Abstract
Objective and background:
We evaluated the feasibility and effectiveness of transsphenoidal surgery for large and giant pituitary adenomas with suprasellar extensions as these tumors have been therapeutic challenge.
Subjects and Methods:
We retrospectively analyzed 50 cases with 56 surgeries in patients with pituitary adenomas that were surgically treated between January 2005 and January 2010 at Fujita Health University. Among those cases, 39 cases were large or giant pituitary adenomas including 11 cases of giant adenomas.
Results:
37 cases 41 approaches were transsphenoidal, 2 approaches were transcranial, and in 1 case transcranial approach following transsphenoidal surgery was performed. The most frequent preoperative symptoms were visual impairment and visual field defect (28 cases, 75.6%), and improvement of visual function after surgery was observed in 18 cases, 64%. As endocrinological results, among the 11 cases of functioning adenomas, improvement of endocrinological examination was observed in 10 cases, and normalization of the hormonal examination and complete remission was seen in 7 cases which was 64%.
Conclusions:
Transsphenoidal approach is safe and effective procedure even in large or giant pituitary adenomas, because it allows rapid and appropriate decompression of the optic nerves and chiasm with low morbidity rates. Transcranial approaches were indicated only in irregular shaped adenomas or eccentric extensions that could not be reached through the transsphenoidal route.
Keywords: pituitary adenoma, suprasellar extension, transsphenoidal surgery
Introduction
Pituitary adenomas account for 10 to 15% of all intracranial tumors and have characteristic endocrinological functions affected by either hypopituitarism or hypersecretion of certain hormones. The most definitive initial treatment of pituitary adenomas is surgical removal of the tumor by either the transsphenoidal or transcranial approach[1,2].
The transsphenoidal approach has become the preferred surgery for the excision of most of the pituitary adenomas, as compared with transcranial operations, transsphenoidal surgery causes less injury to the pituitary gland, and allows rapid recovery of pituitary endocrinological function and visual impairment. However, the surgical approach for adenomas with suprasellar extensions seems to remain controversial[2,3]. We evaluated the feasibility and effectiveness of transsphenoidal surgery of pituitary adenomas with suprasellar extensions, as these tumors are therapeutic challenge.
Subjects and Methods
We retrospectively analyzed 50 cases with 56 surgeries in patients with pituitary adenomas that were surgically treated between January 2005 and January 2010 at Fujita Health University. Diagnosis was confirmed by MRI scanning, and we evaluated the tumor size, suprasellar extensions, and cavernous sinus invasion using Knosp grading and compared between preoperative and postoperative state, and evaluated the improvement of the symptoms postoperatively mainly in visual symptoms. We also evaluated the endocrinological examination in serum hormonal test in anterior lobe of the pituitary gland. Among those cases, 39 cases were large or giant pituitary adenomas including 11 cases of giant adenomas, defined as those measuring at least 4cm in maximum diameter. (The definition of giant pituitary adenomas in the literature has not always been homogeneous, but in the most recent published series, the definition used was that pituitary adenomas with maximum diameter measured 40mm or more[3,5]). We defined macroadenomas that are more than 2cm in diameter as large adenomas. The follow up period was from 3 months to 5 years.
Results
Table 1 represents the results of clinical hormone secreting in patients whose tumors had suprasellar extensions and underwent surgical resection.
Table 1.
Results of tumor subtypes undergoing surgical resection
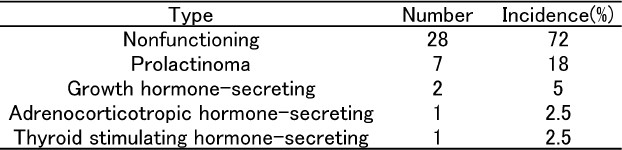
Non-functioning pituitary adenoma was the most frequent type (n=28, 72%), whereas prolactinoma numbered 7 (18%), growth hormone secreting adenoma numbered 2 (5%), and 1 case was ACTH secreting adenoma, and 1 case was TSH-secreting adenoma [Table 1]. There were 12 women and 27 men aged from 22 to 78 years old, with the mean age of 51.2 years old at the time of surgery. All the 11 giant adenomas showed cavernous sinus invasion and revealed to be Knosp grade 4.
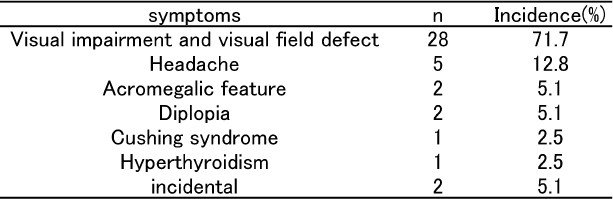
Preoperative symptoms are shown in Table 2. Visual impairment including visual field, visual acuity, or both is the most frequent symptom, which was present in 28 patients, 71.7%. Headache was present in 5 patients, 12.8% acromegalic feature was present in 2 patients, 5.1%, diplopia was present in 2 patients, 5.1%, Cushing syndrome was present in 1 patient, 2.5%, hyperthyroidism (palpitation) was present in 1 patient, 2.5%. 2 cases were incidentally found which was 5.1%.
Table 2.
Preoperative symptoms
As the surgical management, transsphenoidal approach was performed in 37 cases, 41 surgeries. And among the 41 transsphenoidal surgeries, mainly microscopic surgeries were performed in 40 surgeries, and in 1 case, single endoscopic endonasal transsphenoidal surgery was performed. Transcranial surgery was performed in 2 cases, since one of the 2 cases showed extreme extension to the anterior cranial fossa and unless we employ the extended transsphenoidal approach, it was impossible to remove, and we expect management of the cerebrospinal fluid leakage after surgery would be difficult. And in other 1 case which we performed craniotomy, the tumor extended to the third ventricle, and the preoperative initial diagnosis was craniopharyngioma, so interhemispheric approach was performed. In 1 case, transcranial surgery following transsphenoidal surgery was performed because suprasellar portion of the tumor was so irregulary shaped and so fibrous that the suprasellar tumor did not descend into the sella after the transsphenoidal surgery (Fig. 1).
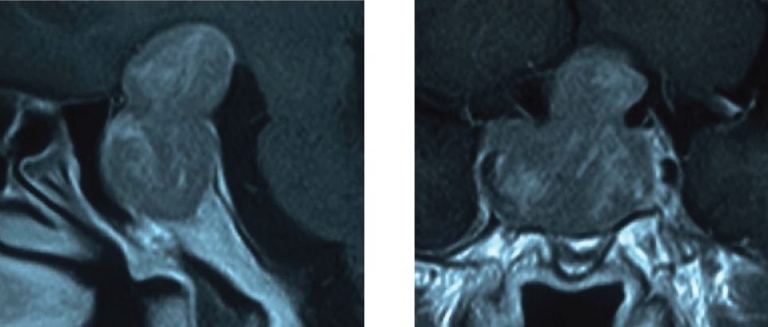
Fig. 1-a.
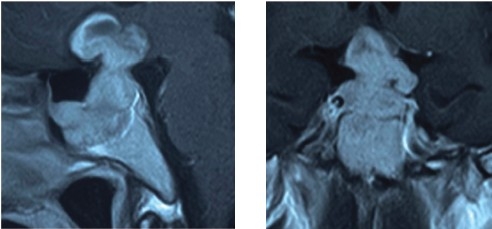
Preoperative MRI of the patient 1 reveals giant pituitary adenoma with irregular shaped suprasellar extension.
Visual results
18 cases among the 28 cases (68%) with visual impairment showed improvement of visual function after the surgery, that is 64% improvement rate.
Endocrinological results
10 cases among the 11 functioning adenomas showed improvement of serum hormonal test, that is 91 % improvement rate and normalization of the hormonal examination and complete remission was seen in 7 cases which was 64%.
Postoperative course
Reoperations were performed in 4 cases transsphenoidally, including 1 intentionally staged surgery after descending the suprasellar tumor into the sella. In other 3 cases, during the follow up period after the initial surgery, because of the worsening of the visual symptoms, after the suprasellar tumor fell into the sella, we performed the second surgery via transsphenoidal approach also.
Gamma knife treatment of cavernous sinus invasion was performed at least in 1 case.
As complications, transient diabetes insipidus in 13 cases (33.3%), cerebrospinal fluid leakage in 3 cases (7.7%), subarachnoid hemorrhage in 1 case (2.6%) were observed. No mortality was seen, and we did not experience any infection, any internal carotid artery injury.
Illustrative cases
Patient 1
A 35-year-old man with non-functioning adenoma presented visual impairment and bitemporal hemianopsia. MRI scan before the initial surgery revealed the giant pituitary adenoma with irregular shaped suprasellar extension (Fig. 1-a). At first, transsphenoidal surgery was performed, but the suprasellar portion of the tumor was impossible to remove as it was so firm, and the tumor did not fall into the sella, so we tried pterional craniotomy. Postoperatively, visual function improved (Fig. 1-b).
Fig. 1-b.
Posoperative MRI of the patient 1 reveals great mass reduction.
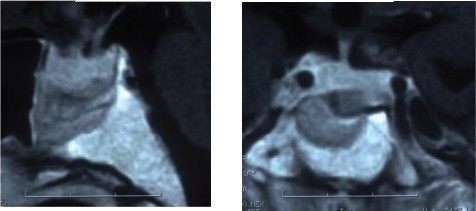
Patient 2
A 53-year-old man with non-functioning adenoma presented visual impairment and visual field defect. Preoperative MRI revealed dumbbell typed large pituitary adenoma with suprasellar extenson (Fig.2-a). For this case, endonasal endoscopic transsphenoidal surgery was performed (Fig.3). The tumor was partially soft, but partially fibrous and we needed to use scissor. Postoperative MRI revealed the great mass reduction and almost subtotal removal (Fig.2-b).
Fig.2-a.
Preoperative MRI of the patient 2 reveals large pituitary adenoma with dumbbell shaped suprasellar extension.
Fig.3.
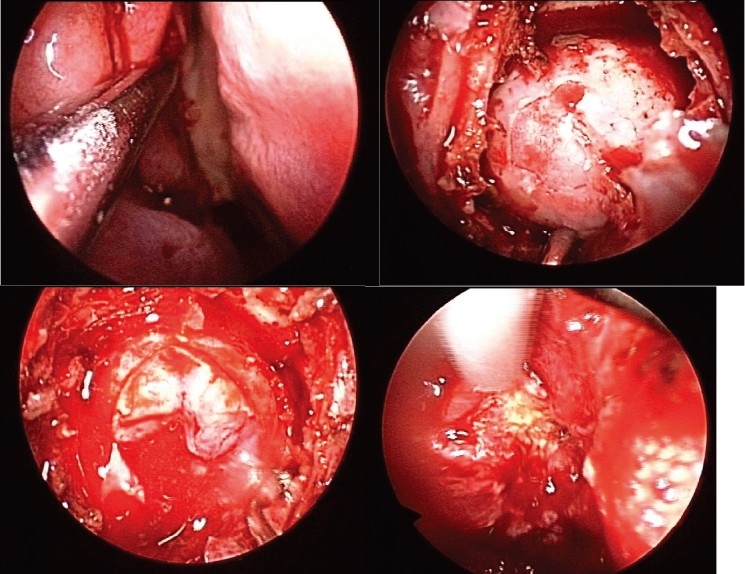
Surgical view of the patient 2. Endonasal endoscopic view. Approached via right nostril, As the dura mater and capsule was incised, soft tumor tissue appeared. Fibrous and firm part of the tumor was removed using a scissor.
Fig.2-b.
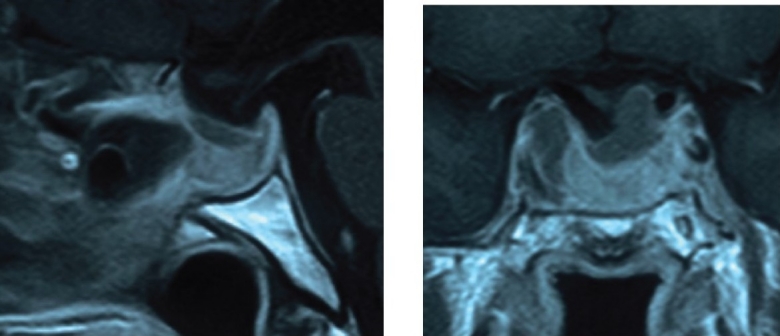
Postoperative MRI of the patient 2 reveals almost subtotal removal.
Discussion
Treatment of large or giant pituitary adenomas with suprasellar extensions has been controversial. At least 2 decades ago, at many centers, pituitary tumors with extrasellar extension and visual compromise were considered indications for a transfrontal approach[1].
Our result showed that 37 cases among the 39 large or giant adenomas (94.8%) were performed transsphenoidal approach. According to the article of Atul Goel et al., among the 118 cases of giant pituitary adenomas, 115 cases (97.5%) were operated on via transsphenoidal route[5]. Similar tendency was seen in some other articles, so the ratio of the transsphenoidal surgery of our series is similar to pervious reports[2,3,4,5].
In our series, 4 cases, after the first transsphenoidal surgery, suprasellar tumor descended into the sella, as the second surgery, transsphenoidal approach was performed, including intentionally staged surgery.
In 2 cases of our transcranial surgery, the reason why we performed craniotomy was, in one case, extreme extension to the anterior cranial fossa and in the other case, the preoperative initial diagnosis was craniopharyngioma because the tumor extended to the third ventricle. In 1 case, transcranial surgery following transsphenoidal surgery was performed because suprasellar portion of the tumor was so irregular shaped and so fibrous that the suprasellar tumor did not descend into the sella after the transsphenoidal surgery (Fig.1).
In the previous articles, although transsphenoidal surgery is recognized as the optimum technique for resecting pituitary adenomas within the sella turcica, the surgical approach for adenomas with suprasellar extensions remains controversial[2,6,7]. The majority of enclosed adenomas even with large suprasellar extension, provided that the tumor extends symmetrically in the midline above the sella turcica are indication for transsphenoidal approach and transcranial approach was indicated only irregular multinodular shaped tumor, or eccentric extensions into the subfrontal, temporal, or retrosellar (posterior fossa) regions that cannot be reached through the transsphenoidal route[2,3].
As we described, we performed staged (repeated) transsphenoidal surgery in 4 cases.
After the initial transsphenoidal surgery, if the suprasellar tumor descended into the sella, then the second step was also transsphenoidal surgery. Some other article described that suprasellar portion of the tumor may descend into the sella turcica as the intrasellar part of the tumor is being removed[4,7]. Besides, there are some reports that infusion of the saline or air via lumbar subarachnoid catheter or valsalva maneuver is sometimes helpful to obtain the descend of the suprasellar tumor into the sella[2,4]. However, approximately 5% of pituitary adenomas are reported to be fibrous, and the suprasellar component of the tumor can be dumbbell-shaped because of compression by the diaphragma sellae, the optic chiasm, or carotid artery[4]. These tumors might require transcranial removal or repeated, staged transsphenoidal removal. We have operated on such patients with intentionally staged transsphenoidal surgery or transcranial surgery as the second surgery.
Transsphenoidal approach is preferable to transcranial route, as it helps preserve normal pituitary function and allows recovery of visual function[1,3,5]. As a consequence, the transsphenoidal approach is the first choice in the surgical treatment of large or giant pituitary adenomas with suprasellar extensions[4,5,8].
In our series, gamma knife treatment for the residual tumor in the cavernous portion was performed at least in one case.
The role of radiation therapy or radiotherapies in preventing the late recurrence or control the residual tumor which was impossible to remove by surgery especially in the cavernous sinus invasion has been important[3].
In our institution, tumor remnant or recurrent tumor in the cavernous region is a problem because invasiveness into the cavernous sinus was significantly associated with incomplete removal of the pituitary tumor. We have tried not to remove aggressively especially in case tumor located lateral part of the cavernous sins. Instead, we treated such part of the tumor with gamma knife therapy, and it was helpful to prevent the growth and recurrence.
Conclusion
Transsphenoidal removal is a relatively safe and effective method, even in large and giant pituitary adenomas with suprasellar extensions in most of the cases, and only in cases of irregular, multinodular or eccentric extenson, craniotomy should be considered. Intentionally staged surgery and to observe for a while if we expect suprasellar tumor descend into the sella is also helpful. Sometimes adjuvant therapy such as radiotherapy should be considered if total resection was difficult. The goal of the treatment of such pituitary tumors are improvement of the visual, endocrinological and neurological symptoms with the lowest morbidity rates possible.
References
- 1.Black PMcL, Zervas NT, Candia G. Management of large pituitary adenomas by transsphenoidal surgery. Surg Neurol. 1988;29:443–7. doi: 10.1016/0090-3019(88)90138-3. [DOI] [PubMed] [Google Scholar]
- 2.Zhang X, Fei Z, Zhang Z, Liu W, Chen Y. Management of non- functioning pituitary adenomas with suprasellar extensions by transsphenoidal microsurgery. Surg Neurol. 1999;52:380–385. doi: 10.1016/s0090-3019(99)00120-2. [DOI] [PubMed] [Google Scholar]
- 3.Mortini P, Barzaghi R, Lossa M, Boari N, Giovanelli M. Surgical treatment of giant pituitary adenomas: Strategies and results in a series of 95 consecutive patients. Neurosurgery. 2007;60(6):993–1004. doi: 10.1227/01.NEU.0000255459.14764.BA. [DOI] [PubMed] [Google Scholar]
- 4.Saito K, Kuwayama A, Yamamoto N, Sugita K. The transsphenoidal removal of nonfunctioning pituitary adenoma with suprasellar extensions. The open sella method and intentionally staged operation. Neurosurgery. 1995;36:668–676. doi: 10.1227/00006123-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Goel A, Nadkarni T, Muzumdar D, Desai K, Phalke U, Sharma P. Giant pituitary tumors: A study based on surgical treatment of 118 cases. Surg Neurol. 2004;61:436–46. doi: 10.1016/j.surneu.2003.08.036. [DOI] [PubMed] [Google Scholar]
- 6.Symon L, Jakubowski J, Kendall B. Surgical treatment of giant pituitary adenomas. doi: 10.1136/jnnp.42.11.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakane T, Kuwayama A, Watanabe M, Kageyama N. Transsphenoidal approach to pituitary adenomas with suprasellar extension. Surg Neurol. 1981;16:225–229. [Google Scholar]
- 8.Hashimoto N, Handa H, Yamashita J, Yamagami T. Long term follow up of large or invasive pituitary adenomas. Surg Neurol. 1986;25:49–54. doi: 10.1016/0090-3019(86)90114-x. [DOI] [PubMed] [Google Scholar]


