Abstract
Endometriosis of the appendix is an entity of extragonadal endometriosis. It commonly affects women in the childbearing age with a wide spectrum of clinical manifestations. Women can present with symptoms mimicking acute appendicitis or chronic pelvic pain. The surgical management varies from simple appendectomy to right hemicolectomy depending on the clinical findings. We report 3 cases of endometriosis of the appendix presenting with appendiceal intussusception. The surgical literature is reviewed and current surgical management is discussed.
Keywords: Appendix, Intussusception, Endometriosis, Case report
1. Introduction
Endometriosis is a common condition that can affect up to 15% of women of childbearing age and 2–5% of post-menopausal women.1 This condition can lead to significant morbidity and is a frequent cause of surgical intervention for chronic pelvic pain. Endometriosis commonly involves the adnexa but can be present anywhere in the peritoneal cavity. Endometriosis involving the appendix is rare and preoperative diagnosis is difficult. In this paper we illustrate three different clinical presentations of endometriosis of the appendix and their subsequent management.
2. Case report 1
A 53-year-old postmenopausal female with known history of endometriosis presented to our clinic for screening colonoscopy. She also complained of mild right lower quadrant tenderness at Mc Burney's point. Endoscopic findings were consistent with an appendiceal submucosal mass and invagination at the base of the appendix (Fig. 1). Biopsies of the mass were consistent with colonic mucosa with lymphoid aggregates. A computed tomograph (CT) of the abdomen and pelvis did not demonstrate any pelvic or abdominal abnormalities. The patient underwent a diagnostic laparoscopy. The appendix was tethered to the terminal ileum. There were several white plaques involving the terminal ileum. Because of the operative findings a laparoscopic ileocecectomy was performed. The specimen histopathology was consistent with endometriosis involving the appendix and the serosal layer of the ileum. The patient went on to make an uneventful recovery with resolution of her abdominal discomfort.
Fig. 1.

Endoscopic picture showing inverted appendiceal submucosal mass (black arrow).
3. Case report 2
A 49-year-old female presented with a history of intermittent right lower quadrant pain for 4 years. She was evaluated with an abdominal CT, which demonstrated a dilated fluid filled appendix (Fig. 2). Optical colonoscopy was performed and demonstrated a 2 cm extrinsic mass adjacent to the appendiceal ostia. The mucosal surface was normal. She underwent a diagnostic laparoscopy. Intra-operatively, dense adhesions were encountered in the right lower quadrant. An appendectomy was performed. Her postoperative course was uneventful. Histopathologic examination demonstrated chronic appendicitis and endometriosis involving the serosa of the appendix.
Fig. 2.

Abdominal computed tomographic scan showing dilated fluid filled appendix and the tip of the appendix.
4. Case report 3
A 55-year-old healthy female underwent a screening colonoscopy, significant for an inverted appendix (Fig. 3). Her past medical history was significant for laparoscopic hysterectomy for dysfunctional uterine bleeding. An endoscopic biopsy of the inverted appendix revealed normal mucosa. The patient underwent diagnostic laparoscopy. Intraoperatively, the appendix was absent at the confluence of the tenia. An ileocecectomy was performed. Her postoperative course was uneventful. When the specimen was opened, the entire appendix appeared inverted. Histologically, there was muscular hyperplasia with endometrial gland and stroma which consistent with endometriosis (Fig. 4).
Fig. 3.

Endoscopic pictures showing inverted appendix (black arrows).
Fig. 4.
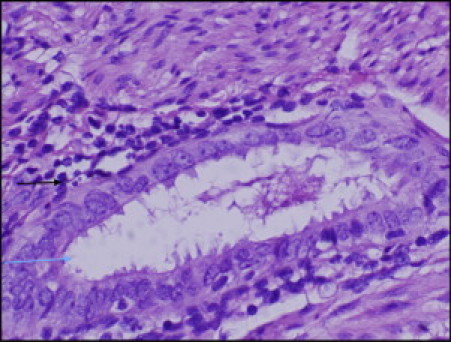
Microscopic picture of the appendix showing endometrial stroma (black arrow) and endometrial gland (blue arrow).
5. Discussion
Endometriosis is a condition characterized by the growth of the endometrial tissue outside the uterine cavity. It was initially described by von Rokitansky in 1860. The majority of endometrial implants are located in the dependent portions of the female pelvis. The most common sites of endometriosis involvement are the ovaries (54.9%), posterior broad ligament (35.2%), anterior cul-de-sac (34.6%), the posterior cul-de-sac (34.0%), and the uterosacral ligament (28.0%).2 Endometriosis is occasionally discovered in the umbilicus and in surgical scars, especially following Caesarean section.3 Rarely, it is seen in the kidney, lung, skin and diaphragm.4,5 Involvement of the gastrointestinal tract is reported to affect between 3% and 37% of patients with pelvic endometriosis.6,7 When endometriosis does involve the GI tract it commonly involves the recto-sigmoid (72%), the recto-vaginal septum (13%), small intestine (7%), cecum (3.6%) and the appendix (3%).8
The histological diagnosis of endometriosis is readily made when both endometrial glands and stroma are present outside of the uterus. The diagnosis can sometimes be difficult in long standing cases in which the tissue is obscured by secondary fibrosis. In the intestine, endometriosis usually involves the serosa and the subserosa. Sometimes the muscularis propria, the submucosa and the mucosa may be involved especially in symptomatic patients.9
Endometriosis has a wide variety of clinical presentations. Common symptoms include pelvic pain, secondary dysmenorrhea, dyspareunia, irregular or heavy menstrual period and infertility.10 Approximately one third of patients with endometriosis are asymptomatic. Endometriosis of the gastrointestinal tract may mimic gastrointestinal pathology causing abdominal cramps, change in bowel habits, nausea,11 rectal bleeding12 and bowel obstruction. Endometriosis of the appendix can present with chronic pelvic pain, melena,13 lower gastrointestinal bleeding,14 or intussusception of the appendix.15
Appendiceal endometriosis is not an uncommon incidental finding during laparoscopy or laparotomy. It is a common diagnosis when an inverted or bulbous appendiceal orifice is noted at the time of colonoscopy. Endometriosis of the appendix during pregnancy is very rare and it is associated with higher risk of bowel perforation, especially in the 3rd trimester.16 Laboratory tests are of limited value. CT of the abdomen and pelvis may show evidence of acute appendicitis, or appendiceal abnormality. Laparoscopy is considered the gold standard for the diagnosis of endometriosis. Grossly, endometriosis appears as raised flame-like patches, whitish opacifications, yellow-brown discoloration, or reddish-blue irregularly shaped islands. If there is an involvement of the mucosa, the differential diagnosis should include crohn's disease, cancer and ischemia. Pain is the most common indication for surgical management.17
The published rate of endometriosis of the appendix varies widely depending on the type of clinical practice. Reports from tertiary centers reported a higher incidence of disease likely because they are referral centers for complicated disease. A study of 50,000 specimen of the human appendix by Collins reported the incidence of endometriosis of the appendix as 0.054.18 Marudanayagam et al. examined 2660 appendix specimens and found that the incidence of appendiceal endometriosis was 0.3%.19 Uohara and Kovara reported the incidence of endometriosis of the appendix as 0.80% in 1496 appendectomies.20 Smith reported an incidence of 0.62%,21 and Haydon reported the incidence as 0.17% in 569 who presented with endometriosis.22 Comparative analysis of the diagnosis of 866 cases of endometriosis including 53 cases of intestinal endometriosis revelled two cases of endometriosis of the appendix, reported by Thiersten et al. with an incidence of 0.22%,23 while Scott and Te reported an incidence of 1.3% in 516 patients who underwent an operation for gynecological reasons.24 Sutton and Hardy reported an incidence of endometriosis of the appendix 0.0217% in 6911 appendectomies.25
The goal of surgical treatment of bowel endometriosis is to remove the disease and restore the bowel continuity and function. The treatment of endometriosis of the appendix is appendectomy, ileocecectomy, and right hemicolectomy (Table 1). At laparotomy or laparoscopy, a careful examination of the abdominal cavity is carried out in order to fully evaluate the extent of disease. Often, involvement of the uterus and adnexa requires a multidisciplinary team approach. When there is appendiceal intussusception, gentle traction is applied to reduce the intussuscepted appendix. This should be performed with some caution. Malignancies or benign tumor of the appendiceal region can present with invagination. If the diagnosis is not clear, ileocecectomy or right hemicolectomy should be performed. Because endometriosis of the appendix maybe missed by visual inspection alone, incidental appendectomy is recommended in patients with severe endometriosis.17 Small bowel involvement is rare, and the ileocecal region is the most common affected area. Superficial spots of endometriosis can be vaporized with CO2 laser. More extensive lesions are treated by small bowel resection and anastomosis.17 Superficial lesions involving the rectal wall can be dissected off the wall using diathermy. Full thickness excision of anterior rectal wall or segmental resection have been reported for more extensive lesions.26
Table 1.
Operative management of appendiceal intussusception due to endometriosis: literature review.
| Author | Year | N | Age | Clinical presentation | Preoperative diagnosis | Method of diagnosis | Operative management |
|---|---|---|---|---|---|---|---|
| Morton | 1952 | 1 | 39 | Right lower quadrant (RLQ) pain | No | – | Cecotomy and appendectomy |
| Fink | 1964 | 1 | 49 | RLQ mass for 8 years | No | – | Cecotomy and appendectomy |
| Hill | 1970 | 2 | 39 | Bleeding per rectum | Yes | Barium enema | Right hemicolectomy |
| 34 | Bleeding per rectum | Yes | Barium enema | Cecotomy and appendectomy | |||
| Howard | 1970 | 1 | 50 | RLQ pain. Barium enema showed cecal mass | No | – | Right hemicolectomy |
| Schmidt | 1971 | 1 | 40 | Mass in the cecum incidentally found during cholecystectomy | No | – | Right hemicolectomy |
| Panganiban | 1972 | 1 | 35 | RLQ pain | No | – | Cecotomy and appendectomy |
| Nissen | 1973 | 1 | 32 | Incidental intra-operative finding | No | – | Cecectomy. |
| Shapiro | 1974 | 1 | 45 | Lower abdominal pain | No | – | Cecotomy and appendectomy. |
| Rodriguez | 1978 | 1 | 41 | RLQ pain for 6 months | No | – | Appendectomy |
| Seaman | 1978 | 1 | 33 | Intermittent abdominal pain | Yes | – | Appendectomy |
| Martin | 1980 | 1 | 32 | RLQ pain | Yes | Colonoscopy | Appendectomy |
| Langsam | 1984 | 1 | 32 | Lower abdominal pain | Yes | Barium enema | Cecotomy and appendectomy |
| Mann | 1984 | 2 | 41 | Incidental intra-operative finding | No | – | Appendectomy |
| 58 | Incidental intra-operative finding | No | – | Appendectomy | |||
| Sonnino | 1985 | 1 | 35 | Midepigastric pain and melena | No | – | Appendectomy and excision of a small rim of the cecum |
| Hartman | 1988 | 1 | 36 | RLQ pain | No | – | Ileocecal resection |
| Gilpin | 1989 | 1 | 34 | Lower abdominal pain | No | – | Appendectomy |
| Ardies | 1990 | 2 | 50 | Asymptomatic. Filling defect in the cecum. | Yes | Double contrast study | Cecectomy |
| 29 | RLQ pain | Yes | – | – | |||
| Jevon | 1992 | 2 | 32 | Bright red blood per rectum, cecal mass. | No | – | Cecotomy and appendectomy |
| 37 | Asymptomatic. Incidentally found umblication of the serosal surface of the cecum during hysterectomy for endometriosis | No | – | Appendectomy | |||
| Jevon | 1992 | 1 | 46 | Recurrent lower abdominal pain for 5 months | No | – | Appendectomy |
| Lauwers | 1993 | 1 | 39 | Diffuse abdominal pain for 1 week | No | – | Right hemicolectomy |
| Sakaguchi | 1995 | 1 | 39 | Ileocecal mass Incidentally found during hysterectomy | No | – | Ileocecal resection |
| Panzer | 1995 | 1 | 39 | RLQ pain for 2 years | Yes | Colonoscopy | Ileocecal resection |
| Kimura | 1999 | 1 | 41 | Abdominal pain and vomiting | Yes | CT and Ultrasound | Appendectomy, and cecal resection (cecal mucosa was necrotic) |
| Nycum | 1999 | 1 | 29 | Incidental intra-operative finding during laparotomy for pelvic mass | No | – | Partial cecectomy |
| Sriram | 2000 | 1 | 63 | Recurrent lower abdominal pain and rectal bleeding | Yes | Colonoscopy | Endoscopic resection |
| Scully | 2000 | 1 | 26 | Abdominal pain and diarrhea | Yes | CT | Ileocolectomy |
| Vogelaar | 2004 | 1 | 25 | RLQ pain | No | – | Cecectomy |
| Duncan | 2005 | 1 | 45 | Rectal bleeding and intermittent RLQ pain | Yes | Colonoscopy | Laparoscopic partial cecectomy |
| Moradi | 2007 | 1 | 41 | RLQ pain for 2 days | No | – | Limited resection of the cecum, because of irreducible tip of the appendix |
| Offodile | 2007 | 1 | 47 | Asymptomatic. Submucosal mass found during colonoscopy | No | – | Laparoscopic right hemicolectomy |
| Ijaz | 2008 | 1 | 40 | Chronic lower abdominal pain | No | – | Appendectomy |
| Chaar | 2009 | 1 | 40 | Intermittent abdominal pain for 4 days | No | – | Ileocecectomy |
| Liang | 2009 | 1 | 55 | RLQ pain for 6 months | Yes | CT | Laparoscopic appendectomy |
Conflicts of interest statement
None declared.
Funding
None.
Ethical approval
Written informed consent was obtained from all the patients for publication of this case report and accompanying images.
References
- 1.Stenchever M.A., Droegemueller W., Herbst A.L. 4th ed. 2001. Comprehensive Gynecology. [Google Scholar]
- 2.Jenkins S., Olive D.L., Haney A.F. Endometriosis: pathogenetic implications of the anatomic distribution. Obstet Gynecol. 1986;67(March (3)):335–338. [PubMed] [Google Scholar]
- 3.Singh M., Sivanesan K., Ghani R., Granger K. Caesarean scar endometriosis. Arch Gynecol Obstet. 2009;279(February (2)):217–219. doi: 10.1007/s00404-008-0672-x. [DOI] [PubMed] [Google Scholar]
- 4.Olive D.L., Schwartz L.B., Endometriosis N Engl J Med. 1993;328(June (24)):1759–1769. doi: 10.1056/NEJM199306173282407. [DOI] [PubMed] [Google Scholar]
- 5.Redwine D.B. Diaphragmatic endometriosis: diagnosis, surgical management, and long-term results of treatment. Fertil Steril. 2002;77(February (2)):288–296. doi: 10.1016/s0015-0282(01)02998-3. [DOI] [PubMed] [Google Scholar]
- 6.Prystowsky J.B., Stryker S.J., Ujiki G.T., Poticha S.M. Gastrointestinal endometriosis. Incidence and indications for resection. Arch Surg. 1988;123(July (7)):855–858. doi: 10.1001/archsurg.1988.01400310069011. [DOI] [PubMed] [Google Scholar]
- 7.Croom R.D., 3rd, Donovan M.L., Schwesinger W.H. Intestinal endometriosis. Am J Surg. 1984;148(November (5)):660–667. doi: 10.1016/0002-9610(84)90347-7. [DOI] [PubMed] [Google Scholar]
- 8.Macafee C.H., Greer H.L. Intestinal endometriosis. A report of 29 cases and a survey of the literature. J Obstet Gynaecol Br Emp. 1960;67(August):539–555. doi: 10.1111/j.1471-0528.1960.tb09211.x. [DOI] [PubMed] [Google Scholar]
- 9.Yantiss R.K., Clement P.B., Young R.H. Neoplastic and pre-neoplastic changes in gastrointestinal endometriosis: a study of 17 cases. Am J Surg Pathol. 2000;24(April (4)):513–524. doi: 10.1097/00000478-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Farquhar C. Endometriosis. BMJ. 2007;334(February (7587)):249–253. doi: 10.1136/bmj.39073.736829.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weed J.C., Ray J.E. Endometriosis of the bowel. Obstet Gynecol. 1987;69(May (5)):727–730. [PubMed] [Google Scholar]
- 12.Barclay R.L., Simon J.B., Vanner S.J., Hurlbut D.J., Jeffrey J.F. Rectal passage of intestinal endometriosis. Dig Dis Sci. 2001;46(September (9)):1963–1967. doi: 10.1023/a:1010647401186. [DOI] [PubMed] [Google Scholar]
- 13.Collins D.C. Endometriosis of the vermiform appendix; review of literature, with addition of nine new instances, one of which caused severe melena. AMA Arch Surg. 1951;63(November (5)):617–622. [PubMed] [Google Scholar]
- 14.Shome G.P., Nagaraju M., Munis A., Wiese D. Appendiceal endometriosis presenting as massive lower intestinal hemorrhage. Am J Gastroenterol. 1995;90(October (10)):1881–1883. [PubMed] [Google Scholar]
- 15.Chaar C.I., Wexelman B., Zuckerman K., Longo W. Intussusception of the appendix: comprehensive review of the literature. Am J Surg. 2009;198(July (1)):122–128. doi: 10.1016/j.amjsurg.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 16.Perez C.M., Minimo C., Margolin G., Orris J. Appendiceal endometriosis presenting as acute appendicitis during pregnancy. Int J Gynaecol Obstet. 2007;98(August (2)):164–167. doi: 10.1016/j.ijgo.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 17.Camran C.R., Berger G.S. Springer; 1995. Endometriosis: advanced management and surgical techniques. [Google Scholar]
- 18.Collins D.C. A study of 50,000 specimens of the human vermiform appendix. Surg Gynecol Obstet. 1955;101(October (4)):437–445. [PubMed] [Google Scholar]
- 19.Marudanayagam R., Williams G.T., Rees B.I. Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol. 2006;41(August (8)):745–749. doi: 10.1007/s00535-006-1855-5. [DOI] [PubMed] [Google Scholar]
- 20.Uohara J.K., Kovara T.Y. Endometriosis of the appendix. Report of twelve cases and review of the literature. Am J Obstet Gynecol. 1975;121(February (3)):423–426. doi: 10.1016/0002-9378(75)90026-5. [DOI] [PubMed] [Google Scholar]
- 21.Smith G.V. Endometrioma: a clinical and pathologic study of 159 cases treated at the clinic of the free hospital for women, Brookilne, Massachusetts. Am J Obstet Gynecol. 1929;17:806. [Google Scholar]
- 22.Haydon G.B. A study of 569 Cases of Endometriosis. Am J Gynecol Obstet. 1942;43:704–709. [Google Scholar]
- 23.Samuel T., Thierstein E.A. A comparative analysis of the diagnosis and treatment of endometriosis. Including a report of fifty three cases of intestinal endometriosis. Am J Obstet Gynecol. 1946;51:635–642. doi: 10.1016/s0002-9378(15)30119-8. [DOI] [PubMed] [Google Scholar]
- 24.Scott R.B., Te L.R. External endometriosis—the scourge of the private patient. Ann Surg. 1950;131(May (5)):697–720. doi: 10.1097/00000658-195005000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sutton C.E., Hardy J.A. Endometriosis of the vermiform appendix. Am J Obstet Gynecol. 1952;63(May (5)):1139–1142. doi: 10.1016/0002-9378(52)90555-3. [DOI] [PubMed] [Google Scholar]
- 26.Brouwer R.W.R. Rectal endometriosis: results of radical excision and review of published work. ANZ J Surg. 2007;77(7):562–571. doi: 10.1111/j.1445-2197.2007.04153.x. [DOI] [PubMed] [Google Scholar]


