Abstract
We report a case of a nine-year-old boy with a 4-week history of general fatigue, loss of appetite, vomits and hematemesis. Laboratory evaluation revealed a hemoglobin level of 4.4 g/dl. After a transfusion of packed red blood cells the patient underwent an esophagogastroduodenoscopy, which showed a smooth, rounded 6–8 cm submucosal lesion with a central depression with ulceration and active bleeding in the cardia extending to the fundus.
Computed tomography (CT) of the chest, abdomen and pelvis showed a large mass originating from the gastric wall but not infiltrating surrounding organs, approximately 8.0 cm × 7.0 cm × 5 cm. Despite the tumor size, no metastases were diagnosed. The patient underwent a total gastrectomy in an en-bloc resection including the distal part of the esophagus (3 cm) and omentum with oncologic margins. Reconstruction was performed with a mediastinal end-to-side esophago-jejunal anastomosis. Immunehistochemic confirmed GIST. He remains well without evidence of disease after 36 months of follow-up with a multiprofessional team.
Keywords: Gastrointestinal stromal tumor, Abdominal tumor, Submucosal tumors, Gastrointestinal bleeding, c-KIT, Children, Gastric, Diagnosis
1. Introduction
Gastrointestinal stromal tumors (GIST) are uncommon mesenchymal neoplasms that are typically described in adults older than 40 years with a peak incidence in the sixth and seventh decades.1 These tumors seem to be very rare in children and young adults. They have malignant potential, but their behavior has been difficult to predict. Furthermore, the clinical characteristics of GIST in children and differences between adult and child cases are not clearly understood.2
We report a case of a gastric GIST in a 9-year-old boy who presented with anemia and gastrointestinal bleeding. Endoscopic findings, clinical course, differential diagnosis and treatment options are reviewed.
2. Case report
A nine-year-old boy presented with general fatigue, loss of appetite and vomiting as for the last four weeks was referred to our hospital after an episode of hematemesis. He had no contributory medical history and family history for cancer or other chronic diseases was negative. The parents reported loss of 4 kg of body in a month. There was no history of melena or trauma. Initial examination was notable for pallor, lethargy and tachycardia (140 beats per minute – bpm). His abdominal examination was unremarkable (Fig. 1).
Fig. 1.
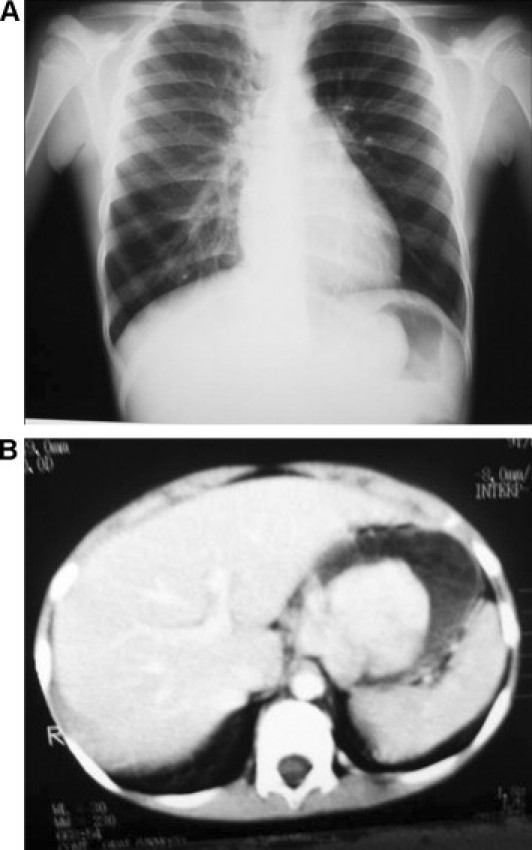
(A) Plain chest radiography with a image of a lesion inside the stomach. (B) Computed tomography (CT) of the abdomen showing a large mass originating from the gastric wall but not infiltrating surrounding organs.
Laboratory evaluation revealed a hemoglobin level of 4.4 g/dl, platelet count of 871,000 cells/mm,3 normal results of coagulation studies and metabolic screening. After a transfusion of packed red blood cells (300 ml) the patient underwent an esophagogastroduodenoscopy, which showed a smooth, rounded 6–8 cm submucosal lesion with a central depression with ulceration and active bleeding in the cardia (posterior) extending to the fundus. Biopsies were inconclusive.
Computed tomography (CT) of the chest, abdomen and pelvis showed a large mass originating from the gastric wall but not infiltrating surrounding organs, approximately 8.0 cm × 7.0 cm × 5 cm (Fig. 2). Tumor markers such as α-fetoprotein, CEA and Ca19-9 were not elevated. After stabilization with blood transfusion and saline solution, surgery was planned.
Fig. 2.
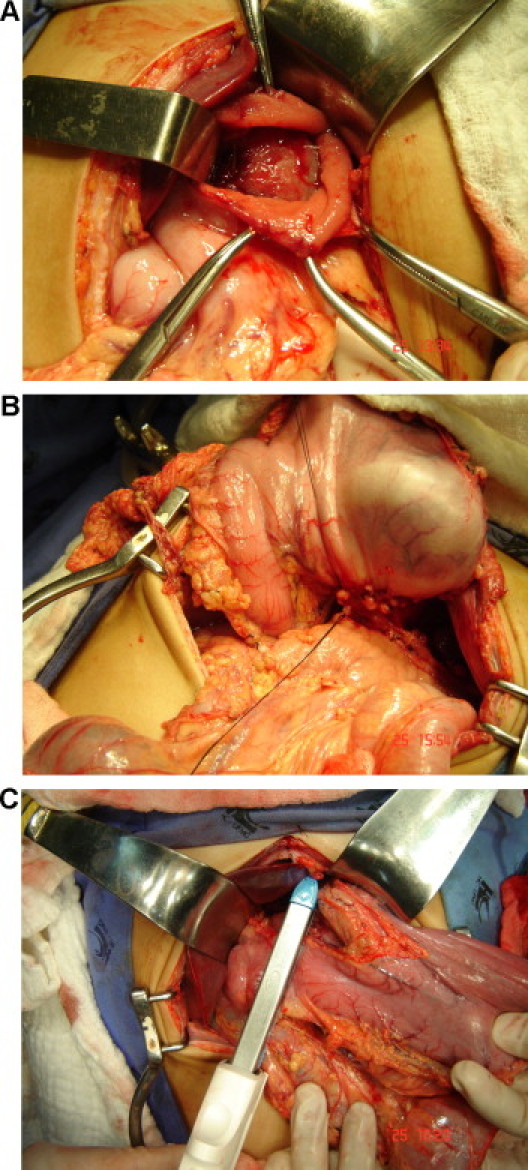
(A) Operative image after opening the anterior gastric wall. (B) View of the posterior gastric wall. (C) Total gastrectomy being performed using a linear stapler.
The patient underwent a median laparotomy with a total gastrectomy in an en-bloc resection including the distal part of the esophagus (5 cm) and omentum with oncologic margins (D2 resection). Reconstruction was performed with a Roux-en-Y esophago-jejunal anastomosis. A nasoenteric tube was placed for early enteral feeding. No liver metastasis or other abnormalities was seen in the abdominal cavity (Figs. 2 and 3).
Fig. 3.
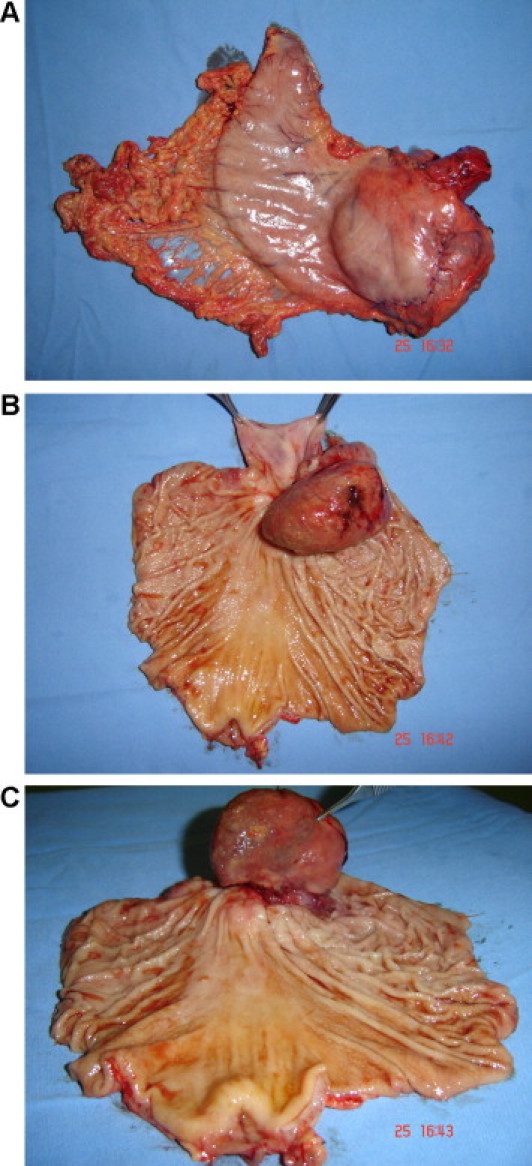
(A–C) En-bloc gastrectomy.
Early enteral feeding was initiated on the third postoperative day. Barium swallow with follow-through in the 11th postoperative day showed anastomosis with no abnormalities and oral feeding was began. The postoperative course was uneventful and the patient was released 20 days after surgery.
The histology assessment was suggestive of a GIST with a reduced mitotic index. In immunehistochemical staining, the tumor stained positive for c-KIT (CD-117) and actin 1 to 4, but negative for PS-100, desmine and vimentine. From these findings, the diagnosis of GIST was made. All margins were negative for tumor involvement.
The patient was followed monthly. CT of abdomen after 12 and 24 months showed no disease.
The patient is using ferrous sulfate and vitamin B12, is gaining weight and laboratory tests are normal. He remains well without evidence of disease after 36 months of follow-up (Fig. 4).
Fig. 4.

Esofagogram after 2 years with no abnormalities.
3. Discussion
GISTs are the most common mesenchymal tumor of the gastrointestinal tract in adults. Pediatric GIST cases are rare and have been reported to represent only 1.4% of all GIST cases. The classification as a GIST requires immunohistochemical assays, characterized as being uniformly positive for stem cell factor CD34 and c-kit (CD-117), variably positive for S-100 and negative for desmin. This distinguishes GISTs from other gastrointestinal smooth muscle tumors such as leiomyomas and leiomyosarcomas.1,3
Literature describes GISTs arising from the interstitial cells of Cajal, a cell having neural and muscular attributes, which primary functions as the pacemaker for muscular motility of the gastrointestinal tract. Both the interstitial cells of Cajal and GIST cells express the receptor tyrosine kinase KIT and the immunohistochemical marker for KIT (CD-117).2,3
In adults, the occurrence of metastatic disease is rare. However in children metastases are seen at the time of diagnosis in more than 50% of pediatric patients.4 Liver involvement or multifocal omental implants has been described as the most common location of metastatic spread. GISTs can occur anywhere along the gastrointestinal tract, including stomach (70%), small intestine (20–30%), anorectum (7%), colon, and esophagus.2
Presenting signs and symptoms are variable depending on the size and anatomic location of the tumor and can include abdominal pain, hematemesis, melena, and anemia from occult gastrointestinal bleeding.4
The use of CT or abdominal ultrasound has been the most frequently used imaging tools to establish the diagnosis of GIST. Typically, the lesion is a lobulated, irregular, intraluminal mass, which contains ulcerations and which may be quite large. Further imaging such as CT and MRI are indicated to show the exophytic component of this tumor as well as the presence of hepatic metastases. CT shows a rounded, low-attenuation mass, which does not enhance with intravenous contrast. MRI shows a rounded increased T2 signal mass that does not significantly enhance with intravenous gadolinium and can be helpful in confirming gastric origin and identifying multifocal disease.1
GIST appears as a submucosal mass of varying size with normal overlying mucosa in esophagogastroduodenoscopy. Although endoscopic biopsy of the mass can be performed, in some cases may not yield enough deep tissue to establish the diagnosis. Because of the depth of involvement of the lesions, snare resection is usually not possible and may result in gastric perforation and uncontrollable bleeding. Endoscopic ultrasound (EUS) is precise for distinguishing different types of submucosal masses.1
Prognostic factors for GISTs include location, size, and histology. A majority of these tumors are clinically indolent with an excellent long-term prognosis. Tumors that are larger than 5 cm are also thought to be associated with worse survival. The likelihood of metastatic disease correlates with tumor size and degree of mitotic activity: one mitosis or fewer per 10 (higher power fields (HPF) is considered to be low grade, whereas 2 or more mitoses per 10 HPF is thought to have a greater malignant potential.3–6
Surgical resection is considered the current standard of care for GIST, and lymphadenectomy has not been shown to improve survival.3 Although the response to conventional chemotherapy and radiotherapy is poor, the oral protein kinase inhibitor, imatinib mesylate, has shown promising antiproliferative and apoptotic effects and may be beneficial for patients with GISTs, particularly those with recurrent metastatic disease.1,4 The indication for adjuvant imatinib mesylate therapy has not been established in pediatric GIST cases thus far.4 Because of the infrequency of GIST in pediatric patients, there is currently no standardized treatment protocol.1,7
The 5-year survival rates for GISTs have ranged from 32% to 63% after complete surgical resection. Treatable recurrences are not uncommon and may reflect initial insufficient excision or multifocal disease escaping surgical detection at the outset.
Imaging postoperative surveillance is performed with magnetic resonance, CT and positron emission tomographic scanning to evaluate for recurrent disease.
4. Conclusion
Gastrointestinal stromal tumor in children are rare but should be considered in the etiology of bleeding and submucosal gastric masses, specially in the gastric antrum. It may present with acute gastrointestinal bleeding, chronic gastrointestinal blood loss, anemia, abdominal pain and left upper quadrant abdominal mass. GISTS tends to be more aggressive in pediatric population, being surgical resection the best current standard of care.
Conflict of interest statement
No conflict of interest.
Funding
No sources of funding.
Ethical approval
Written informed consent was obtained.
References
- 1.Muniyappa P., Kay M., Feinberg L., Mahajan L., Stallion A., Wyllie R. The endoscopic appearance of a gastrointestinal stromal tumor in a pediatric patient. J Pediatr Surg. 2007;42:1302–1305. doi: 10.1016/j.jpedsurg.2007.04.041. [DOI] [PubMed] [Google Scholar]
- 2.Park J., Rubinas T.C., Fordham L.A., Phillips J.D. Multifocal gastrointestinal stromal tumor (GIST) of the stomach in a 11-year-old girl. Pediatr Radiol. 2006;36:1212–1214. doi: 10.1007/s00247-006-0297-9. [DOI] [PubMed] [Google Scholar]
- 3.Durham M.M., Gow K.W., Shehata B.M., Katzenstein H.M., Lorenzo R.L., Ricketts R.R. Gastrointestinal stromal tumors arising from the stomach: a report of three children. J Ped Surg. 2004;39:1495–1499. doi: 10.1016/j.jpedsurg.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 4.Hayashi Y., Okazaki T., Yamataka A., Yanai T., Yamashiro Y., Tsurumaru M. Gastrointestinal stromal tumor in a child and review of the literature. Pediatr Surg Int. 2005;21:914–917. doi: 10.1007/s00383-005-1511-9. [DOI] [PubMed] [Google Scholar]
- 5.Miettinnem M., Lasota J., Sobin L.H. Gastrointestinal stromal tumors of the stomach in children and young adults. Am J Surg Pathol. 2005;29:1373–1381. doi: 10.1097/01.pas.0000172190.79552.8b. [DOI] [PubMed] [Google Scholar]
- 6.O'Sullivan M.J., McCabe A., Gillett P., Penman I.D., MacKinlay G.A., Pritchard J. Multiple gastric stromal tumors in a child without syndromic association lacks common KIT or PDGFR mutations. Pediatr Dev Pathol. 2005;8:685–689. doi: 10.1007/s10024-005-0083-y. [DOI] [PubMed] [Google Scholar]
- 7.Prakash S., Sarran L., Socci N., DeMatteo R.P., Eisenstat J., Greco A.M. Gastrointestinal stromal tumors in children and young adults: a clinicopathologic, molecular, and genomic study of 15 cases and review of the literature. J Pediatr Hematol Oncol. 2005;27:179–187. doi: 10.1097/01.mph.0000157790.81329.47. [DOI] [PubMed] [Google Scholar]


