Abstract
The current paper provides external validation of the bifactor model of ADHD by examining associations between ADHD latent factor/profile scores and external validation indices. 548 children (321 boys; 302 with ADHD), 6 to 18 years old, recruited from the community participated in a comprehensive diagnostic procedure. Mothers completed the Child Behavior Checklist, Early Adolescent Temperament Questionnaire, and California Q-Sort. Children completed the Stop and Trail-Making Task. Specific inattention was associated with depression/withdrawal, slower cognitive task performance, introversion, agreeableness, and high reactive control; specific hyperactivity-impulsivity was associated with rule-breaking/aggressive behavior, social problems, errors during set-shifting, extraversion, disagreeableness, and low reactive control. It is concluded that the bifactor model provides better explanation of heterogeneity within ADHD than DSM-IV ADHD symptom counts or subtypes.
Keywords: ADHD, bifactor, cognitive control, personality, problem behavior
Attention-Deficit/Hyperactivity Disorder (ADHD) is a prevalent childhood behavioral disorder characterized by three continuous symptom dimensions of inattention, hyperactivity, and impulsivity (APA, 2000). The substantial heterogeneity of symptom presentation in individuals diagnosed with the disorder led to the development of three subtypes in DSM-IV (APA, 2000): Predominantly inattentive (ADHD-PI), predominantly hyperactive-impulsive (ADHD-PHI), and combined (ADHD-C). Although the validity of these subtypes has been called into question (e.g., Lahey et al., 2005), an alternative approach to parsing clinical heterogeneity has not been established. One promising approach is factorial, called the bifactor model. A bifactor model of ADHD features a general or “g” factor of ADHD with two specific “s” factors of inattention and hyperactivity-impulsivity that capture unique variance. This structural model has been tested in clinical and community-recruited samples of children with ADHD via comparison with other factor models (Martel, von Eye, & Nigg, 2010; Toplak et al., 2009). Now that the bifactor structure has been replicated by different investigators and samples, evaluation of its external validity via external correlates of ADHD is essential; this was the goal of the present investigation.
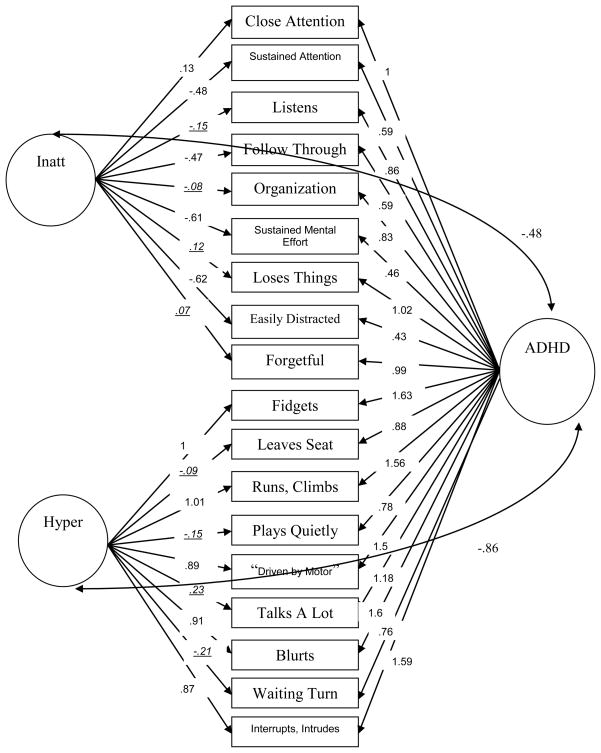
In the bifactor model of ADHD, a general, or “g,” factor of the disorder can exist simultaneously with two (or more) specific, or “s,” factors, in this case, inattention and hyperactivity-impulsivity (as shown in Figure 1). The model can capture interindividual heterogeneity in the symptom presentation of ADHD by suggesting that individuals can manifest with general and/or specific liabilities while carrying the same latent disorder. While individuals with a general liability would highly express both inattentive and hyperactive-impulsive symptoms of ADHD, individuals with a specific liability would present with relatively high inattentive or hyperactive-impulsive symptoms, yet would not have a separate disorder. A bifactor model of ADHD can provide similar information as the current DSM-IV concept of ADHD through (1) continuous measures of behavioral symptom domains, through the “g” ADHD and “s” inattention and hyperactivity-impulsivity latent factor scores, and (2) categorical subtypes, through latent profile analysis of the latent factor scores. Yet, a bifactor model may allow for more accurate quantification of symptom counts and better classification of individuals into categorical subgroups due to the fact that the model is more flexible and allows for measurement free from error. Thus, a bifactor model of ADHD may allow for a more meaningful and empirically sound parsing of clinical heterogeneity than the current DSM-IV conceptualization, allowing for a nuanced examination of external validity.
Figure 1. ADHD Bifactor Model.
Note. All path coefficients are standardized. Nonsignificant factors loadings are italicized and underlined. See Martel, von Eye, & Nigg (2010).
Children with DSM-IV ADHD demonstrate heterogeneity in the key external validation indices of psychiatric comorbidity, cognition or neuropsychology, and personality traits (Cantwell, 1992), and these indices have arguably received the most attention and most extensive validation in empirical work (e.g., Nigg, 2006), suggesting their importance in a complete understanding of the disorder. With regard to psychiatric comorbidity, ADHD is highly comorbid with Oppositional-Defiant Disorder (ODD), Conduct Disorder (CD), and anxiety and mood disorders (Angold, Costello, & Erkanli, 1999; Jensen, Martin, & Cantwell, 1997). Consistent DSM-IV subtype differences have been noted in the profile of comorbid conditions. Other disruptive behavior disorders like ODD and CD are more often seen in individuals with ADHD-C than in individuals with ADHD-PI (Milich, Balentine, & Lynam, 2001). In contrast, comorbid anxiety and mood disorders are more often seen in individuals with ADHD-PI, as compared to individuals with ADHD-C and ADHD-PHI (Barkley, 2006). Thus, anxiety and mood problems in ADHD may be more related to specific inattention, while comorbid disruptive behavior problems may be more related to specific hyperactivity-impulsivity and general ADHD (Lahey & Willcutt, 2010).
Weakness in neuropsychological cognitive control also plagues many individuals with ADHD and has been explored as an endophenotype of the disorder (Doyle et al., 2005). Deficits in response inhibition, working memory, set-shifting, planning, and vigilance have been most consistently associated with ADHD (Nigg, 2006; Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). However, problems with motivation and timing are also found in some children with ADHD. Although many children with ADHD exhibit problems with cognitive control, some children with ADHD have intact cognitive control and some children without ADHD exhibit problems in this domain (Willcutt et al., 2005). Pathway models of ADHD suggest that most aspects of cognitive control are more specifically related to the expression of the inattentive symptoms of the disorder, while motivation, speed, and timing are more related to the hyperactive-impulsive symptoms of the disorder (Sonuga-Barke, 2005). Further, a hypothesized group of children with only inattention and few or no hyperactive-impulsive symptoms may be characterized by slower performance, commonly referred to as sluggish cognitive tempo and/or ADHD-Restrictive Inattentive presentation as proposed in draft DSM-5 criteria (dsm5.org; Carr et al., 2010; Goth Owens et al., 2010; McBurnett, Pfiffner, & Frick, 2001). Thus, cognitive control and slow cognitive performance may exhibit associations with specific inattention, while an impulsive response pattern may show stronger associations with specific hyperactivity-impulsivity.
ADHD has been associated with a characteristic personality trait profile. This trait profile is typically characterized by low effortful control and conscientiousness, high negative emotionality and neuroticism, low agreeableness, and – in some cases – high extraversion (Nigg et al., 2002). When more specific relations between traits and ADHD symptoms have been examined, effortful control and conscientiousness appear to be somewhat differentially related to inattentive symptoms of ADHD, while reactive forms of control and negative emotionality or neuroticism are differentially related to hyperactivity-impulsivity and oppositional-defiance (Martel & Nigg, 2006). Other work also suggests a relationship between high negative emotionality, low agreeableness, and hyperactivity-impulsivity and ODD in school-aged children (Frick et al., 2003; Parker et al., 2004). Thus, effortful control and conscientiousness may be differentially related to specific inattention, whereas more affective forms of control like reactive control, negative emotionality/neuroticism, and low agreeableness may be more related to specific hyperactivity-impulsivity or general ADHD.
The current paper takes a critical approach to externally validating the bifactor structure of ADHD by utilizing a continuous symptom and categorical subtype approach, similar to DSM-IV. In the first approach, we examined the associations of specific inattention, specific hyperactivity, and general ADHD latent factor scores from the ADHD bifactor model with associated child problem behaviors, cognitive control, and personality traits. Hypotheses under this approach were that 1) specific inattention would be related to anxiety/mood symptoms, cognitive control, slower cognitive performance, and effortful control/conscientiousness traits; 2) specific hyperactivity-impulsivity would be related to ODD/CD problems, an impulsive response pattern on cognitive tasks, and reactive control, negative emotionality/neuroticism traits, and low agreeableness; and 3) general ADHD symptoms would show more uniform relations with child problem behaviors, cognitive control, and personality traits with the 4) specific latent factor scores exhibiting a more differentiated profile of association with the external validators, providing a better description of ADHD heterogeneity than the current DSM-IV symptom counts.
In the second approach, we adopted a complementary person-centered statistical approach (Bergman & Magnusson, 1997; von Eye & Bergman, 2003). The hypotheses in this approach were that 1) at least three subgroups, or “subtypes,” within ADHD would be formed: a general ADHD group, a specific hyperactivity-impulsivity group, and a specific inattention group and 2) the specific hyperactivity-impulsivity and specific inattention groups would exhibit distinct profiles in relation to child problem behaviors, cognitive control, and personality traits with more differentiated associations than DSM-IV subtypes.
METHOD
Participants
Overview
Participants were 548 children (321 boys), 6 to 18 years old, recruited from the community and then evaluated for study eligibility and diagnostic status. Children were initially included in one of two groups: ADHD (n=302) and non-ADHD comparison youth (“controls,” n=199). Forty-seven additional children who were classified as having situational or sub-threshold ADHD were included to provide more complete coverage of the dimensional trait space of ADHD (Sherman et al., 1997). The ADHD group included 110 children with ADHD-PI (i.e., met criteria for six or more inattentive symptoms, plus impairment, onset, and duration, and never in the past met criteria for combined type) and 192 children with ADHD-C (i.e., met criteria for six or more inattentive symptoms and six or more hyperactive-impulsive symptoms, plus impairment, onset, and duration). The current sample included no children with the hyperactive-impulsive ADHD subtype, fairly typical in this age range (e.g., Lahey et al., 2005). As shown in Table 1, 161 children met DSM-IV criteria for ODD, and 19 were diagnosed with CD. Forty one met criteria for Major Depressive Disorder (lifetime), 13 for Dysthymia (lifetime), and 45 for Generalized Anxiety Disorder (lifetime). Children came from 468 families; 80 families had two children in the study. All families completed informed consent.
Table 1.
Descriptive Statistics of Sample
| ADHD n=302 |
Control n=199 |
Total N=5481 |
|
|---|---|---|---|
| Boys n(%) | 204(67.5) | 96(48.2) | 321(58.6)** |
| Ethnic Minority n(%) | 78(25.8) | 54(27.1) | 144(26.3) |
| Age | 11.32(2.93) | 12.5(3.24) | 11.67(3.06)** |
| IQ | 110.33(14.92) | 103.78(13.90) | 106.2(14.7)** |
| Family Income | 62643(67080) | 75244(51109) | 66694(59532)* |
| ADHD-Cn(%) | 192(63.6) | -- | 192 (35)** |
| ADHD-PI n(%) | 110(36.4) | -- | 110(20.1)** |
| ODDn(%) | 118(39.1) | 26(13.1) | 161(29.4)** |
| CD n(%) | 18(6) | 1(.5) | 19(3.5)** |
| Inattentive Sx (P+T) | 6.02(2.34) | .41(1.04) | 3.77(3.32)** |
| Hyperactive Sx (P+T) | 6.35(2.38) | .53(1.22) | 4.03(3.44)** |
| Inattentive Sx (P) | 18.03(5.03) | 3.23(3.4) | 11.93(8.41)** |
| Hyperactive Sx (P) | 11.97(7.23) | 2.04(2.21) | 7.9(7.48)** |
| Inattentive Sx (T) | 14.89(6.89) | 2.36(3.18) | 9.68(8.27)** |
| Hyperactive Sx (T) | 9.85(7.94) | 1.35(2.36) | 6.37(7.49)** |
Note.
p<.05.
p<.01, via t-tests or chi-squares.
Forty-seven children were identified as having situational ADHD or were screened out of the study at a later point in time, but were included in study analyses because they had data on traits and comorbid psychopathology. ADHD-C=ADHD combined subtype. ADHD-PI=ADHD, predominantly inattentive subtype. ODD=Oppositional-Defiant Disorder. CD=Conduct Disorder. (P+T)=Parent+teacher rated symptoms using 0–1 rating system. (P)=Parent-rated symptoms using 0–3 rating scale on ADHD-RS. (T)=Teacher-rated symptoms using 0–3 rating scale on ADHD-RS.
Recruitment and Identification
A broad community-based recruitment strategy was used, with mass mailings to parents in local school districts, public advertisements, as well as flyers at local clinics. Families who volunteered then passed through a standard multi-gate screening process to identify cases and non-cases eligible for the study. At Stage 1, all families were screened by phone to rule out youth prescribed long-acting psychotropic medication (e.g. antidepressants), neurological impairments, seizure history, head injury with loss of consciousness, other major medical conditions, or a prior diagnosis of mental retardation or autistic disorder, as reported by parent.
At Stage 2, parents and teachers of remaining eligible youth completed the following standardized rating scales: Child Behavior Checklist/Teacher Report Form (CBCL/TRF; Achenbach, 1991) and the ADHD Rating Scale (ADHD-RS; DuPaul et al., 1998). In addition, parents completed a structured clinical interview to ascertain symptom presence, duration, and impairment. Parents and teachers were instructed to rate children’s behavior when not taking psychostimulant medication.
The diagnostic interview used was dependent on the year of data collection. For participants who participated between 1997 and 2001 (N=218), the Diagnostic Interview Schedule for Children (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) was completed with the parent by telephone or during on-campus visits. A trained graduate student or advanced undergraduate with at least ten hours of training administered the DISC-IV. Fidelity to interview procedure was checked by having the interview recorded with five percent reviewed by a certified trainer. For children who were administered the DISC-IV and met duration, onset (age 7), and impairment criteria for DSM-IV ADHD, a modified “or” algorithm was used to establish the diagnostic group and to create the symptom count. Teacher-reported symptoms on the ADHD-RS (i.e., items rated as a “2” or “3” on the 0 to 3 scale) could be added to the parent-endorsed symptom total, up to a maximum of two additional symptoms, to get the total number of symptoms. This approach was adopted to maximize similarity to the methods used when establishing the DSM-IV cut points as valid (Lahey et al., 1994) while avoiding the over-identification that might occur from an unrestricted “or” count. Children failing to meet cut-offs for all parent and teacher ADHD rating scales at the 80th percentile and having four or fewer symptoms of ADHD with the “or” algorithm were considered controls. However, those in the undefined range were retained in the sample for analyses of the full range of symptoms.
For children who participated from 2002 to 2008, youth and their primary caregiver completed the Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS-E; Puig-Antich & Ryan, 1986). The data from the interviews and parent and teacher rating scales were then presented to a clinical diagnostic team consisting of a board certified child psychiatrist and licensed clinical child psychologist to implement a best-estimate diagnostic procedure. They were allowed to use the same “or” algorithm described above in their diagnostic decision making. Their agreement rates were acceptable for ADHD diagnosis, subtypes, and current ODD and CD (all kappas ≥ .89).
Pooling the data across families that received the KSADS and the DISC was justified based on our analysis of agreement between the two methods in 430 youth for whom a parent completed both a KSADS and a DISC-IV. The two interviews had adequate agreement for total number of symptoms (inattention, ICC=.88; hyperactivity, ICC=.86), presence of six or more symptoms of ADHD (kappa=.79), presence of impairment (kappa=.64), and presence of ADHD (defined as six or more symptoms + cross situational impairment in each interview for purposes of computing agreement; kappa=.79).
Measures
Symptom Counts
Maternal report on ADHD symptoms was available via report on diagnostic interview, and maternal and teacher report on ADHD symptoms was available via report on the ADHD-RS. Confirmatory factor analyses of the bifactor ADHD model utilized parent and teacher report symptom counts, using parent report on diagnostic interview and teacher report on the ADHD-RS, integrated using the “or” algorithm (as discussed above and in Lahey et al., 1994).
Child Problem Behaviors
Child problems behaviors, including anxiety/depression, withdrawal/depression, somatic complaints, social problems, rule-breaking behavior, and aggressive behaviors, were assessed using maternal report on the Child Behavior Checklist (CBCL; Achenbach, 1991). The CBCL is a well-validated instrument that provides valid and reliable information about dimensional and empirically-based symptoms of psychopathology (Achenbach, Dumenci, & Rescorla, 2003).
Cognitive Control
Children completed all cognitive control testing after a 24- to 48-hour medication washout, depending on nature of the preparation, to equal at least 5 half lives. In order to measure response inhibition and response variability, the tracking version of the Stop Task was administered. The tracking version of the Stop Task, a well-validated computer task with alpha reliability higher than .8 (Band, van der Molen, & Logan, 2003; Logan, 1994), measures the ability to effortfully inhibit an automatic key press following a tone. A measure of inhibitory control, stop signal reaction time, was computed by subtracting mean stop signal latency from mean go response time. A response variability measure was obtained, defined as the within-child variability of the reaction time on the “go” trials (Russell et al., 2006). In order to measure speed and set-shifting, the Trailmaking Task, a subtest of the Halstead-Reitan Neuropsychological Battery, was administered in which the child is required to rapidly draw a line between alternating numbers and letters in ascending order. Widely used in neuropsychological research, the outcome measure of the task was set-shifting, measured as time to complete and number of errors made during the more difficult Trails B Task. (Reitan & Wolfson, 1985; Spreen & Strauss, 1991); time to complete Trails A served as a measure of speed.
Temperament and Personality Traits
Parents completed the common language version of the California Q-Sort (Caspi et al., 1992) and a short form of the Early Adolescent Temperament Questionnaire (EATQ; Capaldi & Rothbart, 1992). The CCQ is a typical Q-Sort consisting of 100 cards which must be placed in a forced-choice, nine-category, rectangular distribution. The rater (in this case, the mother) describes the child by placing descriptive cards in one of the categories, ranging from one (least descriptive) to nine (most descriptive). To measure the Big Five Factors, scales developed by John et al. (1994) were used. To measure reactive control, resiliency, and negative emotionality, scales developed by Eisenberg et al (2003; personal communication, 2006) were used (e.g., reactive control, “is shy and reserved;” resiliency, “is resourceful in initiating activities;” negative emotionality, “cries easily”). A composite score was generated by reverse-scoring selected items and computing the average. Scale reliabilities were all above .70 with the exception of the scale for openness (α=.56). To provide a measure of effortful control, mothers completed a short form of the Early Adolescent Temperament Questionnaire (EATQ; Capaldi & Rothbart, 1992). The EATQ Parent Report-Revised consists of 62 items describing child temperament characteristics. The questionnaire instructions consist of asking the parent to rate how well the statements describe her child on a scale from 1 (almost always untrue of the child) to 5 (almost always true of the child), yielding 10 scales. In the current study, the effortful control scale from the EATQ was utilized (Eisenberg et al., 1996). Alpha reliability was acceptable (.84).
Data Analysis
Confirmatory factor analysis for the bifactor ADHD model was conducted on mother- and teacher-rated ADHD symptoms (described above) using the Mplus software package (Muthén & Muthén, 2008), as fully described in Martel, von Eye, and Nigg (2010). The bifactor model of ADHD shown in Figure 1 exhibited good fit to the data based on the comparative fit index of .99, root mean square error of approximation of .05, and CMIN/df of 2.43, although the chi-square statistic was significant (χ2[59]=143.18, p<.01), and the bifactor model exhibited better fit to the data compared to one-factor, two-factor, three-factor, and second-order factor models (e.g., all other models’ RMSEA were .11 or above; see Martel et al., 2010). It should be noted that a bifactor model with orthogonal factors was also tested, but exhibited poor fit to the data (see Martel et al., 2010). However, based on theoretical grounds, the non-orthogonal model was retained as representing a conceptualization of ADHD consistent with partially distinct pathways. Based on the pattern of factor loadings in the bifactor model, which change slightly based on the entry order of symptoms in the factor analysis, these latent factors were conceptualized as representing “s” inattention (or more specifically poor sustained effort), “s” hyperactivity-impulsivity (or overactivity), and “g” ADHD (or throughful attention + overactivity). These factor scores from this model were subsequently saved.
Bivariate correlations were then calculated between the ADHD latent factors scores (i.e., specific inattention, specific hyperactivity-impulsivity, and general ADHD) and child problem behaviors, cognitive control, personality traits, and the genetic risk composite. The same correlations were then repeated with inattentive, hyperactive-impulsive, and total ADHD symptom counts, as defined in DSM-IV, as a comparison. In order to decrease the likelihood of Type I error due to the number of conducted correlations, statistical significance is only interpreted at the .01 level (.05/3 due to three sets of correlations conducted with specific inattention, specific hyperactivity-impulsivity, and general ADHD).
Person-centered analysis of the latent factor scores was conducted via latent profile analysis. Model fit was compared using log-likelihood, Akaike information criteria (AIC), Bayes information criteria (BIC), and entropy. Smaller values of log-likelihood, AIC, and BIC indicate better fit to the data or increased probability of replication, and higher values of entropy reflect better distinctions between groups (Kline, 2005). Because some evidence suggests that the BIC performs best of the information criterion indices (Nylund, Asparouhov, & Muthén, 2007), BIC was prioritized.
External validation of the best-fitting profile solution was conducted via comparison of mean group differences in external validation measures, evaluated using multivariate analysis of variance, followed by corrected Tukey posthoc analyses.
RESULTS
External Validation of Group-Based ADHD Latent Factor Scores
Bivariate correlations were calculated between ADHD latent factor scores, DSM-IV ADHD symptom counts, and child problem behaviors, cognitive control, personality traits, and genetic risk. As shown in Table 2, the ADHD latent factors exhibited a more nuanced pattern of associations compared to ADHD symptom counts. The specific hyperactivity-impulsivity and the general ADHD factors were relatively more common in boys compared to girls and associated with younger age. The specific inattention factor was associated with older age.
Table 2.
Bivariate Correlations Among Psychopathology, Cognitive Control, Traits, and Parent- and Teacher-Rated Specific and General ADHD Latent Factor Scores
| “s” Inattention (Symptoms) | “s” Hyperactive-Impulsive (Symptoms) | “g” ADHD (Symptoms) | |
|---|---|---|---|
| Males (Mean) | −.08(4.49**) | .14**(3.45**) | .22**(9.22**) |
| Females (Mean) | −.08(2.76) | −.13(3.18) | −.11(5.80) |
| Age | .15**(−.27**) | −.28**(−.25**) | −.31**(−.27**) |
| Psychopathology | |||
| Anxiety/depression | .03(.21**) | .28**(.30**) | .20**(.27**) |
| Withdrawal/depression | .15*(.10) | .11(.08) | .01(.09) |
| Somatic complaints | .09(.18**) | .19**(.22**) | .10(.21**) |
| Social problems | .03(.38**) | .43**(.44**) | .35**(.42**) |
| Rule-breaking behavior | −.02(.47**) | .53**(.52**) | .43**(.51**) |
| Aggressive behavior | −.06(.47**) | .56**(.57**) | .47**(.54**) |
| Cognitive Control | |||
| Response inhibition | −.03(.28**) | .29**(.27**) | .26**(.28**) |
| Response variability | −.03(.33**) | .33**(.32**) | .29**(.33**) |
| Trail B Time | .03(.14**) | .14**(.15**) | .11*(.15**) |
| Trails B Errors | .003(.17**) | .18**(.18**) | .15**(.18**) |
| Trails A Time | .06(.10*) | .11*(.12**) | .06(.11**) |
| Traits | |||
| Neuroticism | .14**(.26**) | .24**(.27**) | .13**(.27**) |
| Extraversion | −.24**(.23**) | .29**(.31**) | .36**(.28**) |
| Agreeableness | .14**(−.40**) | −.46**(−.44**) | −.45**(−.43**) |
| Conscientiousness | −.19**(−.65**) | −.64**(−.66**) | −.44**(−.67**) |
| Effortful Control | −.08(−.45**) | −.44**(−.44**) | −.31**(−.46**) |
| Reactive Control | .18**(−.49**) | −.54**(−.55**) | −.53**(−.53**) |
| Resiliency | −.16**(−.39**) | −.37**(−.39**) | −.23**(−.40**) |
| Negative Emotionality | .02(.35**) | .39**(.40**) | .31**(.39**) |
| Genetic Risk | |||
| Genetic Risk Composite | −.01(.10*) | .09*(.10*) | .08(.10*) |
Note.
p<.05.
p<.01.
Correlations with latent factor scores. ( ) Correlations with DSM-IV ADHD symptom counts.
As shown in Table 2, the ADHD latent factor scores showed differential associations with child problem behaviors, but the DSM-IV ADHD symptom counts did not. Specific hyperactivity-impulsivity and general ADHD were significantly associated with increased anxiety/depression (r=.28, .20, p<.01 respectively), social problems (r=.43, .33, p<.01), rule-breaking behavior (r=.53, .43, p<.01), and aggression (r=.56, .47, p<.01 respectively). In contrast, specific inattention was only significantly associated with increased withdrawal/depression (r=.15, p<.05). Inattentive, hyperactive-impulsive, and total ADHD symptoms exhibited significant associations with all child problem behaviors except withdrawal/depression.
The ADHD latent factor scores showed differential associations with child cognitive control, but again the ADHD symptom counts did not. The specific hyperactivity-impulsivity factor and general ADHD factor exhibited significant associations with cognitive control. Specific hyperactivity-impulsivity and general ADHD were significantly associated with worse response inhibition (r=.29, .26; p<.01), increased response variability (r=.34, .29; p<.01), and worse set-shifting (r=.14, .11 time; r=18, .15 errors; all p<.05). In contrast, inattentive, hyperactive-impulsive, and total ADHD symptoms showed significant associations with all indices of cognitive control.
Personality traits exhibited somewhat differential relations with the ADHD factor scores, but the DSM-IV ADHD symptom counts did not. Specific inattention, specific hyperactivity-impulsivity, and general factors of ADHD exhibited uniform associations with low resiliency (r=−.16, −.37, −.23, p<.01 respectively), low conscientiousness (r=−.19, −.64, −.44, p<.01), and high neuroticism (r=.14, .24, .13, p<.01). Specific hyperactivity-impulsivity and general ADHD were additionally associated with low effortful control (r=−.44, −.31, p<.01 respectively) and high negative emotionality (r=.39, .31, p<.01). However, some dissociation in relations was also noted. Specific inattention was associated with high reactive control (r=.18, p<.01), high agreeableness (r=.14, p<.01), and low extraversion (r=−.24, p<.01), while specific hyperactivity-impulsivity and general ADHD were associated with the reverse profile: low reactive control (r=−.54, −.53, p<.01 respectively), low agreeableness (r=−.46, −.45, p<.01), and high extraversion (r=.29, .36, p<.01). In contrast, DSM-IV ADHD symptom counts exhibited significant associations with all personality traits, and the direction of the correlations was the same for inattentive, hyperactive-impulsive, and total ADHD symptoms.
Person-Centered Analysis of Latent Factor Scores
Latent profile analysis evaluating two through six profile solutions was conducted on the three latent factor scores. As shown in Table 3, model fit improved as the number of profiles increased, up to the five profile solution. Beginning at six profiles, model fit declined, particularly as measured by the BIC which was the prioritized fit index. The five profile solution scores were retained for further analysis. Based on descriptive statistics, the five profiles were labeled as follows: “low symptoms,” “specific inattention,” “normative symptoms,” “general ADHD,” and “general ADHD + specific hyperactivity-impulsivity.” There appeared to be three main subgroups within the ADHD diagnostic category: “specific inattention,” “general ADHD,” and “general ADHD+specific hyperactivity-impulsivity;” thus, these three profiles were considered as potential ADHD subtypes during the external validation analyses. Most of the DSM-IV-defined ADHD-C subtype was split between the “general ADHD” and “general ADHD+specific hyperactivity-impulsivity” profile groups, whereas most of the DSM-IV-defined ADHD-PI subtype fell into the “specific” inattention profile group. There were more boys in the “general ADHD+specific hyperactivity-impulsivity” profile group compared to the other groups. Further, the “general ADHD+specific hyperactivity-impulsivity” and “general ADHD” groups were relatively younger than the other groups and the “specific inattention” profile group was relatively older than the other ADHD profile groups.
Table 3.
Latent Profile Analysis Fit Indices and Five-Profile Descriptive Statistics
| Loglikelihood | AIC | BIC | entropy | |
|---|---|---|---|---|
| 2-profile | −1103.34 | 2226.68 | 2269.44 | .88 |
| 3-profile | −947.22 | 1922.44 | 1982.32 | .91 |
| 4-profile | −907.70 | 1851.39 | 1928.37 | .89 |
| 5-profile | −785.75 | 1615.50 | 1709.59 | .91 |
| 6-profile | −785.75 | 1623.50 | 1734.69 | .92 |
| n | inatt | hyper | ADHD | ADHD% | ADHD-PI/C% | |
|---|---|---|---|---|---|---|
| profile 1 | 160 | −.10 | −.56 | −.61 | 6.85 | 3.75/.63 |
| profile 2 | 63 | .95 | −.10 | −.65 | 93.55 | 66.67/1.59 |
| profile 3 | 135 | −.05 | .05 | .09 | 62.28 | 20/17.04 |
| profile 4 | 101 | −.26 | .48 | .71 | 95.65 | 3.96/62.38 |
| profile 5 | 73 | −.71 | .76 | 1.31 | 97.01 | 4.11/61.64 |
Note. ADHD%=percentage of children with ADHD within each profile group. ADHD-PI/C%=percentage of children in each profile group with ADHD-PI/ADHD-C.
External Validation of Person-Centered Latent Profiles
Multivariate analyses of variance (MANOVA) were conducted to examine latent profile and DSM-IV subtype differences in child problem behaviors, cognitive control, and personality traits, examined separately, with corrected Tukey posthoc comparisons. Significant multivariate bifactor profile differences were evident for child problem behaviors (F[24,1156]=6.51; p<.01), cognitive control (F[16,1716]=4.56; p<.01), and personality traits (F[32,1280]=6.87; p<.01), and significant multivariate DSM-IV subtype differences were evident for child problem behaviors (F[16,600]=34.18; p<.01), cognitive control (F[8,864]=4.62; p<.01), and personality traits (F[16,638]=11.20; p<.01). As shown in Table 4, the general ADHD and general ADHD + specific hyperactive-impulsivity groups exhibited elevated social problems, rule-breaking behaviors, and aggressive behaviors, compared to the group with low symptoms (all p<.01). The general ADHD, general ADHD + specific hyperactivity-impulsivity, and specific inattentive groups all exhibited elevated anxiety/depression and somatic complaints compared to the group with low symptoms (p<.01). As shown in Table 5, the DSM-IV ADHD subtypes exhibited a similar pattern of results with the ADHD-PI subtype exhibiting levels of social problems, rule-breaking behaviors, and aggressive behaviors intermediate that of the ADHD-C subtype and control groups, and both ADHD subtypes exhibiting elevated anxiety/depression and somatic complaints compared to controls.
Table 4.
Latent Profile External Validation and Correlates
| Low Symptoms | Inattention | Normative Symptoms | ADHD | ADHD+hyper | |
|---|---|---|---|---|---|
| Mean (standard deviation) | |||||
| Males (percentage) | 45.22 | 53.97 | 59.40 | 63.37 | 82.19** |
| Age | 12.49(3.14)a | 12.43(3)a | 11.77(2.98)a | 10.81(2.89)b | 9.90(2.28)b** |
| Psychopathology | |||||
| Anxiety/depression | 2.07(2.21)a | 3.93(3.54)b | 4.60(3.86) | 4.66(3.36)b | 5.12(3.97)b** |
| Withdrawal/depression | 1.80(2.37) | 2.82(2.94) | 2.80(2.75) | 2.3(2.71) | 2.58(2.98) |
| Somatic complaints | 1.11(1.78)a | 2.68(3.47)b | 2.32(2.31) | 2.79(3.26)b | 2.09(2.27)b** |
| Social problems | 1.32(1.86)a | 2.73(2.55) | 3.15(2.93) | 4.77(3.58)b | 5.33(3.95)b** |
| Rule-breaking | .98(1.46)a | 2.61(2.28) | 3.31(3.35) | 5.28(3.62)b | 4.91(3.48)b** |
| Aggression | 2.26(3.59)a | 6.48(5.31) | 7.33(5.36) | 11.98(6.66)b | 12.12(8.53)b** |
| Cognitive Control | |||||
| Trails A Time | 22.71(.89)a | 28.83(1.42)b | 23.82(.96)a | 26.46(1.12)a | 26.19(1.30)a** |
| Trails B Time | 49.96(28.54)a | 57.62(32.71) | 58.26(45.53) | 59.19(44.99) | 67.56(54.23)b |
| Trails B Errors | .44(.10)a | .67(.17) a | .60(.11) a | .65(.13)a | 1.11(.15)b* |
| SSRT | 243.46(96.91)a | 304.54(167.57)a | 295.05(140.14)a | 332.03(152.99)b | 359.25(177.53)b** |
| RT variability | 148.43(43.29)a | 167.87(55.85)a | 166.58(64.91)a | 192.41(66.63)b | 196.17(61.57)b** |
| Traits | |||||
| Neuroticism | 4.06(1.32)a | 4.70(1.36) | 4.43(1.28) | 4.58(1.22)b | 4.48(1.08)b* |
| Extraversion | 5.37(1.13)a | 5.50(1.28) | 5.60(1.50) | 6.40(1.26)b | 6.63(1.25)b** |
| Agreeableness | 6.92(1.03)a | 6.38(1.21) | 6.12(1.21) | 5.47(1.26)b | 5.47(1.30)b** |
| Conscientiousness | 6.17(1.43)a | 4.21(1.62) | 4.57(1.39) | 3.96(1.33)b | 3.96(1.22)b** |
| Effortful control | 3.46(.55)a | 2.78(.68) | 3.01(.69) | 2.71(.66)b | 2.61(.74)b** |
| Reactive control | 5.10(.87)a | 4.68(1.05) | 4.67(1.07) | 3.71(.88)b | 3.53(.99)b** |
| Resiliency | 6.02(.96)a | 5.47(.94) | 5.62(1.11) | 5.34(.97)b | 5.44(.99)b** |
| Negative emotion | 3.76(1.28)a | 4.49(1.23) | 4.45(1.34) | 4.58(1.27)b | 4.80(1.17)b** |
Note.
p<.05;
p<.01, via chi-square or MANOVA. Subscripts indicate significant differences,
Table 5.
ADHD Subtype External Validation and Correlates
| Control | ADHD-Inattentive | ADHD-Combined | |
|---|---|---|---|
| Mean (standard deviation) | |||
| Males (percent) | 50.81 | 50.91 | 67.19 |
| Age | 11.95 | 12.35 | 10.81 |
| Psychopathology | |||
| Anxiety/depression | 2.80(2.90)a | 4.32(3.54)b | 5.03(3.97)b** |
| Withdrawal/depression | 2.18(2.72) | 2.62(2.55) | 2.73(2.80) |
| Somatic complaints | 1.41(2.1)a | 2.66(2.66)b | 2.67(3.19)b** |
| Social problems | 1.87(2.52)a | 2.89(2.67)b | 4.92(3.59)c** |
| Rule-breaking | 1.54(1.81)a | 2.96(2.45)b | 5.24(3.99)c** |
| Aggression | 3.76(4.85)a | 6.34(4.85)b | 11.86(7.26)c** |
| Cognitive Control | |||
| Trails A Time | 23.77(9.40) | 26.58(10.66) | 25.50(11.03) |
| Trails B Errors | .50(1.13)a | .61(.91) | .86(1.39)b** |
| SSRT | 271.62(124.52)a | 281.09(142.09)a | 343.41(165.05)b** |
| RT variability | 161.38(57.07)a | 161.41(53.70)a | 188.21(65.23)b** |
| Traits | |||
| Neuroticism | 4.12(1.28)a | 4.76(1.29)b | 4.59(1.17)b** |
| Extraversion | 5.56(1.31)a | 5.54(1.41)a | 6.42(1.30)b** |
| Agreeableness | 6.49(1.23)a | 6.31(1.16)a | 5.53(1.31)b** |
| Conscientiousness | 5.58(1.58)a | 4.08(1.40)b | 3.90(1.23)b |
| Effortful control | 3.23(.71)a | 2.86(.63)b | 2.69(.69)b** |
| Reactive control | 4.86(1.08)a | 4.62(.97)a | 3.68(.94)b** |
| Resiliency | 5.93(.97)a | 5.35(1.07)b | 5.36(.98)b** |
| Negative emotion | 4.03(1.33)a | 4.53(1.30)b | 4.72(1.20)b** |
Note.
p<.05;
p<.01, via chi-square or MANOVA. Subscripts indicate significant differences, based on posthoc Tukey tests.
The bifactor profile-based ADHD groups exhibited a distinct profile of cognitive control deficits. While the specific inattentive group exhibited significantly slower cognitive speed than the other groups, the general ADHD + specific hyperactive-impulsive group exhibited worse set-shifting, and the general ADHD and general ADHD + specific hyperactive-impulsive groups exhibited significantly worse response inhibition and greater response variability. The DSM-IV ADHD subtype comparison did not indicate such a differentiated profile; the ADHD-C subtype exhibited significantly worse performance on all measures except for cognitive speed, on which there were no subtype differences.
Finally, the personality trait profiles of the groups were as expected with the general ADHD and general ADHD + specific hyperactive-impulsive groups exhibiting worse, or more extreme, personality trait profiles (i.e., lower effortful/reactive control, resiliency, higher extraversion, and lower agreeableness and conscientiousness) compared to the low symptoms group with the specific inattention group exhibiting an intermediate profile between the extreme general ADHD and general ADHD + specific hyperactive-impulsive groups and the intact low symptoms group. For the DSM-IV ADHD subtype comparisons, neuroticism, conscientiousness, effortful control, resiliency, and negative emotionality were significantly worse in children with ADHD versus controls. Children with ADHD-C had higher extraversion, lower agreeableness, and less reactive control than control children and children with ADHD-PI.
DISCUSSION
The present study provided external validation of the newly-supported bifactor structural model of ADHD (Martel, von Eye, & Nigg, 2010; Toplak et al., 2009) using two approaches: (1) a continuous symptom severity approach using latent factor scores, similar to ADHD symptom domains, and (2) a categorical subtype approach using profiles derived from the latent factor scores, similar to subtypes. The continuous and categorical extensions of the bifactor ADHD model were then evaluated via examination of their utility in explaining heterogeneity within ADHD in relation to child problem behaviors, cognitive control, and temperament and personality traits and as compared to DSM-IV ADHD symptom counts and subtypes. Using a continuous approach, specific inattention (or poor sustained attention, based on item loadings) exhibited a unique pattern of associations and was associated with withdrawal/depression. In contrast, specific hyperactivity-impulsivity (or overactivity, based on item loadings) and general ADHD were associated with anxiety/depression, social problems, rule-breaking and aggressive behavior. Specific inattention was associated with high reactive control, high agreeableness, and low extraversion, while specific hyperactivity-impulsivity and general ADHD were associated with low reactive control, low agreeableness, and high extraversion. Using a subtype approach, individuals with high specific inattention exhibited slower speed-based cognitive performance compared to individuals with other ADHD bifactor subtypes. While these patterns of association were reassuringly similar to patterns seen with a DSM-IV model, the associations seen using the bifactor model indices were more differentiated than those seen using DSM-IV-based indices. Thus, these findings provide support for the validity of the bifactor ADHD model in that it seems to provide a better parsing of DSM-IV ADHD heterogeneity, consistent with a partially distinct dual-pathway model of ADHD (Nigg, 2006; Sonuga-Barke, 2005).
Person-centered data analysis of general ADHD, specific inattention, and specific hyperactive-impulsive latent factors revealed five groups of children across those with and without ADHD: those with low symptoms, high specific inattention, normative levels of symptoms, general ADHD, and general ADHD + specific hyperactivity-impulsivity. Within the ADHD diagnostic category, there appeared to be three “subtypes: high specific inattention,” general ADHD, and general ADHD + specific hyperactivity-impulsivity. Children in the specific inattention group with low “g” ADHD were characterized by a different cognitive profile than children in the general ADHD and general ADHD+ specific hyperactivity-impulsivity groups. Children with specific inattention appear to be slower at completing speeded cognitive tasks, in line with the conception of a group of children with ADHD characterized by a restrictive inattentive presentation as in the proposed DSM-5 criteria (dsm5.org) and similar to the restrictive inattentive or “ADD” group studied in this sample in other reports (Carr et al., 2010; Goth-Owens et al., 2010) and proposed by McBurnett, Pfiffner, & Frick (2001). In contrast, the general ADHD and general ADHD + specific hyperactive-impulsive groups exhibited a more characteristic cognitive profile of impaired set-shifting, poor response inhibition, and greater response variability.
The three latent profile subgroups found in the current study appear to be substantively distinct from the current DSM-IV ADHD subtypes, particularly in regard to their cognitive profiles. The DSM-IV ADHD-C subtype exhibited worse cognitive performance than ADHD-PI and non-ADHD children. In contrast, children with high specific inattention exhibited slow cognitive speed, whereas children with high general ADHD exhibited the classic cognitive profile of poor response inhibition and high performance variability, and children with general ADHD liability + high hyperactivity-impulsivity additionally exhibited classic impulsivity, making many errors. Further, the current study did not find a group of children with relatively “pure” specific hyperactivity-impulsivity, rather only a group of children with specific hyperactivity-impulsivity combined with general ADHD liability.
Thus, there may be some merit in distinguishing children with “pure” inattention from children with a clinically significant number of symptoms across both domains (including those with particularly high levels of hyperactivity-impulsivity). The bifactor ADHD model here suggests that these children are characterized by poor sustained effort, consistent with conceptions of low arousal, poor attention, or perhaps sluggish cognitive tempo (Carr et al., 2010; Goth-Owens et al., 2010; McBurnett, Pfiffner, & Frick, 2001) and perhaps related to the ADHD-Restricted subtype put forward for DSM-5 (www.dsm5.org on 3/1/2011). Consideration of these different cognitive control deficit profiles associated with ADHD is also important because the nature of cognitive control deficits have an impact on children’s academic performance (Biederman et al., 2004; Klingberg et al., 2005; Rueda, Rothbart, McCandliss, Saccomanno, & Posner, 2005).
Child problem behaviors exhibited differential associations with specific and general ADHD latent factor scores, as compared to their associations with DSM-IV ADHD symptom counts. In line with previous reviews (Barkley, 2003; Milich et al., 2001), the current study found that specific inattention was uniquely associated with withdrawal/depression, while specific hyperactivity-impulsivity and general ADHD were associated with rule-breaking and aggressive behavior, as well as social problems and anxiety/mood problems. The current study extends prior work by suggesting that the specific inattention domain is specifically related to withdrawal/depression. Further, the association of rule-breaking and aggressive behaviors and social problems with hyperactivity-impulsivity may explain the high comorbidity between ADHD and other disruptive behavior problems like ODD (Angold et al., 1999; Jensen et al., 1997). Thus, it should be noted that the pattern of associations between the bifactor latent factor scores and child problem behaviors were similar to what one would expect based on prior work conducted on DSM-IV ADHD symptoms. Yet, the external validation profile is somewhat sharper and more differentiated, suggesting some improvements in conceptual explanation using the bifactor model. However, it should be noted that associations with the “s” inattentive factor were modest in nature, compared to associations with the “s” hyperactive-impulsive and “g” ADHD factor.
Personality traits showed largely expected associations with specific and general ADHD factor scores. In line with previous work on trait-symptom associations (Martel & Nigg, 2006; Nigg et al., 2002; Parker et al., 2004), all facets of ADHD (i.e., specific inattention, specific hyperactivity-impulsivity, and general ADHD) were associated with low conscientiousness, high neuroticism, and low resiliency. Specific hyperactivity-impulsivity and general ADHD were associated with low effortful control and high negative emotionality. Extraversion, agreeableness, and reactive control exhibited differential relations with specific inattention versus specific hyperactivity-impulsivity and general ADHD. Whereas high extraversion, low agreeableness, and low reactive control were associated with specific hyperactivity-impulsivity and general ADHD, these relations were reversed for specific inattention. Specific inattention was associated with low extraversion, high agreeableness, and high reactive control. This heterogeneous pattern of association between traits and ADHD facets did not emerge when DSM-IV ADHD symptom counts were examined. Yet, these results help explain prior contradictory findings regarding the association of traits with ADHD, particularly extraversion (e.g., Nigg et al., 2002).
Present study findings should be interpreted in light of several study limitations. The present study tests a bifactor model of ADHD in a community-recruited sample enriched for ADHD. This is a strength in that this type of sample is needed to validate the model. However, the model also needs to be validated using other sampling frames, including clinic referred cases and general population samples (looking at ADHD traits), as well as in other age ranges (e.g., adulthood). Orthogonal bifactor models, which exhibited poor fit in the current sample (Martel et al., 2010), should also be further evaluated, and it should be noted that orthogonal bifactor models have received support in other studies of the bifactor model of ADHD (e.g., Toplak et al., 2009). In addition, the prospective utility for utilizing general and specific ADHD latent factors must be further evaluated using a longitudinal design in order to assess the predictive power of such a method. Personality trait and child comorbid problem behavior measurement was based on mother ratings on questionnaires; teacher ratings and observational measures should also be examined. Future research should evaluate this model using additional external validation indices (e.g., course of illness, treatment response, neuroimaging correlates; Cantwell, 1992), as well as evaluate the utility of bifactor models of general psychopathology (e.g., Krueger et al., 2002; Martel et al., 2010).
Overall, the current study provides some external validation of the bifactor model of ADHD via examination of child problem behaviors, cognitive control, and personality traits in that the bifactor model appears to provide a more nuanced and accurate description of the heterogeneous group of children diagnosed with ADHD. Using variable- and person-centered data analytic strategies, specific inattention was associated with depression/withdrawal and slower cognitive task performance, as well as introversion, agreeableness, and high reactive control, whereas specific hyperactivity-impulsivity was associated with rule-breaking and aggressive behavior, social problems, a more impulsive response pattern, higher extraversion, disagreeableness, and low reactive control. These profiles merit attention during clinical assessment for ADHD and may have implications for the planning of individually-tailored intervention for this heterogeneous group of children. Finally, study results suggest future directions for the development of more homogeneous behavioral compositions that could be used to elucidate etiological genetic associations with complex behavioral phenotypes like ADHD.
Acknowledgments
This research was supported by NIH National Institute of Mental Health Grant R01-MH63146 and MH59105 to Joel Nigg and MH70542 to Karen Friderici and Joel Nigg. We are indebted to the families and staff who made this study possible.
Contributor Information
Michelle M. Martel, Psychology Department, University of New Orleans
Bethan Roberts, Psychology Department, University of New Orleans.
Monica Gremillion, Psychology Department, University of New Orleans.
Alexander von Eye, Psychology Department, Michigan State University.
Joel T. Nigg, Psychiatry Department, Oregon Health and Science University
References
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Dumenci L, Rescorla LA. DSM-oriented and empirically based approaches to constructing scales from the same item pools. Journal of Clinical Child and Adolescent Psychology. 2003;32(3):328–340. doi: 10.1207/S15374424JCCP3203_02. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D.C: American Psychiatric Association; 2000. text rev. [Google Scholar]
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology & Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Band GPH, van der Molen MW, Logan GD. Horse-race model simulations of the stop-signal procedure. Acta Psychologica. 2003;112:105–142. doi: 10.1016/s0001-6918(02)00079-3. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Attention-Deficit/Hyperactivity Disorder. In: Mash EJ, Barkley RA, editors. Child psychopathology. 2. New York: The Guilford Press; 2003. pp. 75–143. [Google Scholar]
- Barkley RA. Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis and Treatment. 3. New York: Guilford Press; 2006. [Google Scholar]
- Bergman LR, Magnusson D. A person-oriented approach in research on developmental psychopathology. Development and Psychopathology. 1997;9:291–319. doi: 10.1017/s095457949700206x. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Doyle AE, Seidman LJ, Wilens TE, Ferrero F, et al. Impact of executive function deficits and Attention-Deficit/Hyperactivity Disorder (ADHD) on academic outcomes in children. Journal of Consulting and Clinical Psychology. 2004;72(5):757–766. doi: 10.1037/0022-006X.72.5.757. [DOI] [PubMed] [Google Scholar]
- Cantwell DP. Clinical phenomenology and nosology. Child and Adolescent Psychiatric Clinics of North America. 1992;1(1):1–11. [Google Scholar]
- Capaldi DM, Rothbart MK. Development and validation of an early adolescent temperament measure. Journal of Early Adolescence. 1992;12(2):153–173. [Google Scholar]
- Carr L, Henderson J, Nigg JT. Cognitive control and attentional selection in adolescents with ADHD versus ADD. Journal of Clinical Child and Adolescent Psychology. 2010;39(6):726–740. doi: 10.1080/15374416.2010.517168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Block J, Block JH, Klopp B, Lynam D, Moffitt TE, Stouthamer-Loeber M. A “common-language” version of the California Child Q-Set for personality assessment. Psychological Assessment. 1992;4:512–523. [Google Scholar]
- Doyle AE, Faraone SV, Seidman LJ, Willcutt EG, Nigg JT, Waldman ID, Pennington BF, et al. Are endophenotypes based on measured of executive functions useful for molecular genetic studies of ADHD? Journal of Child Psychology & Psychiatry. 2005;46(7):774–803. doi: 10.1111/j.1469-7610.2005.01476.x. [DOI] [PubMed] [Google Scholar]
- DuPaul GJ, Power TJ, Anastopolous AD, Reid R. ADHD Rating Scale—IV: Checklists, Norms, & Clinical Interpretation. New York: Guilford Press; 1998. [Google Scholar]
- Eisenberg N, Fabes RA, Guthrie IK, Murphy BC, Maszk P, Holmgren R, et al. The relations of regulation and emotionality to problem behavior in elementary school children. Development and Psychopathology. 1996;8:141–162. [PubMed] [Google Scholar]
- Eisenberg N, Qhou Q, Losoya SH, Fabes RA, Shepard SA, Murphy BC, et al. The relations of parenting, effortful control, and ego control to children’s emotional expressivity. Child Development. 2003;74(3):875–895. doi: 10.1111/1467-8624.00573. [DOI] [PubMed] [Google Scholar]
- Frick PJ, Cornell AH, Bodin SD, Dane HE, Barry CT, Loney BR. Callous-unemotional traits and developmental pathways to severe conduct problems. Developmental Psychology. 2003;39(2):246–260. doi: 10.1037//0012-1649.39.2.246. [DOI] [PubMed] [Google Scholar]
- Goth-Owens TL, Martinez-Torteya C, Martel MM, Nigg JT. Processing speed weakness in children and adolescents with non-hyperactive but inattentive ADHD (ADD) Child Neuropsychology. 2010;16:577–591. doi: 10.1080/09297049.2010.485126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Martin D, Cantwell DP. Comorbidity in ADHD: Implications for research, practice, and DSM-V. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(8):1065–1079. doi: 10.1097/00004583-199708000-00014. [DOI] [PubMed] [Google Scholar]
- John OP, Caspi A, Robins RW, Moffitt TE, Stouthamer-Loeber M. The Little-Five: Exploring the nomological network of the five-factor model of personality in adolescent boys. Child Development. 1994;65:160–178. [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 2. Guilford Press; New York: 2005. [Google Scholar]
- Klingberg T, Fernell E, Olesen PJ, Johnson M, Guustafsson P, Dahlstrom K, et al. Computerized training of working memory in children with ADHD—A randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44(2):177–186. doi: 10.1097/00004583-200502000-00010. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks PM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111(3):411–424. [PubMed] [Google Scholar]
- Lahey BB, Applegate B, McBurnett K, Biederman J, et al. DSM-IV field trials for attention deficit hyperactivity disorder in children and adolescents. American Journal of Psychiatry. 1994;151(11):1673–1685. doi: 10.1176/ajp.151.11.1673. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM-IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62(8):896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Willcutt EG. Predictive validity of a continuous alternative to nominal subtypes of Attention-Deficit Hyperactivity Disorder for DSM-V. Journal of Clinical Child & Adolescent Psychiatry. 2010;39(6):761–775. doi: 10.1080/15374416.2010.517173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan GD. A users guide to the stop signal paradigm. In: Dagenbach D, Carr TH, editors. Inhibitory processes in attention, memory, and language. San Diego: Academic Press; 1994. pp. 189–239. [Google Scholar]
- Martel MM, Gremillion M, Roberts B, von Eye A, Nigg JT. The structure of childhood disruptive behaviors. Psychological Assessment. 2010;22(4):816–826. doi: 10.1037/a0020975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Nigg JT. Child ADHD and personality/temperament traits of reactive and effortful control, resiliency, and emotionality. Journal of Child Psychology and Psychiatry. 2006;47(11):1175–1183. doi: 10.1111/j.1469-7610.2006.01629.x. [DOI] [PubMed] [Google Scholar]
- Martel MM, von Eye A, Nigg JT. Revisiting the latent structure of ADHD: Is there a “g” factor? Journal of Child Psychology & Psychiatry. 2010;51(8):905–914. doi: 10.1111/j.1469-7610.2010.02232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBurnett K, Pfiffner LJ, Frick PJ. Symptom properties as a function of ADHD type: An argument for continued study of sluggish cognitive tempo. Journal of Abnormal Child Psychology. 2001;29(3):207–213. doi: 10.1023/a:1010377530749. [DOI] [PubMed] [Google Scholar]
- Milich R, Balentine AC, Lynam DR. ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. Clinical Psychology: Science and Practice. 2001;8(4):463–488. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide, Fourth Edition. Los Angeles, CA: Muthen & Muthen; 1998–2008. [Google Scholar]
- Nigg JT. What causes ADHD? Understanding what goes wrong and why. New York: The Guilford Press; 2006. [Google Scholar]
- Nigg JT, John OP, Blaskey LG, Huang-Pollock CL, Willcutt EG, Hinshaw SP, Pennington B. Big Five dimensions and ADHD symptoms: Links between personality traits and clinical symptoms. Journal of Personality and Social Psychology. 2002;83(2):451–469. doi: 10.1037/0022-3514.83.2.451. [DOI] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling. 2007;14(4):535–569. [Google Scholar]
- Parker JDA, Majeski SA, Collin VT. ADHD symptoms and personality: Relationships with the five-factor model. Personality and Individual Differences. 2004;36:977–987. [Google Scholar]
- Puig-Antich J, Ryan N. Kiddie Schedule for Affective Disorders and Schizophrenia. Pittsburgh, PA: Western Psychiatric Institute; 1986. [Google Scholar]
- Reitan RM, Wolfson D. Category test and Trailmaking test as measures of frontal lobe functions. Clinical Neuropsychologist. 1985;9:50–56. [Google Scholar]
- Rueda MR, Rothbart MK, McCandliss BD, Saccomanno L, Posner MI. Training, maturation, and genetic influences on the development of executive attention. PNAS. 2005;102(41):14931–14936. doi: 10.1073/pnas.0506897102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell VA, Oades RD, Tannock R, Killeen PR, Auerbach JG, Johansen EB, Sagvolden T. Response variability in Attention-Defict/Hyperactivity Disorder: A neuronal and glial energetics hypothesis. Behavioral and Brain Functions. 2006;(2):30. doi: 10.1186/1744-9081-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas C, Dulcan MK, Schwab-Stone M. NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): Description, differences from previous versions and reliability of some common diagnoses. Journal of American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sherman DK, Iancono WG, McGue MK. Attention-Deficit Hyperactivity Disorder dimensions: A twin study of inattention and impulsivity-hyperactivity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(6):745–753. doi: 10.1097/00004583-199706000-00010. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. Causal models of Attention-Deficit/Hyperactivity Disorder: from common simple deficits to multiple developmental pathways. Biological Psychiatry. 2005;57:1231–1238. doi: 10.1016/j.biopsych.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Spreen O, Strauss E. A compendium of neuropsychological test: Administration, norms, and scoring. New York: Oxford University Press; 1991. [Google Scholar]
- Toplak ME, Pitch A, Flora DB, Iwenofu L, Ghelani K, Jain U, Tannock R. The unity and diversity of inattention and hyperactivity-impulsivity in ADHD: Evidence for a general factor with separable dimensions. Journal of Abnormal Child Psychology. 2009;37:1137–1150. doi: 10.1007/s10802-009-9336-y. [DOI] [PubMed] [Google Scholar]
- von Eye A, Bergman LR. Research strategies in developmental psychopathology: Dimensional identity and the person-oriented approach. Development and Psychopathology. 2003;15:553–580. doi: 10.1017/s0954579403000294. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of Attention-Deficit/Hyperactivity Disorder: A meta-analytic review. Biological Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]