Abstract
Context
Primary hydatid disease of the pancreas is very rare and even rarer to cause pancreatitis.
Case report
We report the case of a 20-year-old man who presented with abdominal pain and an epigastric mass. A diagnosis of a pancreatic hydatid cyst was established by ultrasonography and CT scan before surgery. The treatment consisted of laparoscopic cyst evacuation with omentoplasty. The recovery was uneventful and the patient has remained symptom free so far.
Conclusions
Hydatid disease should be considered in the differential diagnosis of all cystic masses in the pancreas, especially in the geographical regions where the disease is endemic.
Keyword: Primary hydatid cyst of pancreas
1. Introduction
Hydatidosis is caused by the larval stage of Echinococcus granulosus, which remains endemic in many countries of the world.1,2 The cystic form of hydatid disease affects mainly sheep and cattle raising countries of Middle East and other parts of world including India, New Zealand, Australia, Turkey and South Europe.3–5 The liver, lung, kidney, spleen, and brain are the most commonly affected organs, with infestation of bone, thyroid, breast and pancreas rarely encountered.6 Pancreatic location of hydatid disease is extraordinarily rare with an incidence of less than 1% as compared to the sites of hydatid disease7,8 and even rarer to cause pancreatitis. Clinical presentation varies according to the anatomic location of the cyst.
The diagnosis is rarely made before surgery but is currently facilitated by ultrasonography and CT scan which is helpful in identifying the presence of multiloculation, curvilinear calcification or presence of daughter cells. A definitive diagnosis of hydatid disease of pancreas can be made only at surgery and during surgical treatment extreme caution must be taken to avoid rupture of the cyst.
2. Case report
A 20-year-old male presented in February 2010 to our hospital with epigastric pain which is radiating to back, occasional vomiting, and an epigastric mass of 3month duration. On general physical examination the patient had normal vital signs with a blood pressure of 124/80 mm Hg and a pulse rate of 78/min. There was no lymphadenopathy. Recorded temperature was normal. Chest, cardiovascular, central nervous, and the musculoskeletal systems were normal on examination. On abdominal examination, there was mild epigastric tenderness with no rigidity or guarding, with fullness in the epigastric area. There was no organomegaly. Laboratory investigations revealed a haemoglobin level of 12.8 g/dl, WBC 11,800/mm3 and serum amylase 4965 U/L and other blood chemistry, including liver function tests, chest X-ray, ECG and urine examination revealed no abnormalities. Abdominal ultrasonography showed a cystic mass lesion of 8 cm in diameter over the head of the pancreas with oedematous body and tail and the rest of the examination was normal. CT scan of the abdomen confirmed the presence of an oval solitary cyst measuring 8 cm × 8 cm in the head of pancreas causing compression over the pancreatic duct (Fig. 1). The cyst was homogenous and well delineated and it had curvilinear membrane. There was peripancreatic inflammation with diffuse pancreatic oedema. There was single fluid collection around tail of pancreas due to pancreatitis. There were no cysts in other abdominal viscera. The lesion showed no enhancement on contrast-enhanced CT. A preoperative diagnosis of hydatid cyst of the pancreas was made and laparoscopy was done; on laparoscopy there was a cystic mass pushing the stomach and transverse colon upwards. Dissection was carried out in gastrocolic ligament to reach the retroperitoneal space. There was a cystic mass over the head of the pancreas. Under direct vision 10 mm port was placed into the cyst with suction attached to it (Fig. 2). Camera was introduced through that port to see content of cyst. There was no communication with main pancreatic duct. Cyst evacuation was performed leaving behind adventia and cyst cavity was obliterated with omentoplasty. The rest of the abdominal organs including the liver were normal. Histopathology confirmed the diagnosis of hydatid cyst. The postoperative period was uneventful and the patient was discharged on postoperative day 7. The patient was given albendazole (10 mg/kg) for 3months. The clinical and ultrasonographic follow-up has shown no recurrence.
Fig. 1.
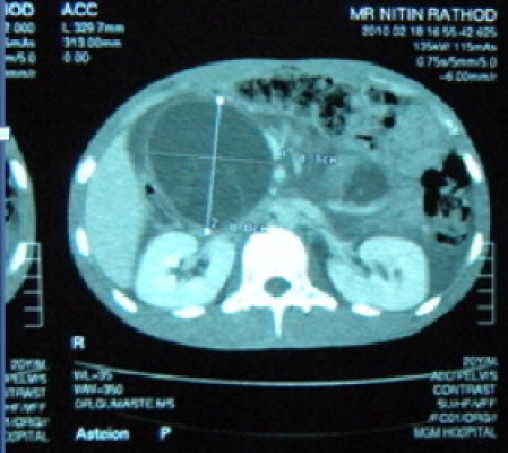
Contrast enhanced CT of abdomen showing rounded cystic lesions with curvilinear laminated membrane at head of pancreas.
Fig. 2.
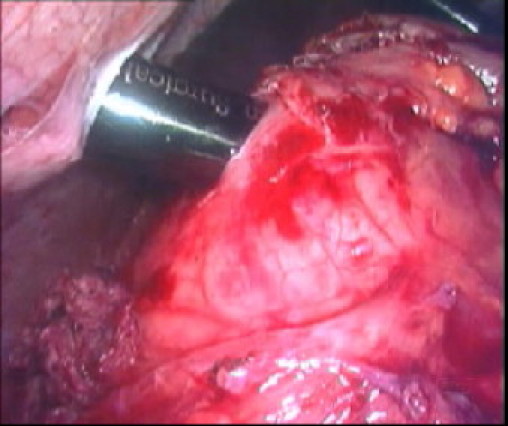
Insertion of 10 mm port directly into cyst wall laparoscopically.
3. Discussion
The pancreas is an organ rarely infected by hydatid cysts, and the figures taken from the literature give an incidence ranging between 0.19 and 2% of the various sites of hydatid disease.8 The embryos of hydatid cysts end up in the pancreas mainly by the haematological route or by peripancreatic lymphatic invasion but very rarely by retroperitoneal spread9; even local spread via the pancreatic or bile ducts has been suggested. Pre-operative diagnosis may be difficult due to the similarity of the presenting symptoms and the radiological findings to those of other more commonly encountered cystic lesions of the pancreas.10 Clinical presentation varies according to the size and anatomic location of the cyst within the pancreas and the degree of bilio-pancreatic involvement.8 Abdominal pain, discomfort and vomiting are the main clinical symptoms. The patient may present with obstructive jaundice, weight loss, epigastric mass, and/or recurrent acute pancreatitis.11 Ultrasonography will typically demonstrate a cyst with a wall of varying thickness. Computed tomographic findings, such as rounded cystic lesions with curvilinear calcification, may allow the diagnosis to be made in the appropriate clinical setting.11,12 Routine blood chemistry, apart from the indirect fluorescent antibody test, latex agglutination test, and enzyme-linked immuno-absorbent assay (ELIZA) test for echinococcal antigens, which is positive in over 85% of infected patients,2 has very little to offer in reaching a correct pre-operative diagnosis. A definitive diagnosis of hydatid disease of the pancreas can be made mainly at surgery.
The treatment of hydatid cyst is mainly surgical. However, pre and postoperative 1 month course of albendazole and 2 week of praziquantel can help in sterilizing the cyst, decrease the chance of anaphylaxis and reduce the recurrence rate postoperatively.11,12,2 Depending on the site, various methods of surgical treatment have been used. For cysts located in the head, pericystectomy is the ideal method of treatment, as was performed in the present case. The surgical treatment of pancreatic hydatid disease is complete excision of the cyst. During surgical treatment of hydatid cysts, extreme caution must be taken to avoid rupture of the cysts, which would release protoscolices into the peritoneal cavity. Other surgical procedures, such as partial cystectomy, cysto-enteric anastomosis, and omentoplasty, are possible. In cases of a large cyst with extensive adherence to the surrounding pancreatic parenchyma, a cystogastrostomy may be a satisfactory treatment.13 A hydatid cyst in the tail of the pancreas can be successfully treated with a distal pancreatectomy.2
Although the incidence of hydatid disease in the West is low, we believe that immigration from endemic areas and the wide travelling of people might lead to an increase in the incidence of hydatid disease cases that a Western physician may encounter in the future.
We conclude that pancreatic hydatidosis, though very rare, should be considered in the differential diagnosis of cystic lesions of the pancreas in the appropriate epidemiological areas.
Conflict of interest statement
None.
Funding
None
Ethical approval
Written and signed consent to publish the case report from the patient taken.
Contributor Information
Pravin Suryawanshi, Email: dr_pravin@hotmail.com.
Sudhir Jatal, Email: jatal.sudhir835@gmail.com, sudhirjatal@rediffmail.com.
References
- 1.Bouree P. Hydatidosis: dynamics of transmission. World J Surg. 2001;25:4–9. doi: 10.1007/s002680020001. [DOI] [PubMed] [Google Scholar]
- 2.Sayek I., Onat D. Diagnosis and treatment of uncomplicated hydatid cyst of the liver. World J Surg. 2001;25:21–27. doi: 10.1007/s002680020004. [DOI] [PubMed] [Google Scholar]
- 3.Altinors N., Senveli E., Donmez T. Management of problematic intracranial hydatid cysts. Infection. 1995;23:283–287. doi: 10.1007/BF01716287. [DOI] [PubMed] [Google Scholar]
- 4.Brown R.A., Millar A.J.W., Steiner Z. Hydatid cyst of the pancreas: a case report in a child. Eur J Pediatr Surg. 1995;5:121–124. doi: 10.1055/s-2008-1066184. [DOI] [PubMed] [Google Scholar]
- 5.Goel M.C., Agarwal M.R., Misra A. Percutaneous drainage of renal hydatid cyst: early results and follow-up. Br J Urol. 1995;75:724–728. doi: 10.1111/j.1464-410x.1995.tb07379.x. [DOI] [PubMed] [Google Scholar]
- 6.Amr S.S., Amr Z.S., Jitawi S., Annab H. Hydatidosis in Jordan: an epidemiological study of 306 cases. Ann Trop Med Parasitol. 1994;88:623–627. doi: 10.1080/00034983.1994.11812913. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez Vargas J., Arroyo Carrera I., Pitarch Esteve V. Pancreatic hydatid cysts. Cir Pediatr. 1992;5:46–47. [PMID 1567748] [PubMed] [Google Scholar]
- 8.Khiari A., Mzali R., Ouali M., Kharrat M., Kechaou M.S., Beyrouti M.I. Hydatid cyst of the pancreas. Apropos of 7 cases. Ann Gastroenterol Hepatol (Paris) 1994;30:87–91. [PMID 8067682] [PubMed] [Google Scholar]
- 9.Ismail K., Haluk G.I., Necati O. Surgical treatment of hydatid cysts of the pancreas. Int Surg. 1991;76:185–188. [PubMed] [Google Scholar]
- 10.Krige J.E., Mirza K., Bornman P.C., Beningfield S.J. Primary hydatid cysts of the pancreas. S Afr J Surg. 2005;43:37–40. [PubMed] [Google Scholar]
- 11.Safioleas M.C., Moulakakis K.G., Manti C., Kostakis A. Clinical considerations of primary hydatid disease of the pancreas. Pancreatology. 2005;5:457–461. doi: 10.1159/000086548. [DOI] [PubMed] [Google Scholar]
- 12.Missas S., Gouliamos A., Kourias E., Kalovidouris A. Primary hydatid disease of the pancreas. Gastrointest Radiol. 1987;12:37–38. doi: 10.1007/BF01885099. [DOI] [PubMed] [Google Scholar]
- 13.Moosavi S.R., Kermany H.K. Epigastric mass due to a hydatid cyst of the pancreas. A case report and review of the literature. JOP. 2007;8:232–234. [PubMed] [Google Scholar]


