Abstract
Introduction
Adrenal cysts represent rare clinical entities. Although surgical indications are well defined, pitfalls arise from the failure to establish an accurate preoperative diagnosis. Cystic lesions of other abdominal organs especially the pancreas complicate the diagnostic field.
Presentation of case
We present the case of a giant adrenal cyst in a young female causing diagnostic dilemma. Imaging studies revealed a large cystic lesion of uncertain origin located between the spleen and the tail of the pancreas. It was decided to perform a laparotomy which confirmed the presence of an adrenal cyst and enucleation of the cyst was performed. Examination at one year confirmed no complications.
Discussion
Adrenal cysts should always be included in the differential diagnosis of cystic abdominal lesions.
Conclusion
When the preoperative diagnosis is uncertain, surgical intervention can be both diagnostic and therapeutic.
Keywords: Giant adrenal cyst, Endocrine surgery, Surgical treatment, Enucleation
1. Introduction
Adrenal cysts constitute clinical entities with a malignant potential rate of approximately 7%. The size of the cyst determines mainly the clinical presentation. Small cysts are usually clinically silent and are discovered incidentally .1 On the other hand, large-sized adrenal cysts (more than 10 cm in diameter) are associated with signs and symptoms either due to mass effect or intracystic pathology, i.e., haemorrhage.2,3
Pancreatic pseudocysts, liver, renal, splenic, mesenteric and retroperitoneal cystic lesions should be included in the differential diagnosis.4 Often, the cyst origin cannot be precisely defined even after a throughout imaging investigation. This adds an element of anxiety to the surgeon, as each laparotomy precludes a carefully designed surgical strategy.
We present an interesting case of a symptomatic giant adrenal cyst in a young female. Even though detailed preoperative work-up was performed, the exact origin of the cyst was finally confirmed intraoperatively. In the present study, we particularly aimed to underline the inability to follow the well defined surgical and treatment algorithm regarding adrenal cysts under the prism of diagnostic uncertainty.
2. Case presentation
A 22 year old female was admitted to our department complaining of dyspepsia, flank pain and sensation of pressure in the left upper quadrant over the past two months. Vital signs were: blood pressure (BP) 120/70 mm Hg, beats per minute (BPM): 74/min and body temperature 36.4 °C. Past medical history was free. Physical examination revealed a palpable, painless mass located in the left upper quadrant. Routine laboratory tests and hormone levels were within normal range. Abdominal ultrasound (US) showed a giant cyst at the left upper quadrant. Further evaluation with abdominal Computed Tomography (CT) with intravenous contrast (Fig. 1) and M.R.I. scan (Fig. 2) revealed a 14 × 10 × 16 cystic mass, located between the spleen and the tail of the pancreas, displacing the left kidney. A US – guided fine – needle aspiration (FNA) was performed. Cytological examination confirmed the hemorrhagic macroscopic characteristics of the fluid while no evidence of malignancy was observed.
Fig. 1.

Computed tomography with intravenous contrast showing the cystic lesion (arrows).
Fig. 2.

Magnetic resonance image of the adrenal lesion (arrows).
It was decided to proceed with laparotomy and a left subcostal incision was undertaken. The cyst was identified retroperitoneally, under the spleen, above the left kidney and at a close proximity to the tail of the pancreas, originating from the left adrenal gland (Fig. 3). The cyst was dissected free from the adjacent organs including the left adrenal gland and was removed intact (Fig. 4). The operative time was 90 min. Intraoperative blood loss was minimal. The postoperative period was uneventful and the patient was discharged on the 5th postoperative day. Histopathological analysis revealed a benign epithelial adrenal cyst. A scheduled examination at the outpatient clinic one year after the operation ruled out long-term complications.
Fig. 3.
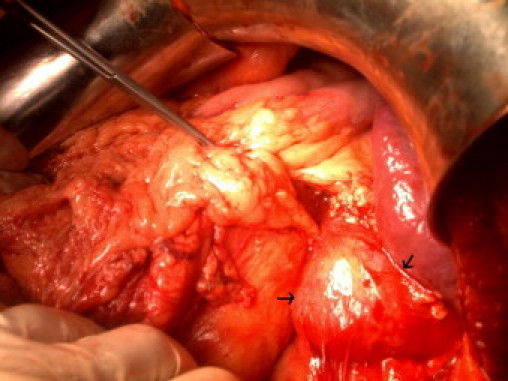
Intraoperative appearance of the cystic lesion (arrows).
Fig. 4.

Surgical specimen.
3. Discussion
CT is the imaging modality of choice for the primary evaluation of an adrenal mass with a reported sensitivity of 85–95%.5,6 Thin slices of 3–5 mm increase the diagnostic accuracy which is especially helpful in cases of small lesions. M.R.I. has similar reported specificity with CT in order to distinguish benign from malignant lesions. However, M.R.I. appears superior in dimension determination, discrimination from fatty tissue and in detecting pheochromocytomas.5 Adrenal cysts have pathognomonic CT imaging characteristics such as thin non-enhancing walls and fluid density content. Peripheral calcifications are only seen in the 15% of patients. Higher density values within the cyst denote intracystic hemorrhage.5,6
The key point in the preoperative work-up of an adrenal mass is to verify its functional status. Although it is of fundamental importance in cases of solid masses, it is also justified in cystic lesions. Biochemical assessment should include 24-h urinary metanephrines (or vanillyl mandelic acid – VMA), 17-hydroxycorticosteroids and 17-ketosteroids measurements. The low-dose dexamethasone test can evaluate the suppression rate of urinary steroids. In hypertensive patients, additional investigation with serial serum potassium levels while the patient is on diet with >200 meq of sodium and <100 meq of potassium is warrant.1,7
Surgical treatment is indicated for cysts more than 5 cm in diameter, parasitic, functional, malignant and generally in complicated and symptomatic cysts.8 In addition, surgical exploration is mandatory when malignancy cannot be ruled out after complete diagnostic workup.9 Nowadays, various surgical options have been proposed ranging from the traditional open anterior transabdominal or posterior retroperitoneal approach to the laparoscopic10,11 and the endoscopic retroperitoneal minimally invasive techniques.12 Simple enucleation with preservation of adrenal gland is the procedure of choice, while marsupialization is recommended for cysts densely adherent to adjacent organs.2 En bloc adrenalectomy with cyst resection represents the proper procedure in cases of malignancy. Laparoscopic approach is advocated in simple, uncomplicated cysts, less than 8 cm in diameter. However, it is contraindicated when a malignant process is presumed.13,14,15
Despite the fact that laparoscopy is the approach of choice for uncomplicated adrenal cysts a significant proportion of patients is not eligible. Either the cysts dimensions or the uncertainty in preoperative diagnosis dictates a laparotomy. In our case, we chose the open approach as the origin of the cyst could not be defined accurately in the preoperative setting. The cyst was dissected free from the adjacent structures with careful surgical manoeuvres and the origin from the left adrenal gland was precisely confirmed. The establishment of diagnosis intraoperatively replaced the initial exploratory intentions with the pathology adjusted surgical strategy. A cyst enucleation was then performed while attention was paid to leave the adrenal gland intact.
In the current study, we present our experience of one giant adrenal cyst case and definitive conclusions would not only be risky but also inappropriate. However, we would like to emphasize the diligence and vigilance that should characterize the surgeon facing challenging clinical scenarios. Aphorisms about possible sites of origin, when undoubtedly proofs are absent, increase the surgeon's inconvenience. In clinical practice, exact interpretation of treatment guidelines regarding adrenal cysts is often futile in the preoperative setting. Parameters, such as the inaccurate preoperative diagnosis transfer the decision time for the proper surgical plan to the operative room.
4. Conclusion
Adrenal cysts should be included in the differential diagnosis of cystic abdominal lesions. When the preoperative diagnosis is uncertain, surgical intervention can be both diagnostic and therapeutic.
Conflict of interest statement
All the authors’ disclosure that they have no conflict of interest.
Funding
None.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
References
- 1.Neri L.M., Nance F.C. Management of adrenal cysts. Am Surg. 1999;65:151–163. [PubMed] [Google Scholar]
- 2.Tagge D.U., Baron P.L. Giant adrenal cyst: management and review of the literature. Am Surg. 1997;63(August (8)):744–746. Review. [PubMed] [Google Scholar]
- 3.Pradeep P.V., Mishra A.K., Aggarwal V., Bhargav P.R., Gupta S.K., Agarwal A. Adrenal cysts: an institutional experience. World J Surg. 2006;30(October (10)):1817–1820. doi: 10.1007/s00268-005-0307-3. [DOI] [PubMed] [Google Scholar]
- 4.Sroujieh A.S., Farah G.R., Haddad M.J., Abu-Khalaf M.M. Adrenal cysts: diagnosis and management. Br J Urol. 1990;65(June (6)):570–575. doi: 10.1111/j.1464-410x.1990.tb14822.x. [DOI] [PubMed] [Google Scholar]
- 5.Lockhart M.E., Smith J.K., Kenney P.J. Imaging of adrenal masses. Err J Radiol. 2002;41(2):95–112. doi: 10.1016/s0720-048x(01)00444-2. [DOI] [PubMed] [Google Scholar]
- 6.Tung G.A., Foster R.C., Papanicolaou N., Yoder I.C. Adrenal cysts: imaging and percutaneous aspiration. Radiology. 1989;173(October (1)):107–110. doi: 10.1148/radiology.173.1.2675177. [DOI] [PubMed] [Google Scholar]
- 7.Ross N.S., Aron D.C. Hormonal evaluation of the patient with an incidentally discovered adrenal mass. N Engl J Med. 1990;323(20):1401–1405. doi: 10.1056/NEJM199011153232007. 15. [DOI] [PubMed] [Google Scholar]
- 8.Lal T.G., Kaulback K.R., Bombonati A., Palazzo J.P., Jeffrey R.B., Weigel R.J. Surgical management of adrenal cysts. Am Surg. 2003;69(September (9)):812–814. [PubMed] [Google Scholar]
- 9.Schmid H., Mussack T., Wörnle M., Pietrzyk M.C., Banas B. Clinical management of large adrenal cystic lesions. Int Urol Nephrol. 2005;37(4):767–771. doi: 10.1007/s11255-005-4662-7. [DOI] [PubMed] [Google Scholar]
- 10.Mercan S., Seven R., Ozarmagan S., Tezelman S. Endoscopic retroperitoneal adrenalectomy. Surgery. 1995;118(6):1071–1075. doi: 10.1016/s0039-6060(05)80116-3. [DOI] [PubMed] [Google Scholar]
- 11.Linos D.A., Stylopoulos N., Raptis S.A. Adrenaloma: a call for more aggressive management. World J Surg. 1996;20(7):788–792. doi: 10.1007/s002689900120. [DOI] [PubMed] [Google Scholar]
- 12.Walz M.K., Peitgen K., Hoermann R. Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg. 1996;20(7):769–774. doi: 10.1007/s002689900117. [DOI] [PubMed] [Google Scholar]
- 13.Pillinger S.H., Bambach C.P., Sidhu S. Laparoscopic adrenalectomy: a 6-year experience of 59 cases. ANZ J Surg. 2002;72(7):467–470. doi: 10.1046/j.1445-2197.2002.02453.x. [DOI] [PubMed] [Google Scholar]
- 14.Hallfeldt K.K., Mussack T., Trupka A., Hohenbleicher F., Schmidbauer S. Laparoscopic lateral adrenalectomy versus open posterior adrenalectomy for the treatment of benign adrenal tumors. Surg Endosc. 2003;17(2):264–267. doi: 10.1007/s00464-002-8810-1. [DOI] [PubMed] [Google Scholar]
- 15.Bellantone R., Ferrante A., Raffaelli M., Boscherini M., Lomnardi C.P., Crucitti F. Adrenal cystic lesions: report of 12 surgically treated cases and review of the literature. J Endocrinol Invest. 1998;21(2):109–114. doi: 10.1007/BF03350324. [DOI] [PubMed] [Google Scholar]


