Abstract
BACKGROUND:
Incidental dural tears or durotomy (ID) during lumbar decompressive surgery is a relatively rare complication causing severe consequences. Their incidence varies widely among different authors (1-17%) and in general depends on the type and complexity of the spinal procedures performed.
With the present investigation the authors aim to evaluate the incidence of incidental durotomies during the different types of decompressive and reconstructive surgical procedures in the lumbar region, also indicating the most common reasons for incidental durotomies, treatment options and the early and remote outcome.
MATERIAL AND METHODS:
The records of 553 consecutive patients with different types of posterior and posterolateral decompressive and reconstructive procedures in the lumbar region are investigated retrospectively for the period January 2005 – march 2009.
RESULTS:
The overall incidence of the incidental durotomies in the investigated group is 12.66%. In the subgroups it varies depending on the specificity of the surgical procedures performed. The biggest is the number of IDs in the reoperative spinal surgery subgroup, followed by the subgroup of the patients who sustained spinal trauma, followed by those with degenerative spinal stenosis, tumors and lumbar disc herniations.
CONCLUSION:
IDs should be considered as a serious complication with a multitude of unwanted consequences for the patients. Prevention is the best way to treat the complications and disability that attend the unwanted dural tears. Knowing about the mechanisms and predisposing factors for that objectionable complication is a matter of utmost importance when planning and performing spinal surgical procedures.
Keywords: incidental durotomy (ID), unintentional dural tear, CSF leak, spinal surgery, complication
BACKGROUND
The incidental durotomy during lumbar decompressive surgery is a relatively rare complication that could cause severe complications. The incidence of incidental durotomies varies widely among authors (1-17%)[3,6–8,10,12,13,16] and in general depends on the type and the complexity of the spinal procedures[3,6,15,16]. The majority of authors relate the increased rate of dural tears with the increase of reoperation rate, respectively with epidural fibrosis, and with the advanced spinal degenerative changes with ossified yellow ligament among elderly people undergoing surgery[3,6,15,16]. The number and complexity of spinal procedures is increasing in the last decades, leading to a greater prevalence of dural tears[1]. One of the important intraoperative mechanisms other than direct laceration of the dura include excessive nerve root traction during the removal of big disc extrusions and implantation of spinal instrumentation. When dural injury occurs, in the majority of cases it is detected intraoperatively, and primary repair is mandatory with the established surgical techniques. Unfortunately not all dural tears can be recognized and repaired adequately primarily. Even with experienced surgeons, inadvertent, pin-hole-type durotomies may go unrecognized during surgery. If a defect goes undetected or is not properly closed, the patient is likely to experience a postural headache with a combination of the following symptoms: nausea, vomiting, pain or tightness in the neck or back, dizziness, diplopia due to VI cranial nerve paresis, photophobia, tinnitus, etc. Cerebrospinal fluid (CSF) leakage following dural tears can pose potentially serious problems such as CSF fistula formation, pseudomeningocele, meningitis, arachnoiditis and epidural abscess[1,3,10,12,15].
With the present investigation we aim to evaluate the incidence of the incidental durotomies during the different types of decompressive and reconstructive surgical procedures in the lumbar region, also to point the most common reasons for the incidental dural tears (durotomies), treatment options and its influence to the early and late outcome.
MATERIAL AND METHODS
The records of 553 consecutive patients with different types of posterior and posterolateral decompressive and reconstructive procedures in the lumbar region treated in our department within the period January 2005 – march 2009 were investigated retrospectively. In the investigated group 237 patients (114 men and 123 women) were operated for lumbar disc herniation, 143 patients (68 men and 75 women) were operated for degenerative lumbar spinal stenosis, 75 patients (52 men and 23 women) were treated for traumatic lumbar vertebral fractures, 38 patients (24 men and 14 women) had spinal tumors (8 primary and 30 metastatic) and 4 (1 man and 3 women) were operated for lumbar spondylolisthesis. (Tabl. 1) A subgroup of 56 (10,13%) patients (23 men and 33 women) are re-operated (up to 4 reoperations). Another subgroup of 111 patients, out of 553, were treated with complex surgical procedures that include decompression and spinal reconstructions. In the whole investigated group incidental durotomies (IDs) were found in 70 cases and in 59 of them the ID was diagnosed and treated during the initial surgery. The most important signs and symptoms, that were considered suggestive for IDs were persisting or postural headache, signs of meningeal irritation, neurological deficit, subcutaneous fluid collection or pseudomeningocele formation. MRI was used as a diagnostic tool for three patients with pseudomeningocele. (Fig. 1) One patient was diagnosed with CT myelography. The overall incidence of the clinically significant undetected intraoperative IDs was 0.2%. Seven patients were reoperated: 3 for closure of pseudomeningocele and one due to CSF leak through the surgical site.
Table 1.
Distribution of the patients and incidence of IDs respecting the indication for surgery.
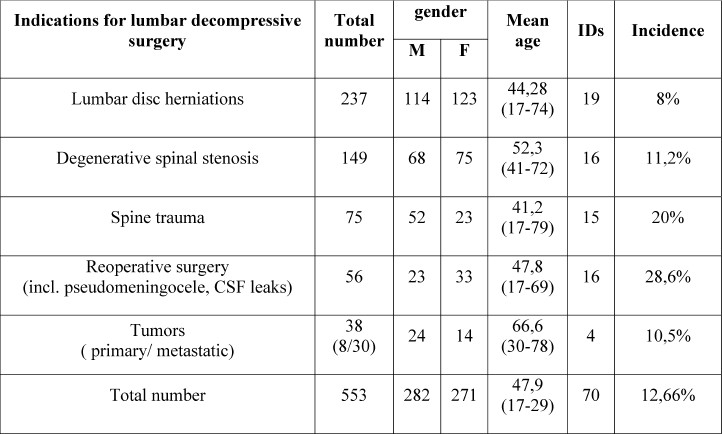
Fig. 1.
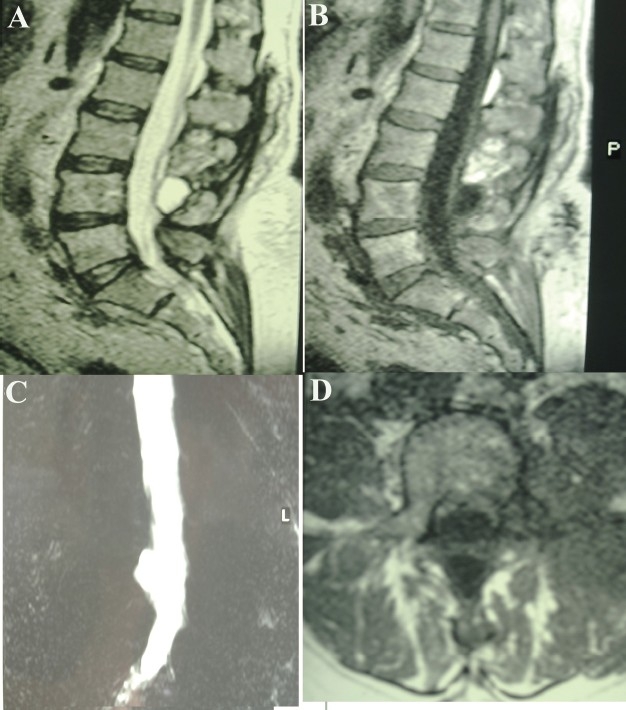
MRI demonstrating pseudomeningocele formed after ID of a patient operated for lumbar disk herniation.
If intaoperative ID occured and it was detected by the surgeon, the closure was achieved by application of running suture over the localized dural defect together with autologous free muscle or fat graft sutured over the defect. When suturing was technically difficult or impossible the graft was fixed with fibrin glue. At re-operations the existing CSF fistulas and pseudomeningoceles were excised and the dural defect was closed. The conservative management included application of continuous spinal drainage and bed rest for 4-7 days together with administration of broad-spectrum-antibiotics.
The early postoperative results among the patients with IDs were evaluated on the 1st, 6th and 24th month after the intervention. VAS (Visual Analog Scale) and ODI (Oswestry Disability Index) scales were used for the evaluation of 66 (93%) of the patients on the 1st month after the intervention, 50 (71.4%) patients were evaluated on the 6th month after the intervention and 42 (60%) patients on the 24th month after the intervention.
Statistical Analysis
The stastical significance was evaluated using Student-Fisher t test with value of P = 0.05.
RESULTS
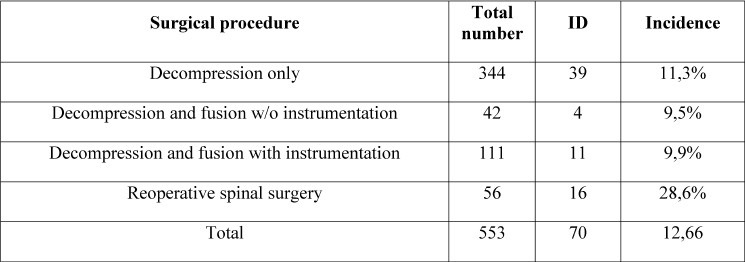
The overall incidence of the IDs in the investigated group was 12.66%. In the subgroups it varied depending on the specifics of the surgical procedures performed. The biggest number of IDs was in the subgroup of re-operations– 16 (28.6%) cases, followed by the group of spinal traumatic injury cases – 15(20%), the patients with degenerative spinal stenosis – 16 (11.2%), tumors – 4 (10.5%) and finally -lumbar disc herniations - 19(8%). ID was found in 11 (9.9%) out of 111 patients with reconstructive spinal procedures. (Tabl. 2) Patients with ID, especially those reoperated and those with pseudomeningocele had worse postoperative functional status if compared to the rest of the patients. One month follow up of 66 patients with ID showed higher VAS rates – mean 4 (4±2), while the patients without IDs were with VAS rates mean 2 (3±3). (_≤0,05). Similar were the results after 6 and 24months. The evaluation of the functional status of the patients with ODI scale rendered similar results – marked difference between the subgroups with and without IDs. After 2 years follow-up of 42 patients with IDs ODI was mean 32% (40±20). For the subgroup without IDs ODI was mean 25% (30±30). (P≤0,05)
Table 2.
Distribution of the patients and incidence of IDs respecting the surgical procedure.
DICUSSION
ID and CSF leakage is an undesirable but significant complication of lumbar decompressive surgery. The introduction and development of spinal instrumentation during the last decades, in association with the aggressive management of many spinal disorders raised the number of IDs. In an investigation Wang et al.[16] reported 88 (14%) IDs out of 641 consecutive patients who sustained surgical procedures in the lumbar region. Goodkin and Laska8 found 23 (16%) IDs out of 146 cases and reported that all 23 patients have residual complaints. Analyzing their results these authors claim that ID is a serious complication in spinal surgery. Investigating the postoperative complications in a large cohort of 18122 patients sustained different spinal procedures Deyo et al. 4 report that ID was with its lowest rate among young patients and microdiscectomy procedures, while the highest rate of IDs they found among the elderly patients and re-interventions. Similar results report also Morgan-Hough et al.[13]. They found 29 (5.5%) IDs out of 531 primary interventions (3 of them with pseudomeningocele), and 14.3% IDs among the patients with re-interventions respectively. In our series of 553 lumbar decompressive interventions, IDs were detected in 70 (12.66%) cases, 3 of them with pseudomeningocele. Our investigation showed the highest rate of IDs among the patients with re-interventions (28.6%) and spinal trauma (20%), while the lowest rate was found among the patients that underwent microdiscectomy procedures (8%) and spinal reconstructive interventions (9.9%).(Tabl. 2)
IDs could be detected during the initial surgery or during the postoperative period based on clinical signs and symptoms that suggest CSF leakage, or with MRI study[9]. Usually IDs followed by CSF leaks are produced by the surgeon himself directly causing dural tear while manipulating the dural sack or nerve roots. In respect of unwanted dural tears manipulations of the dura and nerve roots are extremely dangerous among the patients with advanced degenerative spinal stenosis and in re-operated patients. As the area of the dural defect is exposed to the surgeon the tear could be immediately repaired. Leaving behind small sharp bone particles during surgery is another mechanism that could contribute to small dural tears that could be left unattended during surgery, especially if the arachnoid membrane is intact and there are no CSF leaks. These small dural tears could be converted to open ones (with arachnoid membrane opened and CSF leakage) due to rapidly increased intradural pressure during the recovery from anesthesia, especially if it is very fast and violent.
The CSF leaks after IDs are most commonly detected during the initial surgical procedure. In these cases they are immediately sealed with suture, fibrin glue, autologous muscle or fascial graft, heterologous dural graft, etc.[1,2,6,15]. Ocasionally ID remains undetected and unattended by the surgeon and is detected after surgery. If a defect goes undetected or is not properly closed, the patient is likely to experience a postural headache, nausea, vomiting, pain or tightness in the neck or back, dizziness, diplopia due to VI cranial nerve paresis, photophobia, tinnitus, etc. Furthermore cerebrospinal fluid (CSF) leakage following dural tears can pose potentially serious complications such as CSF fistula formation, pseudomeningocele, meningitis, arachnoiditis and epidural abscess[1,3,4,7,10,11,13,15]. Though rarely, complicated CSF leaks could be lethal.[4]
Many authors describe different operative and nonoperative methods for the treatment of unattended ID detected after the surgery. Unfortunately there are no comparative randomized clinical trials demonstrating the advantages of one or another approach to the problem.[3,15] Some of the authors prefer immediate reoperation once CSF leakage is detected while others initially start with conservative management. A widely used conservative method for CSF leakage treatment is spinal drainage and bed rest for 4-7 days. Another method is the “blood patch” - injection of 10-20ml autologous blood into the epidural space at the site of the dural puncture[1,10,15]. However all of the authors consider the prevention of IDs as a matter of utmost importance when planning and performing spinal surgical procedures.
There are many studies that analyze early and late postoperative results among patients with IDs. Several authors report that patients do not have residual complaints attributable to IDs if they are detected and closed during the initial surgery[3,5,11,16]. Nevertheless in a long 10 years follow-up of a large goup Saxler et al.[15] report that patients with IDs have worse clinical results, namely functional restrictions and reduced working capacity, if compared with the patients without IDs. Furthermore the patients with IDs have increased tendency for reoperations. Though our investigation spans the close postoperative results within 2 years after surgery, the analysis of our results supports the aforementioned conclusions.
CONCLUSION
ID should be considered as a serious complication with a multitude of unwanted consequences for the patients. Prevention is the best way to treat the complications and disability that relates to inadvertent dural tears. Knowing about the mechanisms and predisposing factors for that serious complication is a matter of utmost importance when planning and performing spinal surgical procedures.
References
- 1.Bosacco SJ, Gardner MJ, Guille JT. Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin.Orthop.Relat Res. 2001:238–47. doi: 10.1097/00003086-200108000-00033. [DOI] [PubMed] [Google Scholar]
- 2.Cain JE, Jr, Lauerman WC, Rosenthal HG, et al. The histomorphologic sequence of dural repair. Observations in the canine model. Spine. 1991;16:S319–S323. [PubMed] [Google Scholar]
- 3.Cammisa FP, Jr, Girardi FP, Sangani PK, et al. Incidental durotomy in spine surgery. Spine. 2000;25:2663–7. doi: 10.1097/00007632-200010150-00019. [DOI] [PubMed] [Google Scholar]
- 4.Deyo RA, Cherkin DC, Loeser JD. Morbbidity and mortality in associations with operations on the lumbar spine: the influence of age, diagnosis, and procedure. J Bone Joint Surg. Am. 1992;74:536–43. [PubMed] [Google Scholar]
- 5.Eismont FJ, Wiesel SW, Rothman RH. Treatment of dural tears associated with spinal surgery. J. Bone Joint Surg.Am. 1981;63:1132–6. [PubMed] [Google Scholar]
- 6.Epstein NE. The frequency and etiology of intraoperative dural tears in 110 predominantly geriatric patients undergoing multilevel laminectomy with noninstrumented fusions. J.Spinal Disord.Tech. 2007;20:380–6. doi: 10.1097/BSD.0b013e31802dabd2. [DOI] [PubMed] [Google Scholar]
- 7.Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine. 1996;21:626–33. doi: 10.1097/00007632-199603010-00017. [DOI] [PubMed] [Google Scholar]
- 8.Goodkin R, Laska LL. Unintended “incidental” durotomy during surgery of the lumbar spine: medicolegal implications. Surg.Neurol. 1995;43:4–12. doi: 10.1016/0090-3019(95)80031-b. [DOI] [PubMed] [Google Scholar]
- 9.Gundry CR, Fritts HM. Magnetic resonance imaging of the musculoskeletal system: the spine. Clin.Orthop.Relat Res. 1998:262–78. [PubMed] [Google Scholar]
- 10.Hodges SD, Humphreys SC, Eck JC, et al. Management of incidental durotomy without mandatory bed rest.A retrospective review of 20 cases. Spine. 1999;24:2062–4. doi: 10.1097/00007632-199910010-00017. [DOI] [PubMed] [Google Scholar]
- 11.Jones AA, Stambough JL, Balderston RA, et al. Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine. 1989;14:443–6. doi: 10.1097/00007632-198904000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Le AX, Rogers DE, Dawson EG, et al. Unrecognized durotomy after lumbar discectomy: a report of four cases associated with the use of ADCON-L. Spine. 2001;26:115–7. doi: 10.1097/00007632-200101010-00020. [DOI] [PubMed] [Google Scholar]
- 13.Morgan-Hough CV, Jones PW, Eisenstein SM. Primary and revision lumbar discectomy.A 16-year review from one centre. J.Bone Joint Surg.Br. 2003;85:871–4. [PubMed] [Google Scholar]
- 14.Ragab AA, Fye MA, Bohlman HH. Surgery of the lumbar spine for spinal stenosis in 118 patients 70 years of age or older. Spine. 2003;28:348–53. doi: 10.1097/01.BRS.0000048494.66599.DF. [DOI] [PubMed] [Google Scholar]
- 15.Saxler G, Kramer J, Barden B, et al. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine. 2005;30:2298–302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 16.Wang JC, Bohlman HH, Riew KD. Dural tears secondary to operations on the lumbar spine.Management and results after a two-year-minimum follow-up of eighty-eight patients. J.Bone Joint Surg.Am. 1998;80:1728–32. doi: 10.2106/00004623-199812000-00002. [DOI] [PubMed] [Google Scholar]


