Abstract
Introduction
Prolapse of abdominal viscera into the thoracic subcutis through the chest wall is known as transdiaphragmatic intercostal hernia (TIH). Herein, we present the first case of spontaneous TIH presenting as a thoracoabdominal emergency.
Presentation of case
A 78-year-old male presented with acute left thoracoabdominal pain following a sudden bulge at the left posterolateral chest wall corresponding to a partially reducible soft tissue mass with ecchymosis at the overlying skin. Paroxysmal cough during the last four days was also reported along with a prolonged daily application of a special tight abdominal belt that used while milking sheep. CT-scan of the abdomen showed intrathoracic proptosis of the splenic flexure through a defect of the left hemidiaphragm and subcutaneous prolapse of the herniated colon through the 7th intercostal space. On laparotomy, the herniated colon showed signs of ischemic necrosis leading to segmental colectomy followed by repair of the diaphragmatic defect.
Discussion
The clinical diagnosis of spontaneous TIH demands very high index of suspicion and thorough patient's history. In this case the daily elevation of the intraabdominal pressure due to an abdominal milking belt might have caused gradual slimming and loosening of the diaphragm and the intercostals muscles rendering them vulnerable to sudden increases of the thoracoabdominal pressure due to violent coughing. Such a hypothesis is reasonable in the absence of traumatic injury in this patient.
Conclusion
Spontaneous TIH should be suspected in patients presenting with a sudden palpable chest wall bulge and associated thoracoabdominal symptoms in the absence of preceding injury.
Keywords: Incarcerated, Transdiaphragmatic intercostal hernia, Pleuroperitoneal hernia
1. Introduction
Most diaphragmatic ruptures are caused by blunt or penetrating injury and only 1% are considered spontaneous. Spontaneous transdiaphragmatic hernia results from a sudden increase in the thoracoabdominal pressure gradient due to a violent Valsalva maneuver such as paroxysmal coughing, vomiting or vigorous exercise.1 Even rarer is the concomitant prolapse of abdominal viscera into the thoracic subcutis through the chest wall, a condition known as spontaneous transdiaphragmatic intercostal hernia (TIH) or intercostal pleuroperitoneal hernia.2,3 Herein, we present a case of spontaneous TIH presenting as a thoracoabdominal emergency.
2. Case report
A 78-year-old male patient presented to the emergency department with acute left thoracoabdominal pain following a sudden bulge at the left posterolateral chest wall. Dry, paroxysmal cough, inability to pass gas or stool and a single episode of dark-colored vomiting four days prior to admission were also reported. The patient had been a non-smoker for the past 30 years. His medical history was significant for medically controlled hypertension and diabetes mellitus. A thorough patient history revealed an uncommon, albeit relevant, clinical information: a prolonged daily application of a special tight abdominal belt that Cretan villagers use while milking sheep.
On examination, a palpable, partially reducible soft tissue mass of approximately 15 cm could be easily observed at the site of the bulge, corresponding to the patient's 7th intercostal space. Extensive ecchymosis was present at the overlying skin [Fig. 1A]. Diminished lung sounds involving the ipsilateral lower chest were heard on auscultation. The abdomen was soft and non-tender, exhibiting hyperactive bowel sounds.
Fig. 1.
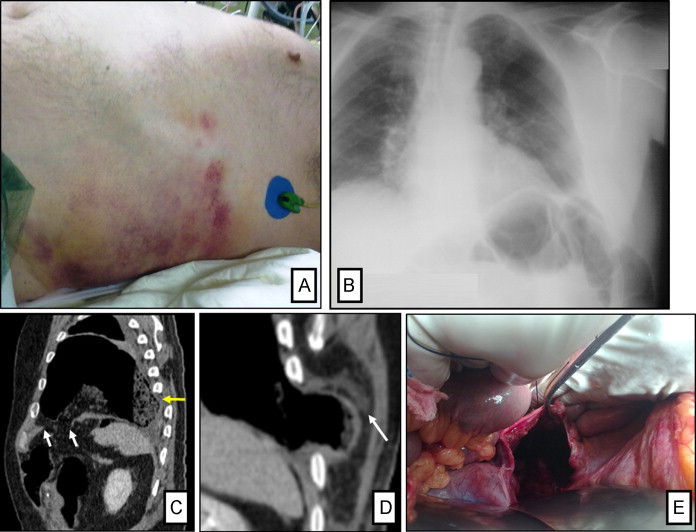
(A) Palpable chest wall mass with audible bowel sounds and overlying ecchymosis. (B) Posteroanterior chest radiograph at initial presentation revealed herniation of colon segment through the left lateral thoracic wall. (C) Sagittal reconstruction CT image shows direct discontinuity of the left hemidiaphragm (white arrows) and endothoracic herniation of a dilated colon segment (yellow arrow). (D) Enlarged coronal reconstruction CT image reveals intercostal muscle disruption (arrow) and protrusion of the bowel into the adjacent subcutis. (E) Intraoperative views of the diaphragmatic defect.
Laboratory results showed a raised white blood cell count (WBC: 14.1 K/μl, normal range: 3.5–10 K/μL) and increased serum creatine phosphokinase (CPK: 1121 U/l, normal range: 26–140 U/l).
The presence of a subcutaneous colon segment hernia with accompanying mild elevation of the ipsilateral hemidiaphragm and blunted left costophrenic angle was observed on posteroanterior chest X-ray [Fig. 1B]. The patient went on to further evaluation with contrast-enhanced CT-scan of the abdomen. A 5.5 cm defect at the anterolateral aspect of the left hemidiaphragm with resultant intrathoracic herniation of the splenic flexure and omental fat was depicted [Fig. 1C]. Subcutaneous prolapse of the peripheral part of the herniated colon through the ruptured musculature of the 7th intercostal space was also observed at the left lateral thoracic wall [Fig. 1D]. Additional imaging findings included a mild left pleural effusion and ipsilateral lower lobe subsegmental atelelectasis.
Clinical and imaging assessment established the diagnosis of spontaneous transdiaphragmatic intercostal hernia. The patient was urgently led to the operating theater. Transabdominal exploration identified a 10 cm gap at the left anterolateral hemidiaphragm [Fig. 1E]. Through this defect a large segment of the transverse colon entered the left hemithorax and subsequently bulged into the subcutaneous fat via the disrupted intercostal musculature at the level of the anterior axillary line. The herniated colon showed signs of ischemic necrosis leading to segmental colectomy followed by repair of the diaphragmatic defect, reapproximation of the intercostal defect and tube drainage of the right hemithorax. The postoperative course was complicated by a multiloculated left pleural effusion following the chest drain removal, as well as a dehiscence of the surgical wound. Both complications were treated conservatively and the patient was discharged on postoperative day 16. Five months after the operation the patient remains in good condition without clinical or radiological evidence of disease recurrence.
3. Discussion
This is the first case of incarcerated spontaneous TIH presenting as a thoracoabdominal emergency reported in the literature.1,2 Clinical suspicion and a thorough patient history are important steps to accurate diagnosis. In our case, the daily use of a milking belt is possibly associated with substantial elevation of intraabdominal pressure might have caused a gradual slimming and loosening of diaphragmatic and intercostals muscle fibers rendering them vulnerable to sudden surges in thoracoabdominal pressure gradient due to violent coughing or other antecedent factors (mentioned above). Such a hypothesis is reasonable considering the lack of traumatic injury or other obvious pathology in our patient.
There are no specific symptoms or signs indicating a non-traumatic rupture of the diaphragm. Thus it is extremely difficult for the physician to suspect it initially. The majority of patients suffer from intense pain of acute onset, localized in the abdomen, the chest or both. Cough, nausea, vomiting and dyspnea may coexist.1–3 If there is a concomitant intercostal muscle rupture, as in our patient, a reducible soft tissue mass can be palpated at the lateral chest wall and may protrude further with deep inspiration, coughing or whenever the patient is asked to reproduce the Valsalva maneuver. Non-violent expiration or contralateral decubitus positioning of the patient can lead to mass retraction. Ecchymosis of the overlying skin may be also present.2,3 Differential diagnosis of the palpable chest wall mass may also include, a spontaneous hematoma (especially in a patient on warfarin or clopidogrel), an intercostal muscle rupture, a rib fracture (seen with coughing, for instance), a lipoma or another chest wall tumor.
Although direct visualization of a diaphragmatic defect is difficult on plain chest X-rays, certain radiographic findings such as intrathoracic location of abdominal viscera and/or clear demonstration of a nasogastric tube tip above the left hemidiaphragm can be highly suggestive of rupture in the right clinical setting.1 Thoracoabdominal computed tomography is currently the imaging modality of choice for the diagnosis of diaphragmatic rupture, with a reported overall sensitivity and specificity of 70–100%.4,5 Direct discontinuity of the ruptured hemidiaphragm, intrathoracic herniation of abdominal contents, the collar sign (a waistlike constriction of the herniating hollow viscus at the site of the diaphragmatic tear) and the dependent viscera sign (viscera lying against the posterior chest wall in the supine patient), all present in our case, are considered diagnostic CT findings.4,5
Surgical intervention remains the gold standard for diagnosing and treating diaphragmatic rupture. Depending on the underlying cause and extent of pathology a thoracic, abdominal or thoracoabdominal approach is appropriately chosen. Diaphragmatic laceration is repaired with non-absorbable sutures. Simultaneous reapproximation of the intercostal defect is essential as well.2,3
4. Conclusion
Spontaneous transdiaphragmatic intercostal hernia should be suspected in patients presenting with a sudden palpable chest wall bulge and associated thoracoabdominal symptoms in the absence of preceding injury. Computed tomography is a valuable diagnostic tool with potential contribution in surgical planning. Prompt surgical exploration and repair of the hernia defects are of great importance.
Conflict of interest
The authors have no conflict of interest.
Funding
None.
Ethical approval
Informed consent for this publication has been signed by the patient and is in the disposition of the editor for review.
Authors’ contribution
Lasithiotakis Konstantinos: had the origina idea, searched the literature, reviewed and finalized the manuscript.
Venianaki Maria: drafted the manuscript, searched the literature.
Tsavalas Nikolaos: prepared the fotographs, searched the literature regarding radiological findings, reviewed the manuscript.
Zacharioudakis George: was the operating surgeon, reviewed the manuscript.
Petrakis Ioannis: was the 2nd operating surgeon, reviewed the final version of the manuscript, completed the follow-up of the patient.
Daskalogiannaki Maria: provided radiological analysis of the X-rays and CT scan, discussed the radiological findings and provided literature.
Chalkiadakis George: finalized and reviewed the final version of the manuscript and the figures.
References
- 1.Losanoff J., Edelman D., Salwen W. Spontaneous rupture of the diaphragm: case report and comprehensive review of the world literature. J Thorac Cardiovasc Surg. 2010;139:e127–e128. doi: 10.1016/j.jtcvs.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 2.Biswas S., Keddington J. Soft right chest wall swelling simulating lipoma following motor vehicle accident: transdiaphragmatic intercostal hernia. A case report and review of literature. Hernia. 2008;12:539–543. doi: 10.1007/s10029-008-0342-8. [DOI] [PubMed] [Google Scholar]
- 3.Aggarwal G, Khandelwal G, Shukla S, Maheshwari A, Mathur R, Acharya D. Spontaneous transdiaphragmatic intercostal hernia: a rare clinical entity. Hernia 2010 [Epub ahead of print]. [DOI] [PubMed]
- 4.Sliker C. Imaging of diaphragmatic injuries. Radiol Clin N Am. 2006;44:199–211. doi: 10.1016/j.rcl.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Mirvis S., Shanmuganagthan K. Imaging hemidiaphragmatic injury. Eur Radiol. 2007;17:1411–1421. doi: 10.1007/s00330-006-0553-2. [DOI] [PubMed] [Google Scholar]


