Abstract
Pancreatic islet β-cells produce large amounts of γ-aminobutyric acid (GABA), which is co-released with insulin. GABA inhibits glucagon secretion by hyperpolarizing α-cells via type-A GABA receptors (GABAARs). We and others recently reported that islet β-cells also express GABAARs and that activation of GABAARs increases insulin release. Here we investigate the effects of insulin on the GABA-GABAAR system in the pancreatic INS-1 cells using perforated-patch recording. The results showed that GABA produces a rapid inward current and depolarizes INS-1 cells. However, pre-treatment of the cell with regular insulin (1 µM) suppressed the GABA-induced current (IGABA) by 43%. Zinc-free insulin also suppressed IGABA to the same extent of inhibition by regular insulin. The inhibition of IGABA occurs within 30 seconds after application of insulin. The insulin-induced inhibition of IGABA persisted in the presence of PI3-kinase inhibitor, but was abolished upon inhibition of ERK, indicating that insulin suppresses GABAARs through a mechanism that involves ERK activation. Radioimmunoassay revealed that the secretion of C-peptide was enhanced by GABA, which was blocked by pre-incubating the cells with picrotoxin (50 µM, p<0.01) and insulin (1 µM, p<0.01), respectively. Together, these data suggest that autocrine GABA, via activation of GABAARs, depolarizes the pancreatic β-cells and enhances insulin secretion. On the other hand, insulin down-regulates GABA-GABAAR signaling presenting a feedback mechanism for fine-tuning β-cell secretion.
Introduction
Gamma-aminobutyric acid (GABA) is a major neurotransmitter in the central nervous system (CNS), where GABA produces fast inhibition in mature neurons primarily by activation of A-type GABA receptor (GABAAR), a hetero-pentameric Cl- channel [1]. A large amount of GABA is also produced in the pancreatic islet [2], where it exists at the highest concentration outside of the CNS [3]. Pancreatic GABA is primarily produced by the β-cell [4], in which GABA is stored in synaptic-like microvesicles that are distinct from insulin-containing large-dense core vesicles (LDCVs) [5]. However, recent evidence indicates that GABA is co-localized with insulin in LDCVs in human islets and that the release of GABA from the β-cells is glucose-dependent [6]. The release of GABA from β-cells is “tonic” [7], [8], yet the amount of released GABA is regulated by the metabolic state of β-cells [9].
In the pancreatic islet, GABA released from β-cells plays a critical role in the regulation of glucagon secretion from α-cells. Specifically, GABA activates GABAARs in α-cells, sequentially leading to an influx of Cl- and membrane hyperpolarization, and hence an inhibition of glucagon secretion. The GABAAR-mediated hyperpolarization of α-cells represents a physiological mechanism for glucose-induced suppression of glucagon release because blockade of GABAAR diminishes the inhibitory effect of high glucose on glucagon secretion in isolated rat [10] or mouse [11] islets. In relation to this notion, we have recently demonstrated that insulin suppresses glucagon secretion by enhancing intra-islet GABA-GABAAR signaling through translocation of GABAAR from an intracellular pool to the cell surface of α-cells [12].
Studies, including ours, have demonstrated that GABAARs are also expressed in the primary islet β-cells [12], [13] and insulin-secreting clonal β-cell lines [14], [15]. Unlike in mature neurons and α-cells, stimulation of GABAARs in β-cells induces membrane depolarization, enhancing insulin secretion in the presence of physiological concentrations of glucose [6], [15]. Consistent with the notion that the autocrine insulin is essential for β-cell function [16], [17], we recently demonstrated that GABA, in cooperation with insulin, enhances the proliferation and survival of the β-cells through activation of the PI3-K/Akt pathway. Remarkably, GABA promotes β-cell regeneration and reverses diabetes in mouse models [18]. In the present study, we found that insulin negatively regulates GABAAR function and inhibits GABA-induced β-cell secretion. Our results demonstrated a feedback mechanism that fine-tunes β-cell secretion.
Materials and Methods
Cell culture
Rat insulinoma INS-1 cells (passage 50–65) were maintained in RPMI 1640 medium (Invitrogen, Burlington, ON, Canada) containing fetal bovine serum (10% v/v), 100 Units/ml penicillin G sodium, 100 µg/ml streptomycin sulphate, 55 mg/500 ml sodium pyruvate, 1.14 g/500 ml HEPES, and 1.7 µl/500 ml β-mercaptoethanol at 37°C in an atmosphere of humidified air (95%) and CO2 (5%). Four hours before being used for patch-clamp recordings, INS-1 cells were glucose-starved in serum-free RPMI 1640 medium that contained 1.4 mM glucose.
Electrophysiology
For electrophysiological recordings, cells were bathed in the standard extracellular solution (ECS) containing (in mmol/l) 145 NaCl, 1.3 CaCl2, 5.4 KCl, 25 HEPES and 1.4 glucose (pH 7.4, 320–340 mOsm), and the ECS was maintained at 30°C. Patch-clamp recordings were performed using an Axopatch-1D amplifier (Axon Instruments, Foster City, CA, USA). Electrodes (1.8–2.3 MΩ) were constructed from thin-walled glass (1.5 mm diameter, World Precision Instruments, Sarasota FL, USA) using a two-stage puller (PP-830; Narshige, East Meadow NY, USA). The standard intracellular solution (ICS) consisted of (in mmol/l) 150 KCl, 10 KOH, 10 HEPES, 2 MgCl2 and 1 CaCl2 (ATP-free). The pore-forming agent gramicidin (60 mg/ml, Sigma-Aldrich Corp., Buchs, Switzerland) [19] was included in the ICS to perforate the membrane patch of the recorded cell. Under voltage-clamp mode, the membrane perforation was observed as a constant decrease in serial resistance after the electrode seal. In most of the recordings, the resistance declined to a value ranging from 28 to 301MΩ within 5–15 min after the seal, and then stabilized for 45–80 min. All perforated patch recordings began when the serial resistance had attained values below 30 MΩ. To monitor a possible formation of whole-cell configuration, a testing voltage-ramp (a gradual voltage-change from -100 to 100 mV in 1.5 s) was applied to the cell at the start of the recording. With this testing protocol, a sigmoid-shaped current-voltage (I–V) curve was seen under stable perforated patch recordings, whereas a large linear I–V relationship appeared after whole-cell configuration due to the activation of KATP channels by dilution of the cytosolic ATP. The endogenous membrane potential of INS-1 cells was about −60 mV [20]. Thus, INS-1 cells were voltage-clamped at −60 mV while under constant perfusion by fresh ECS. Patch-clamp recording was performed under voltage- or current-clamp mode. Via a computer-controlled multi-barreled perfusion system (SF-77Bl Warner Instruments, Hamden, CT, USA), 30 µM GABA [the EC50 of GABA in INS-1 cell is 22.3 µM [15]] was briefly (6 s) applied to the patched cells in two-minute intervals. After four stable recordings of GABA-induced current (IGABA), insulin was added to the standard ECS. All electrical signals were digitized, filtered (30 kHz), and acquired on-line using the program Clampex and analysed off-line using the program Clampfit 9 (Axon Instruments).
Measurement of intracellular calcium levels
Cells cultured in 96-well plates were loaded with 5 µM Fluo-3 AM (Molecular Probes, Eugene, OR, USA) for 2 hours in Locke's Buffer. Cells were then treated with GABA (30 µM), or 5 mM KCl as positive control. Changes in relative fluorescence units (RFU) were monitored with the Fluoroskan Ascent FL fluorescent plate reader equipped with a micro-injection syringe pump (Labsystems, Helsinki, Finland), based on the method provided by the manufacturer (Molecular Probes and Labsystems Fluo-3 AM Application Note).
Plasmids transfection
Dominant negative Akt (DN-Akt) vector was constructed as described previously [12], Green fluorescent protein (GFP)-expressing vector (Invitrogen) was used as an indicator of transfection. INS-1 cells transfected with or without relevant plasmids using Lipofectamine™ 2000 (Invitrogen, 24 hrs) according to manufacture's instruction.
Western blot analysis
Cells were serum-starved (16 hrs) and treated with or without insulin (100 nM) for 10 min, or in the presence of PI3-K inhibitor wortmannin (100 nM) or MEK/ERK inhibitor PD98059 (20 µM). Cells were lysed in RIPA lysis buffer containing the protease inhibitors phenylmethylsulphonylfluoride (PMSF) (1 mol/l) and EDTA (1 mol/l), Na3VO4 (1 mol/l), and NaF (1 mol/l). Protein of 25 µg was resolved by SDS-PAGE, transferred to nitrocellulose membranes and probed by anti-Akt and anti-phospho-Akt, or anti-ERK1/2 and anti-phospho-ERK1/2 (1∶1,000, Cell Signaling) as described previously [12] .
Insulin secretion
INS-1 cells were plated in 24-well plates with a density of 2.5×105 cells/well in RPMI 1640 medium containing 10% FBS. The following day, the medium was replaced with fresh KRB buffer (containing, in mmol/l, 115 NaCl, 5 KCl, 24 NaHCO3, 2.5 CaCl2, 1 MgCl2, 10 HEPES, 1.4 glucose, and 0.1% BSA) for 60 min. The cells were then treated with 1.4 or 11.1 mM glucose in KRB buffer for 2 h, in the presence or absence of GABA (30 µM). To determine the effects of insulin and/or GABA on the INS-1 cell secretion, in some parallel assays, cells were pre-treated with insulin (Novolin Toronto, Novo Nordisk, 1 µM) or picrotoxin (50 µM) for 15 min prior to GABA treatment during the secretion assay. The insulin levels in conditioned KRB buffer were evaluated by measuring C-peptide using a rat C-peptide RIA kit (Linco Research, St. Louis, MO, USA), according to the manufacturer's instructions.
Confocal Imaging
INS-1 cells were grown on poly-D-lysine (Sigma)-coated 8-well chamber slides (BD Falcon). Serum-starved cells were pre-treated with or without wortmannin (100 nM, 15 min) and incubated with or without insulin (1 µM) for 15 min). Cells were fixed with 4% paraformaldehyde and blocked with 2% BSA in PBS containing 0.1% Triton X-100 at room temperature for 1 hour. The cells were then incubated with monoclonal mouse anti-GABAAR β2/3 subunit (UBI 1∶100) and Cy3-conjugated anti-mouse IgG (Jackson Labs, 1∶500), consecutively. The images were captured using a Leica TCS 4D laser confocal fluorescence microscope.
Statistical Analysis
IGABA is expressed as mean current normalized to the current amplitude obtained immediately preceding insulin treatment (in all cases the fourth sweep in the series of same-cell current recordings) ± SEM. All data were presented as mean ± SEM. Statistical analysis was performed using unpaired or paired Student's t-test where appropriate. A p-value<0.05 was considered as significant. Statistical analyses were performed using SigmaPlot 2002 from SPSS Inc. (Chicago, IL, USA) and Microsoft Excel from Microsoft Corp. (Redmond, WA, USA).
Results
GABA induces membrane depolarization and increases intracellular Ca2+ levels in INS-1 cells
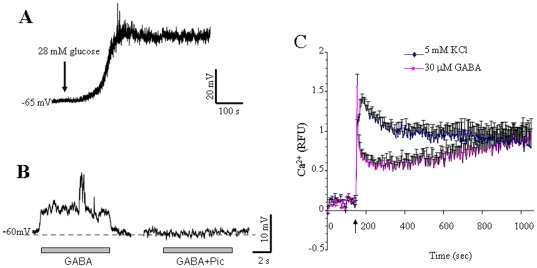
As previously demonstrated [20], under current-clamp conditions INS-1 cells displayed a quiescent membrane potential around −60 mV when ECS contained 1.4 mM glucose ( Figure 1A ). Perfusion of the cell with ECS containing 28 mM glucose caused a gradual and sustained depolarization. In some cases, bursts of action potentials were superimposed on the glucose-induced depolarization ( Figure 1A ). Under the same recording conditions, perfusion of GABA induced a fast membrane depolarization in the INS-1 cell ( Figure 1B ). The GABA-induced depolarization was completely blocked by GABAAR antagonist picrotoxin ( Figure 1B ) or largely attenuated by bicuculline (not shown), consistent with our previous findings, and those of others in the same cell line or isolated human islet beta β-cells [6], [18]. These results suggest that GABA, via activation of GABAAR, induces membrane potential depolarization in pancreatic INS-1 cells.
Figure 1. GABA depolarizes membrane potential and increases intracellular Ca2+ in INS-1 cells.
(A) Perfusion of ECS containing 28 mM glucose induces a gradual and sustained depolarization of the membrane potential (Vm) (n = 5). (B) GABA induces a rapid and GABAAR inhibition-sensitive depolarization of Vm under the current-clamp conditions at 1.4 mM glucose (n = 5). (C) Cells cultured in 96-well plates pre-loaded with Fluo-3 AM were treated with GABA (30 µM), or 5 mM KCl as positive control. Changes in relative fluorescence units (RFU) were monitored with a fluorescent plate reader. Data are Mean±SE, n = 6.
We then performed intracellular Ca2+ measurements to determine if GABA-induced membrane depolarization increases intracellular Ca2+ levels in INS-1 cells. As shown in Figure 1C , GABA (30 µM) evoked a steep rise in intracellular Ca2+ concentrations, which declines and then persists at a stable level during the course of the 20 to 30 min recording period. These results indicate that GABA induces membrane depolarization that is associated with increased intracellular Ca2+ in a population of pancreatic β-cells.
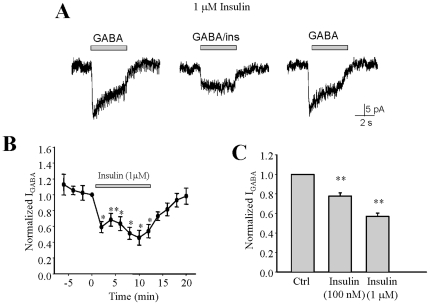
Insulin inhibits IGABA in INS-1 cells
Under voltage-clamp mode, perfusion of GABA evoked typical bicuculline-sensitive GABA current ( Figure 2A ). We next determined the effect of insulin on GABA-induced current (IGABA). Treatment of INS-1 cells with insulin (100 nM) significantly decreased IGABA by 22% (P<0.05, n = 8). The insulin-induced suppression of IGABA was more prominent when the insulin concentration was increased, for instance a reduction of 43% in IGABA was achieved with 1 µM insulin ( Figure 2A, 2B p<0.05, n = 5). Thus, insulin-induced suppression of IGABA was dose-dependent ( Figure 2C ).
Figure 2. GABA-evoked currents (IGABA) is inhibited by insulin in INS-1 cells.
GABA-evoked inward current was measured by means of a computer-controlled multi-barrelled perfusion system, in two-minute intervals, under voltage-clamp conditions. Representative traces of GABA-evoked currents in the absence and presence of insulin (100 nM, (A), 1 µM, (B)) in the same INS-1 cell. A' and B' represents the average of IGABA from separated experiments. (C) Normalized average IGABA during the course of experiment (control = average of first 4 IGABA, insulin = average of IGABA in the presence insulin at indicated concentrations). Data were mean ± SE. *p<0.05 ** p<0.01, n = 6.
Zinc-free insulin inhibits IGABA in INS-1 cells
Clinically-used insulin contains zinc [21] and zinc inhibits IGABA in neurons [22] by directly binding to GABAAR channel and lowering its open probability [23]. Therefore, we used zinc-free insulin to verify the suppressive effects of insulin on IGABA. Our result showed that the zinc-free insulin also suppressed IGABA in INS-1 cells ( Figure 3A , p<0.05). The efficacy of zinc-free insulin was similar to that of regular insulin ( Figures 3B and 3C ). However, the suppression of IGABA by insulin disappeared when zinc-free insulin was applied simultaneously with GABA ( Figures 3D and 3E , p>0.05, n = 3). We found that the reduction of IGABA was seen only when zinc-free insulin was pre-applied to the cell (i.e., >30 seconds) prior to GABA application ( Figures 3D and 3E , p<0.05, n = 3). These results suggest that zinc-free insulin-induced inhibition of IGABA is not a result of direct blockade of GABAAR channels, but rather through a signaling process.
Figure 3. Zinc-free insulin inhibits GABA-evoked currents in INS-1 cells.
(A) Representative traces of GABA-evoked currents in the absence and presence of zinc-free insulin and regular insulin in the same INS-1 cell. (B) The average of IGABA from separated experiments. (C) Normalized average IGABA was separately recorded during the course of experiment (control = average of first 4 IGABA, ZFI = average of IGABA in the presence zinc-free insulin, insulin = average of IGABA in the presence of insulin after washing out). (D) Representative traces of IGABA obtained from when GABA was applied simultaneously with insulin or 30 seconds after insulin pre-treatment. (E) Normalized average IGABA of separated experiments as described in (C). Data were mean ± SE. *p<0.05, n = 5.
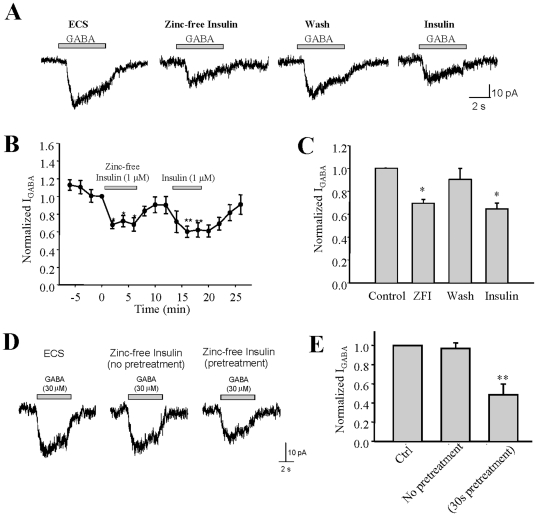
Insulin-induced inhibition on IGABA is PI3-K/Akt independent
PI3-K is a key signaling molecule that mediates the trophic effects of insulin [24]. We therefore examined whether insulin-induced inhibition of IGABA requires involvement of PI3-K. INS-1 cells were pretreated with 100 nM of the specific PI3-K inhibitor wortmannin for 10 minutes, and then treated with 1 µM zinc-free insulin prior to measurement of IGABA. As shown ( Figures 4A and 4B ), the zinc-free insulin-induced inhibition of IGABA persisted in the presence of PI3-K inhibitor, which is suggestive of a PI3-K independent process. To confirm this finding, we transfected INS-1 cells with a vector expressing a dominant-negative form of Akt (DN-Akt) and tagged with green fluorescent protein (GFP) [12]. The dominant negative effect of DN-Akt was determined in parallel experiments by Western Blot using anti-phospho-Akt (Ser473) antibody in either transfected or non-transfected INS-cells treated with or without inhibitors as indicated ( Figure 4C ). Application of zinc-free insulin (1 µM) to the transfected INS-1 cells still caused a remarkable reduction of IGABA ( Figures 4D ). Normalized IGABA from separated experiments showed zinc-free insulin reduced IGABA by approximately 30% in INS-1 cells expressing DN-Akt ( Figure 4E , n = 5, p<0.05). These observations suggest that zinc-free insulin-induced inhibition on IGABA is not sensitive to the PI3-K/Akt inhibition.
Figure 4. Insulin-induced inhibition of IGABA in INS-1 cells is PI3-K/Akt independent.
(A) Representative traces of GABA-evoked currents in the absence and presence of zinc-free insulin (1 µM) along with PI3-K inhibitor wortmannin (100 nM). (B) Normalized average of IGABA from separated experiments. (C) Akt activity determined by Western Blotting using anti-phospho Akt (S473) in cells treated without or with wortmannin (Wort), or in the cells transfected with dominant-negative Akt (DN-Akt). (D) Representative traces of GABA-evoked currents in cells expressing DN-Akt in the absence and presence of zinc-free insulin (ZFI,1 µM). (E) Average IGABA from separated time-course experiments. Data were mean ± SE. *p<0.05, ** p<0.01, n = 5.
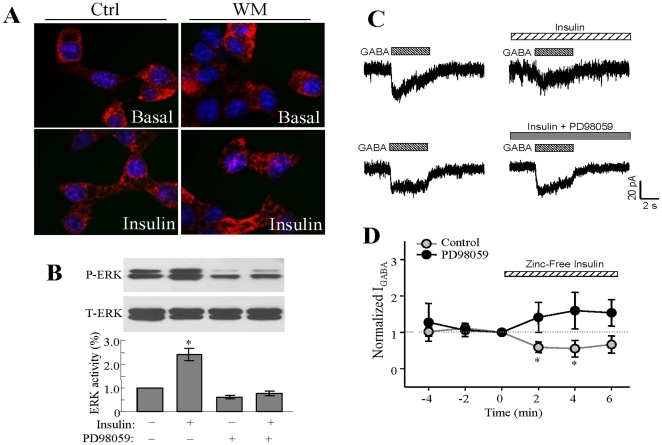
Insulin does not alter the localization of GABAAR at the INS-1 plasma membrane
We previously demonstrated that insulin enhances the insertion of GABAAR into the plasma membrane in neuron [25] and α-cell [12]. We thus investigated whether insulin could alter GABAAR membrane expression in INS-1 cells by immunostaining using antibody against the GABAARβ2/3 subunits. As shown, insulin (1 µM, 15 min) did not alter the staining profile of GABAARβ2/3 subunits ( Figure 5A ) in INS-1 cells treated with or without wortmannin, suggesting that insulin-induced suppression of IGABA is not related to GABAAR redistribution in INS-1 cells.
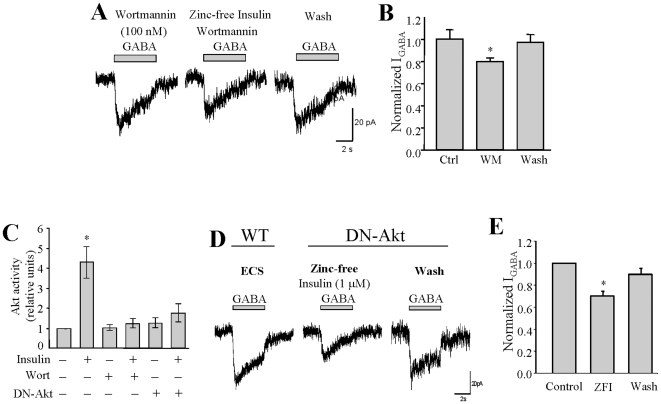
Figure 5. Insulin suppresses IGABA which is not associated with GABAAR membrane relocalization and is ERK-dependent.
(A) Confocal microscopic image of INS-1 cells immunostained for GABAARs using anti-GABAAR β2/3 mouse IgG and Cy3-conjugated secondary antibody (red) with DAPI-nuclear staining (blue). Cells were treated with or without insulin, in the presence or absence of PI3-K inhibitor wortmannin. (B) Insulin (100 nM, 5 min) stimulated ERK phosphorylation in INS-1 cells, which was blocked by pre-treatment of the cells with PD98059 (20 µM, 10 min). (C) Representative traces of GABA-evoked currents in the absence and presence of zinc-free insulin (0.6 µM) with or without PD98059 (20 µM). (D) Normalized average of IGABA from separated experiments. Data were mean ± SE. *p<0.05, ** p<0.01, n = 5–6.
Insulin-induced inhibition of IGABA is ERK dependent
Activation of the MRK/ERK pathway represents another important branch of the insulin receptor signal transduction pathway in pancreatic β-cells [26]. We performed experiments to examine whether or not insulin-induced inhibition of IGABA requires activation of MEK/ERK. We found that incubation of INS-1 cells with insulin (100 nM, 5 min) resulted in rapid ERK1/2 phosphorylation, which was blocked by the MEK/ERK inhibitor PD98059 (20 µM) ( Figure 5B ). Perforated patch clamp recordings were then performed in the control INS-1 cells and INS-1 cells that were pretreated with PD98059 (20 µM, 10 min). We found that application of zinc-free insulin to the cells failed to inhibit IGABA in the presence of PD98059 ( Figures 5C, 5D ; p<0.05, n = 6). This result suggests that insulin suppresses GABAAR function via activation of the MEK/ERK pathway.
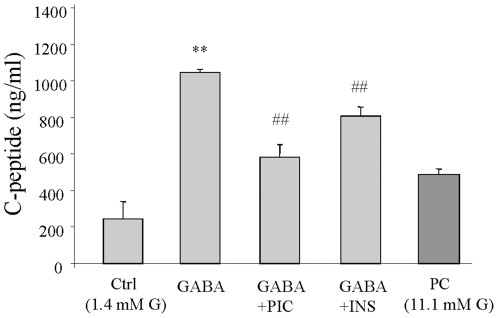
Insulin inhibits GABA-induced INS-1 cell secretion
We next conducted C-peptide radioimmunoassays (RIA) to determine whether or not the effect of insulin on the modulation of GABA-GABAAR system has an impact on GABAAR-mediated secretory function in INS-1 cells. As shown, consistent with our previous findings [15], GABA (30 µM) significantly increased C-peptide secretion in INS-1 cells, which was diminished by the GABAAR antagonist picrotoxin (50 µM) ( Figure 6 , p<0.01, n = 3), suggesting that GABA-induced insulin secretion in the β-cells is mediated by GABAAR. Furthermore, pre-treatment of the INS-1 cells with insulin (1 µM) resulted in a statistically-significant decrease in GABA-induced C-peptide secretion ( Figure 6 , p<0.01, n = 3). These results suggest that insulin-mediated inhibition of IGABA is related to down-regulation in GABA-induced insulin secretion in INS-1 cells.
Figure 6. GABA enhances insulin secretion which is attenuated by insulin in INS-1 cells.
Insulin secretion was evaluated by C-peptide RIA. Cells were serum-starved in KRB buffer containing 1.4 mM glucose for 60 min prior to the RIA. The RIA was conducted using cells which had their culture medium replaced with fresh KRB buffer containing 1.4 mM glucose (or 11.1 mM glucose as positive control, PC), in the presence of GABA (30 µM), with or without either picrotoxin (Pic, 50 µM) or insulin (Ins, 1 µM) for 120 min. Data were mean ± SE, from three independent experiments with each sample counted in triplication. ** p<0.01 (Ctrl vs GABA), ## p<0.01 (GABA vs GABA+Bic or GABA+Ins).
Discussion
Pancreatic β-cells produce a large amount of GABA [27], whereas GABAARs are expressed in both β-cells [6], [15] and α-cells [7], [12]. In α-cells, GABA hyperpolarizes the membrane potential and suppresses glucagon secretion [7], [12], via a mechanism involving PI3-K/Akt signaling dependent GABAAR plasma membrane translocation [12]. In contrast, we and others demonstrated that GABA depolarizes β-cells and stimulates insulin secretion from these cells [6], [15]. These observations suggest that GABA, as a paracrine or autocrine factor plays an important role within pancreatic islets in the regulation of islet cell secretion and function. In the present study, we sought to investigate how insulin affects GABA-GABAAR system in the β-cells and thereby modulates its secretory pathways.
In INS-1 cells, glucose induces a gradual and sustained depolarization, whereas GABA produces rapid and bicuculline- or picrotoxin-sensitive membrane depolarization, associated with remarkable increases in intracellular Ca2+ concentration and insulin secretion. A recent study by Braun et al. suggested that glucose stimulates feed-forward release of GABA from the β-cells [6]. Furthermore, the GABA-stimulated insulin release appears to be glucose concentration-dependent [6], [15]. Of note, our results showed that GABAAR antagonist picrotoxin attenuated about 50% of the GABA-induced C-peptide release. This is likely due to the fact that GABA-stimulated insulin secretion in the β-cells is partially contributed by activation of B-type GABA receptor (GABABR) [28]. These observations suggest that the autocrine GABA-GABAAR system in β-cells constitutes an effective signaling component of the glucose-sensing machinery.
The opposite effects of GABA in the two types of islet endocrine cells are likely because β-cells and α-cells have different Cl- reversal potential (ECl). The direction of Cl- flow upon opening of the GABAAR channel is dependent on the electrochemical driving force which is determined by the resting membrane potential and the ECl [29]. For example, in the early developing brain, GABA induces depolarizing effects in immature neurons [30], while it exerts inhibitory effects by hyperpolarizing the membrane potential in mature neurons of the adult brain [31]. The switch from excitation to inhibition of GABAAR activation is due to a shift of ECl which is controlled by increased activity of K+-Cl- co-transporter-2 (KCC2) in the brain during development [32]. In this regard, functional KCC has been identified in pancreatic α-cells, but not in the β-cells [33], [34].
Regular human insulin is a complex of insulin and zinc [35]. The finding that zinc-free insulin suppressed IGABA to a degree similar to that of regular insulin suggests that the inhibitory effects of insulin on IGABA is dependent on the insulin peptide. It is interesting to note that application of zinc-free insulin together with GABA did not inhibit IGABA, whereas pre-treating the cell for at least 30 seconds with zinc-free insulin inhibited IGABA. These results suggest that insulin-induced inhibition of IGABA in INS-1 cells requires insulin signaling processes. Such inhibitory effects of insulin on GABA-induced current was also observed in the non-islet β-cells [36] The potentiating effect of insulin on IGABA in neurons and α-cells is attributed to GABAAR insertion into the plasma membrane, which occurred about 10-15 min after insulin treatment [12], [25]. Under similar experimental conditions, however, we did not observe increased GABAAR localization at the plasma membrane upon insulin treatment in INS-1 cells. Furthermore, unlike in the α-cells, where the insulin-enhanced IGABA is PI3-K/Akt dependent, our data does not suggest the involvement of PI3-K/Akt signaling in the inhibition of IGABA by insulin in the β-cells. In contrast, MEK/ERK inhibitor PD98059 blocked the inhibitory effect of insulin on GABA-induced current, suggesting that insulin regulates GABAAR function in INS-1 cells via activation of the MEK/ERK signaling pathway.
The explanation for the opposite effects of insulin on GABAAR in α- and β-cells is largely unknown, although it may be due to the different subunit composition of GABAAR in the two types of islet cells [12], [15]. It is interesting to note that in neurons, activation of the insulin-PI3-K signaling pathway enhances IGABA due to the increase in cell surface-localized GABAAR, whereas activation of insulin receptor with ERK kinase causes inhibition of IGABA through phosphorylation of a specific subunit of GABAAR [36], [37]. Particularly, α-subunits of the GABAAR have a putative phosphorylation site for ERK [37]. Presumably, such phosphorylation occurs on an intracellular site allowing immediate allosteric modifications of GABAAR.
Given the relatively rapid inhibitory effect of insulin on IGABA, it is possible that insulin may also act as a non-competitive inhibitor of the GABAAR in the β-cells, as has been observed in non-β-cells [36]. In relation to this notion, it has been reported that a direct receptor-receptor interaction occurs between GABAAR and dopamine D5 receptor, which affects the GABAAR activation [38]. Further study is warranted to test if there is an interaction between insulin receptor and GABAAR, and to determine the molecular mechanism by which insulin modulates GABA-GABAAR signaling in the β-cells.
In INS-1 cells, insulin suppresses IGABA and decreases GABA-mediated insulin secretion in the β-cells which suggests that insulin may utilize the GABA-GABAAR system to constitute a feedback mechanism for the β-cell secretion. Our findings are in a good agreement with previous observations suggesting that activation of insulin receptor inhibits insulin secretion in the β-cells [39]. Conversely, inhibition of PI3-K signaling pathways enhances insulin secretion in the β-cells [40], [41]. A study by Khan et al suggested that insulin inhibits insulin secretion through activation of KATP channels in the β-cells [42]. A study by Jimenez-Feltstrom and colleagues [43] suggested that the effect of insulin on IGABA is insulin-dose dependent, exemplified by the observation that, insulin, at low concentrations (i.e., from 0.05 to 0.1 nM) stimulated insulin release, while at concentrations higher than 250 nM, insulin inhibited insulin secretion from the β-cells.
It should be noted that under certain circumstance, effects of insulin on IGABA are excitatory [16]. These previous reports that describe the stimulatory effects of insulin on β-cell secretory process were mostly supported by experiments involving β-cells from organisms with genetic knockout or overexpression of the insulin receptor [44]–[48], The different outcomes imply that the modulation of insulin on the GABA-GABAAR system in the β-cells may be dependent on their metabolic status.
The physiological relevance of GABA signaling in the regulation of islet β-cell function has yet to be fully identified. We demonstrated recently that the depolarizing effects of GABA may lead to activation of PI3-K/Akt dependent cell growth and survival pathways in the β-cells [18]. Insulin is an important positive autocrine regulator of β-cell growth and survival [17], [49]. GABA, when co-released with insulin [6], synergistically enhances insulin-stimulated cell growth and survival pathways in the β-cells [18]. In support of previous findings that insulin is a negative regulator of insulin secretion [39]–[42], [50], our data suggest that insulin utilizes the autocrine GABA-GABAAR pathway to operate its negative feedback suppression in the β-cells.
Such a negative feedback modulator appears to be important for maintaining islet hormones at appropriate levels [51]. It is conceivable that basal insulin may serve as a maintenance signal that primes the β-cell to respond to subsequent glucose stimulus, insulin may utilize GABA-GABAAR system to inhibit further release at the peak of the exocytotic event, particularly, at very high local insulin concentration. Previous euglycemic hyperinsulinemic clamp studies in humans suggest that this negative short-loop insulin-β-cell feedback is an important mechanism in maintaining appropriate β-cell secretion, since inadequate feedback suppression is found in obese patients, and may partly account for their prevailing hyperinsulinemia [52]. Given that autocrine insulin action is critical in maintaining normal β-cell function [16], [17], and that β-cell insulin resistance can deteriorate β-cell function that accelerates the progression of diabetes [53], [54], future studies are required to determine whether the impairment of the autocrine insulin-GABA-GABAAR signaling contributes to β-cell insulin resistance in type 2 diabetes.
Acknowledgments
The authors wish to thank Novo Nordisk (Canada) for providing zinc-free insulin. The authors also thank Xiaoming Li, Nina Zhang and Joel Perrella for excellent technical assistance.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by grants from the Canadian Institute for Health Research (CIHR) (MOP-79534 to Q. Wang and MOP-84517 to W.Y. Lu). Research in Dr. Wang's laboratory was also supported by grants from the Canadian Diabetes Association (CDA) and the Juvenile Diabetes Research Foundation. Q. Wang is presently supported by the New Investigator Program from CIHR. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Luscher B, Keller CA. Regulation of GABAA receptor trafficking, channel activity, and functional plasticity of inhibitory synapses. Pharmacol Ther. 2004;102:195–221. doi: 10.1016/j.pharmthera.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 2.Okada Y, Taniguchi H, Shimada C. High Concentration of GABA and High Glutamate Decarboxylase Activity in Rat Pancreatic Islets and Human Insulinoma. Science. 1976;194:620–622. doi: 10.1126/science.185693. [DOI] [PubMed] [Google Scholar]
- 3.Gerber JC, III, Hare TA. Gamma-aminobutyric acid in peripheral tissue, with emphasis on the endocrine pancreas: presence in two species and reduction by streptozotocin. Diabetes. 1979;28:1073–1076. doi: 10.2337/diab.28.12.1073. [DOI] [PubMed] [Google Scholar]
- 4.Vincent SR, Hokfelt T, Wu JY, Elde RP, Morgan LM, et al. Immunohistochemical studies of the GABA system in the pancreas. Neuroendocrinology. 1983;36:197–204. doi: 10.1159/000123456. [DOI] [PubMed] [Google Scholar]
- 5.Reetz A, Solimena M, Matteoli M, Folli F, Takei K, et al. GABA and pancreatic beta-cells: colocalization of glutamic acid decarboxylase (GAD) and GABA with synaptic-like microvesicles suggests their role in GABA storage and secretion. EMBO J. 1991;10:1275–1284. doi: 10.1002/j.1460-2075.1991.tb08069.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braun M, Ramracheya R, Bengtsson M, Clark A, Walker JN, et al. Gamma-Aminobutyric Acid (GABA) Is an Autocrine Excitatory Transmitter in Human Pancreatic Beta-Cells. Diabetes. 2010;59:1694–1701. doi: 10.2337/db09-0797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rorsman P, Berggren PO, Bokvist K, Ericson H, Mohler H, et al. Glucose-inhibition of glucagon secretion involves activation of GABAA-receptor chloride channels. Nature. 1989;341:233–236. doi: 10.1038/341233a0. [DOI] [PubMed] [Google Scholar]
- 8.Smismans A, Schuit F, Pipeleers D. Nutrient regulation of gamma-aminobutyric acid release from islet beta cells. Diabetologia. 1997;40:1411–1415. doi: 10.1007/s001250050843. 10.1007/s001250050843. [DOI] [PubMed] [Google Scholar]
- 9.Winnock F, Ling Z, De Proft R, Dejonghe S, Schuit F, et al. Correlation between GABA release from rat islet beta -cells and their metabolic state. Am J Physiol Endocrinol Metab. 2002;282:E937–E942. doi: 10.1152/ajpendo.00071.2001. [DOI] [PubMed] [Google Scholar]
- 10.Wendt A, Birnir B, Buschard K, Gromada J, Salehi A, et al. Glucose Inhibition of Glucagon Secretion From Rat [alpha]-Cells Is Mediated by GABA Released From Neighboring [beta]-Cells. Diabetes. 2004;53:1038–1045. doi: 10.2337/diabetes.53.4.1038. [DOI] [PubMed] [Google Scholar]
- 11.Bailey SJ, Ravier MA, Rutter GA. Glucose-dependent regulation of gamma-aminobutyric acid (GABA A) receptor expression in mouse pancreatic islet alpha-cells. Diabetes. 2007;56:320–327. doi: 10.2337/db06-0712. [DOI] [PubMed] [Google Scholar]
- 12.Xu E, Kumar M, Zhang Y, Ju W, Obata T, et al. Intra-islet insulin suppresses glucagon release via GABA-GABAA receptor system. Cell Metab. 2006;3:47–58. doi: 10.1016/j.cmet.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 13.Glassmeier G, Hopfner M, Buhr H, Lemmer K, Riecken EO, et al. Expression of functional GABAA receptors in isolated human insulinoma cells. Ann N Y Acad Sci. 1998;859:241–248. doi: 10.1111/j.1749-6632.1998.tb11138.x. [DOI] [PubMed] [Google Scholar]
- 14.Blankenfeld G, Enkvist MOK, Kettenmann H, Turner J, Ahnert-Hilger G, et al. Expression of functional GABAA receptors in neuroendocrine gastropancreatic cells. Pflugers Archiv European Journal of Physiology. 1995;430:381–388. doi: 10.1007/BF00373913. 10.1007/BF00373913. [DOI] [PubMed] [Google Scholar]
- 15.Dong H, Kumar M, Zhang Y, Gyulkhandanyan A, Xiang YY, et al. Gamma-aminobutyric acid up- and downregulates insulin secretion from beta cells in concert with changes in glucose concentration. Diabetologia. 2006;49:697–705. doi: 10.1007/s00125-005-0123-1. [DOI] [PubMed] [Google Scholar]
- 16.Leibiger IB, Leibiger B, Berggren PO. Insulin Signaling in the Pancreatic [beta]-Cell. Annual Review of Nutrition. 2008;28:233–251. doi: 10.1146/annurev.nutr.28.061807.155530. doi: 10.1146/annurev.nutr.28.061807.155530. [DOI] [PubMed] [Google Scholar]
- 17.Wang Q, Jin T. The role of insulin signaling in the development of beta-cell dysfunction and diabetes. Islets. 2009;1:95–101. doi: 10.4161/isl.1.2.9263. [DOI] [PubMed] [Google Scholar]
- 18.Soltani N, Qiu H, Aleksic M, Glinka Y, Zhao F, et al. GABA exerts protective and regenerative effects on islet beta cells and reverses diabetes. Proc Natl Acad Sci U S A. 2011;108:11692–11697. doi: 10.1073/pnas.1102715108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sugita M, Hirono C, Shiba Y. Gramicidin-perforated Patch Recording Revealed the Oscillatory Nature of Secretory Cl- Movements in Salivary Acinar Cells. The Journal of General Physiology. 2004;124:59–69. doi: 10.1085/jgp.200308948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li J, Zhang N, Ye B, Ju W, Orser B, et al. Non-steroidal anti-inflammatory drugs increase insulin release from beta cells by inhibiting ATP-sensitive potassium channels. Br J Pharmacol. 2007;151:483–493. doi: 10.1038/sj.bjp.0707259. 0707259 [pii];10.1038/sj.bjp.0707259 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith GD, Swenson DC, Dodson EJ, Dodson GG, Reynolds CD. Structural stability in the 4-zinc human insulin hexamer. Proc Natl Acad Sci U S A. 1984;81:7093–7097. doi: 10.1073/pnas.81.22.7093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aguayo LG, Alarcon JM. Modulation of the developing rat sympathetic GABAA receptor by Zn++, benzodiazepines, barbiturates and ethanol. Journal of Pharmacology and Experimental Therapeutics. 1993;267:1414–1422. [PubMed] [Google Scholar]
- 23.Hosie AM, Dunne EL, Harvey RJ, Smart TG. Zinc-mediated inhibition of GABAA receptors: discrete binding sites underlie subtype specificity. Nat Neurosci. 2003;6:362–369. doi: 10.1038/nn1030. 10.1038/nn1030. [DOI] [PubMed] [Google Scholar]
- 24.Taniguchi CM, Emanuelli B, Kahn CR. Critical nodes in signalling pathways: insights into insulin action. Nat Rev Mol Cell Biol. 2006;7:85–96. doi: 10.1038/nrm1837. 10.1038/nrm1837. [DOI] [PubMed] [Google Scholar]
- 25.Wang Q, Liu L, Pei L, Ju W, Ahmadian G, et al. Neuron. 38; 2003. Control of Synaptic Strength, a Novel Function of Akt. pp. 915–928. doi: 10.1016/S0896-6273(03)00356-8. [DOI] [PubMed] [Google Scholar]
- 26.Assmann A, Ueki K, Winnay JN, Kadowaki T, Kulkarni RN. Glucose effects on beta-cell growth and survival require activation of insulin receptors and insulin receptor substrate 2. Mol Cell Biol. 2009;29:3219–3228. doi: 10.1128/MCB.01489-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adeghate E, Ponery AS. GABA in the endocrine pancreas: cellular localization and function in normal and diabetic rats. Tissue and Cell. 2002;34:1–6. doi: 10.1054/tice.2002.0217. doi: 10.1054/tice.2002.0217. [DOI] [PubMed] [Google Scholar]
- 28.Ligon B, Yang J, Morin SB, Ruberti MF, Steer ML. Regulation of pancreatic islet cell survival and replication by gamma-aminobutyric acid. Diabetologia. 2007;50:764–773. doi: 10.1007/s00125-007-0601-8. [DOI] [PubMed] [Google Scholar]
- 29.Bormann J. Electrophysiology of GABAA and GABAB receptor subtypes. Trends in Neurosciences. 1988;11:112–116. doi: 10.1016/0166-2236(88)90156-7. doi: 10.1016/0166-2236(88)90156-7. [DOI] [PubMed] [Google Scholar]
- 30.Chen G, Trombley PQ, van den Pol AN. Excitatory actions of GABA in developing rat hypothalamic neurones. The Journal of Physiology. 1996;494:451–464. doi: 10.1113/jphysiol.1996.sp021505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Owens DF, Kriegstein AR. Is there more to gaba than synaptic inhibition? Nat Rev Neurosci. 2002;3:715–727. doi: 10.1038/nrn919. 10.1038/nrn919. [DOI] [PubMed] [Google Scholar]
- 32.Ludwig A, Li H, Saarma M, Kaila K, Rivera C. Developmental up-regulation of KCC2 in the absence of GABAergic and glutamatergic transmission. Eur J Neurosci. 2003;18 doi: 10.1111/j.1460-9568.2003.03069.x. 3199-3206. 3069 [pii] [DOI] [PubMed] [Google Scholar]
- 33.Davies SL, Roussa E, Le Rouzic P, Thevenod F, Alper SL, et al. Expression of K+-Cl- cotransporters in the [alpha]-cells of rat endocrine pancreas. Biochimica et Biophysica Acta (BBA) - Biomembranes. 2004;1667:7–14. doi: 10.1016/j.bbamem.2004.08.005. doi: 10.1016/j.bbamem.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 34.Takayama C, Inoue Y. Developmental localization of potassium chloride co-transporter 2 (KCC2), GABA and vesicular GABA transporter (VGAT) in the postnatal mouse somatosensory cortex. Neurosci Res. 2010;67:137–148. doi: 10.1016/j.neures.2010.02.010. [DOI] [PubMed] [Google Scholar]
- 35.Chausmer AB. Zinc, Insulin and Diabetes. J Am Coll Nutr. 1998;17:109–115. doi: 10.1080/07315724.1998.10718735. [DOI] [PubMed] [Google Scholar]
- 36.Williams DB. A novel, rapid, inhibitory effect of insulin on [alpha]1[beta]2[gamma]2s [gamma]-aminobutyric acid type A receptors. Neuroscience Letters. 2008;443:27–31. doi: 10.1016/j.neulet.2008.07.038. doi: 10.1016/j.neulet.2008.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bell-Horner CL, Dohi A, Nguyen Q, Dillon GH, Singh M. ERK/MAPK pathway regulates GABAA receptors. J Neurobiol. 2006;66:1467–1474. doi: 10.1002/neu.20327. [DOI] [PubMed] [Google Scholar]
- 38.Liu F, Wan Q, Pristupa ZB, Yu XM, Wang YT, et al. Direct protein-protein coupling enables cross-talk between dopamine D5 and [gamma]-aminobutyric acid A receptors. Nature. 2000;403:274–280. doi: 10.1038/35002014. 10.1038/35002014. [DOI] [PubMed] [Google Scholar]
- 39.Persaud SJ, Asare-Anane H, Jones PM. Insulin receptor activation inhibits insulin secretion from human islets of Langerhans. FEBS Letters. 2002;510:225–228. doi: 10.1016/s0014-5793(01)03268-9. doi: 10.1016/S0014-5793(01)03268-9. [DOI] [PubMed] [Google Scholar]
- 40.Collier JJ, White SM, Dick GM, Scott DK. Phosphatidylinositol 3-kinase inhibitors reveal a unique mechanism of enhancing insulin secretion in 832/13 rat insulinoma cells. Biochem Biophys Res Commun. 2004;324:1018–1023. doi: 10.1016/j.bbrc.2004.09.149. [DOI] [PubMed] [Google Scholar]
- 41.Eto K, Yamashita T, Tsubamoto Y, Terauchi Y, Hirose K, et al. Phosphatidylinositol 3-kinase suppresses glucose-stimulated insulin secretion by affecting post-cytosolic [Ca(2+)] elevation signals. Diabetes. 2002;51:87–97. doi: 10.2337/diabetes.51.1.87. [DOI] [PubMed] [Google Scholar]
- 42.Khan FA, Goforth PB, Zhang M, Satin LS. Insulin Activates ATP-Sensitive K+ Channels in Pancreatic [beta]-Cells Through a Phosphatidylinositol 3-Kinase–Dependent Pathway. Diabetes. 2001;50:2192–2198. doi: 10.2337/diabetes.50.10.2192. [DOI] [PubMed] [Google Scholar]
- 43.Jimenez-Feltstrom J, Lundquist I, Obermuller S, Salehi A. Insulin feedback actions: complex effects involving isoforms of islet nitric oxide synthase. Regul Pept. 2004;122:109–118. doi: 10.1016/j.regpep.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 44.Aspinwall CA, Lakey JRT, Kennedy RT. Insulin-stimulated Insulin Secretion in Single Pancreatic Beta Cells. J Biol Chem. 1999;274:6360–6365. doi: 10.1074/jbc.274.10.6360. [DOI] [PubMed] [Google Scholar]
- 45.Aspinwall CA, Qian WJ, Roper MG, Kulkarni RN, Kahn CR, et al. Roles of Insulin Receptor Substrate-1, Phosphatidylinositol 3-Kinase, and Release of Intracellular Ca2+ Stores in Insulin-stimulated Insulin Secretion in [beta]-Cells. J Biol Chem. 2000;275:22331–22338. doi: 10.1074/jbc.M909647199. [DOI] [PubMed] [Google Scholar]
- 46.Kulkarni RN, Bruning JC, Winnay JN, Postic C, Magnuson MA, et al. Tissue-Specific Knockout of the Insulin Receptor in Pancreatic [beta] Cells Creates an Insulin Secretory Defect Similar to that in Type 2 Diabetes. Cell. 1999;96:329–339. doi: 10.1016/s0092-8674(00)80546-2. doi: 10.1016/S0092-8674(00)80546-2. [DOI] [PubMed] [Google Scholar]
- 47.Otani K, Kulkarni RN, Baldwin AC, Krutzfeldt J, Ueki K, et al. Reduced {beta}-cell mass and altered glucose sensing impair insulin-secretory function in {beta}IRKO mice. Am J Physiol Endocrinol Metab. 2004;286:E41–E49. doi: 10.1152/ajpendo.00533.2001. [DOI] [PubMed] [Google Scholar]
- 48.Xu GG, Rothenberg PL. Insulin receptor signaling in the beta-cell influences insulin gene expression and insulin content: evidence for autocrine beta-cell regulation. Diabetes. 1998;47:1243–1252. doi: 10.2337/diab.47.8.1243. [DOI] [PubMed] [Google Scholar]
- 49.Bansal P, Wang Q. Insulin as a physiological modulator of glucagon secretion. Am J Physiol Endocrinol Metab. 2008;295:E751–E761. doi: 10.1152/ajpendo.90295.2008. [DOI] [PubMed] [Google Scholar]
- 50.Elahi D, Nagulesparan M, Hershcopf RJ, Muller DC, Tobin JD, et al. Feedback inhibition of insulin secretion by insulin: relation to the hyperinsulinemia of obesity. N Engl J Med. 1982;306:1196–1202. doi: 10.1056/NEJM198205203062002. [DOI] [PubMed] [Google Scholar]
- 51.Zhang Y, Zhang N, Gyulkhandanyan A, Xu E, Gaisano H, et al. Presence of functional hyperpolarisation-activated cyclic nucleotide-gated channels in clonal alpha cell lines and rat islet alpha cells. Diabetologia. 2008;51:2290–2298. doi: 10.1007/s00125-008-1166-x. [DOI] [PubMed] [Google Scholar]
- 52.Elahi D, Nagulesparan M, Hershcopf RJ, Muller DC, Tobin JD, et al. Feedback inhibition of insulin secretion by insulin: relation to the hyperinsulinemia of obesity. N Engl J Med. 1982;306:1196–1202. doi: 10.1056/NEJM198205203062002. [DOI] [PubMed] [Google Scholar]
- 53.Ueki K, Okada T, Hu J, Liew CW, Assmann A, et al. Total insulin and IGF-I resistance in pancreatic [beta] cells causes overt diabetes. Nat Genet. 2006;38:583–588. doi: 10.1038/ng1787. 10.1038/ng1787. [DOI] [PubMed] [Google Scholar]
- 54.Zhao J, Zhang N, He M, Yang Z, Tong W, et al. Increased Beta-Cell Apoptosis and Impaired Insulin Signaling Pathway Contributes to the Onset of Diabetes in OLETF Rats. Cellular Physiology and Biochemistry. 2008;21:445–454. doi: 10.1159/000129637. [DOI] [PubMed] [Google Scholar]