Abstract
OBJECTIVES
To evaluate the associations between comorbidities, functional limitations, geriatric syndromes, treatment patterns, and outcomes in a population-based cohort of older patients diagnosed with colorectal cancer and receiving home health care.
DESIGN
Retrospective study.
SETTING
Data from the Ohio Cancer Incidence Surveillance System, Medicare claims and enrollment files, and the home health care Outcome and Assessment Information Set.
PARTICIPANTS
Ohio residents diagnosed with incident colorectal cancer in 1999 to 2001 and receiving home health care in the 30 days before or after cancer diagnosis (N = 957).
MEASUREMENTS
Outcome measures included receipt of cancer treatment and survival through 2005.
RESULTS
Not having surgery was associated negatively with comorbidities but positively with functional limitations and geriatric syndromes. Receipt of chemotherapy was negatively associated with comorbidities and functional limitations. The presence of two or more geriatric syndromes was significantly associated with unfavorable survival outcomes when analyzing overall survival and disease-specific survival (DSS). Having limitations in two or more activities of daily living was associated with unfavorable overall survival but not with DSS. Comorbity was associated with favorable DSS at borderline level of statistical significance but not with overall survival.
CONCLUSION
The findings highlight the importance of incorporating functional limitations and geriatric syndrome data in geriatric oncology outcomes studies.
Keywords: colorectal cancer, comorbidity, functional limitations, geriatric syndromes, cancer treatment, survival
The characterization of comorbidity burden and clinical presentation in older adults with cancer poses an important methodological challenge in outcomes research, especially when using population-based data. Such data, usually originating from the linked Surveillance, Epidemiology, and End Results (SEER)-Medicare files, rely solely on diagnosis codes documented in Medicare claims data.
In addition to multiple sources of error that can affect completeness and accuracy,1 diagnosis codes retrieved from claims data seldom reflect the level of severity of comorbid conditions. Instead, a comorbid condition identified from claims data is usually coded in a dichotomous fashion—“present” if the diagnosis code is found in claims history and “absent” otherwise. Furthermore, comorbidities are coded in a similar fashion irrespective of the patient’s functional or health status or the setting in which care is received. Thus, for example, the presence of a given condition is coded the same way in a nursing home patient with cognitive or functional impairment and a community-dwelling person with normal cognitive or functional status. As a result, comorbidities derived from claims data probably provide little information when analyzing patterns of care and outcomes in relation to clinical presentation.
In addition, claim records lack data on functional limitations and on most geriatric syndromes. Functional limitations and geriatric syndromes are considered important components of the Comprehensive Geriatric Assessment (CGA)2 and critical in identifying frail patients who may have limited physiological and functional reserves to tolerate aggressive cancer treatment.3 Because of the limitations of population-based data noted above, associations between functional limitations, geriatric syndromes, and outcomes have not been studied in population-based cohorts, and their utility in cancer-related health services research has remained largely unexplored, except in a few small studies using primary clinical data.4,5
To address these gaps in knowledge, this study used the home health care Outcome Assessment and Information Set (OASIS), which includes detailed clinical assessment data encompassing comorbidities, functional limitations, and geriatric syndromes. When linked with additional relevant sources, the use of OASIS data would make it possible to assess the utility of comorbidities, functional limitations, and geriatric syndromes in studying patterns of care and outcomes in a cohort of cancer patients admitted to home health care. The study hypothesis is that functional limitations and geriatric syndromes are strongly associated with patterns of care and survival outcomes and thus would be highly useful in geriatric oncology outcomes research.
METHODS
The study used the Ohio Cancer-Aging Linked Database (CALD), developed by linking records from the Ohio Cancer Incidence Surveillance System (OCISS) with Medicare and Medicaid enrollment and claims files, the Ohio death certificate files, and the home health care OASIS, among others. The CALD data pertain to Ohio residents aged 65 and older diagnosed with incident breast, prostate, or colorectal cancer during 1997 to 2001.
The files were linked using patient identifiers, including the patient’s social security number, name, and date of birth, as detailed elsewhere.6 The Centers for Medicare and Medicaid Services (CMS) linked Medicare enrollment and claims files with OCISS records, whereas the investigative team linked the other data sources with the OCISS. More than 97% of all patients in the OCISS were identified in Medicare files.6
The institutional review board of the University Hospitals of Cleveland and the government agencies that supplied the data, including CMS and the Ohio Department of Health approved the development of the CALD and relevant studies.
In this study, the OCISS was used to identify cases with incident colorectal cancer and to retrieve the date of diagnosis and cancer stage. OASIS data were used to identify patients admitted to home health care in the 30 days before or after initial cancer diagnosis. Medicare enrollment data were used to identify and exclude patients with history of participation in managed care programs, whereas claims data served as the basis to identify colorectal cancer–related surgery and chemotherapy. Ohio death certificate files were used to ascertain vital status at the end of the study period (December 31, 2005) and to retrieve the date and cause of death. Finally, the OASIS served as the source of data on comorbidities, functional limitations, and geriatric syndromes, reflecting the patient’s status in the 14 days before the date of assessment or at baseline, as described elsewhere.7 Using the diagnosis codes documented in the OASIS, comorbid conditions included in the National Cancer Institute, National Institute on Aging (NCI/NIA) list of comorbidities were identified.8 Functional limitations were defined as need for assistance in activities of daily living (ADLs). The list of geriatric syndromes was retrieved from a previous publication.3 The variables available through the OASIS could identify all of these geriatric syndromes except neglect and abuse. Comorbidities, functional limitations, and geriatric syndromes were each categorized in counts of 0, 1, and 2t. Because OASIS data were not available until July 1999, the study cohort was limited to patients diagnosed with colorectal cancer between August 1, 1999 and November 31, 2001.
The study outcomes were surgery (yes/no), indicating whether patients underwent colorectal resection; receipt of chemotherapy (yes/no); overall survival; and disease-specific survival (DSS). Treatment modalities were identified by examining Medicare claims data in the 6 months after initial cancer diagnosis. Logistic regression models were developed to analyze the associations between treatment and comorbidities, functional limitations, and geriatric syndromes and treatment patterns after adjusting for demographic variables and cancer stage. Cox regression models were developed to study the association between survival and clinical presentation after adjusting for patient attributes, cancer stage, and cancer treatment.
RESULTS
The study included 957 patients. The mean age (± standard deviation) was 77.6 ± 7.0. Nearly 89% of patients underwent colorectal resection, and 36% received chemotherapy. Not having surgery was associated negatively with the presence of one comorbid condition (adjusted odds ratio (AOR) = 0.52, 95% confidence interval (CI) = 0.29–0.93) but positively with the presence of limitations in one ADL (AOR = 1.96; 95% CI = 1.09–3.53). Additionally, not having surgery was positively associated with the presence of two or more geriatric syndromes (AOR = 2.20, 95% CI = 1.25–3.86). Patients with two or more comorbid conditions and those presenting limitations in two or more ADLs were 35% to 40% less likely to receive chemotherapy than their healthier counterparts.
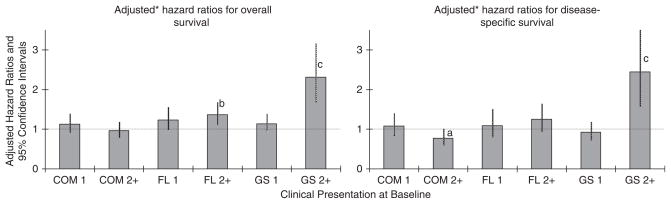
Findings from the Cox regression models showed that the presence of two or more geriatric syndromes was associated with unfavorable overall survival (adjusted hazard ratio (AHR) = 2.31, 95% CI = 1.69–3.17), and unfavorable DSS (AHR = 2.45, 95% CI = 1.59–3.75). Having limitations in two or more ADLs was associated with unfavorable overall survival but not with DSS. The presence of two or more comorbid conditions was associated favorably with DSS but only at borderline statistical significance levels (AHR = 0.77, 95% CI = 0.60–1.00). Having comorbid conditions was not associated with overall survival (Figure 1).
Figure 1.
Results from the multivariable survival models. *Adjusted for patient age, race, sex, tumor stage, and treatment received. The reference categories are no comorbidities for COM1 and COM2+, no functional limitations for FL1 and FL2+, and no geriatric syndromes for GS1 and GS2+. a.05≤P<.01; b.01≤P<.001; cP<.001; all other statistics not significant at P<.05. COM = comorbidity; FL = functional limitations; GS = geriatric syndromes.
DISCUSSION
Findings from this study show that functional limitations and geriatric syndromes are significantly associated with the outcomes of interest, highlighting the importance of variables characterizing clinical presentation that extend beyond comorbidities. The results from the survival analysis imply that comorbidities may not be associated with survival outcomes in the absence of functional limitations and geriatric syndromes. Furthermore, the negative and borderline significant association between two or more co-morbidities and DSS is of interest and should be explored in future studies.
Because of the small size of the study population, specific comorbid conditions, limitations in certain ADLs, and geriatric syndromes that were associated with various patterns in the outcomes could not be identified. Similarly, it was not possible to analyze outcomes when comorbidities, functional limitations, and geriatric syndromes coexist. This is an important weakness of this study, given that such conditions are often simultaneously present in older adults, as shown previously.7
Most population-based studies derived from claims data account for the presence or absence of comorbidities and not for disease severity. Although severity is also difficult to capture from the OASIS, the presence of functional limitations or geriatric syndromes adds considerably to the ability to assess clinical presentation, because they probably reflect a heightened state of vulnerability that the presence of comorbidities alone is not able to capture.
Few previous studies have accounted for functional limitations or geriatric syndromes in their analysis of cancer-related outcomes, and although these studies originate from clinical trials, their findings support the need to extend beyond comorbidities in characterizing older patients’ clinical presentation, because they indicate the importance of such factors as depression,4 quality-of-life measures, and dependency in instrumental ADLs5 in prognostic predictions, although the findings vary between studies. In one previous study,4 taking more than six different co-medications (reflecting comorbidity) was associated with outcomes in older patients with ovarian cancer. In another study,5 neither comorbidities nor dependency in ADLs was associated with outcomes in older patients with lung cancer.
Unfortunately, the use of such variables in studies of cancer-related outcomes at the population level is impractical because of the efforts required to append such variables to relevant administrative databases. Even then, these variables may be available only for select subgroups of the elderly population, leading to limited generalizability of the studies. Emerging needs in cancer–aging research warrant that frequently used population-based databases, such as the SEER-Medicare data, be enhanced to make such variables available for more broadly representative groups of older adults.
Acknowledgments
The author thanks Ms. Fang Xu, MS, and Dr. Paul M. Bakaki, MD, MS, for their analytical support.
Cancer incidence data were obtained from the OCISS, Ohio Department of Health. Use of these data does not imply that the Ohio Department of Health agrees or disagrees with any presentation, analyses, interpretations, or conclusions. Information about the OCISS may be obtained at odh.state.oh.us/ODHPrograms/CI_SURV/ci_surv1.htm.
Sponsor’s Role: The sponsor had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the manuscript.
Footnotes
A version of this study was presented at the “Geriatric Oncology and Primary Care: Promoting Partnerships in Practice and Research Conference,” April 3–4, 2008, Case Comprehensive Cancer Center of Case Western Reserve University, Cleveland, Ohio.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the author and has determined that the author has no financial or any other kind of personal conflicts with this paper. This study was supported by a Career Development Grant from the National Cancer Institute (K07 CA096705 to Dr. Koroukian) and a National Institutes of Health Cancer-Aging Research Development Grant (P20 CA103736 to Dr. Nathan Berger, Case School of Medicine; Dr. Koroukian, pilot project investigator).
Author Contributions: The author was responsible for securing funding for the study, the design, obtaining and linking the data, analysis and interpretation of the data, and manuscript writing.
References
- 1.Terris DD, Litaker DG, Koroukian SM. Health state information derived from secondary databases is affected by multiple sources of bias. J Clin Epidemiol. 2007;60:734–741. doi: 10.1016/j.jclinepi.2006.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Extermann M, Aapro M, Bernabei R. Use of comprehensive geriatric assessment in older cancer patients: Recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG) Crit Rev Oncol Hematol. 2005;55:241–252. doi: 10.1016/j.critrevonc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Balducci L, Extermann M. Management of the frail person with advanced cancer. Crit Rev Oncol Hematol. 2000;33:143–148. doi: 10.1016/s1040-8428(99)00063-3. [DOI] [PubMed] [Google Scholar]
- 4.Freyer G, Geay JF, Touzet S. Comprehensive geriatric assessment predicts tolerance to chemotherapy and survival in elderly patients with advanced ovarian carcinoma: A GINECO study. Ann Oncol. 2005;16:1795–1800. doi: 10.1093/annonc/mdi368. [DOI] [PubMed] [Google Scholar]
- 5.Maione P, Perrone F, Gallo C. Pretreatment quality of life and functional status assessment significantly predict survival of elderly patients with advanced nonsmall-cell lung cancer receiving chemotherapy: A prognostic analysis of the multicenter Italian lung cancer in the elderly study. J Clin Oncol. 2005;23:6865–6872. doi: 10.1200/JCO.2005.02.527. [DOI] [PubMed] [Google Scholar]
- 6.Koroukian SM. Linking the Ohio Cancer Incidence System with Medicare, Medicaid, and clinical data from home health care and long term care assessment instruments: Paving the way for new research endeavors in geriatric oncology. J Registry Manage. 2008;35:156–165. [PMC free article] [PubMed] [Google Scholar]
- 7.Koroukian SM, Murray P, Madigan E. Comorbidity, disability, and geriatric syndromes in elderly cancer patients receiving home health care. J Clin Oncol. 2006;24:2304–2310. doi: 10.1200/JCO.2005.03.1567. [DOI] [PubMed] [Google Scholar]
- 8.Yancik R, Wesley MN, Ries LAG. Comorbidity and age as predictors of risk for early mortality of male and female colorectal carcinoma: A population-based study. Cancer. 1998;82:2123–2134. [PubMed] [Google Scholar]