Abstract
Object:
The aim is to evalute the outcome of posterior lumbar interbody fusion with autologous bone graft versus titanium Cages, BAK system (Bagby – Kuslich, Spine Tech, Inc. Minneapolis, MN) for low grade spondyloisthesis (Grade1,11). Interbody cages have been developed to replace tricortical Interbody grafts in posterior lumbar interbody fusion (PLIF) procedures. The cages provide immediate post operative stability and facilitate bony union with cancellous bone packed in the cage itself.
METHOD:
We Evaluated 50 consecutive patients in whom surgery was performed between June 2000 to June 2003 in the Main Alexandria University Hospital at EGYPT. Twenty five patients were operated using autologous bone graft and 25 patients using the BAK cages. The neuro–radiologic al work up consisted of; plain X – ray lumbosacral spine including dynamic films preoperative and postoperative follow up; C.T lumbosacral spine and MRI lumbosacral spine.
The surgery was performed at L4-5 level in 34 cases and at L5-S1 level in 16 cases. The median follow up was 15 months.
RESULTS:
Satisfactory fusion was obtained at all levels at a minimum one year follow – up. The fusion rate was 96% (24 patients) for the cage group and 80% (20 patients) for bone graft group however clinical improvement was 64% (16 patients) for those with bone graft group.
CONCLUSION:
A higher fusion rates and a better clinical outcome have been obtained by Instrumented PLIF with titanium cages that with bone graft.
Inderbody fusion cages help to stabilize spainal segment primarily by distracting them as well as by allowing bone ingrowth and fusion. The procedure is safe and effective with 96% fusion rate and 76% overall Satisfactory rate.
The use of cages help to distract the space between the vertebral bodies making the correction of the degree of spondylolisthesis easier.
Long term follow up revealed better fusion rate and better realignment and less resorption with cages than with bone grafts.
Introduction
Spondylolisthesis was first described by Kilian’ in1854 as a slowly developing displacement of a lumbar vertebra and it is now generally accepted that a defect in the pars interarticularis (spondylolysis) is the commonest cause of spondylolisthesis in the older children and young adult while degenerative spondylolisthesis is a condition of older people. Patients with spondylolisthesis may present with acute low back pain in the early stages of slipping. Chronic low back pain is due to ligamentous strain from instability at the level of the slip. Occasionally, pressure or traction on the nerve roots at the level of the defect causes sciatica but this is rare in minimal vertebral displacement. Even more infrequently an associated bulging disc may cause nerve pressure[3,4]
Several procedures have been described in the surgical management of spondylolisthesis where fusion with or without instrumentation is the most popular. There are several types of lumbar fusion and among that the most used are the following: posterior lumbar fusion (PLF), posterior lumbar interbody fusion (PLIF), anterior lumbar interbody fusion (ALIF), circumferential 360 fusion (front and back) and more recently, the transforaminal lumbar interbody fusion (TLIF)[5]
Interbody cages have been developed to replace tricortical interbody grafts in posterior lumbar interbody fusion (PLIF) procedures. Bone grafting was associated with several complications as graft resorption, failure of hardware and complications related to the donor site. Recently the threaded fusion cage has been recognized to provide solid fusion of the unstable segment in the central axis of the vertebral column. Furthermore, maintenance of the disc height is significantly increased with this technique.[10–12]
Superior fusion rates and clinical outcome have been obtained by titanium cages.
Aim of the Work
To evaluate the instrumental (by plate and screw) interbody fusion in low grade spondylolisthesis by interbody bony fusion in comparison with titanium cages.
The comparison regards the indications and the outcome between the two groups of patients.
Patients and Methods
Fifty patients with low grade lumbar spondylolisthesis, 22 males and 28 females, aged from 27 to 55 years
(Mean 36 years) were treated by posterior lumbar interbody fusion in the Main Alexandria University Hospital. In twenty five patients PLIF was performed using iliac graft and in the other 25 patients a BAK cage was inserted. Transpedicular screws and rods were added in 29 patients to enhance stabilization.
The presenting symptoms were chronic low back pain in all 50 patients, neurogenic intermittent claudication in 31 and sensorimotor dysfunction of the lower extremities in 36 patients. All patients were assessed radiologically by:
-
-
Plain X-ray lumbosacral spine: Anteroposterior view, lateral view, dynamic flexion and extension radiographs.
-
-
Computed Tomography (C.T) of the lumbosacral spine.
-
-
Magnetic Resonance Imaging (MRI) lumbosacral spine.
The disc height was measured pre, intra, and postoperatively as well as in the last follow up for each case. Preoperative lateral radiography showed grade I spondylolisthesis in 28 patients and grade 2 in 22 patients with a segmental motion in flexion and extension studies in all patients. Computed tomography (CT) disclosed various degrees of facet hypertrophy, disc herniation, and posterior spur formation. Magnetic resonance (MRI) of the lumbar spine demonstrated nerve root compression as well as canal stenosis. Spondylolisthesis was caused by facet defect in 35 cases and by spondylolysis in 15 patients. Twenty eight fusions were carried out at L4-L5, 18 at L5-S1, and 4 at L3-L4.
All patients were operated on at one level. The patients were placed in a prone position. Posterior midline incision was performed and the posterior elements were exposed to the origin of the transverse process. A wide posterior decompressive procedure was then performed removing the spinous processes, the laminae and facets to allow enough space for insertion of the cages and to avoid excessive thecal and root retraction. Bone that was derived from the posterior elements was used to fill the cages. The dura and traversing roots were freed enough to accommodate the tang retractor.
In spondylolisthesis, the slightly overhanging lip of the more posterior vertebral margin and attached annulus may by cut off with a small osteotome before driving tang instrument. On distracting the space, the tang will usually reduce the slippage by a few millimeters. The drilling depth was, either 24 mm (for 20 mm cage) or 28 mm (for a 24 mm cage).
The vertebral bodies are rather oval in shape and the squared – off ends of the cages must not project outside this oval, otherwise the posterolateral aspect of the cages may encroach on the neural foramen and irritate the ganglion, on the anterolateral aspect may slip the ventral rim of the vertebra to be in contact with a major retroperitoneal vessels.
An important rule in placement is to position the cages near the midline, in close proximity to each other. However, no cage should cross the midline; otherwise the second cage will be crowded too far lateral to the opposite side. Selection of the appropriate cage diameter according to the disc height is important to avoid over distraction. Cages screwed tightly into the space to create sufficient stability.
Finally the rod-screw system was screwed, tightened in compression. We confirmed that all cages were properly positioned by evaluating intraoperative lateral radiographs.
Cases operated using iliac bone graft for performing PLIF had the same steps as mentioned before with the exception of placement of the bone graft instead of the cages.
Postoperatively, hospitalization averaged 5 postoperative days. The patients were mobilized out of bed with a corsette a few days after surgery. Radiography was performed immediately postoperative and 3, 6, and 12 months postoperatively. CT was performed occasionally.
Fusion success was determined by:
-
-
Absence of motion on flexion-extension radiographic views.
-
-
The absence of any dark hole around a cage on anterior-posterior, and lateral View.
-
-
Continued presence of visible bone within each cage.
The mean follow up period was 9.5 months (range 3-24 months).
Outcome assessed as excellent, good, fair or poor. Excellent and Good outcomes were considered satisfactory; fair or poor outcomes were considered unsatisfactory.
Outcome was assessed according to the following criteria:
-
-
Radiologically demonstrated fusion
-
-
Clinical improvement of pain and level of activity
-
-
Active employment status at the time of follow-up.
Statistical analysis:
The Data was collected and entered into the personal computer. Statistical analysis was done using Statistical Package for Social Sciences (SPSS version-15) software. The statistical test used as follow:
Arthematic mean, standard deviation for categorized parameters, chi square test was used for numerical data. The level of significant was 0.05.
Results
The study consisted of 50 patients aged from 27 to 55 years (Mean 36 years). There were 22 males and 28 females. The mean follow up period was 9.5 months (range 3-24 months), there was no significant difference between the two studied groups regarding demographic data.
Twenty five patients underwent lumbar interbody fusion with threaded Titanium BAK Cages and the other 25 patients underwent the PLIF using iliac bone graft. All our patients suffered from low-grade spondylolisthesis.
-
-
Grade I spondylolisthesis in 28 patients (15 with cage and 13 with iliac graft).
-
-
Grade II spondylolisthesis in 22 patients (10 with cage and 12 with iliac bone graft).
-
-
As regards the level:
Spondylolisthesis was caused by lumbar degeneration in 35 cases and by spondylolysis in 15 patients. Transpedicular screws were added in 29 patients in whom enhanced stabilisation was required (obese patients, diabetic patients and heavy smokers) as well as the surgeon's preference. Thirteen patients operated with titanium cages had an added instrumentation while 16 patients with the iliac graft received a posterior instrumentation.
Clinical outcome: 30% of patients (32% with titanium cages and 28% with iliac bone graft) suffered low back pain for 2-3 months postoperatively. This pain was managed by using non steroidal anti-inflammatory drugs together with physiotherapy with a favorable response. At the time of follow-up visit, 80% of the patients operated with titanium cages were satisfied with the results of the surgery in comparison with 72% of those operated using a bone graft. The overall clinical outcome was 76% of patients with a satisfactory clinical outcome.
Table (1).
Patients characterization and out come in the two studied groups
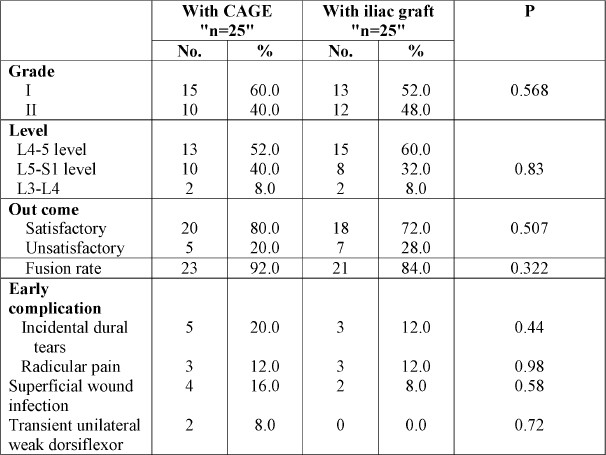
Figure (1).
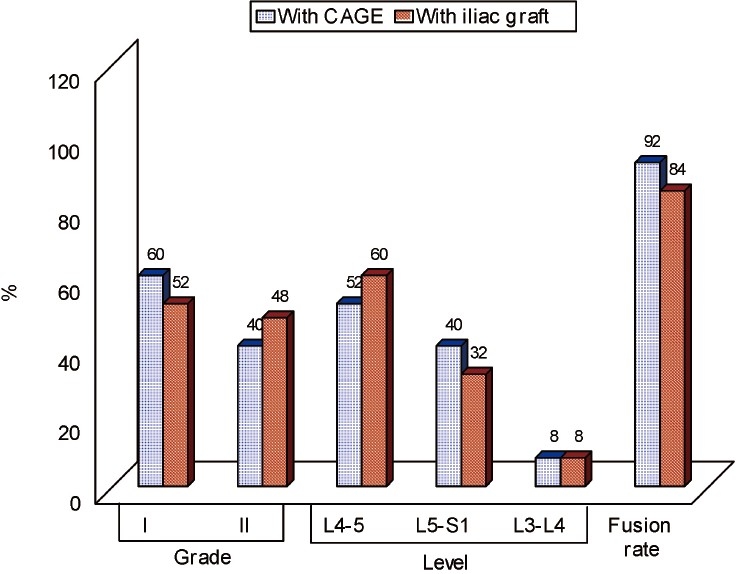
Patients characterization and out come in the two studied groups.
Fusion rate, of total of 25 patients operated for PLIF using titanium cages, 23 patients (92%) were radiographically shown to have good fusion while the rate of fusion for patients operated using iliac bone graft was 84% (21 cases). These data favors a better fusion rate with titanium cages than with iliac bone graft.
In this study, there have been no serious complications that persisted beyond 6 weeks postoperatively. Incidental dural tears occurred in 8 cases; 5 cases with the group treated with cages and three with those treated with a graft. All these cases passed without any clinical consequence. Two patients operated for PLIF using titanium cages showed a temporary weak unilateral dorsiflexor, one patient recovered with conservative management and the second required re-exploration and foraminotomy. Six patients developed radicular pain, three in each group. The radicular symptoms resolved spontaneously within one month. Superficial wound infections occurred more commonly with the titanium group (four out of six), but all of these cleared on antibiotics and routine care before the 6th week return visit.
DISCUSSION
Interbody fusion provides several theoretical advantages over other fusion techniques. From a biochemical point of view, the graft is placed at the weight bearing center of the spine where 80% of the axial load occurs. The disc height and the sagittal balance can be restored just as well as because optimal conditions are created for a higher fusion rate by placing the graft under compression with an extensive blood supply from the adjacent vertebral end plates. PLIF limits the extent of posterolateral soft tissue exposure, muscle stripping, and injury as well as allowing direct neural decompression. PLIF can be performed using either iliac bone graft or titanium cages however certain bone grafts tend to collapse and fracture. In addition the loss of disc space height after insertion of these bone grafts had been identified because the compressive strength of the grafts does not exceed the physiologic compressive loads of the spine
In cage fusion the amount of bone required for graft is significantly reduced. The cage design allows bone growth through and around it. When used in conjunction with a rigid posterior instrumentation system, the BAK system was effective in significantly increasing the initial stiffness of the fused segment above all other constructs[4,6,11,12,14].
Clinical outcome
A sound fusion is often believed to be a prerequisite for clinical success in patients with mechanical low back pain[11,15].
According to the authors of several reports, PLIF in which autogenous bone alone is used and even posterolateral fusion, achieve very similar results. The fusion rates ranges from 88 to 94% and clinical success ranges from 82% to 92%[3,16].
Molinari et al[17], reported in their series of 30 patients; who underwent an instrumented PLIF for treating low grade spondylolisthesis; a high rate of postoperative satisfaction (70% of their patients) with return to a full physical activity. In that series PLIF was performed using non threaded titanium cages together with supplemented posterior fixation for all the cases. This was coincides with our results where 76% of the patients had a satisfactory clinical outcome in the post operative period.
Jacobs et al[18] evaluated the clinical and radiological outcomes in treating low grade spondylolisthesis using different methods of fusion reported the following:
With PLF good or excellent clinical outcome varied from 60 to 98% and fusion rate varied from 81 to 100%. Circumferential fusion was compared to PLF, but no difference was found. With ALIF good or excellent clinical outcome varied from 85 to 94% and fusion rate varied from 47 to 90%.
With PLIF good or excellent clinical outcome was 45% and fusion rate was 80 and 95%.
In addition no benefit from additional instrumentation was found.
Fusion for low-grade isthmic spondylolisthesis has better outcomes than non-operative treatment. The current study could not identify the best surgical technique (PLF, PLIF, ALIF, instrumentation) to perform the fusion. However, instrumentation and/or decompression may play a beneficial role in the modern practice of reduction and fusion for low-grade isthmic spondylolisthesis, but there are no studies yet available to confirm this. The outcomes of fusion are generally good, but reports vary widely.
Figueiredo et al[19], reported a series of 34 cases operated for spondylolisthesis using TLIF with 80% satisfaction with the surgery. The main advantage of TLIF is that it allows the complete removal of the intervertebral disc through the vertebral foramen, decompression of the spinal canal and vertebral foramen with minimum risk of neural lesion, due to the access being lateral to the nerve roots.
Fusion rate
In the present study, the fusion rate was 92% in the PLIF with cages and 84% in the PLIF with iliac graft with overall fusion rate of 88%. This is close to the 90%, 89% reported by another independent series from Sweden who used the same technique but does not produce higher rate claimed by the innovators of the procedure.[6]
The need for supplement pedicle fixation remains unresolved issue. Brooke et al[7], have reported higher stabilization of the motion segment with the use of cages alone and no significant increase in stiffness when pedicle screws were added; other series, reported that cages supplemented by transpedicular screws fixation produce more sound fusion from a biochemical point of view.
Some authors reported that PLIF procedures without a supplemented posterior fixation are associated with graft retropulsion, graft collapse, and pseudarthrosis[13].
As well as Broodke et al, demonstrated that segmental internal fixation greatly enhances the stiffness of the spinal motion after a PLIF procedure[13].
Complication rate
Complications observed in this series may by classified into two groups: those are specifically related to implementation of the cages and those not related to cages.
30% of patients (32% with titanium cages and 28% with iliac bone graft) suffered from low back pain for 2-3 months postoperatively. This pain was managed using non steroidal anti-inflammatory drugs together with physiotherapy with a favorable response within 3 months post operative. Regarding the intraoperative complications there was a higher rate of dural tears with the group treated with titanium cages (5 cases) than those treated with iliac graft (3 cases). Inadvertent durotomy is a common complication sited for this procedure with incidence 16% in our study, coincide with other series ranging from 6-10%. This can be attributed to more required space for placement of the titanium cages that necessitates more dural traction. Infection was also more frequent in the titanium group than with the bone graft. The presence of foreign body like a cage was found to be associated with higher infection rate than with autogenous bone graft.
Radiculopathy had occurred in 12% of the patients in the present series following PLIF. This may be explained by extensive exposure of the exiting nerve root following facetectomy. Additionally we believe that neural retraction required for cage insertion is an important contributing factor in this complication. Extensive removal of facet joints, however may contribute to more epidural fibrosis[3,7] . Intraoperative fluoroscopy was done immediately before and after placement of all cages to confirm accurate trajectory and depth of implementation. There were two cases that had presented with weakness in the group operated with titanium cage. One case was explained by neuropraxia associated with nerve root traction and had improved with conservative management while the second required reintervention for decompression of the nerve root that had been found to be compressed by a bony spicule in the follow up CT scan of the lumbar spine.
Although a higher complication rate was found to be associated with PLIF using titanium cages, the majorities of these complications were minor complications and had been managed without any further sequelae.
Molinari et al[17], operated 30 patients for low grade spondylolisthesis using PLIF, there were 4 cases of dural tear, one case with unilateral transient lower extremity paresthesia, and one case with wound seroma requiring reoperation.
Similarly Jacobs et al[18], in a systematic review of the literature to evaluate the clinical and radiological outcomes in treating low grade spondylolisthesis using different methods of fusion had reported a wide variety of complications in 18 studies and included neurological complications, instrument failure, and infections.
Conclusion
PLIF is a safe and highly effective surgical method in treating low grade spondylolisthesis. The fusion rate was 88% and the overall satisfaction rate was 76%.
PLIF is associated with a high postoperative clinical satisfaction as well as a high fusion rate. The high rates of fusion associated with PLIF may be attributed in part to removal of the body end plates and exposure of the bleeding cancellous bony surfaces, reestablishment of anatomic intradiscal height and tension of the annulus and ligamentous structures around the disc spaces.
Posterior lumbar interbody fusion with Titanium Cages had been associated with a better clinical outcome and higher fusion rate than with iliac bone graft. Titanium cages provide several advantages:
(1)The Cage is placed in between the center of the vertebral bodies, which restricts segmental motion and reconstitutes the anterior column.
(2)The graft is placed under compression and receives blood supply from the adjoining vertebral bodies, so rapid re- growth of cancellous bone.
(3)Distraction of the interspace occurs, with restoration of posterior foraminal height and re-alignment of the vertebral body
So, The function of interbody fusion cages is to stabilize spinal segment primarily by distracting them as well as by allowing bone ingrowth and fusion. Threaded titanium cages provide adequate strength to ensure that no plastic deformation occurs within the maximum physiologic range. Dynamic testing of these implants has also shown that the fatigue performance of these implants occurs within normal daily physiologic loading. Stability testing has shown that these implants reduce the intervertebral motion and increase spinal stability.
Clinical outcomes using these titanium cages can be improved by adding of trans-pedicle screw fixation leading to increase rates of fusion and improving the sagittal contour of the lumbar spine.
References
- 1.Balderston RA, Brummet RS. Degenerative and isthmic spondylolisthesis: Evaluation and management. In: vaccaro AR, Betz RR, zeidman SM, editors. principlesand practice of spine surgery. Philadelphia: Mosby; 2005. pp. 527–38. [Google Scholar]
- 2.Agazzi S, Reverdin A, May D. Posterior lumbar interbody fusion with cages: an independent review of 71 case. Spine. 1999;91:186–92. doi: 10.3171/spi.1999.91.2.0186. [DOI] [PubMed] [Google Scholar]
- 3.Fraser RD. Interbody, posterior and combined lumbar fusions. Spine. 1995;20(24S):S167–77. doi: 10.1097/00007632-199512151-00016. [DOI] [PubMed] [Google Scholar]
- 4.Elias J, Simmons N, Kaptain G. Complications of posterior lumbar interbody fusion when using a titanium cage device. J Neurosurg [Spine] 2000;93:45–52. doi: 10.3171/spi.2000.93.1.0045. [DOI] [PubMed] [Google Scholar]
- 5.Lee CK, Kopacz KJ. Lumbosacral: Posterior Lumbar interbody fusion. In: Herkowitz HN, et al., editors. Rothman – Simeone The Spine. Philadelphia: Elsevier; 2006. pp. 350–60. [Google Scholar]
- 6.Bradke DS, Dick JC, Zeblick T, et al. Posterior lumbar interbody fusion: A biomechanical comparison, including a new threaded cage. Spine. 1997;22:26–31. doi: 10.1097/00007632-199701010-00005. [DOI] [PubMed] [Google Scholar]
- 7.Lehmann TR, Spratt KF, Tozzo JE, et al. Long – term follow up of lower lumbar fusion patients. Spine. 1987;12:97–104. doi: 10.1097/00007632-198703000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Wetzel FT, La Rocca H. The failed posterior lumbar interbody fusion. Spine. 1999;16:839–45. doi: 10.1097/00007632-199107000-00027. [DOI] [PubMed] [Google Scholar]
- 9.Ray CD. Threaded Titanium cages for lumbar interbody fusions. Spine. 1997;22:667–680. doi: 10.1097/00007632-199703150-00019. [DOI] [PubMed] [Google Scholar]
- 10.Dickman CA. Internal fixation and fusion of the lumbar spine using threaded interbody cages. BNI Quarterly. 1997;13:4–25. [Google Scholar]
- 11.Klara PM, Freidonk SA, Rezaimiri S. Comparison of lumbar interbody fusion techniques using Ray Threaded fusion cages and pedicle screw fixation systems. Neurosurgry Quarterly. 2003;13(1):20–9. [Google Scholar]
- 12.Kuslich SD, Ulstrom CL, Griffith SL, et al. The Bagby and Kuslich method of lumbar interbody fusion History ,techniques and 2 year follow –up results of aunited states prospective ,multicenter trial. Spine. 1998;23:1267–79. doi: 10.1097/00007632-199806010-00019. [DOI] [PubMed] [Google Scholar]
- 13.Burkus JK. Interbody fusion devices: biomechanics and clinical outcomes. In: Vaccaro AR, Betz RR, Zeidman SM, editors. Principles and practice of spine surgery. Philadelphia: Mosby; 2005. pp. 385–97. (P and P spine surgery page 388) [Google Scholar]
- 14.Bradley KW, Robert DF. Lumbar interbody cages. Spine. 1998;23:634–40. doi: 10.1097/00007632-199803010-00020. [DOI] [PubMed] [Google Scholar]
- 15.Rapoff AJ, Ghonayem Aj, Zdeblick TA. Biomechanical comparison of posterior lumbar interbody fusion cages. Spine. 1997;22:2375–79. doi: 10.1097/00007632-199710150-00010. [DOI] [PubMed] [Google Scholar]
- 16.Cagli S, Crawford NR, Dickman C, et al. Biomechanics of grade I degenerative lumbar spondylolisthesis.Part 2: Treatment with threaded cages /dowels and pedicle screws. J Neurosurg [spine1] 2001;94:51–60. doi: 10.3171/spi.2001.94.1.0051. h. [DOI] [PubMed] [Google Scholar]
- 17.(Molinari RW, Sloboda JF, Arrington EC. Low-grade isthmic spondylolisthesis treated with instrumented posterior lumbar interbody fusion in U.S. servicemen. J Spinal Disord Tech. 2005 Feb;18(Suppl):S24–9. doi: 10.1097/01.bsd.0000140197.07619.8b. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs WC, Vreeling A, De Kleuver M. Fusion for low-grade adult isthmic spondylolisthesis: a systematic review of the literature. Eur Spine J. 2006 Apr;15(4):391–402. doi: 10.1007/s00586-005-1021-4. Epub 2005 Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Figueiredo N, Martins JW, Arruda AA, Serra AR, Figueiredo MA, Diniz RC, Cavicchioli AA. TLIF--transforaminal lumbar interbody fusion. Arq Neuropsiquiatr. 2004 Sep;62(3B):815–20. doi: 10.1590/s0004-282x2004000500014. Epub 2004 Oct 5. [DOI] [PubMed] [Google Scholar]


