Abstract
Light polymerizable tooth colored restorative materials are most widely preferred for advantages such as esthetics, improved physical properties and operator's control over the working time. Since the introduction of these light polymerizable restorative materials, there has been a concern about the depth of appropriate cure throughout the restoration. Photopolymerization of the composite is of fundamental importance because adequate polymerization is a crucial factor for optimization of the physical and mechanical properties and clinical results of the composite material. Inadequate polymerization results in greater deterioration at the margins of the restoration, decreased bond strength between the tooth and the restoration, greater cytotoxicity, and reduced hardness. Therefore, the dentist must use a light curing unit that delivers adequate and sufficient energy to optimize composite polymerization. Varying light intensity affects the degree of conversion of monomer to polymer and depth of cure.
Keywords: Light curing unit intensity, light polymerizable restorative materials photopolymerization
INTRODUCTION
In recent years the popularity of tooth colored restorative materials has led to a rapid increase in the use of resins. Composite resins, polyacid modified resin-based composites (compomer) and resin-modified glass ionomers (RMGIC) are most commonly used light polymerizable restorative materials. Composite resins are recommended for use mostly in permanent teeth whereas compomers and RMGIC are preferred in primary teeth and non-stress-bearing cavities in permanent teeth as well.[1,2] Light polymerizable restorative materials are most widely preferred due to advantages such as esthetics, improved physical properties and operator's control over the working time.[3–6]
Since the introduction of these light polymerizable restorative materials, there has been a concern about the appropiate depth of cure throughout the restoration. Moreover, the significant role of effective polymerization in long-term clinical success of resin restorations has been well-documented.[5]
Clinical studies related to the survival rate of direct resin composite restorations revealed 30-60 % of all restorations had been replaced within 3-8 years. The reasons were mainly due to secondary caries followed by discoloration, degradation, microleakage, wear or ditching at the margins.[7–9]
Studies revealed that inadequate polymerization can contribute to a variety of clinical conditions such as discoloration, pulpal irritation, post-operative sensitivity and eventual failure of the restoration.[6] Factors affecting the polymerization of the resins include those directly related to restorative material including shade, thickness during polymerization and composition of the material. Light intensity, wavelength, exposure duration, size, location and orientation of the tip of the source are factors related to the light curing units (LCU).[10,11]
In a composite restoration, photopolymerization is of fundamental importance because adequate polymerization is a crucial factor for optimization of the physical and mechanical properties and clinical results of the composite material. Inadequate polymerization results in greater deterioration at the margins of the restoration, decreased bond strength between the tooth and the restoration.[12] greater cytotoxicity[13–17] and reduced hardness.[14] Therefore, the dentist must use a LCU that delivers adequate and sufficient energy to optimize composite polymerization.[15,16] Varying light intensity affects the degree of conversion of monomer to polymer and depth of cure.
Four types of polymerization sources have been developed like quartz tungsten halogen (QTH) lamps, light emitting diodes (LED) units, plasma-arc lamps and argon-ion lasers.[16,17] Halogen lights and LED units are overwhelmingly applied in daily clinical practice.[18] Halogen lights, a low cost technology, have been the most frequent source employed for polymerization of composite resin materials.[19] Their broad emission spectrum allows the polymerization of all known resin composite materials available.[17] However, they have several drawbacks. Their efficiency in converting electronic energy into light is estimated to be low. Up to 70% is transformed to heat and only 10% is visible light, including the blue range desired for polymerization.[19] Therefore, filters are required to reduce heat energy transferred to the oral structures and provide further restriction of visible light into the narrower spectrum of photoinitiators.[17] Of the visible light, due to the use of cut-off filters, a further 90% is wasted. Therefore, the final blue light output is less than 1% of the total energy input.[17] Moreover, light filters degrade with time due to the high operating temperatures and proximity to the halogen bulb.[20]
Several studies have pointed out that many halogen units used by clinicians do not reach the minimum power output specified by the manufacturers.[18] A lack of maintenance, such as failure to check the LCUs irradiance or to replace the halogen bulb from time to time, maybe a cause for this.[19] The lifespan of a conventional QTH lamp ranges between 30 and 50 hours.[21] These shortcomings could result in inadequate curing which in turn could negatively affect the long-time success.
In 2001, with the objective of overcoming the limitations inherent to halogen lamps, the first LED curing units were introduced into the dental market[22] LEDs use a combination of two different doped semiconductors instead of a hot filament.[18–20,23,24] The spectral output of gallium nitride blue LED conveniently falls within the absorption spectrum of camphoroquinone.[16,17] Therefore, they do not require filters to produce blue light and they convert electricity into light more efficiently.[24] The advantages of the LEDs are they produce less heat therefore no cooling fan is required, they are smaller in size and cordless.[24] Moreover, LEDs can operate for thousands of hours with a constant light output in power and spectra.[21] Contrary to first generation LED curing lights, newer units deliver with an intensity power higher than 400 mW/cm2, allowing a reduction of the exposure time recommended by composite manufacturers.[22]
On an average, the LED light source is expected to perform for thousands of hours compared with the 30- to 50-hour performance or QTH bulbs. Degradation of bulbs and loss of reflectors caused by heat from the filament commonly seen in QTH lights does not apply to LED lights, because LEDs use gallium nitrate semiconductors as the source of luminescence. However, this long-term performance should not exempt LED lights from routine in-office evaluation.
An adequate polymerization of resin composites is essential for the ultimate success of the restorations. Depth of cure and microhardness testing have been widely used to assess the relative degree of cure of resins and thus, the efficiency of light sources .Most of the studies on composite resin curing, stress the importance of sufficient intensity output of curing lights.
In the process of polymerization, light intensity and light curing time are two important factors that impact the number of photons delivered to a specimen. In general, a light intensity of 400 mW/cm2 for 40 seconds is sufficient to polymerize composite of 2-mm thickness. Recently, light intensity modulation methods for the irradiation mode have been introduced with the expectation that they may reduce polymerization shrinkage. Unlike the conventional method (continuous and constant curing), these methods employ soft-start protocols such as step curing and ramp curing, or a pulse-delay curing procedure. However, in many cases, the results achieved with these light intensity modulation methods were not better than the conventional method.
Causes of variable light output from light cure units:
Internal factors
Units
Input
Battery
Filters
Connections
External factors
Distance from material
Tip
Cover/Sleeve
Contaminated material
The determination of the actual light intensity of polymerization lights is an important issue. Comprehensive tests conducted by the University of Mainz (Prof. Ernst) in dental practices have shown that many curing lights do not achieve the light intensities stipulated by the manufacturer. In extreme cases, the lights did not even achieve half of the specified power. Therefore, it is recommended that dentists check the light intensity of their polymerization lights at regular intervals. Radiometers (L.E.D, QTH) are useful for quick routine tests to check the light output of a curing light in the dental office.
Roberts and colleagues reported that the two radiometers (QTH and LED) Figure 1 may be used interchangeably for measuring the irradiance of QTH and LED lights. They also reported that the two radiometers give slightly different but correlated readings. In their study, readings from LED radiometers were slightly lower than readings of QTH radiometers. Irradiance values obtained from hand-held radiometers (QTH or LED) were significantly different from those obtained from a laboratory-grade power meter. In general, intensity outputs measured by handheld radiometers are relative and not absolute.
Figure 1.
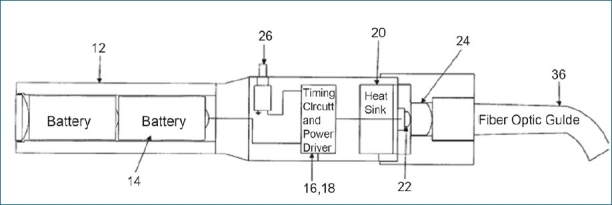
Various parts of LED
Also there are a number of factors with a direct effect on the power intensity measured by radiometers. These include
The size of the curing tip.
Composite resin build-up on the curing tip.
The temperature of the bulb in QTH units.
The orientation position of the curing tip to the radiometer.
The voltage regulation and
The reliability of the radiometer itself.
Handling of the LCU.
Studies have shown that the power intensity of curing lights is significantly reduced by the presence of composite resin build-up on the curing tip. Leonard and colleagues examined the reliability of several commercial radiometers. They reported that only 1 built-in radiometer with a 10.5-mm tip provided an accurate measurement of the irradiance value.
Barghi N, Berry T, Hatton C. Evaluated intensity output of curing lights in private dental offices[13] and concluded that 30% of the curing units had power densities <199 mW/cm2 which were inadequate for curing composite resin. The remaining lights displayed power densities between 200 and 349 mW/cm2 and were labeled adequate output for use with small increments of composite resin and increased curing time to ensure sufficient energy density.
CONCLUSIONS
After reviewing the above literature, every clinician will agree that one must check not only the intensity of the curing units but also other important factors like battery, filters, internal connections, cleanliness of the tip and sleeve periodically in order to avoid unwanted composite failure in our day-to-day clinical practice.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.McLean JW, Nicholson JW, Wilson AD. Proposed nomenclature of glass- ionomer dental cements and related materials. Quintessence Int. 1994;25:587–9. [PubMed] [Google Scholar]
- 2.Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: A review of the current literature. J Prosthet Dent. 1998;80:280–301. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- 3.David JR, Gomes OM, Gomes JC, Loguercio AD, Reis A. Effect of exposure time on curing efficiency of polymerizing units equipped with light-emitting diodes. J Oral Sci. 2007;49:19–24. doi: 10.2334/josnusd.49.19. [DOI] [PubMed] [Google Scholar]
- 4.Dietschi D, Marret N, Krejci I. Comparative efficiency of plasma and halogen light sources on composite microhardness in different curing conditions. Dent Mater. 2003;19:493–500. doi: 10.1016/s0109-5641(02)00095-7. [DOI] [PubMed] [Google Scholar]
- 5.Geurtsen W, Spahl W, Leyhausen G. Residual monomer/ additive release and variability in cytotoxicity of lightcuring glass-ionomer cements and compomers. J Dent Res. 1998;77:2012–9. doi: 10.1177/00220345980770121001. [DOI] [PubMed] [Google Scholar]
- 6.Geurtsen W, Leyhausen G, Garcia-Godoy F. Effect of storage media on the fluoride release and surface microhardness of four polacid modified composite resins (compomers) Dent Mater. 1999;15:1196–201. doi: 10.1016/s0109-5641(99)00034-2. [DOI] [PubMed] [Google Scholar]
- 7.Mjør IA, Toffenetti F. Placement and replacement of resin-based composite restorations in Italy. Oper Dent. 1992;17:82–5. [PubMed] [Google Scholar]
- 8.Mjør IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in Iceland. Oper Dent. 2002;27:117–23. [PubMed] [Google Scholar]
- 9.Heft MW, Gilbert GH, Dolan TA, Foerster U. Restoration fractures, cusp fractures and root fragments in a diverse sample of adults: 24-month incidence. J Am Den Assoc. 2000;131:1459–64. doi: 10.14219/jada.archive.2000.0057. [DOI] [PubMed] [Google Scholar]
- 10.Kwon YH, Kwon TY, Ong JL, Kim KH. Light polymerized compomers: Coefficient of thermal expansion and microhardness. J Prosthet Dent. 2002;88:396–401. doi: 10.1067/mpr.2002.128121. [DOI] [PubMed] [Google Scholar]
- 11.Nomoto R, Uchida K, Hirasawa T. Effect of light intensity on polymerization of light-cured composite resins. Dent Mater J. 1994;13:198–205. doi: 10.4012/dmj.13.198. [DOI] [PubMed] [Google Scholar]
- 12.Rueggeberg FA, Caughman WF, Curtis JW., Jr Effect of light intensity and exposure duration on cure of resin composite. Oper Dent. 1994;19:26–32. [PubMed] [Google Scholar]
- 13.Barghi N, Berry T, Hatton C. Evaluating intensity output of curing lights in private practice. J Am Dent Assoc. 1994;25:992–6. doi: 10.14219/jada.archive.1994.0204. [DOI] [PubMed] [Google Scholar]
- 14.Mouthaan T. Semiconductor Devices Explained: Using Active Simulation. Baffins Lane: Wiley; 2000. [Google Scholar]
- 15.Mills RW. Blue light emitting diodes-An alternative method of light curing? Br Dent J. 1995;178:169. doi: 10.1038/sj.bdj.4808693. [DOI] [PubMed] [Google Scholar]
- 16.Sze SM. Physics of semiconductor devices. New York: Wiley; 1981. [Google Scholar]
- 17.Stahl F, Ashworth SH, Jandt KD, Mills RW. Light-Emitting Diode (LED) Polymerisation of Dental Composites: Flexural Properties and Polymerisation Potential. Biomaterials. 2000;21:1379–85. doi: 10.1016/s0142-9612(00)00029-6. [DOI] [PubMed] [Google Scholar]
- 18.Hervás-García A, Martínez-Lozano MA, Cabanes-Vila J, Barjau-Escribano A, Fos-Galve P. Composite resins. A review of the materials and clinical indications. Med Oral Patol Oral Cir Bucal. 2006;11:215–20. [PubMed] [Google Scholar]
- 19.Mills RW, Uhl A, Blackwell GB, Jandt KD. High power light emitting diode (LED) arrays versus halogen light polymerization of oral biomaterials: Barcol hardness, compressive strength and radiometric properties. Biomaterials. 2002;23:2955–63. doi: 10.1016/s0142-9612(02)00024-8. [DOI] [PubMed] [Google Scholar]
- 20.Price RB, Felix CA, Andreou P. Knoop hardness of ten resin composites irradiated with high-power LED and quartz-tungsten-halogen lights. Biomaterials. 2005;26:2631–41. doi: 10.1016/j.biomaterials.2004.06.050. [DOI] [PubMed] [Google Scholar]
- 21.Yap AU, Soh MS. Curing efficacy of a new generation high-power LED amp. Oper Dent. 2005;30:758–63. [PubMed] [Google Scholar]
- 22.Miyazaki M, Hattori T, Ichiishi Y, Kondo M, Onose H, Moore BK. Evaluation of curing units used in private dental offices. Oper Dent. 1998;23:50–4. [PubMed] [Google Scholar]
- 23.Uhl A, Mills RW, Vowles RW, Jandt KD. Knoop hardness depth profiles and compressive strength of selected dental composites polymerized with halogen and LED light curing technologies. J Biomed Mater Res. 2002;60:729–38. doi: 10.1002/jbm.10390. [DOI] [PubMed] [Google Scholar]
- 24.Vandewalle KS, Roberts HW, Tiba A, Charlton DG. Thermal emission and curing efficiency of LED and halogen curing lights. Oper Dent. 2005;30:257–64. [PubMed] [Google Scholar]


