk factors
INTRODUCTION
Heparin is an intravenous anticoagulant used in treatment and prophylaxis of pulmonary thromboembolism, deep vein thrombosis, and in post-myocardial infarction patients. It is now being replaced by low-molecular weight heparin (LMWH) because of certain advantages like equal efficacy, increased bioavailability, and less frequent dosing interval. Also, monitoring of activated partial thromboplastin time is not required. The major adverse effects of these drugs are bleeding, thrombocytopenia, alopecia, and osteoporosis. A rare adverse effect of heparin reported is hyperkalemia which manifests within a few days of initiation of therapy.[1] Insufficient and conflicting data are available regarding the effects of LMWH (enoxaparin) on serum potassium levels. Hence, this study was carried out to compare the effect of heparin and LMWH on serum potassium levels and also sodium.
MATERIALS AND METHODS
The protocol was approved by the Institute Human Ethics Committee and written informed consent was obtained from all the study patients. It was a single blind and parallel study conducted at a tertiary care hospital in Kolar from March to December 2010. Sixty patients of either sex in the age group of 40–60 years suffering from angina, myocardial infarction, and stroke were included in this study. Alternate patient receiving heparin and LMWH were recruited, 30 patients in each. Patients with first and recurrent attacks of angina, myocardial infarction, and cortical venous thrombosis were enrolled. Patients with baseline serum potassium <3.5 and >5 meq/l and serum sodium levels <135 and >145 meq/l were excluded. The serum potassium and sodium levels were estimated at the time of admission (baseline level) and on the fifth day after therapy in both the groups. Creatinine clearance (CrCl) was estimated at baseline using the Cockroft–Gault formula, and the patients were excluded if CrCl was <30 ml/min.[2]
Statistical analysis
Sample size was determined by power analysis with power of 0.95 and was found to be 30 in each group. Data are expressed as mean ± standard deviation (SD) for continuous variables and as percentages for categorical variables. Serum potassium and sodium were analyzed using Student's paired and unpaired “t” test. Correlation of potassium with continuous variables was done using Pearson's r coefficient. Predictor variables for hyperkalemia were evaluated using the logistic regression in both univariate and multivariate models, and odds ratio with 95% confidence intervals were computed. For the analysis of potential risk factors for hyperkalemia, continuous variables were dichotomized. Known risk factors from the literature were included in a multiple logistic regression model to analyze the independent association of these risk factors with a higher risk of the development of hyperkalemia. The median was used to dichotomize the continuous variables. Variables independently associated with higher risk in multiple logistic regression were defined as “major risk factors.” A value of P<0.05 was considered to indicate statistical significance.
RESULTS
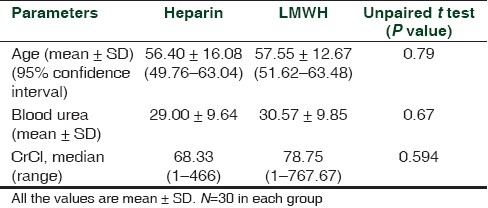
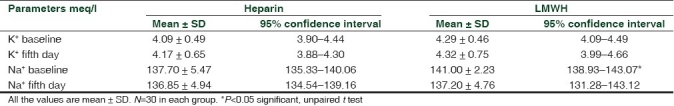
In our study, we had 41 males and 19 females, and they were age matched [Table 1]. There were 20 (67%) male and 10 (33%) female patients in heparin group, and LMWH group had 21 (70%) male and 9 (30%) female patients. Eleven (37%) and 10 (33%) patients had diabetes in heparin and LMWH groups, respectively. There was no significant difference in serum K+ and Na+ on fifth day when compared with baseline with heparin P=0.715 and 0.897 and with LMWH P=0.773 and 0.057, respectively.
Table 1.
Age distribution and kidney functions of the patients at baseline
Subcutaneous heparin and LMWH are commonly used in the treatment of angina, myocardial infarction, cortical venous thrombosis, and deep vein thrombosis [Table 2]. In this study, males were predominant, and majority of females were diagnosed as cortical venous thrombosis (17%). Neither of the drugs increased serum potassium levels significantly after 5 days of therapy [Table 3]. The K+ exceeded 5 meq/dl in two and four cases, which received heparin and LMWH respectively, and this was statistically significant (P=0.001). Patients who received LMWH had high levels of K+ at baseline and on fifth day [Table 3], but insignificant. The serum sodium levels were significantly higher with LMWH [Table 3] at baseline (P=0.04) and it lowered on fifth day. These findings prove the role of heparin and LMWH in inhibiting the aldosterone physiology thereby leading to increase in serum potassium levels and natriuresis. It can also be observed that patient receiving LMWH have significant alteration of the electrolytes, which indicates relatively more interference with aldosterone, and this effect was related to basal serum potassium (P=0.001) and did not show correlation with age, gender, and diagnosis (P>0.05).
Table 2.
Indications for heparin and LMWH
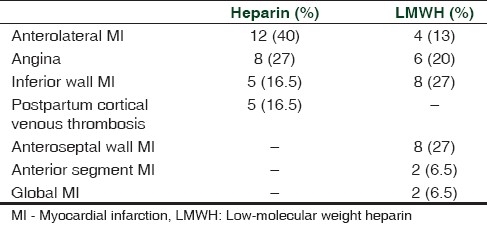
Table 3.
Serum K+ and Na+ values in both groups
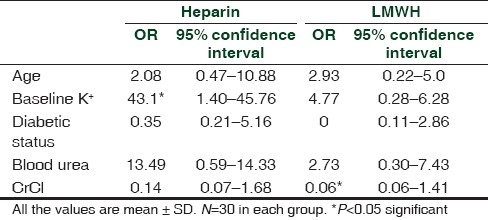
On the basis of univariate analysis, patients who received heparin developed hyperkalemia which was significant. The odds of developing hyperkalemia is eight times more with heparin if the baseline K+ was >4.3 meq/l. The odds ratios (ORs) and P values are shown in Table 4 and 5. Multivariate-adjusted ORs in the logistic regression model were 43.10 for baseline potassium in case of heparin (95% CI: 1.40–45.76; P=0.02) and 0.06 for CrCl for enoxaparin (95% CI: 0.06–1.41; P=0.05). There were no significant correlations between increase in potassium levels with age, diabetic status, and blood urea in the two groups. The univariate and multivariate analysis report for K+ levels on day 5 in both heparin and LMWH group is presented in Tables 4 and 5.
Table 4.
Univariate analysis of parameters with K+ levels on day 5
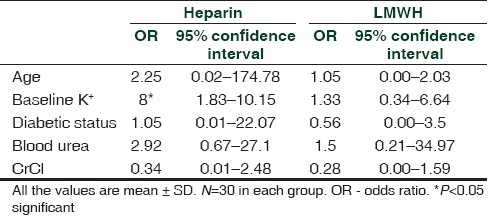
Table 5.
Multivariate analysis of parameters with K+ levels on day 5
DISCUSSION
Effect of heparin on adrenal metabolism has been documented since 1960s.[3] Heparin-induced hyperkalemia is mediated by a reversible effect on aldosterone through blockage of an enzymatic step in the synthesis and angiotensin II receptors in adrenal gland.[3,4] The most important mechanism of heparin-induced hypoaldosteronism involves the reduction in both number and affinity of angiotensin II receptors in the zona glomerulosa.[5] Prolonged administration of heparin has caused marked reduction in the width of adrenal zona glomerulosa thereby leading to hyperkalemia and natriuresis. These side effects are more common in elderly, renal insufficiency and diabetic patients.[6] This reversible suppression of aldosterone occurs within a few days of initiation of therapy and is independent of either the anticoagulant effect or the route of administration.[7] LMWHs have similar effects on aldosterone as unfractionated heparin or there may be a different risk of hyperkalemia which is still unsettled. This could possibly be because of the heterogeneity of the populations studied and the regimens of heparin used.[8,9] The inhibitory action is specifically on the glomerulosa zone of the adrenal cortex thereby other corticosteroids are spared.
Our findings confirm the role of renal insufficiency (measured as CrCl) in development of hyperkalemia. We found a marginally significant correlation between the development of hyperkalemia and basal potassium level, and similar findings have been reported by Gonzalez-Martin et al.[3] As baseline potassium level reflects pretreatment aldosterone level, its value has a predictive role for susceptibility to develop hyperkalemia. The various risk factors for the development of hyperkalemia according to univariate and multivariate analysis were found to be baseline potassium and CrCl (P≤0.05). The other risk factor identified was diabetes,[10,11] which is not seen in this study. Our results concur with those of Monreal et al.[2] who reported increase in serum potassium >5 meq/l in 7% receiving heparin and 15% LMWH among 30 patients. The practical implications of these findings are that routine monitoring of serum potassium concentration may be necessary.
Although aldosterone suppression is reported to occur within a few days of heparin treatment, the time needed to develop hyperkalemia may be extremely variable among patients, depending on their clinical background. This observation underlines the potential risk associated with an unmonitored treatment for a period longer than that used in our study. But longer duration of heparin administration for chronic conditions needs careful monitoring. None of the patients had clinically relevant consequences. In conclusion, the short-term treatment with LMWH induces a significant increase in serum potassium level, but the related risk of clinically relevant hyperkalemia remains low.
The limitations of the study are that the confidence interval of various parameters in univariate and multivariate analysis is wide (i.e., difference between lower and higher value is more) and it is less than 1. So a large sample size more than 30 will actually predict the risk of hyperkalemia. A further study with larger sample size has to be undertaken. Serum creatinine is not a risk factor in multivariate analysis because some other factor is masking its effects in predicting Hyperkalemia. Hence CrCl is a better marker in establishing hyperkalemia.
CONCLUSIONS
LMWH-induced aldosterone suppression leading to hyperkalemia and hyponatremia (natriuresis) is more than heparin. This adverse effect needs to be better anticipated by clinicians. Serum potassium should be monitored periodically in patients on heparin or LMWH for five or more days, especially in high-risk patients for hyperkalemia.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Thomas CM, Thomas J, Smeeton F, Leatherdale BF. Heparin-induced hyperkalemia. Diabetes Res Clin Pract. 2008;80:e7–8. doi: 10.1016/j.diabres.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 2.Katzung BG, editor. 9th ed. New York: Mcgraw Hill Companies; 2004. Basic and Clinical Pharmacology; pp. 1007–14. [Google Scholar]
- 3.Gheno G, Cinetto L, Savarino C, Vellar S, Carraro M, Randon M. Variations of serum potassium level and risk of hyperkalemia in inpatients receiving low-molecular-weight heparin. Eur J Clin Pharmacol. 2003;59:373–7. doi: 10.1007/s00228-003-0626-y. [DOI] [PubMed] [Google Scholar]
- 4.Orlando MP, Dillon ME, O’Dell MW. Heparin-induced hyperkalemia confirmed by drug rechallenge. Am J Phys Med Rehabil. 2000;79:93–6. doi: 10.1097/00002060-200001000-00019. [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Martin G, Dıaz-Molinas MS, Martınez AM, Ortiz M. Heparin-induced hyperkalemia; prospective study. Int J Clin Pharmacol Ther Toxicol. 1991;29:446–50. [PubMed] [Google Scholar]
- 6.Edes TE. Heparin-induced hyperkalemia. Postgrad Med J. 1990;87:104–6. doi: 10.1080/00325481.1990.11704598. [DOI] [PubMed] [Google Scholar]
- 7.Oster JR, Singer I, Fishman LM. Heparin-induced aldosterone suppression and hyperkalemia. Am J Med. 1995;98:575–86. doi: 10.1016/s0002-9343(99)80017-5. [DOI] [PubMed] [Google Scholar]
- 8.Cailleux N, Moore N, Levesque H, Courtois H, Godin M. A low molecular weight heparin decreases plasma aldosterone in patients with primary hyperaldosteronism. Eur J Clin Pharmacol. 1992;43:185–7. doi: 10.1007/BF01740668. [DOI] [PubMed] [Google Scholar]
- 9.Abdel-Raheem MM, Potti A, Tadros S, Kola V, Hanehom D, Framan G, et al. Effect of low-molecular weight heparin on potassium homeostasis. Pathophysiol Haemost Thromb. 2002;32:107–10. doi: 10.1159/000065208. [DOI] [PubMed] [Google Scholar]
- 10.Indermitte J, Burkolter S, Drewe J, Krahenb uhl S, Hersberger KE. Risk Factors Associated with a High Velocity of the Development of Hyperkalaemia in Hospitalised Patients. Drug Saf. 2007;30:71–80. doi: 10.2165/00002018-200730010-00007. [DOI] [PubMed] [Google Scholar]
- 11.Wiggam MI, Beringer TR. Effect of low-molecular-weight heparin on serum concentrations of potassium. Lancet. 1997;350:292–3. doi: 10.1016/s0140-6736(05)62260-x. [DOI] [PubMed] [Google Scholar]


