Abstract
Mesenteric cysts are rare abdominal tumors of unclear histologic origin, usually asymptomatic. Post-traumatic mesenteric cyst usually results as a consequence of a mesenteric lymphangitic rupture or a hematoma followed by absorption and cystic degeneration. The preoperative histological and radiological diagnosis is difficult. We present the case of a 45-year-old male patient with sizable, palpable abdominal tumor, the gradual swelling of which the patient himself combined with the blunt abdominal trauma he acquired from an opponent's knee in a football game 5 months ago.
Keywords: Traumatic mesenteric cyst, Blunt abdominal trauma, Lymphangioma, Mesothelioma
1. Introduction
Mesenteric cysts are usually benign abdominal tumors originating from developmental lymphangitic abnormalities or from their traumatic rupture.1 In adults, they are usually asymptomatic, contrary to children's cases whose symptoms can be intense. They are incidentally discovered during an image study, an exploratory laparotomy for other reasons, or for the treatment of their complications. We present the case of a 45-year-old man with sizable, palpable abdominal tumor, the swelling of which the patient combined with a blunt abdominal injury acquired by his opponent's knee in a football game 5 months ago.
2. Case presentation
A 45-year-old man arrived at the outpatient's facilities of our clinic complaining of remittent pain in the epigastrium and abdominal discomfort. He also mentioned that he was palpating a sizable abdominal mass that was gradually growing during the last 5 months. He had no medical history. He was a football player and for that reason he always followed regular medical health examinations.
The patient mentioned a collision with an opponent player during a football game 5 months ago. A strong injury on the epigastrium caused by his opponent's knee made him stop the game and quit every sport activity for a month. The post-traumatic pain decreased with an anti-inflammatory medication and it was attributed to muscle load. The pain lasted for about 20 days, however, it remained as a non specific abdominal discomfort combined with bloating.
Physical examination revealed a large, soft, palpable mass of the epigastrium extended to the right hypochondrium. Upon palpation, the mass was also transversally movable. Laboratory findings and tumor markers were within normal limits. The abdominal ultrasound (US) revealed a cystic multiloculated mass of uneven shape at the right hypochondrium (140 mm × 110 mm in diameter) extending from the liver and the pancreas towards the right kidney.Abdominal computed tomography (CT) demonstrated a cystic polylobulated lesion, 12 cm in diameter, arising from the head and from the uncinate process of the pancreas, pushing forward the mesenteric vessels and pressing the inferior vena cava (Figs. 1–3). CT findings suggested the process was rather suspicious for a mucous macrocystic neoplasm of the pancreatic parenchyma.
Figs. 1 and 2.
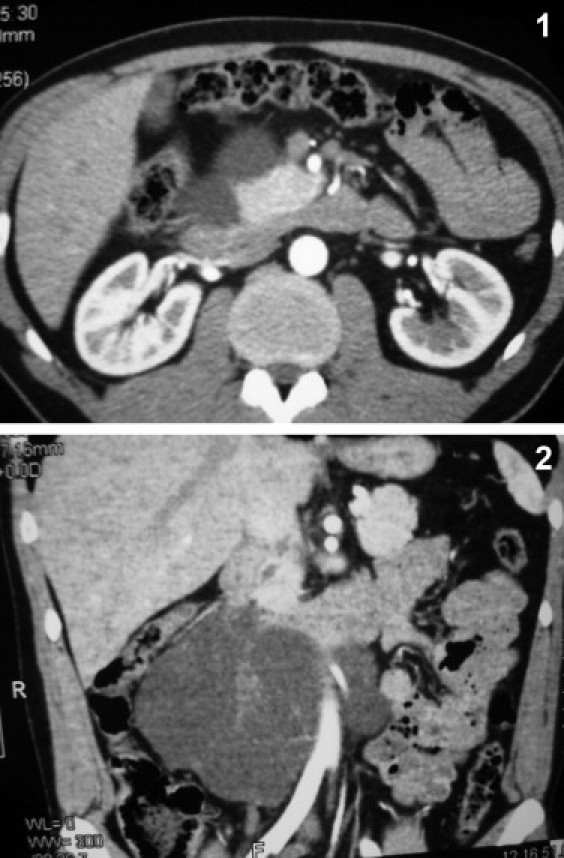
Abdominal axial and coronal CT images demonstrating a large lesion originating from the anatomic region of the head of the pancreas causing mass effect.
Fig. 3.

Large intraabdominal, multilobulated (probably cystic) mass with fine septations.
The magnetic resonance imaging (MRI) and the magnetic cholangiopagreatography (MRCP) demonstrated that the tumor was only in touch with the uncinate process, the inferior cava vein, the aorta, the lower pole of the right kidney and the superior mesenteric vessels and included in the differential diagnosis a mesenteric cyst, a lymphangioma, and a cystic mesothelioma (Fig. 4).
Fig. 4.
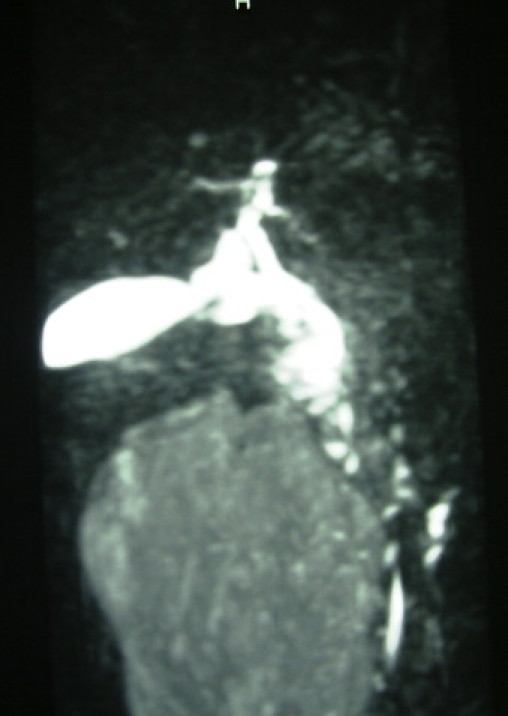
Abdominal MRI–MRCP demonstrating no filling or dilatation of the common hepatic, cystic, common bile and pancreatic duct.
The patient underwent an exploratory laparotomy. It was ascertained a sizable, yellowish, movable cystic mass, coming out of the mesentery root 1.2–2 cm on the right side of the superior mesenteric vein (Fig. 5). A total enucleation and resection of the tumor was carried out. The paracentesis of the cyst outside the operational field demonstrated a high viscosity, milk-like material. Frozen section of the speciment excluded malignancy. The biochemical analysis revealed high levels of triglycerides (12384 mg/dl), high cholesterol levels (325 mg/dl) and absence of amylase. The patient was discharged the sixth postoperative day without postoperative complications. The pathology report revealed a mesenteric cystic wall with elements of chronic inflammation, ‘foam’ macrophages, cholesterol granulomas and the absence of epithelium.
Fig. 5.
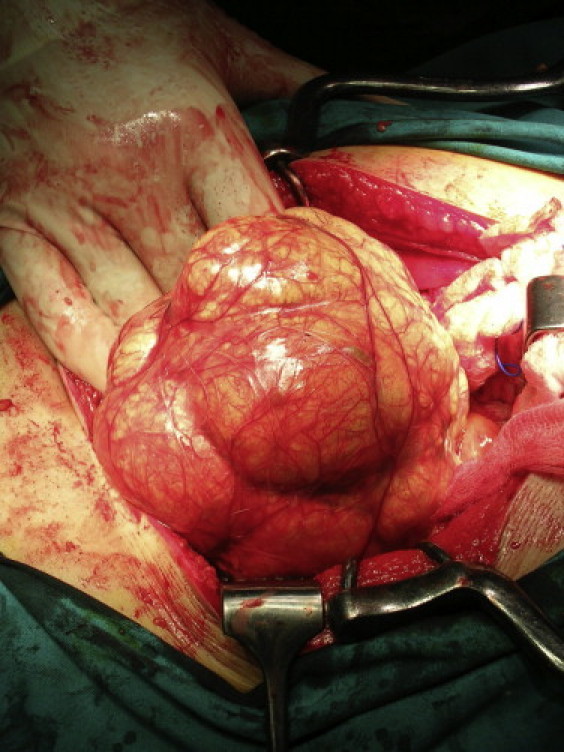
Intraoperative findings. Mesenteric multiloculated chylous cyst.
3. Discussion
Mesenteric cysts (MCs) are rare, usually benign tumors, with an incidence of 1/105,000–250,000 in hospitalized surgical patients.1 The cysts usually involve the mesentery of the ileum, the omentum, the mesocolon and the retroperitoneum.2 Mesenteric cyst was first described in 1507 by the Florentine anatomist Benevieni in a 7-year-old boy autopsy while the first successful resection was performed in 1880 by Tilaux.3,4
The limited number of cases described in the literature justifies the lack of experience in the surgical treatment and in the creation of unanimous classification of their histological origin and structure. In 1950, Bhears classified cysts in 4 groups: (1) embryonal and developmental (2) traumatic (3) neoplastic and (4) infectious.5 Actually, a classification based on histological and immunohistochemical findings, propose a distinction of the cysts in 6 groups 1) cysts of lymphatic origin (simple lymphatic cysts and lymphangioma 2) cysts of mesothelial origin (benign or malignant 3) enteric cysts 4) cysts of urogenital origine 5) dermoid cysts 6) pseudocysts (infectious or traumatic).6 The traumatic and infectious ones usually have fibrous wall, macrophage foam cells, cholesterol granulomas, absence of epithelium and histologically resemble to pancreatic pseudocysts.6 The lymphangioma and the benign mesothelioma present infiltration tendency and aggressive development. A relation between them and previous pelvic inflammations, surgery or endometriosis has been reported.7 The malignant cystic mesothelioma is the only mesenteric cystic tumor potentially malignant and presents a prominent tendency to recur after excision.6
In adults, mesenteric cysts are usually asymptomatic. Patients rarely complain of intermittent abdominal pain or painful abdominal mass. Acute abdomen due to rupture, inflammation or intestinal occlusion is an uncommon finding. On the other hand, mesenteric cysts are usually symptomatic in children, mainly the lymphangioma, with presenting symptoms similar to those of appendicitis or volvulus.8 Physical examination is often unremarkable even if an objective finding of a soft abdominal mass transversally movable has also been described.9 In our case the patient presented only recurrent abdominal pain and palpable, stable swelling mass at the epigastrium. The patient linked the presence of the mass with the previously experienced blunt abdominal trauma in a football game.
Preoperative diagnosis of MCs is difficult. Laboratory findings are usually within normal limits. The US of the abdomen reveals a hypoechogenic cystic mass with or without internal echos (diaphragms). The CT scan allows determining the size of the mass, sometimes the point of the origin, the relation to the neighboring organs and depicts better wall calcifications, however, does not highlight the correlation with the soft tissues. MRI offers more information and describes accurately the relation between the mass and the soft tissues. Furthermore, the different shots allow determining the relation among the mass, the pancreas, the liver and the ovaries in women, organs often involved in similar cystic processes.10–12 In our case, the tumor was identified by US and its extension was estimated by CT and MRI. The CT scan revealed the size of the tumor but it did not define its origin. The MRI–MRCP appeared to be specific, defining the dimensions of the tumor, its cystic component and its position with other retroperitoneal organs. The MRI–MRCP excluded that the tumor arose from the pancreas and enforced the suspicion of the mesenteric cyst.
Surgery has both diagnostic and curative role. Voluminous and symptomatic mesenteric cysts need immediate surgery in order to prevent malignancy or complication such as inflammation, rupture or obstruction. The enucleation of simple lymphatic and mesothelial cysts is usually easy and safe. On the contrary, the lymphangioma, the benign cystic mesothelioma and the malignant mesothelioma can be strongly adherents to neighboring organs or to large vessels. This fact makes their radical resection quite difficult.13–17 The resection of the intestine, pancreas and spleen is often necessary for the complete removal of the tumor. Resection of the intestine is only necessary in 1/3 of the cases while it is necessary in 50–60% of children with mesenteric cyst.18 Laparoscopic excision of MCs has also been described in many cases.18,19 Malignant mesothelioma, benign cystic mesothelioma and lymphangioma may also recur.20
In our case, the information obtained from the patient, regarding his experienced abdominal injury, made us consider the traumatic cause of the abdominal mass formation. Mesenteric injury probably caused a rupture of a lymph vessel favoring a gradual chylous leak. Imaging studies were helpful, although definitive diagnosis was posted only after the excision and the histological examination.
4. Conclusion
MC is a rare abdominal tumor usually asymptomatic. The pre-operative diagnosis is difficult and the radiologic findings are not always specific. Surgery is both diagnostic and curative. History of blunt abdominal trauma should be always taken into account when treating abdominal cystic lesions.
Contributors
EF and SM participated to the sequence alignment, researched sources for the reference and drafted the manuscript. KVL, EP took the photographs and drafted the manuscript. GA and CV helped in the interpretation of the photos and helped draft the final version of the manuscript. All authors read and approved the final manuscript form.
Conflicts of interest
The authors declare that they have no competing interests.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- 1.Kurtz M.D., Heiman T.M., Berk A.R., Holt J. Mesenteric and retroperitoneal cysts. Ann Surg. 1986;203:109–112. doi: 10.1097/00000658-198601000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saviano S.M., Fundaro S., Gelmini R., Begosi G., Perrone A., Farinneti A., Oriscuolo M. Mesenteric cystic neoformations: report of two cases. Surg Today. 1999;29(2):174–177. doi: 10.1007/BF02482245. [DOI] [PubMed] [Google Scholar]
- 3.Braquehaye J. Des Kystes du mesentery. Arch Gen. 1892:170–291. [Google Scholar]
- 4.Tilaux P., Millard P., Cyst du mesentere chez une home Bull Acad Med. 1880;7:831. [Google Scholar]
- 5.Beahrs O.H., Judd E.S., Dockerty M.B. Chylous cyst of the abdomen. Surg Clin North Am. 1950;30:1081–1096. doi: 10.1016/s0039-6109(16)33090-0. [DOI] [PubMed] [Google Scholar]
- 6.Mennemeyer R., Smith M. Multicystic, peritoneal mesothelioma: a report with electron microscopy of a case mimicking intra-abdominal cystic hygroma (lymphangioma) Cancer. 2006;44:692–698. doi: 10.1002/1097-0142(197908)44:2<692::aid-cncr2820440242>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 7.Payan H.M., Gilbert E.F. Mesenteric cyst-ovarian implant syndrome. Arch Pathol Lab Med. 1987;111:282–284. [PubMed] [Google Scholar]
- 8.Hebra A., Brown M.F., McGeehin K.M., Ross A.J., 3rd Mesenteric,omental and retroperitoneal cyst in children: a clinical study of 22 cases. South Med. 1993;86:173–176. doi: 10.1097/00007611-199302000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Caropreso P.R. Mesenteric cyst: a review. Arch Surg. 1974;108:242–246. doi: 10.1001/archsurg.1974.01350260094024. [DOI] [PubMed] [Google Scholar]
- 10.Cutillo D.P., Swayne L.C., Cucco J., Dougan H. CT and MR imaging in cystic abdominal lymphangiomatosis. J Comput Assist Tomogr. 1989;13:534–536. doi: 10.1097/00004728-198905000-00038. [DOI] [PubMed] [Google Scholar]
- 11.Stoupis C., Ros P.R., Abbitt P.L., Burton S.S., Gauger J. Bubbles in the belly: imaging of cystic mesenteric or omental masses. Radiographics. 1994;14:729–737. doi: 10.1148/radiographics.14.4.7938764. [DOI] [PubMed] [Google Scholar]
- 12.Curry C.A., Eng J., Horton K.M., Urban B., Siegelman S., Kuszyk B.S., Fishman E.K. CT of primary cystic pancreatic neoplasm: can CT be used for triage and treatement. AJM Am Roentgenol. 2001;177:469–470. doi: 10.2214/ajr.175.1.1750099. [DOI] [PubMed] [Google Scholar]
- 13.Bury T.F., Pricolo VE Malignant transformation of benign mesenteric cyst. AJG. 1994;89:2085–2087. [PubMed] [Google Scholar]
- 14.Vlazakis S.S., Gardikis S., Sanidas E., Vlachakis I., Charissis G. Rupture of mesenteric cust after blunt abdominal trauma. Eur J Surg. 2000;166:262–264. doi: 10.1080/110241500750009384. [DOI] [PubMed] [Google Scholar]
- 15.Goutsogiannis N.C., Bays D., Malamas M., Mouchtouris A. Mesothelial cyst complicated by torsion: preoperative imaging evaluation. Hepatogastroenterology. 1993;40:509–512. [PubMed] [Google Scholar]
- 16.Milliaras S., Trygonis S., Papandoniou A., Kalamaras S., Trygonis C., Kiskinis D. Mesenteric cyst of the discending colon: a case report. Acta Chir Belg. 2006;106:714–716. doi: 10.1080/00015458.2006.11679990. [DOI] [PubMed] [Google Scholar]
- 17.Ozdogan M. Acute abdomen caused by ruptured spontaneously infected mesenteric cyst. Turk J Gastroenterol. 2004;15:120–121. [PubMed] [Google Scholar]
- 18.Raghupathy R.K., Krishnamurthy P., Rajamani G., Babuji N., Diriviraj R., Mohan N.V. Intraabdominal cystic swelling in children—laparoscopic approach, our experience. J Indian Assoc Pediatr Surg. 2003;8:213–217. [Google Scholar]
- 19.Kwan E., Hung L., Wai-Key Y. Laparoscopic resection of a mesenteric cyst. Gastrointest Endosc. 2004;59:154–156. doi: 10.1016/s0016-5107(03)02365-4. [DOI] [PubMed] [Google Scholar]
- 20.Gmijovic D., Jeremic M., Stojianovic M., Radojkovic M. Mesenteric cysts. Acta Fac Med Naiss. 2007;24:189–194. [Google Scholar]


