Abstract
The majority of ingested foreign bodies will pass through the gastrointestinal tract without incident, with less than 1% of cases resulting in complications. Herein we present a case of small bowel perforation secondary to the accidental ingestion of a dental plate. A diagnosis of perforation was made by CT imaging, but the exact cause could only be determined after resection of the affected bowel and histo-pathological examination. We re-iterate the importance of accurate and thorough history taking in patients with possible foreign body ingestion.
Keywords: Bowel perforation, Dental plate, Foreign body
1. Introduction
The ingestion of foreign bodies, whether intentional or accidental, is not uncommon amongst the general population.1 Most foreign bodies will pass through the gastrointestinal tract without consequence, but around 1% of cases will see complications including bowel perforation.2 Patients can not always recall ingesting a foreign body and examples within the literature include chicken3 and fish bones.4 Here we present a case of small bowel perforation secondary to the accidental ingestion of a plastic dental plate. The diagnosis could only be made following resection of the affected bowel and histo-pathological examination.
2. Presentation of case
A 50-year-old gentleman was referred to the surgical team with a 1-day history of generalised abdominal pain, fever and vomiting. His past medical history included type 2 diabetes mellitus and a previous open right inguinal hernia repair. Routine observations revealed a low-grade pyrexia of 37.5 °C, pulse rate of 100 beats per minute, normotensive blood pressure and oxygen saturations of 100% on room air. Physical examination confirmed generalised abdominal tenderness with involuntary guarding in the left iliac fossa. Normal bowel sounds were heard on auscultation and rectal exam demonstrated soft stool with no blood and no palpable masses. Initial blood tests were all within normal limits except for a mildly elevated c-reactive protein of 40 mg/L. Subsequent plain abdominal and erect chest films (Fig. 1) showed multiple dilated loops of small bowel, suggestive of a degree of obstruction, but no pneumoperitoneum.
Fig. 1.
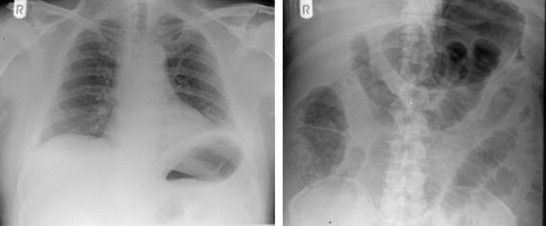
Erect chest X-ray and supine abdominal X-ray showing multiple loops of dilated small bowel.
After 24 h with no improvement in the patients symptoms, a CT-scan was requested (Fig. 2). A long segment of abnormal proximal ileum, with a thickened wall and localised inflammatory changes, was reported. Pockets of free air were seen within the mesentry suggestive of a localised perforation. Lymphadenopathy within the small bowel mesentery, close to the right ileocolic vessels lead to a differential diagnosis including lymphoma and Crohn's disease.
Fig. 2.
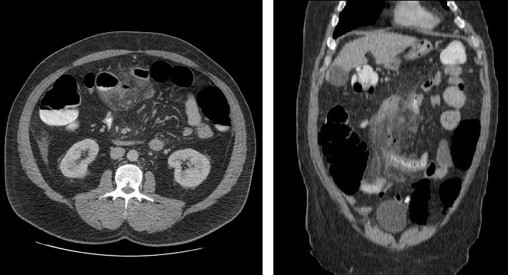
CT images illustrating a long segment of abnormal proximal ileum, with a thickened wall and localised inflammatory changes. Pockets of free air are noted within the mesentry.
The patient underwent an emergency laparotomy where he was found to have a 65 cm area of small bowel matted together with an intra-loop abscess, 60 cm upstream from the ileocaecal valve. The central position of the abscess contained thickened small bowel that macroscopically did not look typical of malignancy. A single-band adhesion from this area of small bowel to the omentum was also noted and it was thought that this adhesion may have caused chronic inflammatory small bowel obstruction and subsequent perforation. The area was resected and a primary anastomosis completed.
The patient's post-operative recovery was complicated by a respiratory arrest secondary to opioid excess, from which he made a full recovery. Histopathological examination of the tissue reported a plastic dental plate bearing two teeth that were embedded in the bowel – the sharp edges being responsible for the perforation (Fig. 3). The adhesion to the adjacent loop was located at the site of the perforation, sealing it off. When informed about the histopathology result at follow-up, the patient could recall accidentally swallowing the dental plate when eating a sandwich a couple of weeks prior to admission.
Fig. 3.

AP view of the recovered dental plate.
3. Discussion
Foreign body ingestion is most commonly seen in children, alcoholics, people with mental health problems and people wearing dental prostheses.5 Most foreign bodies will traverse the gastrointestinal tract uneventfully, however between 10 and 20% will fail to pass. Less than 1% of cases are reported to lead to complications.2 Elongated and/or sharp objects often impact at points of intestinal narrowing, with 83% of perforations occurring within the ileum.3
The clinical presentation of complicated foreign body ingestion is variable and includes bowel obstruction, abscess formation, recurrent sepsis and bowel perforation with generalised peritonitis. In the case of the latter, it is very difficult to differentiate foreign body perforation from any other cause of bowel perforation on physical examination alone. In this instance, an accurate and complete patient history is vital to making the diagnosis, prior to any further investigations. We have presented a case of small bowel perforation secondary to accidental dental plate ingestion which could only be diagnosed after histopathalogical examination of tissue removed following a small bowel resection. The patient involved in this case report was never questioned about the possibility of foreign body ingestion, despite the fact his dental plate was missing throughout his inpatient stay (Fig. 4). Remarkably when questioned at follow-up he could clearly recall accidentally swallowing the dental plate.
Fig. 4.
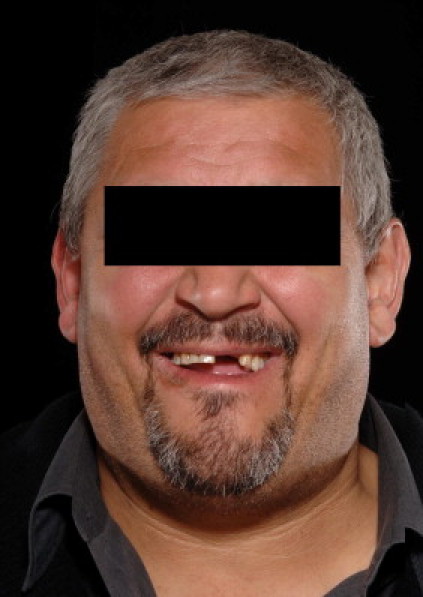
The patient smiling without his dental plate.
The base used in the reconstruction of dental prostheses is methylmethacrylate – a type of plastic which is radiolucent and thus difficult to identify on imaging studies. CT scans of the abdomen have been reported to have a high performance in identifying intestinal perforation caused by alimentary foreign bodies.6 With respect to this case, it did successfully identify the small bowel perforation (not detectable on plain abdominal or chest films), but failed to attribute it to an ingested foreign body.
Patients that present with abdominal pain of unknown cause with muscle guarding should always be questioned about their recent food intake, including the possibility of foreign body ingestion. In this case the patient was not questioned and was observed for 24 h before having a CT scan. However, it is unclear whether the patient would have been able to recall ingestion of his dental plate at the time of admission. Ultimately CT scanning provides detailed imaging of the abdomen and accurately picks up the serious complications associated with foreign body ingestion, such as perforation. This patient was able to have a prompt laparotomy and small bowel resection with primary anastomosis and made a full recovery.
4. Conclusion
This case report highlights the importance of accurate and thorough history taking in patients presenting with abdominal pain attributable to foreign body ingestion. In such cases, CT imaging is vital in recognising complications, such as perforation, but may not always be able to identify the offending object.
Funding
None.
Conflict of interest statement
All authors have no competing interests.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author's contributions
All authors contributed to this case report. Peter John Webster was responsible for drafting the article, literature search, acquisition of data (images); Adam Peckham-Cooper contributed towards drafting of the article and acquisition of data (images); Mark Lansdown supervised the project and did critical revision prior to final submission.
References
- 1.Goh B.K., Chow P.K., Quah H.M., Ong H.S., Eu K.W., Ooi L.L. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg. 2006;30:372–377. doi: 10.1007/s00268-005-0490-2. [DOI] [PubMed] [Google Scholar]
- 2.Velitchkov N.G., Grigorov G.I., Losanoff J.E., Kjossev K.T. Ingested foreign bodies of the gastro-intestinal tract: a retrospective analysis of 542 cases. World J Surg. 1996;20:1001–1005. doi: 10.1007/s002689900152. [DOI] [PubMed] [Google Scholar]
- 3.Singh R.P., Gardner J.A. Perforation of the sigmoid colon by a swallowed chicken bone: case reports and a review of literature. Int Surg. 1981;66:181–183. [PubMed] [Google Scholar]
- 4.Bhatia R., Deane A.J., Landham P., Schulte K.M. An unusual case of bowel perforation due to fish fin ingestion. Int J Clin Pract. 2006;60:229–231. doi: 10.1111/j.1742-1241.2006.00610.x. [DOI] [PubMed] [Google Scholar]
- 5.Hunter T.B., Taljanovic M.S. Foreign Bodies Radiographics. 2003;32:731–757. doi: 10.1148/rg.233025137. [DOI] [PubMed] [Google Scholar]
- 6.Coulier B., Tancredi M.H., Ramboux A. Spiral CT and multidetector-row CT diagnosis of perforation of the small intestine caused by ingested foreign bodies. Eur Radiol. 2004;14:1918–1925. doi: 10.1007/s00330-004-2430-1. [DOI] [PubMed] [Google Scholar]


