Abstract
Patients with cervical cancer may develop local recurrence or distant metastasis, and the rate of these events is increased in proportion to the clinical stage. Cutaneous metastasis of cervical cancer is very rare and only a few cases have been reported in Korean literature. It is common at the abdominal wall, vulva, and anterior chest wall and mainly presents as an asymptomatic dermal or subcutaneous nodule, ulcer or plaque. We herein report on an interesting case of vulval metastasis from squamous cell carcinoma of the cervix with an unusual clinical manifestation resembling lymphagioma circumscriptum.
Keywords: Uterine cervical neoplasms, Neoplasm metastasis, Vulva
INTRODUCTION
Carcinoma of the cervix is a common malignancy occurring in females worldwide, and the death rate from cervical cancer ranks in the top 10 in Korea1. Patients with cervical cancer may develop local recurrence or distant metastasis, and the rate of these events is increased in proportion to the clinical stage. Cutaneous metastasis of cervical cancer is very rare, ranging from 0.1~1.3%2, and presents mainly as an asymptomatic dermal or subcutaneous nodule, ulcer, or plaque2. We report on an interesting case of vulval metastasis from squamous cell carcinoma of the cervix with an unusual clinical manifestation resembling lymphagioma circumscriptum.
CASE REPORT
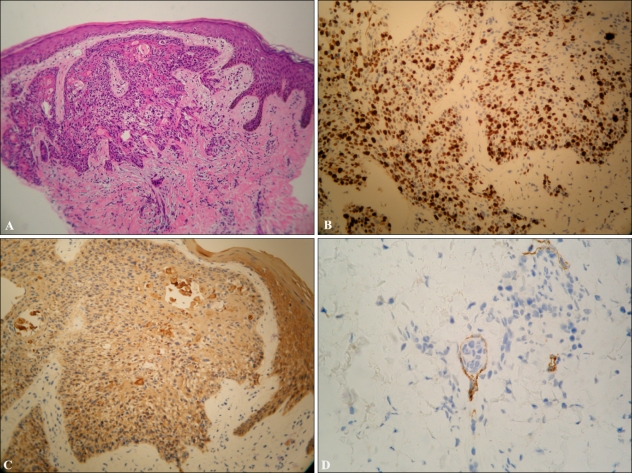
A 46-year-old female presented with a 3-week history of asymptomatic waxy and erythematous papules on the vulva. She was diagnosed as cervical cancer (FIGO stage Ib) 2 years ago and surgery was recommended. Due to her refusal of surgical treatment, she received treatment with concurrent chemoradiotherapy (8 cycles of cisplatin-paclitaxel chemotherapy with 41 radiotherapy treatments), and the result was successful. However, 9 months after the end of treatment, cervical cancer recurred and she received chemotherapy again. During 4 cycles of chemotherapy, her vulval lesion appeared. On physical examination, multiple skin-colored papules and vesicles with focal coalescence on the vulva were noted (Fig. 1). Computed tomography findings of the abdomen and pelvis showed a uterin myoma measuring 3 cm and small reactive lymph nodes on the retroperitoneum; however, no specific interval change was found, compared with one year ago. Her laboratory and simple radiologic findings were also normal, except for increased squamous cell carcinoma antigen level in serum (5.01 ng/ml, reference <2.0 ng/ml). A biopsy specimen demonstrated numerous infiltrating tumor nests in the dermis, which were composed of moderately differentiated squamous cells (Fig. 2A), consistent with her primary cervical cancer. Tumor cells expressed a high Ki-67 labeling index (≥50%) and showed positivity on pan-cytokeratin staining with a cytoplasmic pattern (Fig. 2B, C); tumor cells were also observed in the lymphatic channel (Fig. 2D). She underwent a vulvectomy and received 6 cycles of cisplatin-paclitaxel chemotherapy, and she has remained alive for 6 months after the initial diagnosis of cutaneous metastasis.
Fig. 1.
Multiple skin-colored papules and vesicles with focal coalescence on the vulva.
Fig. 2.
Infiltrating tumor nests were observed in the dermis, which were composed of moderately differentiated squamous cells (A: H&E stain, ×100). Tumor cells were positive at Ki-67 (B: ×200) with a high labeling index (≥50%) and pan-cytokeratin staining (C: ×200) with a cytoplasmic pattern; some tumor cells were observed in the lymphatic channel (D: D2-40 stain, ×400).
DISCUSSION
Cutaneous metastasis of cervical cancer is common at the abdominal wall, vulva, and anterior chest wall2; however, cases presenting at the scalp3,4, extremities5, umbilical surgical scar6,7, and drainage site8 have been reported. Only a few cases have been previously reported in Korean literature (Table 1)9-11. Most lesions present as single or multiple asymptomatic subcutaneous nodules, plaque, ulcer, or inflammatory telangiectatic areas12. However, our patient had a very unusual clinical feature, like that of lymphagioma circumscriptum.
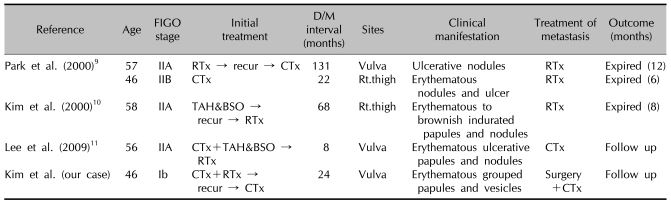
Table 1.
Cases of cutaneous metastasis of cervical cancer reported in Korean literatures
D/M interval: interval between diagnosis of cervical cancer and that of cutaneous metastasis, CTx: chemotherapy, RTx: radiotherapy, TAH&BSO: total abdominal hysterectomy and bilateral salpingo-oophorectomy.
Lymphagioma circumscriptum is a rare benign disorder of lymphatic channels in dermis characterized by the appearance of multiple small and discrete skin-colored vesicles13. Histopathologically, numerous dilated lymphatics are lined by a single layer of endothelial cells in the papillary dermis. Occurrence of lymphagioma circumscriptum of the vulva is relatively rare and the most common predisposing condition is surgery and/or radiotherapy13,14.
We first supposed lymphagioma circumscriptum due to her history of radiotherapy and complete remission after previous treatment. However, because the lesions were solid on palpation, cutaneous metastasis had to be differentiated. Her biopsy specimen showed numerous infiltrating tumor nests in the dermis, which were composed of moderately differentiated squamous cells; based on the experience of this case, not only lymphagioma circumscriptum, but also cutaneous metastasis, should be considered when the vulval lesion resembles lymphagioma circumscriptum. At onset, lymphagioma circumscriptum commonly manifests as small millimeter-sized soft clear vesicles, whereas metastatic lesions are relatively firm and often appear in papulonodular structures. Therefore, careful history taking and palpation are important in differential diagnosis.
Cutaneous spread of primary cancer occurs by direct extension, or dissemination via bloodstream or by lymphatics. In cervical cancer, tumor cells metastasize through retrograde lymphatic dissemination secondary to lymphatic obstruction2,15. Our case supports this idea that the patient showed clinical evidence of lymphatic obstruction and leg edema after radiotherapy, and the histopathology showed cancer cells in the dilated lymphatic channel.
Although skin metastasis of cervical cancer is thought to indicate a 'pre-terminal', or 'end-stage' disease, some patients survived longer than a year with treatment of a combination of surgical excision and chemotherapy or radiotherapy2,5. Our patient has also survived longer than 6 months by treatment with surgery and chemotherapy.
In summary, this is a very interesting case in that cutaneous metastasis of cervical cancer clinically resembled lymphagioma circumscriptum. In the case of multiple small clear vesicles on the vulva, lymphagioma circumscriptum is the foremost impression; however, cutaneous metastasis, particularly in the cervix of cancer patients, should be included in differential diagnosis.
References
- 1.Chung HH, Jang MJ, Jung KW, Won YJ, Shin HR, Kim JW, et al. Cervical cancer incidence and survival in Korea: 1993-2002. Int J Gynecol Cancer. 2006;16:1833–1838. doi: 10.1111/j.1525-1438.2006.00708.x. [DOI] [PubMed] [Google Scholar]
- 2.Imachi M, Tsukamoto N, Kinoshita S, Nakano H. Skin metastasis from carcinoma of the uterine cervix. Gynecol Oncol. 1993;48:349–354. doi: 10.1006/gyno.1993.1061. [DOI] [PubMed] [Google Scholar]
- 3.Park JY, Lee HS, Cho KH. Cutaneous metastasis to the scalp from squamous cell carcinoma of the cervix. Clin Exp Dermatol. 2003;28:28–30. doi: 10.1046/j.1365-2230.2003.01128.x. [DOI] [PubMed] [Google Scholar]
- 4.Maheshwari GK, Baboo HA, Ashwathkumar R, Dave KS, Wadhwa MK. Scalp metastasis from squamous cell carcinoma of the cervix. Int J Gynecol Cancer. 2001;11:244–246. doi: 10.1046/j.1525-1438.2001.00074.x. [DOI] [PubMed] [Google Scholar]
- 5.Pertzborn S, Buekers TE, Sood AK. Hematogenous skin metastases from cervical cancer at primary presentation. Gynecol Oncol. 2000;76:416–417. doi: 10.1006/gyno.1999.5704. [DOI] [PubMed] [Google Scholar]
- 6.Martínez-Palones JM, Gil-Moreno A, Pérez-Benavente MA, Martinez-Palones JM, Garcia-Giménez A, Xercavins J. Umbilical metastasis after laparoscopic retroperitoneal paraaortic lymphadenectomy for cervical cancer: a true port-site metastasis? Gynecol Oncol. 2005;97:292–295. doi: 10.1016/j.ygyno.2004.11.056. [DOI] [PubMed] [Google Scholar]
- 7.Deka D, Gupta N, Bahadur A, Dadhwal V, Mittal S. Umbilical surgical scar and vulval metastasis secondary to advanced cervical squamous cell carcinoma: a report of two cases. Arch Gynecol Obstet. 2010;281:761–764. doi: 10.1007/s00404-009-1235-5. [DOI] [PubMed] [Google Scholar]
- 8.Behtash N, Ghaemmaghami F, Yarandi F, Ardalan FA, Khanafshar N. Cutaneous metastasis from carcinoma of the cervix at the drain site. Gynecol Oncol. 2002;85:209–211. doi: 10.1006/gyno.2001.6559. [DOI] [PubMed] [Google Scholar]
- 9.Park JH, Kim JO, Kim BC, Lee KS. Two cases of cutaneous metastasis from carcinoma of cervix. Korean J Dermatol. 2000;38:1508–1511. [Google Scholar]
- 10.Kim JS, Cho CH, Park SH, Kim YS, Kim KT, Kim HC. A case of skin metastasis from uterine cervical cancer. Korean J Gynecol Oncol Colposc. 2000;11:411–415. [Google Scholar]
- 11.Lee JS, Noh HT, Rhee YE, Lee KH, Ko YB. One case of vulva metastasis from cervical squamous cell carcinoma. Korean J Obstet Gynecol. 2009;52:368–371. [Google Scholar]
- 12.Schwartz RA. Cutaneous metastatic disease. J Am Acad Dermatol. 1995;33:161–182. doi: 10.1016/0190-9622(95)90231-7. [DOI] [PubMed] [Google Scholar]
- 13.Gönül M, Cakmak SK, Soylu S, Kiliç A, Gündüz H, Gül U, et al. Lymphangioma circumscriptum of the vulva: a case report. Acta Derm Venereol. 2009;89:180–181. doi: 10.2340/00015555-0574. [DOI] [PubMed] [Google Scholar]
- 14.Stewart CJ, Chan T, Platten M. Acquired lymphangiectasia ('lymphangioma circumscriptum') of the vulva: a report of eight cases. Pathology. 2009;41:448–453. doi: 10.1080/00313020902885052. [DOI] [PubMed] [Google Scholar]
- 15.Malfetano JH. Skin metastases from cervical cancer: a fatal event. Gynecol Oncol. 1986;24:177–182. doi: 10.1016/0090-8258(86)90025-9. [DOI] [PubMed] [Google Scholar]