Abstract
Introduction
Colorectal cancer most often presents with a change in bowel habit, weight loss or with bleeding per rectum. Much less commonly, colorectal cancer may present as part of a paraneoplastic syndrome. Polymyositis is a rare disease most often considered a complement-mediated idiopathic inflammatory myopathy manifested by proximal muscle weakness. However, polymyositis may also be part of a paraneoplastic syndrome associated with an underlying malignancy. The relationship between polymyositis and malignancy is well known, but it has been suggested that tumours of the large bowel are rarely complicated by myositis.
Presentation of case
The authors describe a case report of an 82-year-old gentleman with a presumed musculoskeletal or neurological deficit who was subsequently diagnosed with metastatic colon cancer in the setting of progressive fatigue and muscle weakness. Concurrently, we review the current literature looking at the relationship between cancer and polymyositis.
Discussion
Colorectal cancer rarely presents with symptoms such as muscle weakness, however it is important to be aware of the possibility of an underlying malignancy when seeing patients with symptoms which are suggestive of polymyositis.
Conclusion
The diagnosis of polymyositis in the elderly population should raise suspicion of an underlying malignancy.
Keywords: Colorectal cancer, Polymyositis, Paraneoplastic syndrome
1. Introduction
Colorectal cancer most often presents with a change in bowel habit, weight loss or with bleeding per rectum. Much less commonly, colorectal cancer may present as part of a paraneoplastic syndrome, defined as, a symptom that is a consequence of the presence of cancer in the body but is not caused by the local effect of neoplastic cells. Polymyositis is a rare disease most often considered a complement-mediated idiopathic inflammatory myopathy manifested by proximal muscle weakness. However, polymyositis may also be manifested as part of a paraneoplastic process associated with an underlying malignancy.
2. Presentation of case
A previously active 82-year-old man presented to his general practitioner, complaining of bilateral leg weakness that had progressed gradually during the preceding 6 months. More recently he had developed aches in his shoulders and proximal weakness affecting all four limbs. Clinical examination revealed symmetrical muscle weakness of the quadriceps and flexor muscles of the knee. The patient required assistance to stand from a seated position and displayed a ‘waddling’ gait. He displayed no skin changes suggestive of dermatomyositis. Initial blood tests were unremarkable apart from a mildly elevated ESR of 28 mm/h. The patient was initially diagnosed with polymyalgia rheumatica and commenced on steroids. No improvement was noted in the patient condition over the next three months. Conversely, deterioration was noted in the symptoms and a rheumatology referral was made.
Investigations by the Rheumatologist including an autoantibody screen, which was positive for ANA and Anti-Ro. The Rheumatologist also made an urgent referral for a neurology opinion to rule out a neurological cause to his symptoms. An MRI thigh was reported with “gross multi-compartmental fatty atrophy with widespread inflammation, highly suspicious of a polymyositis”. Neurological tests, including a muscle biopsy and neurophysiology, excluded motor neurone disease or demyelination, but were described as “complex changes, including both atrophic and hypertrophic muscle fibres, suggestive of polymyositis and likely to be part of a paraneoplastic syndrome”.
It was now considered highly likely that this patient's weakness had occurred as part of a paraneoplastic syndrome, despite him being otherwise well, with a stable weight and no obvious symptoms that might localise a potential malignancy, and so a CT chest, abdomen and pelvis was requested.
Despite the absence of bowel symptoms, CT images (Fig. 1) revealed “significant irregular descending colon thickening with mesenteric lymphadenopathy and hepatic metastases affecting both lobes of the liver”. A right sided renal mass was also seen on CT (Fig. 2) and was described as “a solid well-defined rounded mass” and considered as an associated second tumour. A flexible sigmoidoscopy visualised a large tumour affecting the proximal descending colon (Fig. 3), whilst histology confirmed an invasive moderately differentiated adenocarcinoma. The patient also underwent further blood tests and was found to be anaemic, with an Hb = 10.6 g/dL, and had an elevated CEA (285).
Fig. 1.

Coronal CT scan identifying tumour in descending colon.
Fig. 2.
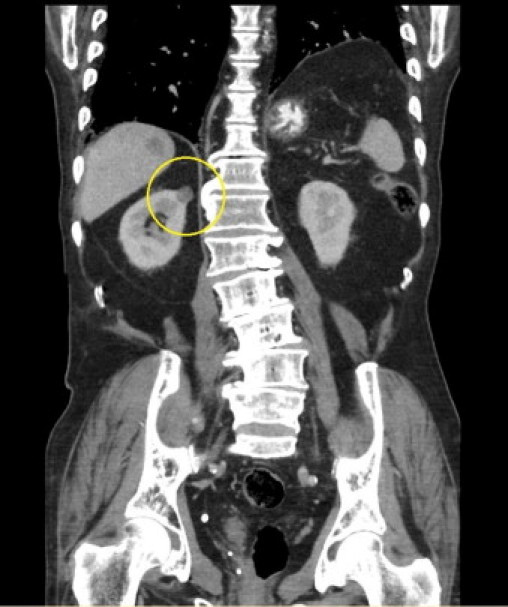
Coronal CT scan identifying right sided renal mass.
Fig. 3.
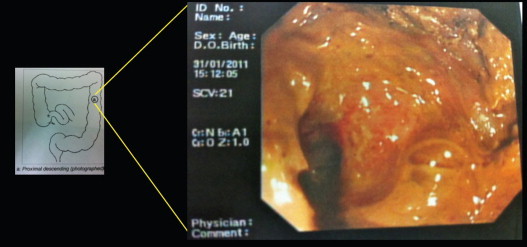
Flexible sigmoidoscopy image of tumour.
Subsequently, a multidisciplinary team discussion concluded that an oncology referral for consideration of palliative chemotherapy would be the most appropriate plan. In view of the duration and persistence of his paraneoplastic myopathy, it was decided that chemotherapy was not likely to provide symptomatic relief or a significant gain in life expectancy; now thought to be months rather than years. The patient continues to experience limiting proximal muscle weakness and recently stated that he was shocked when he found out his symptoms were due to colorectal cancer, stating “I never even considered that my symptoms could have been caused by cancer”.
3. Discussion
The term myopathy applies to both congenital and acquired muscle diseases. Within the acquired group of diseases there is distinction between dermatomyositis and polymyositis, which are both inflammatory myopathies of unknown aetiology. Dermatomyositis presents with characteristic skin changes accompanying, or often preceding, muscle weakness, where as, polymyositis involves muscle weakness in the absence of any skin changes. The risk of cancer is increased in both myopathies, but there is a greater risk with dermatomyositis when compared to those with polymyositis.1,2
The association between myopathies, occurring as part of a paraneoplastic syndrome, and cancer is well recognised, however, epidemiological studies have been hindered by small case numbers, referral bias and diagnostic inconsistencies. A population based study conducted by Hill et al.3 described the link between myositis and malignancy, which concluded that patients suffering from polymyositis were at an increased risk of cancer when compared to the general population. Table 1 summarises three other population based cohort studies, from Scandinavia,4–6 investigating the relationship between myositis and malignancy. All these studies concluded that there is an increased relative risk of malignancy in myositis, but this is more pronounced in relation to dermatomyositis as compared to polymyositis. These studies also showed that the relationship was very rare below the age of 45.
Table 1.
Population-based cohort studies on the link between myositis and malignancy.
Hill et al. concluded that the most common types of cancer associated with polymyositis were non-Hodgkin lymphoma, lung and bladder cancer. It has been suggested elsewhere that other solid tumours, such as prostate and ovarian cancer, as well as haematological malignancies can be associated with myositis. However, this suggestion is not supported by definitive evidence and they reported prevalence for various cancer types varies greatly in different studies.7,8
More recent studies on this association have explored the pathophysiological mechanisms behind this relationship, finding that myositis-specific antigens are over-expressed in cancer tissue.9 It is hypothesized that increased myositis-specific antigens in a nascent tumour can lead to the formation of specific B-cells and T-cells against the antigens, which is the cause of muscular inflammation.
In colorectal cancer the relationship with myopathy is extremely rare, particularly in the absence of cutaneous features. Ours is the first case report of colon cancer, with polymyositis as the presenting complaint of the patient, occurring as part of a paraneoplastic syndrome. Our patient is unique as he had extensive disease with metastases in the liver and the possibility of an associated renal tumour, which may have also played a part in the paraneoplastic syndrome.
Some research has also looked into the use of surgical resection of a tumour or chemotherapy in managing this problem, which was discussed with regard to our patient. Theoretically, tumour-driven autoimmunity may help to explain any improvement in a patient's polymyositis following such interventions. In view of his extensive metastatic disease, it was decided that our patient was not to undergo radical surgery and the oncologist decided that chemotherapy would not provide sufficient symptom relief or increase in life expectancy.
4. Conclusion
This case demonstrates the value of knowledge about associated paraneoplastic syndromes, as this may help solve uncommon but serious diagnostic conundrums. Early diagnosis of malignancy is critical in cases of polymyositis.10 Any hints we as clinicians can gain to aid a diagnosis are essential and therefore our study identifies the importance in considering neoplasm as a differential for patients presenting with symptoms of myopathy, as although rare, it can be the first symptom at presentation and can provide a clinician with a vital clue to provide an earlier diagnosis of occult cancer. We suggest that patients over the age of 45, with a newly diagnosed myositis, should be screened for occult cancer, including a thorough history and extensive examination, and investigations including blood tests for haematological and biochemical screening and assessment of tumour markers (CEA, CA-125, PSA, etc.).
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of interest statement
The authors report no conflicts of interest for this case report.
Funding
The authors report that the case report was self-funded.
Author contribution
Dr. Broman wrote up the case report and analysed current literature on the topic to format a discussion, conclusion and learning point from the presented case.
Mr. Rajaganeshan helped with the case report design and aided Dr. Broman with the writing up of the case report. He also contributed by revising it critically for intellectual content.
Mr. Selvasekar was the consultant surgeon overseeing the care of this patient. He had final approval of the case report to be submitted.
References
- 1.Zahr Z.A., Baer A.N. Malignancy in myositis. Curr Rheumatol Rep. 2011;13(June (3)):208–215. doi: 10.1007/s11926-011-0169-7. [DOI] [PubMed] [Google Scholar]
- 2.Chen Y.J., Wu C.Y., Huang Y.L., Wang C.B., Shen J.L., Chang Y.T. Cancer risks of dermatomyositis and polymyositis: a nationwide cohort study in Taiwan. Arthritis Res Ther. 2010;12(2):R70. doi: 10.1186/ar2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill C.L., Zhang Y., Sigurgeirsson B., Pukkala E., Mellemkjaer L., Airio A. Frequency of specific cancer types in dermatomyositis and polymyositis: a population-based study. Lancet. 2001;January (357):96–100. doi: 10.1016/S0140-6736(00)03540-6. [DOI] [PubMed] [Google Scholar]
- 4.Sigurgeirsson B., Lindeloff B., Edhag O., Erik Allander Risk of cancer in patients with dermatomyositis and polymyositis: a population based study. N Engl J Med. 1992;326:363–367. doi: 10.1056/NEJM199202063260602. [DOI] [PubMed] [Google Scholar]
- 5.Airio A., Pukkala E., Isomaki H. Elevated cancer incidence in patients with dermatomyositis: a population-based study. J Rheumatol. 1995;22:1300–1303. [PubMed] [Google Scholar]
- 6.Chow W.H., Gridley G., Mellemkjaer L., McLaughlin J.K., Olsen J.H., Fraumeni J.F., Jr. Cancer risk following polymyositis and dermatomyositis: a nationwide cohort study in Denmark. Cancer Causes Control. 1995;6:9–13. doi: 10.1007/BF00051675. [DOI] [PubMed] [Google Scholar]
- 7.Callen J.P. Myositis and malignancy. Curr Opin Rheumatol. 1994;6:590–594. doi: 10.1097/00002281-199411000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Maoz C.R., Langevitz P., Livneh A., Blumstein Z., Sadeh M., Bank I. High incidence of malignancies in dermatomyositis and polymyositis: an 11-year analysis. Semin Arthritis Rheum. 1998;27:319–324. doi: 10.1016/s0049-0172(98)80052-8. [DOI] [PubMed] [Google Scholar]
- 9.Levine S.M. Cancer and myositis: new insights into an old association. Curr Opin Rheumatol. 2006;18:620–624. doi: 10.1097/01.bor.0000245721.02512.77. [DOI] [PubMed] [Google Scholar]
- 10.Wakata N., Kurihara T., Saito E., Kinoshita M. Polymyositis and dermatomyositis associated with malignancy: a 30-year retrospective study. Int J Dermatol. 2002;41(11):729–734. doi: 10.1046/j.1365-4362.2002.01648.x. [DOI] [PubMed] [Google Scholar]


