Abstract
Rhinoplasty is considered to be one of the most challenging procedures in otolaryngology head and neck surgery. Meticulous planning and excellent surgical skills are pre-requisites for reproducible good outcomes. More than 100 years after the first rhinoplasty, many controversies regarding indication and techniques remain unresolved. The aim of this article is to review current concepts and arguments.
Keywords: rhinoplasty, psychology, surgical technique, indication, osteotomy, alar cartilage surgery, augmentation rhinoplasty
1 Introduction
Rhinoplasty is a frequent operation that only few surgeons are considered to truly master the wide scope of technical nuances [1], [2]. Rhinoplasty was said to be a procedure that is not too difficult to carry out but extremely challenging for consistent outstanding results [1]. Rhinoplastic changed considerably in the last decades from a standardised reduction procedure to a highly differentiated problem oriented procedure with reductions, relocation and augmentation of tissues are frequently combined [3]. In addition, different techniques are popularised by opinion leaders [4]. These sometimes contradictory approaches can be confusing and intimidating for both the novice and the advanced surgeon. Even the expert will admit that “noses are difficult to predict” [5].
1.1 A look back
John Orlando Roe entered history as the father of aesthetic rhinoplasty after having reported a “simple operation” in 1887 describing the correction of a “pug nose” through an endonasal approach [6]. Four years later Roe performed endonasal hump reductions [7]. It was seven years later that Jacques Joseph published similar techniques, presumably without knowledge of Roe’s reports. Joseph is generally accepted as the founder of functional rhinoplasty. In 1982 Weir described the technique of “nasal infraction”, augmented saddle noses with implants made of duck-sternum and described the rotation of the drooping tip by a wedge excision from the caudal septum. The latter technique is today still named after him. The first transplantation of costal cartilage was published by Mangoldt in1900 [7]. Many new instruments were introduced between the 1960’s and 1980’s [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18]. At the time, various modifications of osteotomes replaced the hand-held saw for the lateral osteotomy. Reports on the use of a drill in 1981 were long forgotten when the development of shavers and endo-nasal drill systems 20 years later brought up the discussion of powered instrumentation for rhinoplasty again, indicating the unresolved issues regarding ideal instrumentation.
1.2 A look ahead
Reliable data on growing interest in facial plastic surgery in Europe are not available. In the US the number of facial plastic surgical procedures increased by 34% between 2000 and 2004 [19]. This increase was mainly attributable to the popularity of non-surgical procedures such as botulinum toxin and fillers, whereas the most popular aesthetic procedures were blepharoplasty followed by rhinoplasty [19]. The impression shared by many facial plastic surgeons is that there is a growing interest in rhinoplasty in Europe as well and this trend is expected to become stronger.
2 Indication
2.1 The patient
2.1.1 Motivation
Patients who undergo surgery for a functional problem frequently appreciate the aesthetic aspect of the procedure even though the indication is mainly functional. We know little about what motivates the patient to accept the inconvenience, risk and financial burden of an operation aimed at aesthetic improvement. In most patients, the wish to undergo surgery is not related to the objective degree of deformity. In addition, psychometric data do not correlate with the degree of deformity [20]. Patients whose motivation is primarily aesthetic are psychologically more distressed compared to patients whose indication is mainly functional [21]. For patient satisfaction after functional aesthetic rhinoplasty, meeting the aesthetic expectations of the patient was found to be more important than the functional outcome [22]. The mere fact that rhinoplasty patients pay more attention to deformities that may remain unnoticed by peers and would not cause distress in subject not considering a rhinoplasty is a clear indicator of a psychological alteration in the rhinoplasty patient. Dissatisfaction with appearance is most pronounced in rhinoplasty patients compared to candidates for other aesthetic procedures [23] and the mirror daily reminds the patient of the deformity causing distress, mostly since puberty [24], [25]. Eight out of 10 patients are motivated by their wish for a change or seeing the outcome of successful surgery in others [25], [26]. The step of applying for surgery is frequently taken when self-esteem declines with advancing age or when patients take on the role of “highly motivated doers” who simply wish to improve their appearance [27], [28], [29]. Both patients and surgeons expect the improved appearance to foster self esteem, reduce social anxiety, obsessiveness, hostility and paranoia, and thereby improve quality of life [21], [23], [30], [31], [32], [33], [34]. These positive changes can be attributed to the operation and not to other circumstances as the improvement of self esteem becomes more pronounced with passing time after surgery [32]. From this perspective the operation may be seen as a psycho-therapeutic intervention [35], [36]. None the less, it remains unclear to what extent the patients benefit psychologically from a rhinoplasty [37].
2.1.2 Rhinoplasty and body image
In early psychoanalytic studies [38], [39] dissatisfaction with appearance was interpreted as a projection of inner conflicts [22]. Patients were described as obsessive and narcissistic and were considered to be candidates for the psychiatric couch rather than the operating table. Later studies based on clinical interviews came to the conclusion that the majority of patients had psychological alterations such as personality disorders including neurotic and obsessive disorders [30], [31], [40], [41]. Other authors opposed to the clinical relevance of these findings [42], [43]. Psychiatric disorders were seen as a contraindication because of the high risk of post-operative dissatisfaction [44], [45] even though this opinion was not backed by clear evidence. From a psychiatric perspective more than eight out of ten patients with diagnosed psychological abnormalities did benefit from the operation [46], [47] with patients experiencing a new social identity after surgery [22].
2.1.2.1 Body image disorder and dysmorphophobia
An altered perception of own appearance that causes distress is called body dysmorphic disorder or, in its extreme form, dysmorphophbia [48]. Body image disorder is found in 7-10% of aesthetic surgical patients [48]. Body image disorder typically manifests during adolescence and surgeons should be especially alert when young patients apply for aesthetic surgery. The most frequent causes for distress are acne and hair loss followed by the appearance of the nose. It is estimated that 26-40% of the patients with a body dysmorphic disorder received the procedure they applied for [48], even though body dysmorphic disorder is improved by surgery in 3.6% only, with 25% of the patients reporting a subjective improvement of appearance. Three questions are supposed to help the surgeon screen for body dysmorphic disorder:
Is the degree of preoccupation with a visible deformity not justified from the surgeon’s perspective?
Does this preoccupation cause clinically relevant suffering?
Is this preoccupation not attributable to other psychological disturbances such as anorexia nervosa?
If the answer to these three questions is yes, a severe body image disorder or dysmorphophobia is likely. Even one positive answer is suggestive of a body image disorder and the surgeon should refrain from offering a procedure [49], even though this issue is a matter of debate [48]. Behavioural therapy or medical treatment with SSRI (selective serotonin reuptake inhibitors) should be discussed prior to surgery [48].
2.2 A caveat for the surgeon?
Every experienced rhinosurgeon has operated a number of patients in whom the unfavourable postoperative course clearly indicated that the indication was a mistake. Unfortunately, patients frequently manifest themselves as bad candidates after surgery and one of the major unresolved problems is how to recognise the high risk patient early in the consultation [50], [51]. As reliable criteria have not been defined, the surgeon has to rely on his instinct. Long lists of attributes such as obsessive, perfectionist, compulsive, impolite, flattering etc., have been proposed to help the surgeon [1]. The acronym SIMON (single, immature, male, over-expectant, narcissistic) was coined for the male high-risk patient whereas SYLVIA (secure, young, listens, verbal, intelligent, attractive) can be considered to be a good candidate [1], [52], [53]. These criteria are clearly of little help in face of the individual patient and the first sign of alarm for the surgeon is frequently an intuitive spontaneous feeling of disliking the patient. A psychiatrist condensed the role of instinct into the phrase “if you cannot elicit a smile from your patient, don’t operate” [54].
2.3 Preparation of surgery
2.3.1 Attractiveness and surgical goal
Most textbooks on rhinoplasty include a description of angles and proportions that are generally perceived as being attractive. Leonardo da Vinci and Albrecht Duerer divided the face according to aesthetic principles. This concept was extended by Powell and Humphreys in 1984 [55]. Analyses of the ideal nasal length and nasal tip projection have been proposed to help plan the surgery [2]. Most surgeons, however, keep it simple by looking at the nasolabial angle which should be larger than 90° and 100° for male and female patients respectively. In profile the columella should be 2-3 mm below the inferior border of the nostril and a double break of the columella as well as a slight depression in the supra-tip (supra-tip break) are also found to be pleasing, especially in women [49], [56]. This may be helpful as an orientation for the surgeon but cannot be imposed on the patient in most cases, as the patient is interested in improving appearance and not in matching ideal proportions. Emphasizing the deviation from ideal proportions may be perceived as offensive by the patient who wishes to improve his or her looks and expects personal and ethnic character to be respected [56], [57]. The author of this review has quit analysing facial proportions in favour of computer imaging of the desired outcome. This approach respects the concept that a universal standard of aesthetic proportions does not exist and the shape of the nose should primarily be brought into harmony with individual physiognomy, gender and character [58].
2.4 Assessment of the nose
Visual analysis of the nose will allow the surgeon to accept the patient’s complaint as realistic or acceptable and match the patient’s preferences with surgical options. Careful palpation is equally important to analyse thickness and rigidity of the soft tissue and skin envelope and the length of the nasal bones. Thick skin of the nasal tip should not be overlooked because it significantly reduces the degree to which the tip can be narrowed [59]. Thin skin over rigid alar cartilages ideally lends itself to narrowing of the tip with suture techniques, but carries a high risk of visible asymmetries or irregularities. In sebaceous skin, transcutaneous mattress-sutures carry the risk of infection and permanent visible scars. Short nasal bones should be recognised as a challenging anatomical situation for osteotomies. Even in purely aesthetic indications, the nasal vestibule and nasal cavity should be thoroughly assessed for signs of obstruction or nasal inflammation. Pre-operative plain x-ray or computed tomography has been proposed as a routine examination to rule out sinus pathology [49]. The author of this review relies on endoscopy of the middle meatus and does not include radiological examination in the absence of clinical evidence of sinus disease. Post-operative hyposmia or anosmia has been reported [60]. Olfactory function testing should therefore be part of pre-operative assessment [49]. A threshold and identification test (‘sniffin-sticks’) or a screening discrimination test (‘smell diskettes’) can be used for this purpose [61], [62].
2.5 Photography
Patient’s photographs are the basis for preoperative analysis and planning of the procedure with the patient. In addition, pre- and post-operative photographs are crucial for outcome monitoring and are indispensable from a medico-legal point of view. As a minimum requirement, the whole face en face, both profile views and a basal view should be included. Additional perspectives are both half profile and the view directly from above. Initial scepticism regarding the quality of digital photography [63], is now history and digital techniques are standard. The images should be taken in a standardised fashion, preferably using a dark homogenous background, two flashlights illuminating the face from both sides using a diffuser (‘soft box’). The zoom lens setting should be a moderate tele (80-150 mm SLR equivalent). Images may be archived without compression or in a format of 15x10 cm with 200 dpi resolution. For intra-operative photography, several compact digital cameras lend themselves to packing in a sterile bag with a cut opening for the lens which allows the surgeon or assistant to take advantage of the macro-module.
2.6 Planning and informed consent
Patient information and documentation of informed consent must meet the highest standards in a primarily aesthetic procedure as these procedures have a low priority from a medico-legal perspective [64]. A minimum requirement is an extensive consultation not less than 24 hours before surgery. Preferably a second pre-operative consultation is planned to confirm or modify the initial surgical goal. The author of this review finds it helpful to offer a second consultation for computer imaging and incorporate the result of this imaging into the informed consent. It is prudent to include the information that the result of surgery will differ from the simulated outcome. The patient should confirm that he or she accepts the risk of
a significant discrepancy between the planned and actual outcome,
operative impaired nasal breathing due to scarring,
temporary or long lasting numbness of the nasal tip,
alteration of skin texture and colour,
reduced mechanical stability of the nasal framework after osteotomy,
the eventual necessity of a revision.
The wise surgeon will be ready to inform the patient about personal revision rates and offer an estimate of the risk of needing a revision in the individual patient. The cost of a revision operation should also be discussed prior to the initial surgery.
2.6.1 Computer imaging – Implicit guarantee?
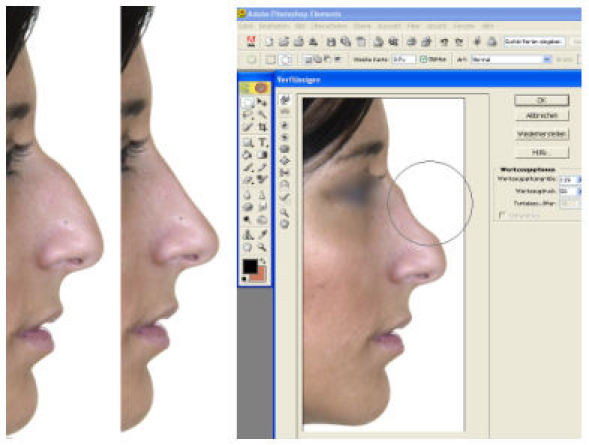
The concern that computer imaging may be turned against the surgeon has been repeatedly discussed in the literature but generally found to be not justified [1], [49], [54], [65], [66]. Computer software for digital imaging is widely available (‘Adobe Photoshop’ e.g.) which allows simulation of a desired outcome in less than one minute (Figure 1 (Fig. 1)). The question remains, whether this is a fair procedure for the patient and a wise step to take for the surgeon. If simulation is used to discuss individual anatomy and possibilities as well as limitations of surgical interventions in a modest and prudent way, the patient will not be encouraged to be over-expectant. The written informed consent should contain the information that the outcome of surgery will differ from the planning image. Pre-operative simulated images should not be handed out to the patient before surgery as this may lead to strong mental fixation in the patient [2]. The prudent surgeon will, in addition, be honest about the chances of fully achieving or coming close to the simulated outcome.
Figure 1. The reduction of a hump (left) may be simulated with the filter “liquify” of the program Adobe Photoshop Elements® (right).
2.6.2 Patient information for the post-operative period
A well informed patient will find it easier to cope with post operative swelling and bruising of the eyelids, nasal obstruction due to mucosal swelling, and the inconvenience of nasal packs. There is no evidence regarding the question “how long the nose should not be exposed to the sun”. In most textbooks, a period of six weeks is recommended [54]. Many patients do not respect this recommendation and permanent hyperpigmentations appear to be rare if patients wear sun protection. Further recommendations such as no alcohol for two weeks, reduced speaking and laughing for ten days, and no physical exercise for six weeks [54] are even found in recent publications [58], but are not accepted by the patient. Wearing glasses during the first six weeks after lateral osteotomies carries the risk of inward dislocation of the nasal sidewall [58]. It is common to accept the result after one year as “final outcome” [1], even though it is common knowledge that mostly unfavourable changes occur well after the first post operative year, such as visible thinning and blanching of the skin over bony or cartilaginous ridges.
2.6.3 Post-operative dissatisfaction: after surgery is before surgery?
A most unpleasant situation is a dissatisfied patient facing a surgeon who is satisfied with his or her performance [67]. It is important to remember that patient dissatisfaction is frequently caused by emotional disappointment rather than by an insufficient surgical technique [68]. If both patient and surgeon are unhappy with the result, the preoperative consultations will be a good basis to discuss a revision. If the surgeon fails to understand the unhappy patient, the surgeon should at all costs avoid opposing to the patient and creating an atmosphere of empathy. Repeated consultations are perceived by the patient as an indication of being taken seriously. In addition, a second opinion from a colleague will be welcomed by the patient as a sign of critical self-reflection by the surgeon who should not forget that malpractice claims are more often caused by insufficient communication than by surgical mistakes.
3 General surgical techniques
3.1 Perioperative measures
3.1.1 Maintaining a dry surgical field
A dry surgical field not only facilitates surgery, but also reduces post-operative swelling and bruising. A low mean arterial pressure and reduced venous pressure by elevation of the head as well as the local injection of a vasoconstrictor are generally accepted. Transient minor alterations of the nasal relief are acceptable as trade-off [54]. The injected volume should not exceed 5-8 ml for a septorhinoplasty [54], [58], [69]. Lidocaine or Ultracaine solutions with 1:200,000 or 1:100,000 adrenalin solutions are most frequently used [49], [69]. For vasoconstriction of the nasal mucosa, pledgets with cocaine solution (10%), adrenalin pledgets (1:5000) or, if contra-indicated, oxymetazoline or naphazoline (1%) can be used. A so-called hydro-dissection or hydraulic dissection [49] of the endonasal mucoperichondrium by forceful infiltration of the Perichondrium does not facilitate dissection in most patients and carries the risk of a systemic reaction to the increased volume of the injected vasoconstrictor. The infiltration of adrenalin into the nasal mucosa causes of one of three haemodynamic instable phases of rhinoplasty with tachycardia and increased blood pressure [70]. The other two unstable phases are anxiety in the immediate pre-operative phase and the lateral osteotomies. If, in exceptional cases, operating times should exceed two hours, hypothermia should be avoided as this has a negative affect on coagulation [71].
3.1.2 Antibiotic prophylaxis
The use of antibiotics in routine rhinoplasty is controversial. Some authors advocate a prophylactic use up to 10 days after surgery using a first generation cephalosporin in revision cases or after transplantation of cartilage with a Chinolone [72], [73]. A recent study demonstrated that one week of post-operative antibiotic prophylaxis did not reduce the post-operative infection rate compared to a single shot prophylaxis but caused significantly more side effects [74]. As antibiotic concentrations peak in the cartilage after 20 minutes, they should be administered upon induction of general anaesthesia [75]. A valid alternative to systemic prophylaxis is intra-operative antibiotic impregnation of cartilage transplants [76]. Bathing the cartilage transplant in an intravenous Chinolone solution impregnates the transplant by free diffusion. Within minutes, a minimal inhibitory concentration (MIC-90) for Pseudomonas species extends up to 1 mm below the surface of the transplant [76]. Free diffusion out of the transplant into surrounding haematoma or seroma will protect a transplant in the immediate post-operative phase. The author of this review has therefore stopped using systemic antibiotic prophylaxis in most cases.
3.1.3 Corticosteroids
Older publications advocated the use of systemic corticosteroids [77]. This is still discussed as an option [2]. A study showed however, that systemic corticosteroids significantly reduced post operative swelling over the eyelids during the first two post operative days only without any effect afterwards [78]. Weighing risks and benefits, systemic corticosteroids should not routinely be used [73]. Local application of Triamcinolone however, was found to be a helpful adjunct to reduce persistent swelling of soft tissue, especially in the supra-tip region [79], [80]. Care should be taken to place the corticosteroids deep subcutaneously to avoid the risk of persistent depigmentation. The most efficient way of avoiding post operative swelling is causing minimal trauma to soft tissues.
3.1.4 Transplants and implants
Transplants are commonly used to reconstruct the supporting structures for the nasal tip, correction of a saddle nose, improvement of the nasal valve function or shape of the nasal tip. Transplants can also be successfully used to recreate harmony by augmenting as opposed to reducing volume and protection. However, this strategy was found to frequently result in well-shaped but subjectively too big noses [5]. In addition, the edges of many cartilage transplants became visible after years due to thinning of the overlying skin. In recent years the number of cartilage transplants to the nasal tip has therefore fallen and suture techniques are increasingly being used [81], [82].
3.1.4.1 Cartilage
Septal, conchal and costal cartilages are good options for structural transplants. If available, septal cartilage is well suited for reconstruction of nasal tip support with a columella strut and improvement of vestibular function due to its rigidity and straight shape. Conchal cartilage in comparison is elastic, which can be of advantage in reconstructing nasal tip support. The transplant is thicker compared to septal cartilage especially if it has to be straightened by suturing two segments face to face but it gives a more natural feel to the tip due to its elasticity. Costal cartilage is considered to be first choice for the augmentation of severe saddle deformities [2], [49], [83], [84], [85]. Partial resorption of transplanted costal cartilage frequently occurs to an unpredictable degree and complete resorption of autologous costal cartilage after 10 years is infrequent, but has been described [5]. As individual absorption cannot be predicted, significant over-correction is not advised [86]. One objection against the use of costal cartilage for nasal augmentation is the unnatural stiffness of the reconstructed nose (“frozen nose”). The patients operated on by the author of this review found the stiffness of the nose acceptable in view of an aesthetically pleasing outcome. Fragmentation or crushing of cartilage has been said to lead to absorption of 30-50% of the transplanted volume [73]. Studies failed to confirm this statement [87], [88]. Minced cartilage wrapped in Surgicel has been called ‘Turkish delight’ and was initially described as a safe and long-lasting alternative for nasal augmentation [89], [90]. Subsequent studies, however, showed a rapid resorption of the transplanted cartilage by a marked foreign body reaction upon histology if cartilage fragments were wrapped in alloplastic material. This resorption was not seen when cartilage was wrapped in fascia instead of oxymethylcellulose (Surgicel®) [87], [88].
3.1.4.2 Bone
Bone is not considered to be a suitable transplant tissue for rhinoplasty as it is frequently resorbed or otherwise leads to a stiffness that is more pronounced than after transplantation of costal cartilage. The use of an osteo-cartilaginous rib segment with an osteosynthesis at the nasion has been used with good success for augmentation rhinoplasty in adolescents [91].
3.1.4.3 Fascia, dermis and fat
Fascia, dermis and fat tissue while being inadequate as structural transplants, can be used to correct volume deficits or to camouflage irregularities. Dermis has been used to augment the nasal dorsum [92], [93]. Transplantation of dermis however, carries the risk of cyst or erythema formation if de-epithelialisation is incomplete. Alloderm®, a homologue acellular dermis transplant, has been used for augmentation and camouflage. The volume of the transplant has been said to be stable over a period of two years [86]. Other authors stress that augmentation cannot exceed 3 mm and in about half of the cases, partial or total resorption of the transplant occurs within two years [94], [95]. Temporalis fascia has also been used for this purpose [96], [97], [98]. Handling of this slippery, thin transplant is a major drawback [99]. In facelift patients, SMAS transplants have been used with success [100]. Fat tissue lends itself to augmentation of volume deficits, especially of the nasal sidewall, but a resorption of about 50% of the volume must be anticipated [101].
An impressive plethora of alloplastic materials has been implanted into the nose. It is widely accepted that autologous tissues should be used whenever possible. Nonetheless, the discussion whether the primary use of alloplastic materials in the presence of autologous tissue seems acceptable is ongoing. Initial enthusiasm for new materials was usually followed by disappointment when unacceptable incidences of complications were reported [49], [102]. Up to now, none of the materials used can be considered as ideal [49].
3.1.4.4 Silastic
In Western countries silastic is considered to be not suitable for implantation into the nose. In Asian countries however, large numbers of silastic implants have been used with long-term success [103]. Pre-requisite for successful use of silastic is that the material should lie deep to the skin with a minimum of 1 cm distance to endonasal incisions [5]. The use of silastic for a columellar strut was discruraged [5], even though some authors report good results after placing the silastic through a midline incision in the columella [104], [105]. A preformed, combined dorsal and alar silastic tripod has been abandoned [106].
3.1.4.5 Medpore, Gore-Tex and Proplast
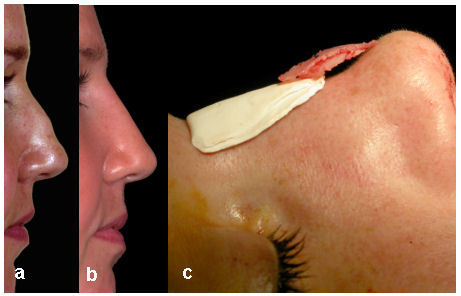
Both Proplast and polytetrafluorethylene (Gore-Tex) have been successfully used as 1 mm or 2 mm foils [107], [108], [109], [110] (Figure 2 (Fig. 2)). The risk of infection and extrusion is said to be considerable and is especially high if the implant bed is dissected close to the sebaceous glands of the nasal skin. High density porous polypropylene (Medpore) is well integrated into the surrounding tissue due to large pores of the material which allow ingrowth of connective tissue [102]. Anecdotal reports indicate that the risk of infection is high if Medpore sheets are implanted into the ala. Resorbable materials, such as lactosorb, have been used as spreader-grafts [111]. Vicryl mesh [112] and Gellatine [113] have also been used. The rationale behind these techniques is the concept that scar tissue will gradually replace the resorbed implant. Clinical evidence from resorption of autologous tissues gives little hope that these resorbable materials can be used with lasting success.
Figure 2. Example of a pseudo-hump, caused by a posttraumatic loss of projection of the cartilaginous dorsum (a). Result 4 months after augmantation of the nasion with two layers of Gore-Tex (thickness: 1 mm) and augmentation of the supratip with a two layers of crushed septal cartilage and apalcement of a columellar strut (b; c).
3.2 Sequence of surgical steps
It is advisable to perform septal corrections prior to corrections of the external nose. Osteotomies on the dorsum (median and paramedian osteotomy) should be performed prior to the lateral osteotomies. There is some controversy whether the nasal dorsum or the nasal tip should be corrected first. The author of this review prefers to correct the nasal dorsum prior to modifications of the nasal tip, because manipulations on the nasal dorsum may cause sutures in the nasal tip to tear. In addition, the argument that the nasal dorsum can be aligned more precisely after shaping of the tip is flawed by inevitable swelling of the tip during the procedure.
3.3 Splints and dressings
The aim of splints and dressings is an immobilisation and protection of mobilised nasal tissues. A splint may therefore also be indicated in case of cartilaginous corrections without osteotomies. In addition, bruising and oedema can be reduced by external splints. Plaster of Paris, thermoplastic splints and aluminium splints (Denver splints) are commonly used. Advantages of plaster of Paris splints are low cost and unparalleled versatility [45].
3.4 Post operative care
Many patients feel insecure in the immediate post-operative period. A positive comment from a bystander (nurse, e.g.) upon removal of the splint can make a big difference in the way the patient will react to the first glance in the mirror. A careful massage of the nasal soft tissues beginning two weeks after surgery and local injections of corticosteroids (Triamcinolone) can speed up the resorption of oedema [72] (see 3.1.3).
4 Specific surgical techniques
4.1 Management of a hump deformity
The most common complaint of rhinoplasty patients in most countries is an excessive projection or convexity of the upper two thirds of the nose in profile. It is interesting that a strong projection of the nasal dorsum developed phyllogenetically in regions of low absolute air humidity and increasing distance from the equator [114]. The length of the nasal airway supposedly increased with the development of a long-distance locomotor anatomy about 1.6 million years ago in order to increase the air conditioning capacity of the nose and thereby improving the endurance in long distance running during hunting [115].
4.1.1 Hump or pseudo-hump?
The term “hump” is not clearly defined, but usually describes displeasing convexities of the nasal profile. These may be caused by a true projection of the upper two thirds of the nose or by excavations of the nasion or loss of projection of the nasal tip. As a consequence, the correction of a hump deformity may be achieved by augmenting the nasion or recreating a correct projection of the nasal tip as an alternative to reduction of the nasal profile. Whether reduction or augmentation suits the individual patient can be readily demonstrated by using computer imaging techniques (see 2.6.1).
4.1.2 Hump resection – how much, where and how
The correction of the nasal profile may be based on morphometric criteria. In clinical practice it appears more suitable to let the patient’s and surgeon’s preference guide the planning. It is important to respect age and gender of the patient [2]. A straight nasal dorsum in profile is generally accepted as being ideal with the profile line being located a few millimetres dorsocaudal of the line between the frontal angle and the nasal tip in women whereas this line in men should be more anterior [2]. It should be remembered that the osseous part of the hump in most patients is much smaller than the cartilaginous part [1], [54]. The author of this review found resection of the hump in one piece starting with the cartilaginous part and continuing the bony resection in a straight, smooth line is the safest way to obtain a straight nasal dorsum without irregularities. The rasp may be used to smooth small bony edges but is not well suited for significant reductions of the bony dorsum. Further lowering of the nasal dorsum by 1 or 2 mm in the bony part after initial hump reduction wit an osteotome carries the risk of fragmentation and asymmetry with visible and palpable irregularities [116]. Five steps for hump reduction were suggested in order to reduce the risk of over- or under-corrections and asymmetries: 1) separation of the triangular cartilages from the septum; 2) step-wise reduction of the cartilaginous septum; 3) reduction of the bony and nasal dorsum; 4) assessment of the resection line by palpation; 5) final shaping and osteotomies or spreader grafts [117]. Preservation of the triangular cartilages is said to reduce the risk of dynamic nasal valve collapse. The functional relevance of this preservation was questioned, however, as iatrogenic nasal valve stenosis after conventional hump reduction including segments of the triangular cartilage seems to be very uncommon from the patient’s perspective [118]. The most common iatrogenic deformity after hump reduction is a so called 'polly-beak’ deformity (Figure 3 (Fig. 3) a). This deformity is caused by an unnatural appearing fullness and convexity of the nasal dorsum cranial to the nasal tip. The most common cause is an insufficient resection of the cartilaginous nasal dorsum. These deformities can then be corrected by further resection. In other cases, the supra-tip fullness is caused by shrinking of the soft tissue and skin cover over the nasal dorsum [5]. Correction of this deformity is very challenging [1]. A prophylactic over-resection of the cartilaginous dorsum cranial to the tip is anatomically incorrect and inefficient to prevent soft tissue contraction [54]. Another challenging problem is the correction of a “Greek” profile caused by a high nasion, as reduction of the bony radix is technically difficult due to the thickness of the bone and shrinking of the concave soft tissue cover over the nasion which conceals ¾’s of the bony resection due to scar contraction [119].
Figure 3. Cartilaginous pollybeak caused by inadequate resection of the cartilaginous hump with overzealous resection of the bony dorsum (a) and inverted-V-deformity after a high lateral osteotomy (b).
4.1.3 Décollement: dissect periosteum and mucosa?
In contrast to surgery of the septum, where dissection should always be subperichondral or subperiostal, most authors advocate a supraperichondral dissection over the dorsum [120] and a subperiostal dissection over the bony dorsum [54], [58], [73]. However, this subperiostal dissection over the convex nasal dorsum will lead to tearing of the periosteum in most cases. The author of this review therefore prefers to dissect in a tissue plane between the periosteum and the nasal equivalent of the superficial musculo-aponeurotic system (SMAS). In most cases it is necessary to extend the soft tissue dissection cranial to the planned osteotomy line and free inserting procerus fibres by sharp dissection. A very extensive décollement of the nasal dorsum was found to support techniques for upward rotation of the nasal tip due to contraction of the skin and soft-tissue cover [54] (Figure 4 (Fig. 4) a+b). Elevation of the mucoperichondrium in the fornix nasi of the endonasal aspect of the nasal hump has been advocated in order to reduced intra-operative bleeding and minimise the risk of endonasal trigeminal neural fibres being trapped in scar tissue of the nasal dorsum [73]. This prophylactic measure may also help to reduce the risk of middle vault collapse [2], [54]. Other authors advocate the elevation of the endonasal mucoperichondrium only in very large humps [1].
Figure 4. Dissection of the skin and soft-tissue cover (décollement) with scissors in a plane between the perichondrium and periosteum and the nasal equivalent of the SMAS (a). Depending on the size of the hump, the décollement is then extended latero-posteriorly using scissors or a N°15 blade for 15 mm – 20 mm (b). The cartilaginous part of the hump is incised first, either under direct vision using an Aufricht retractor, or by palpation (c). Using the widest osteotome that can be inserted (14 mm or 16 mm in most patients) reduces the risk of an uneven resection of the hump (d, e). Rounded ends of the cutting edge reduce the risk of skin perforations. Whenever possible, the cartilaginous and bony part of the hump should be removed in one piece (f). The cut edges of the nasal bone are smoothed with a rasp, preferrably with a tungsten-carbide tip (g). By sliding the wet index finger over the dorsum, irregularities and insufficient resections may be palpated and corrected (h). The nasal bones are mobilised cranially by paramedian oblique osteotomies with a 2 mm or 3 mm osteotome being inserted through the nostril of the opposide side. The osteotome is driven in a latero-cranial direction towards a point that lies approximately 1 cm medial and rostral to the medial canthus (i-k). For the lateral osteotomy, the osteotome is placed on the piriform crest (l; white curve) at the level of the insertion of the inferior turbinate (l: blue marking) by perforating the skin parallel to the piriform crest and then rotating the osteotome by 90°. The osteotome is driven towards the end of the paramedian oblique osteotomy, staying as far lateral as possible. In most patients the osteotome will cleave the bone ahead of the osteotome connecting the two osteotomy lines well before the tip of the osteotome reaches the end of the paramedian oblique osteotomy (m). At this moment the palpating finger will feel that the nasal bone “gives in” and the pitch of sound of the mallet striking the osteotome changes from high to low. In the great majority of patients, the nasal bone is now sufficiantly mobile with the remaining persiosteum acting as a hinge keeping the lateral aspect of the mobilised nasal bone from falling medially. The index finger and thumb palpate the position of the osteotome (n). Bruising and swelling of the eylids can be reduced by moderate pressure over the osteotomy and immediate placement of a cast or splint with digital pressure maintained (o).

4.1.4 Rasp or osteotome?
Several authors propose the use of a rasp for hump resections, claiming that this reduces the risk of an over-correction and that the osteotome therefore should only be used for very large humps [2], [73], [117], [121]. Opponents concede that the use of the rasp is technically simple but point to the fact that the rasp may cause significant soft tissue trauma and should only be used for smoothing bony edges after osteotomy [1], [73]. A modified rasp with a disposable blade [122] as well as a motor driven rasp and rotating drill [16], [17] have not met widespread acceptance. A widely used technique includes an incision of the cartilaginous part of the hump starting at the bony-cartilaginous junction and extending the incision towards the nasal tip (Figure 4 (Fig. 4) c). The osteotome is then placed in the cartilaginous incision on the edge of the bony part of the hump [1], [123]. An alternative is a primary resection of the cartilaginous portion with a separate resection of the bony part [124]. The replantation of a modified en-bloc resected nasal hump onto the nasal dorsum has also been advocated [125]. The author of this review prefers to resect the hump en-bloc using the scalpel and flat osteotome for the cartilaginous and bony part respectively and using the rasp for smoothing bony edges only (Figure 4 (Fig. 4) d+e). The nasal tip is then modified and put into position with techniques described below.
4.1.5 Cranial mobilisation of the nasal bones
Resection of a hump in almost all cases leaves a defect of a bony dorsum called ‘open-roof’. This diastasis should always be closed to prevent visible bony edges, a flattening of the nasal dorsum and, most importantly, to prevent an ingrowth of endonasal trigeminal fibres under the skin of the nasal dorsum. The diastasis of the nasal bones with a hyperaesthesia of the nasal dorsum has been called ‘open roof syndrome’ [73]. In order to medialise the nasal bones, these have to be mobilised laterally and cranially by lateral and median or paramedian osteotomies. The techniques for the latter are subject to controversy [1] as osteotomies in the sagittal plane carry the risk of irregularities at the level of the nasion [126]. The paramedian osteotomy should not be carried out cranial to the intercanthal line in order to avoid a so called ‘rocker deformity’ (lateralisation of the cranial aspect of mobilised bones by medialising the caudal aspect [2]). This complication can be avoided by using oblique paramedian osteotomies with an angle of 15° and 25° between the osteotomy line and the sagittal plane [1], [126]. The author of this review prefers a further angulation of up to 45° (Figure 4 (Fig. 4) i-k). One option to prevent a rocker-deformity is the resection of a bony wedge from the nasion using a Heanley bone forceps [127]. Traditionally, a lateral and paramedian sagittal osteotomy had been connected by a transverse osteotomy which is now considered to be indicated only in patients with a very short nasal bone [1]. Osteotomies should always be carried out from medial to lateral [128].
4.1.6 Lateral mobilisation of the nasal bones
Even though the lateral osteotomy is only a single step in rhinoplasty, it is crucial for its success [2]. The desired course of the osteotomy follows a curved line from the insertion of the inferior turbinate on the piriform aperture to a point medial to the medial canthus [2]. Indications for lateral osteotomies are closing an open roof, narrowing the upper third or correcting a deviation of the bony nose [129], [130]. The “when” and “how” of lateral osteotomies are still a matter of controversy [54], [128]. The lateral osteotomy was initially described by Weir in 1892 [7]. After 1900, a hand-held saw was frequently used. In the 1950’s, motor-driven jigsaws and drills were used for the osteotomy [131]. Recently published modifications of the saw [132], [133] did not meet acceptance. Perforating osteotomies creating a stamp-like pattern of small, bony perforations was initially published in 1971 [134], but was apparently used much earlier in the 1950’s with a 2 mm osteotome [135]. Two basic techniques have gained widespread acceptance; 1) the endonasal continuous technique, preferably using a narrow osteotome and 2) the transcutaneous perforating technique with a 2 mm osteotome [136], [137], [138], [139], [140]. The perforating technique may also be used endonasally [141], [142]. This technique causes an irregular course of the osteotomy and has been found to be less traumatising to the soft tissues compared to the endonasal continuous technique [137], [143], [144], [145]. A decisive advantage of the perforating technique are small periosteal bridges across the osteotomy line allowing the nasal bone to be rotated inward without displacing the nasal bone at the level of the osteotomy [137], [141], [145]. In addition, the endonasal or transcutaneous perforating technique with a 2 mm osteotome was found to cause less post operative bruising and swelling compared to a 4 mm guarded osteotome [146], [147], [148]. Bruising can be further reduced by transcutaneously placing the 2 mm osteotome rostral to the angular blood vessels and displacing these laterally before performing the osteotomy lateral to the skin puncture site [2]. The skin perforations do not leave visible scars, even without skin sutures [2], [149], [150]. Another argument is that the novice will find it easier to create a transcutaneous osteotomy at the desired site with the perforating technique compared to the continuous endonasal technique [150].
4.1.6.1 2, 3 or 4 mm osteotome, guarded or unguarded?
For most authors, micro-osteotomies appear to be the standard of care even though the use of a 7 mm chisel in conjunction with subperiostal tunnels has been advocated recently [73]. Changing the rotation of the chisel (“bevel up” or “bevel down”) facilitates the creation of a curved osteotomy line [73]. The guard on guarded osteotomes was initially designed for endonasal guidance of the instrument [151], but was found to frequently lacerate the nasal mucosa. If placed on the outer surface of the nasal bone, trauma to the soft tissue can be reduced by using a 3 or 2.5 mm osteotome with a flattened guard [152]. The width of the osteotome correlates with the degree of trauma to the endonasal mucosa [136], [141], [153], [154]. The thickness of the bone along the course of the lateral osteotomy does not exceed 2.5 mm in most patients [126], [153]. In theory, lacerations of the periosteum could be avoided by using a 2 mm osteotome for a continuous endonasal osteotomy. However, the straight osteotome cannot follow the curve of the nasal bone and minor lacerations of the periosteum will be inevitable. Some authors have claimed that narrow osteotomes in the hands of inexperienced surgeons may cause significantly more trauma [145], [152]. The author if this review found that continuous endonasal micro-osteotomies can be performed safely by junior surgeons after correct instructions. Excellent results can be obtained with different lateral osteotomy techniques, depending on personal preference [136]. Studies demonstrate that the degree of trauma to soft tissues depends on the technique. This suggests a clinical relevance. It must be stressed however, that an effect on the final outcome has not been demonstrated.
4.1.6.2 High low-high
Another controversy regards the ideal course of a lateral osteotomy. Textbooks and publications suggest that a straight osteotome can follow a curved path through compact bone. Three common variants are described as low-low, low-high and high-low-high [143]. Following a general consensus, the lateral osteotomy should start on the piriform crest at the level of the insertion of the inferior turbinate which is 3-4 mm cranial to the nasal floor and should leave the most caudal aspect of the piriform crest in place (Webster triangle) [144], [152] in order to prevent vestibular stenosis [143], [144]. The lateral osteotomy should be carried out as far lateral as technically feasible to prevent visible or palpable ridges of the nasal sidewall which can create an inverted V-deformity [1], [54], [128], [144] (Figure 3 (Fig. 3) b). In exceptional cases after the resection of very small humps with a minimal diastasis of the nasal bones, a low-to-high osteotomy without paramedian or lateral osteotomies may be achieved without the risk of inverted-V deformity [2]. Subperiosteal tunnels are considered to be unnecessary if 2 mm or 3 mm osteotomes are used [1]. Very thin, tapered osteotomes will create an osteotomy by cleaving the bone ahead of the osteotome with the cleavage following the thickness gradient of the bone [126], [148] (Figure 4 (Fig. 4) m+n). As this thickness gradient roughly follows the piriform crest, the distal part of the osteotomy will be curved.
4.1.6.3 The periosteum as a hinge
Aufricht is said to have spent a large part of his creative energy to create nasal splints that should prevent an excessive medialisation of nasal bones that were completely mobilised using his technique [5], [56]. A complete mobilisation of the nasal bones has been advocated as a prerequisite for a successful reposition more recently [123]. In contrast, most authors agree that the integrity of the periosteum should be preserved as far as possible, either using a perforating technique [13], [145], [146], [148] or by not advancing the osteotome after accomplishing a fracture by cleaving [155], [156]. The remaining periosteum acts as a hinge and allows a rotation of the nasal bone without medial dislocation at the site of the osteotomy. If necessary the periosteal attachment may be disrupted by digital pressure.
4.1.6.4 Finesse
Besides a good outcome, the surgeon who manages to reduce bruising and swelling by choosing minimal traumatising techniques will be considered first choice by potential patients. The roles of vasoconstriction, head position and lowered blood pressure have been discussed earlier. The lateral osteotomy should be placed at the end of the procedure as this is the most soft tissue traumatising part of the operation. This “logic change” of the sequence of surgical steps has been advocated more than 40 years ago [5] and repeated thereafter [123], [128], [140], [148]. In addition the use of a 2-3 mm flat tapered osteotome has been shown to reduce swelling and bruising [154]. Immediate digital compression after a lateral osteotomy followed by rapid splinting with a splint extending over the lateral osteotomy further reduces haematoma formation [1], [116], [147].
4.2 Straightening of the crooked nose
The term “the crooked nose” is not clearly defined and is used to define noses with a longitudinal axis that lies not in the sagittal plane or a dislocation or bending of the tip, middle third or upper third. It is important to remember that a straight nose may appear crooked due to facial asymmetry caused by a non-horizontal inter-ocular axis. In these patients, creating a degree of crookedness may even give the face a more symmetric appearance. The correction of a crooked nose can be extremely challenging, especially if it is caused by an S-shaped bending of the cartilaginous dorsum or if a severe septal pathology is the underlying cause. A correction of the cartilaginous deviation is considered to be more demanding than a correction of the bony dorsum [155], [157].
4.2.1 Straightening of the bony pyramid
Straightening of the bony dorsum may be achieved by augmenting the site with a bone deficit with camouflage grafts in much selected cases. With very few exceptions, however, osteotomies will be necessary. Likewise a straightening of the cartilaginous septum with no residual tension will be necessary. The resection of a dorsal hump facilitates the procedure. If a reduction of the profile is not desirable, mobilisation of the bony pyramid is most effectively achieved through transcutaneous osteotomies. One traditional technique is the resection of a bony wedge parallel to the lateral osteotomy on the side opposed to the deviation (longer nasal bone) [120]. Combining in-fracturing the nasal bone on one side and out-fracturing on the opposite side has also been described as a standard technique [120]. The author of this review prefers transcutaneous osteotomies or continuous endonasal osteotomies combined with a hump reduction.
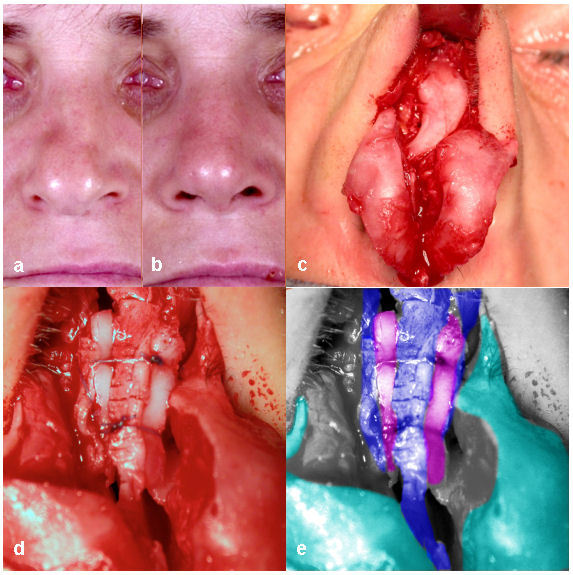
4.2.2 Straightening of the deviated cartilaginous dorsum
In patients with a deviated cartilaginous dorsum, this pathology inevitably extends to the cartilaginous septum. Straightening of the cartilaginous septum is therefore the basis for a correction. Frequently the surgeon will have to resort to a division of the triangular cartilages from the septal cartilage and use straightening manoeuvres such as spreader grafts. Most authors agree that this is most easily accomplished by an external approach. These spreader grafts also widen the middle third of the nose which can be desirable in order to smooth the eyebrow-nasal tip curve. If a widening of the middle third is not desirable, a segment of the perpendicular plate of the septum may be quilted onto the septal cartilage [2], [117], [158] (Figure 5 (Fig. 5)).
Figure 5. Correction of a deviation caused by a S-shaped deformity of a very narrow cartilaginous dorsum. In addition the bulbous drooping tip is deviated to the right (a). The result four months after surgery was obtained by partial thickness incisions on the concave side of the septum after the triangular cartilages were separated (e: blue), spreader grafts (e: magenta) and a resection of the cranial half of the alar cartilages (f: green) and a transdomal suture.
4.2.3 Correction of an asymmetric tip
Asymmetries or deviations of the tip may be caused by a septal deviation, asymmetries of the triangular cartilages or deformities of the alar cartilages. Vertical aspects of asymmetry are frequently caused by the nasal septum or triangular cartilages whereas the horizontal component is usually caused by asymmetries of the alar cartilages [159]. The septoplasty or straightening of the cartilaginous dorsum will solve the problem if the nasal tip itself is symmetric. In case of alar cartilage asymmetry, suture techniques are most versatile and reliable to correct the problem.
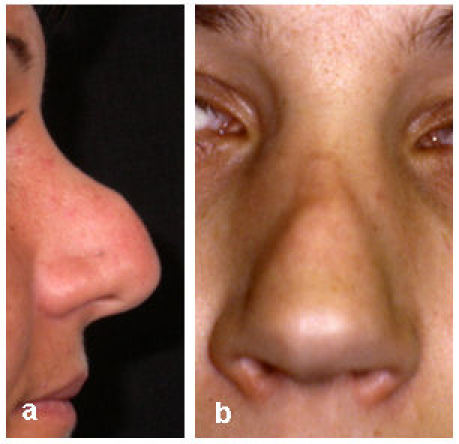
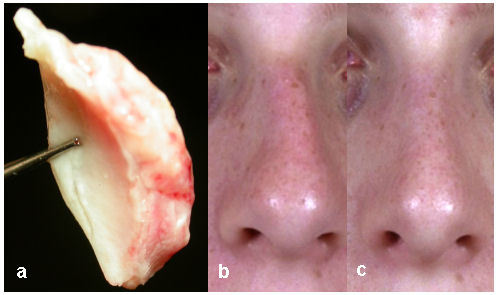
4.3 Augmentation of a saddle nose deformity
A saddle deformity can be caused by a concavity of the whole nasal dorsum or by an isolated loss of projection of the cartilaginous dorsum. These deformities frequently occur with a widening of the bony dorsum after trauma. A loss of septal support with a deprojection of the nasal tip and ensuing pseudo-hump are also one of the characteristic complications of septoplasty. The term ‘saddle-nose’ should not be applied for ethnic concavities of the nasal dorsum. If the anterior segments of the cartilaginous septum and the bony nasal dorsum are intact, a rotation of the septum may be sufficient to straighten the nasal dorsum. An alternative for minor saddling of the cartilaginous dorsum is the augmentation with a septal or conchal cartilage graft (Figure 6 (Fig. 6)). The author of this review prefers to use costal cartilage for the augmentation of severe post-traumatic bony and cartilaginous saddle deformities in conjunctions with osteotomies. The whole length of the concavity should be augmented with a single transplant whenever feasible [160], [161]. It is important to make the dorsal transplant sufficiently wide in the upper third of the dorsum. The author of this review prefers to use a compound L-strut with a slightly mobile connection between the two segments with non-resorbable sutures (Figure 7 (Fig. 7)). This allows both lengthening of the nose and improved nasal tip projection.
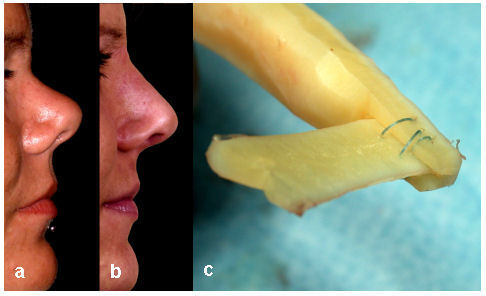
Figure 6. Augmentation of a posttraumatic saddle deformity (a; b) with subtotal loss of the cartilaginous septum using a multilayered quilted septal and conchal cartilage graft (c).
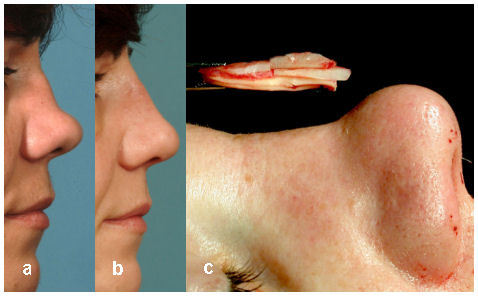
Figure 7. Augmentation and lengthening of a posttraumatic saddle deformity before (a) and three years after augmentation with a costal cartilage L-strut (b). The two components of the L-strut are connected with a loose suture allowing some mobility in the tongue and groove connection upon insertion (c).
4.4 Shaping and positioning of the nasal tip
Correcting a malformed nasal tip is considered to be one of the most challenging aspects of rhinoplasty [49]. 120 years ago changing the shape of the alar cartilages by multiple incisions with a tenotomy knife was described as a “simple operation” [6]. Surgery of the nasal tip has been refined mainly by the introduction of nasal tip transplants and suture techniques in conjunction with the increasing popularity of the external approach [162]. The thickness of the skin soft tissue cover over the alar cartilages is of eminent importance, as correcting a thin alar cartilage under a thick, soft tissue cover will be insufficient to refine the tip regardless of the technique used [54]. In patients with a skin soft tissue cover of more than 3.5 mm the attempt to narrow the tip with transdomal sutures has little chances of success, even if the alar cartilage is strong [59]. Isolated suturing techniques are frequently sufficient for minor corrections of the tip, especially if a rotation of the tip is the main goal of surgery [163].
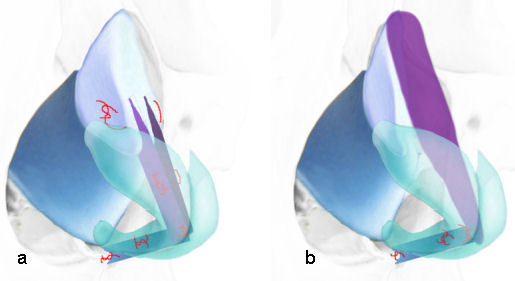
4.4.1 Access to the nasal tip – Is it better to open up?
The controversy regarding the ideal approach to the nasal tip is as old as rhinoplasty itself. Jacques Joseph initially used the external approach before developing the endonasal technique. The external approach was initially described by Rethi in 1934 but was ignored for a long period because of the general acceptance of the endonasal techniques [5], [9]. Even today, this discussion is not free of emotions with proponents of the endonasal techniques considering themselves as mastering the more elegant techniques and proponents of the external approach emphasizing improved teaching and versatility. Severe deformities of the cartilaginous dorsum or nasal tip such as cleft deformities are generally considered to be best operated on through the external approach [69]. One matter of debate is whether it is justified to use the external approach even for less complex problems [164]. A recent survey among US facial plastic surgeons revealed that one quarter of the surgeons almost exclusively use the external approach and more than half of the surgeons use the external approach in more than 50% of their rhinoplasty cases [165]. It is openly discussed that many of the younger rhinoplasty surgeons use the external approach even for minor corrections, because they are not trained in endonasal techniques any more. Some say that this change is justified by a better visualisation in training situations, easier placing of transplants and sutures which is of advantage especially for the inexperienced surgeon and surgeons from other disciplines [2], [159], [166], [167], [168], [169], [170]. It is generally accepted that the columellar scar is a negligible issue if the incision is closed meticulously [171], [172]. On the other hand, it is also generally accepted that the external approach causes a longer period of oedema and hypaesthesia of the tip and prolongs the procedure itself [173], [174]. Morphometric analysis on fresh cadavers demonstrated that the external approach caused a larger loss of nasal tip projection after various modifications of the alar cartilage [151]. Therefore, the external approach should be reserved for selected cases based on the limitations of the endonasal approach [57], [175], [176], [177]. An extension of the infra-cartilaginous incision to the columella has been described as an alternative to the external approach for extensive resections of fibro-adipose tissue from the tip and alar cartilage modifications [178]. Jack Sheen commented 10 years ago “I simply do not agree with the advocates of the open approach who argue that only a few exceptional surgeons can truly master the endonasal approach”, adding that every surgeon should aim for the highest level of surgical perfection [179]. This implies that the more challenging endonasal techniques should be learned [155]. The external approach gives an excellent impression of the three-dimensional anatomy of the nasal tip. This insight should then be used for endonasal procedrues [5]. The most conservative and tissue sparing techniques are the trans-cartilaginous and the retrograde approaches to the nasal tip as these approaches preserve the integrity of the caudal ala. The drawback of the transcartilaginous approach is that it is difficult to place the incisions exactly opposing and symmetrical [2]. The luxation or delivery technique using an infra-cartilaginous and inter-cartilaginous incision is in many cases a good alternative to the external approach [2]. A slightly more challenging but elegant variation is the approach via an isolated infra-cartilaginous incision [54], [81]. This technique is preferred by the author of this review (Figure 8 (Fig. 8)). A great majority of surgical manoeuvres to the nasal tip can be accomplished through this approach. Severe tip asymmetries, scarring or loss of tip support can be limiting factors. The isolated infracartilaginous approach can be extended by an additional intercartilaginous incision (delivery technique) or by extending the incision along and across the columella (external approach) [164].
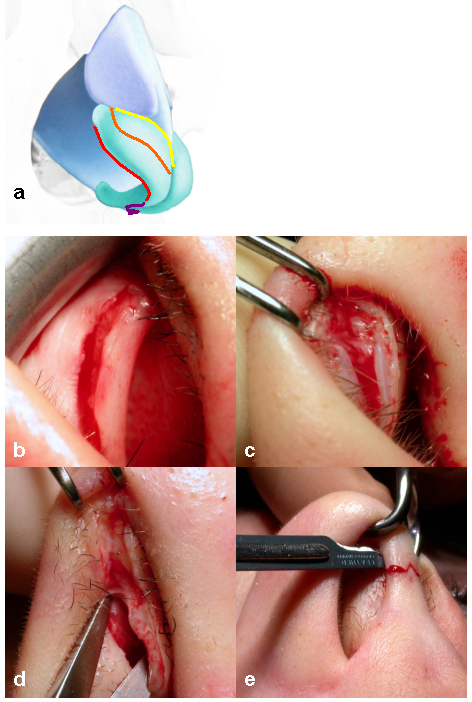
Figure 8. Common rhinoplasty approaches (a): intercartilaginous (yellow), transcartilaginous (orange), infracartilaginous (red), external (purple). The intercartilaginous incision is located next to the caudal edge of the triangular cartilage (b). In the transcartilaginous approach, the dissection is facilitated by incising the vestibular skin on the endonasal surface of the alar cartilage first and dissecting the vestibular skin before the cartilage is transected (c). The infracartilaginous approach follows the caudal border of the intermediate and lateral crus (d). For the external approach, the incision follows the caudal border of the medial crus approximately 2 mm cranial to the caudal border of the columella (e).
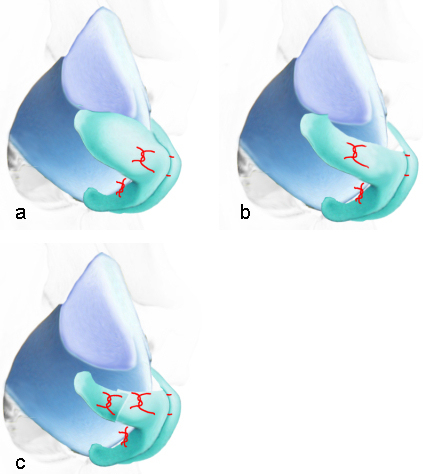
4.4.2 The tripod model of the nasal tip
A concept that helps to understand the dynamics of tip modifying techniques is the tripod concept introduced in 1969 by J. Anderson [180] (Figure 9 (Fig. 9)). One leg of the tripod is the two medial crura in the columella with the other two legs being the lateral crura of the alar cartilage. By shortening or lengthening individual legs of the tripod, both projection and rotation of the nasal tip can be modified. A significant limitation of this concept is that the three legs are mobile and compressible [2]. The nasal tip is kept in position by the cartilaginous septum, the length and rotation of the lateral and medial crura of the alar cartilage, by fibrous attachments between the alar cartilage and triangular cartilage and by fibrous connections between the alar cartilage domes and the skin of the nasal tip [2]. These retaining structures should be reconstructed if they are transected through the procedure. One study described a loss of nasal tip projection by ¼ if the connective fibres between the alar cartilage domes were transected whereas a transdomal mattress suture or a columella strut increased the projection by ⅓ and ½ respectively [181].
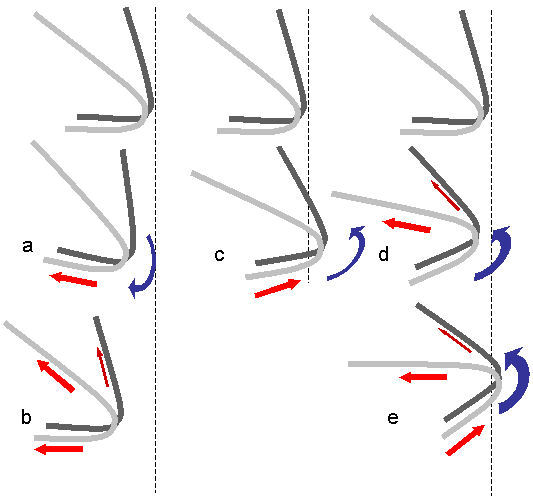
Figure 9. Tripod modell of the nasal tip according to Anderson. The lateral crura (light grey and dark grey) represent two legs of the tripod, whereas the two parallel medial crura represent the third leg. The projection and rotation of the tip may be altered by lengthening or shortening of individual legs: downward rotation and retroposition by relocating the columella posteriorly (a). Additional shortening of the lateral crura increases the deprojection of the tip and counterbalances the downward rotation (b). Increased projection and rotation by repositioning the columella anteriorly (c). Additional shortening of the lateral crura further rotates the tip and counterbalances the icrease in tip projection (d). Maximum rotation is achieved by a rostral repositioning of the columella and shortening of the lateral crura (e).
4.4.3 Suture techniques
Suture techniques have had a profound impact on rhinoplasty technique mainly during the past decade [81], [170], [182], [183], [184], [185], [186]. The wide acceptance of these techniques that have been introduced many decades ago may be a consequence of unsatisfactory results and secondary deformities after aggressive cartilage resecting techniques and the high incidence of revision procedures after cartilage transplants to the nasal tip [187]. A fundamental advantage of suture techniques is that the integrity of the cartilage is respected or reconstructed and cartilage may be transposed or curvatures modified [185]. Sutures have also been successfully applied to correct deviations of the anterior cartilaginous septum [188]. In addition, the effect of sutures is fully reversible during surgery and partially reversible after wound healing [189]. In order to obtain a permanent result, the use of non-resorbable monofile sutures (4.0 or 5.0 nylon e.g.) has been advocated [189]. Nylon sutures have been shown to cause a more pronounced foreign body reaction in the rabbit ear compared to polydioxanon sutures [190] but, this reaction has not been demonstrated for the human nose. Horizontal spanning sutures of the lateral crus to correct concavities or convexities have been described as being universal, simple and efficient [189]. In contrast to scarification, the suture techniques strengthen rather than weaken the lateral crus [191]. Another application of spanning sutures is the lateralisation of the triangular cartilage by a suture than runs across the cartilaginous dorsum (flaring suture) [192], [193], [194], [195]. A recently published simple technique rotates the nasal tip by placing a suspension suture between the osteo-cartilaginous junction of the dorsum and the cranial alar cartilages [196]. This technique has raised concerns about long term success.
4.4.4 Alar cartilage: preserve a complete strip?
More than 50 years ago Goldmann described a technique of a vertical transection of the alar cartilage dome and a narrowing of the tip by approximating the medial cut ends with a suture [197]. In the hands of most surgeons, this technique has been replaced by suture techniques respecting the integrity of the alar cartilage (complete strip procedure) because the Goldmann technique frequently led to unnatural appearing excessive narrowing of the tip especially in thin skinned patients [1], [198]. If the alar cartilage is vertically transected, the integrity should be reconstructed with a suture, preferably with overlapping of the cut edges [1] (Figure 10 (Fig. 10)). The lateral crus can be shortened effectively and predictably by a vertical transection and overlapping of the cut edges (lateral crural overlay) which leads to a predictable and durable rotation of the nasal tip [1], [199] (Figure 11 (Fig. 11), Figure 12 (Fig. 12)).
Figure 10. Narrowing of a boxy tip without changing projection and rotation. As an alternative to the techniques detailed in Figure 12, the dome may be dissected (a), transected (b) and reconstructed after resection of a segment of the intermediate crus (c; d). Preoperative (d) and 5 months postoperative (e).
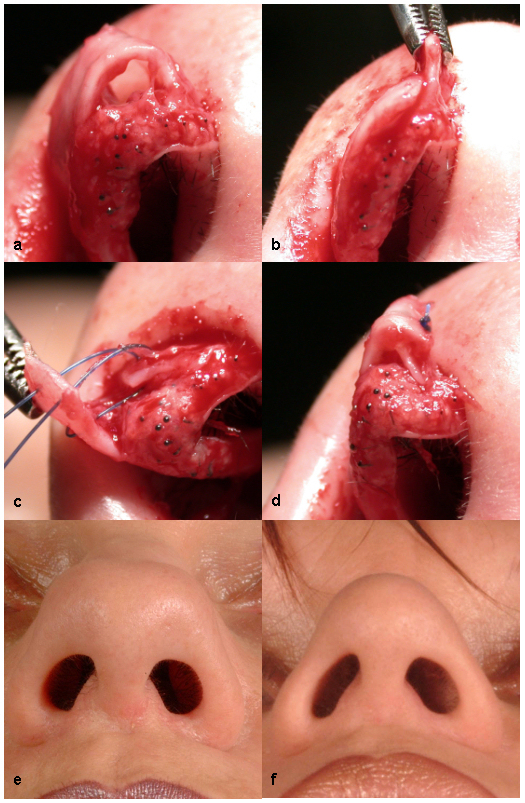
Figure 11. The lateral crus is shortened by transection and a mattress suture of the overlapping ends (lateral crural overlay).
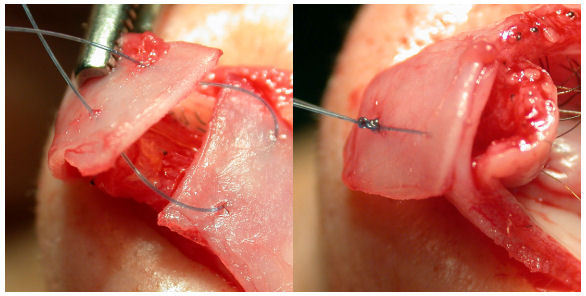
Figure 12. A transdomal suture narrows the tip and slightly augments the projection and rotation of the tip (a). Placing the mattress suture in a more lateral position shortens the lateral crus (lateral crural steal; b). Volume reduction of the tip and rotation are further improved by resecting the cranial part of the lateral crus. For a maximum rotation these manouevres are combined (c).
4.4.5 Transplants for the columella, nasal tip and ala
A columellar strut is a well recognised standard technique to improve nasal tip projection and protection. It may be placed through an endonasal approach via a caudal septal incision [200]. If pronounced improvement of tip projection is desired, an external approach facilitates the fixation of an alar strut on the nasal spine and also allows a more efficient augmentation by fixation of the alar cartilage domes to the alar strut. In severe alar cartilage asymmetries as in cleft lip deformities, the columellar strut effectively splints the repositioned alar cartilage. Due to its rigidity and straight shape, septal cartilage should be preferred if it is available. Slight alar retractions may be corrected by an alar rim graft placed parallel to the alar rim, caudal to the alar cartilage [201]. In patients with a thick, soft tissue cover over the alar cartilages, suture techniques are frequently insufficient to narrow the tip [59]. In these cases, a heart- or shield-shaped cartilage graft may be sutured onto the intermediate crura to accentuate the nasal tip. Care should be taken to round the edges of the transplant in order to avoid visible edges after long term thinning of the nasal tip skin. Even though absorption appears to be more pronounced in crushed cartilage transplants, superior long term results compared to shield grafts have been seen when transplants have been crushed before being placed over the alar cartilage domes [202].
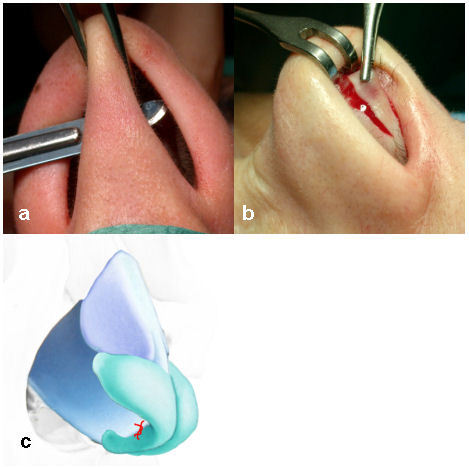
4.4.6 Rotation of the hanging tip
Shortening of a long nose with or without rotation of the hanging nasal tip is frequently requested. This may be achieved by dissecting a triangle of the caudal membranous and cartilaginous septum in conjunction with further tip rotating manoeuvres (Figure 13 (Fig. 13)). An isolated resection of the caudal septum carries the risk of retracting the columella without sufficient rotation which may accentuate the drooping of the tip [1], [203]. An efficient technique to rotate the tip is a shortening of the lateral crura by transection and overlay of the cut edges secured by a mattress suture (lateral crural overlay) [199], [203], [204] (Figure 11 (Fig. 11), Figure 12 (Fig. 12)). A minor rotation is achieved by a laterally placed mattress suture (lateral crural steal suture) [199]. If the length of the lateral crus has been adequately reduced, the resulting defect from the crural septal excision should be closed without tension. Additional projection and rotation may be achieved by anchoring sutures between the medial crura and the caudal septum [1], [83], [205]. In selected cases, a resection of the caudal aspect of the triangular cartilage may be justified. This should be indicated with caution, however, as excessive resection may cause an undesirable narrowing of the middle third [1]. It should be noted that the resection of a cranial strip of the lateral crus will reduce the volume of the cranial half of the nasal tip but will only lead to a minimal upward rotation [1] and may even cause a downward rotation due to loss of the tip supporting fibres between the lateral crus and the triangular cartilage. An illusion of rotation may be created by resection of the caudal aspect of the intermediate crus and medial crus and opening of the nasolabial angle with pre-maxillary transplants (plumper grafts) or by reducing the projection of the nasal dorsum below the level of the nasal tip [1]. Upward rotation may also be achieved by a technique that mainly aims at the correction of a functional vestibular stenosis (alar collapse). This technique is based on a transposition of a medially based skin cartilage flap of the cranial edge of the alar cartilage to me midline after transecting the triangular cartilage from the septal cartilage [206], [207].
Figure 13. Rotation of the tip: Transfixion (a) and excision of a skin and cartilage wedge of the caudal septum (b). In most patients it will be necessary to shorten the lateral crura for a marked rotation (see Figures 11, 12). The columella may be anchored to the caudal cartilaginous septum in the desired position with an anchoring suture.
4.4.7 Lengthening of the nose
In contrast to shortening the nose and upward rotation of the tip, lengthening and downward rotation is technically more challenging [208]. An illusion of lengthening may be achieved by placing transplants on the caudal aspect of the alar domes [209], [210], or by placing a transplant caudal to the medial crura [211]. The nose may be lengthened by quilting a septal extension graft on to the septum and creating a new septal angle in a more caudal position [2], [208]. An illusion of a lengthening may also be achieved by resection of the caudal edge of the cartilaginous septum close to the nasal spine by reducing the nasal labial angle [208]. Bilateral extended spreader grafts can be used an alternative to the caudal septal extension graft [2], [212] (Figure 14 a (Fig. 14)). In post-traumatic cases, a lengthening of the nose is part of the augmentation procedure with an L-shaped rib-graft (Figure 7 (Fig. 7), Figure 14 b (Fig. 14)).
Figure 14. Lengthening of the nose with a L-shaped reconstruction of the septal angle based on caudally extended spreader grafts (purple), a columellar strut and fixation of the alar cartilages to the reconstructed septal angle (a). In posttraumatic deformities the short nose is combined with a saddle deformity. These deformities can be reconstructed with a L-shaped costal cartilage graft (b).
4.4.8 Volume reduction and narrowing of the tip
Techniques that respect the continuity of the alar cartilage (continuous strip) are considered to be safer compared to transecting techniques. Breaking the tension of the dome by partial cuts on the convex surface of the dome has been advocated as a less aggressive technique compared to vertical transection [54], [57]. More recent publications focus on the use of sutures emphasizing the reliability, efficiency and reversibility [2], [170], [182]. An algorithm for narrowing of the tip with sutures advocates a transdomal suture to narrow the dome, an interdomal suture to recreate symmetry, mechanical resilience and narrowing of the tip and horizontal mattress sutures of the lateral crus in order to correct concavities or convexities. In most cases it is advisable to add an anchor suture between the columella and caudal septum to further modify the rotation of the tip or to prevent an unwanted de-rotation of the tip after surgery [170]. A bulbous tip may also be caused by a cranial rotation of the lateral crus [213]. It may be necessary to resect fibro-adipose tissue between the alar cartilage domes in very wide nasal tips (Figure 15 (Fig. 15)). A reduction of the volume of the cranial half of the nasal tip may be achieved by an isolated bilateral transcartilaginous incision with resection of a layer of fibroid tissue on the resected segment of cartilage [2] (Figure 16 (Fig. 16)).
Figure 15. Resection of fibroadipose tissue between the alar cartilage domes and intermediate crura.
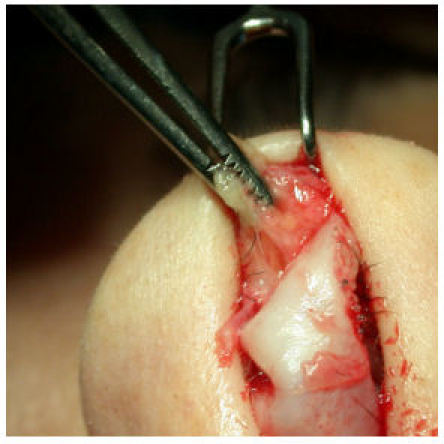
Figure 16. Volume reduction of the cranial half of the tip by resecting the the medio-cranial half of the lateral crus with adherent fibroadipose tissue (a). Preoperative (b) and 6 months postperative (c).
4.4.9 Reduction of nasal tip projection
The nasal tip may be set back by reducing the length of the lateral crus and a retroposition of the columella as described earlier [199]. By shortening all three legs of the tripod, the rotation of the tip is respected (Figure 9 (Fig. 9), Figure 12 (Fig. 12), Figure 17 (Fig. 17)). The technique may be modified by resecting a segment of the columella which additionally reduces the circumference of the nostril [156]. Another alternative is the resection and reconstruction of the alar cartilage domes (Figure 10 (Fig. 10)).
Figure 17. Preoperative profile (a) and postoperative outcome (b): rotation and narrowing and retroposition of the tip using the technique described in Figure 12 c.

4.4.10 Increasing tip projection
Tip projection may be improved by a transfixion incision and anchoring the columella to the caudal septum in a further rostral position. This manoeuvre induces some upward rotation of the tip. Interdomal sutures and the lateral crural steal suture help to accentuate nasal tip projection in combination with an upward rotation [199] (Figure 9 (Fig. 9), Figure 13 (Fig. 13)). If an insufficient projection of the tip is caused by a loss of septal support, the septum should be reconstructed or the support should be recreated with a columellar strut with fixation of the medial crura and domes to the strut [2]. The tip may be further accentuated by applying a tip shield or overlying graft as described earlier [163].
5 Future perspective
5.1 Evidence
With few exceptions, the cited references fulfil the requirements of evidence level four or five [214]. This seems of little surprise as most surgical techniques do not lend themselves to randomized controlled trials for ethical reasons. Where a randomisation is considered to be acceptable, a study may not be justified due to limited clinical relevance of the topic. Few studies match the requirements of the evidence level 1b or 1c [74], [78], [126], [147]. These studies show for instance, that the difference between perforating or continuous osteotomies is not significant [147], that corticosteroids reduce post operative swelling only during the first 2 post-operative days without effect on the following reconvalescence [182], that a single shot of an antibiotic is not inferior to longer antibiotic prophylaxis [175], or that parasagittal osteotomies compared to fifteen degree osteotomies have a higher risk of rocker deformities in the nasal root in cadaver specimen [126]. That patients benefit psychologically from a rhinoplasty [22], [36] was demonstrated on evidence level 3b and 4. Some surgical recommendations are based on very large case series [172], [89], may however be confronted with conflicting results from other case series [87], [88]. Nevertheless, the lack of evidence in rhinoplasty surgical techniques is striking and efforts should be made to conduct controlled studies.
5.2 Outcome studies
An important aspect of outcome studies in aesthetic surgery is the fact that patient satisfaction rather than objective measures or complications are key criteria for surgical success. None of the proposed measuring methods have been accepted as a general standard. Generally accepted measuring instruments would allow a comparison of surgical techniques, a quantification of the positive effect of surgery and may even help to define a profile of the psychological high risk patient [215]. For the assessment of body image, the multi-dimensional body states relations questionnaire (MBSRQ) has been suggested. The facial appearance sorting test (FAST) may be of interest for the assessment of rhinoplasty outcome. The effect of subjective appearance on quality of life can be assessed with the Derriford Ford Scale (DAS-59). In addition, individual benefit should be assessed with a quality of life instrument like the health utilities index (HUI) or the Euroqol (Eq-5D) [215]. Patients’ perspective should be incorporated in questions regarding indication and techniques of rhinoplasty.
Acknowledgements
I thank Lyn Martin, Department of Otolaryngology, Head and Neck Surgery, The Queen Elizabeth Hospital, Adelaide, Australia for helping with editing this manuscript.
References
- 1.Tardy ME., Jr . Rhinoplasty: The art and the science. Philadelphia, Pennsylvania: W.B. Saunders Company; 1997. [Google Scholar]
- 2.Gunter JP, Rohrich RJ, Adams WP, editors . Dallas rhinoplasty: nasal surgery by the masters. St. Louis: Quality Medical Publishing; 2002. [Google Scholar]
- 3.Sheen JH. Rhinoplasty: personal evolution and milestones. Plast Reconstr Surg. 2000;105:1820–1852. doi: 10.1097/00006534-200004050-00033. [DOI] [PubMed] [Google Scholar]
- 4.Stucker FJ. Rhinoplasty from the Goldman/Cottle schools to the present: a survey of 7447 personal cases. Am J Rhinol. 2003;17(1):23–26. [PubMed] [Google Scholar]
- 5.Millard DR. A rhinoplasty tetralogy: corrective, secondary, congenital, reconstructive. Little, Brown and Company (Inc.); 1996. [Google Scholar]
- 6.Roe JO. The Deformity Termed "Pug Nose" and its correction with a simple operation. Plast Reconstr Surg. 1970;45(1):78–83. [PubMed] [Google Scholar]
- 7.Hauben DJ. Die Geschichte der Rhinoplastik. Laryngo Rhinol Otol. 1983;62:53–54. [PubMed] [Google Scholar]
- 8.Rubin FF. Reconstruction of the bony nasal pyramid. Three new instruments. Arch Otolaryngol. 1968;88(3):279–282. doi: 10.1001/archotol.1968.00770010281014. [DOI] [PubMed] [Google Scholar]
- 9.Safian J. Instruments for rhinoplasty. Plast Reconstr Surg. 1970;45(3):288–289. doi: 10.1097/00006534-197003000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Wilkie TF. A nasal saw of modified design. Br J Plast Surg. 1967;20(2):220–221. doi: 10.1016/s0007-1226(67)80040-7. [DOI] [PubMed] [Google Scholar]
- 11.Peet E. An improved rasp for corrective rhinoplasty. Br J Plast Surg. 1968;21(2):215. doi: 10.1016/s0007-1226(68)80016-5. [DOI] [PubMed] [Google Scholar]
- 12.McGregor IA. A nasal osteotome. Br J Plast Surg. 1967;20(2):222. doi: 10.1016/s0007-1226(67)80041-9. [DOI] [PubMed] [Google Scholar]
- 13.Drever JM. A guided osteotome for the resection of the osteocartilaginous nasal hump. Plast Reconstr Surg. 1978;62(4):611–612. doi: 10.1097/00006534-197810000-00029. [DOI] [PubMed] [Google Scholar]
- 14.Georgi W. The double chisel - a new nasal osteotome. HNO. 1977;25(11):401–403. [PubMed] [Google Scholar]
- 15.Goodman WS. The rotating burr in rhinoplasty. Arch Otolaryngol. 1981;107(7):436–438. doi: 10.1001/archotol.1981.00790430038010. [DOI] [PubMed] [Google Scholar]
- 16.Becker DG. The powered rasp: advanced instrumentation for rhinoplasty. Arch Facial Plast Surg. 2002;4(4):267–268. doi: 10.1001/archfaci.4.4.267. [DOI] [PubMed] [Google Scholar]
- 17.Becker DG, Park SS, Toriumi DM. Powered instrumentation for rhinoplasty and septoplasty. Otolaryngol Clin North Am. 1999;32(4):683–693. doi: 10.1016/s0030-6665(05)70164-x. [DOI] [PubMed] [Google Scholar]
- 18.Berghaus A. New instruments for rhinoplasty: operating mirror and alar guiding set. Plast Reconstr Surg. 2006;117(7):2224–2225. doi: 10.1097/01.prs.0000218719.51674.d6. [DOI] [PubMed] [Google Scholar]
- 19.American Academy of Facial Plastic and Reconstructive Surgery. 2004 Membership Survey: Trends in Facial Plastic Surgery. March, 2005. [Google Scholar]
- 20.Hay GG, Heather BB. Changes in psychometric test results following cosmetic nasal operations. Br J Psychiatry. 1973;122:89–90. doi: 10.1192/bjp.122.1.89. [DOI] [PubMed] [Google Scholar]
- 21.Ercolani M, Baldaro B, Rossi N, Trombini G. Five-year follow-up of cosmetic rhinoplasty. J Psychosom Res. 1999;47:283–286. doi: 10.1016/s0022-3999(99)00041-0. [DOI] [PubMed] [Google Scholar]
- 22.Dinis PB, Dinis M, Gomes A. Psychological consequences of nasal aesthetic and functional surgery: a controlled prospective study in an ENT setting. Rhinology. 1998;36:32–36. [PubMed] [Google Scholar]
- 23.Rankin M, Borah GL, Perry AW, Wey PD. Quality-of-life outcomes after cosmetic surgery. Plast Reconstr Surg. 1998;102:2139–2145. doi: 10.1097/00006534-199811000-00053. [DOI] [PubMed] [Google Scholar]
- 24.Haraldsson P. Psychological impact of cosmetic rhinoplasty. Aesthetic Plast Surg. 1999;23:170–175. doi: 10.1007/s002669900264. [DOI] [PubMed] [Google Scholar]
- 25.Shulman J, Westreich M. Rhinoplasty update: preoperative evaluation of 4,040 cases. Aesthetic Plast Surg. 1983;7:227–232. doi: 10.1007/BF01570665. [DOI] [PubMed] [Google Scholar]
- 26.Shulman O, Westreich M, Shulman J. Motivation for rhinoplasty: changes in 5970 cases, in three groups, 1964 to 1997. Aesthetic Plast Surg. 1998;22:420–424. doi: 10.1007/s002669900227. [DOI] [PubMed] [Google Scholar]
- 27.Napoleon A, Lewis CM. Psychological considerations in lipoplasty: The problematic or "special care" patient. Ann Plast Surg. 1989;23:430–432. doi: 10.1097/00000637-198911000-00009. [DOI] [PubMed] [Google Scholar]
- 28.Edgerton MT, Langmen MW. Psychiatric considerations. In: Courtiss EH, editor. Male aesthetic surgery. St Louis: Mosby; 1982. [Google Scholar]
- 29.Goin JM, Goin MK. Psychological understanding and management of the plastic surgery patient. In: Georgiade NG, Georgiade GS, Riefkohl R, Barwick WJ, editors. Essentials of Plastic, Maxillofacial and reconstructive surgery. Baltimore: Williams and Wilkins; 1987. [Google Scholar]
- 30.Marcus P. Psychological aspects of cosmetic rhinoplasty. Br J Plast Surg. 1984;37:313–318. doi: 10.1016/0007-1226(84)90073-0. [DOI] [PubMed] [Google Scholar]
- 31.Robin AA, Copas JB, Jack AB, Kaerser AC, Thomas PJ. Reshaping the psyche: The concurrent improvement in appearance and mental state after rhinoplasty. Br J Psychiatry. 1988;152:539–543. doi: 10.1192/bjp.152.4.539. [DOI] [PubMed] [Google Scholar]
- 32.Sheard C, Jones NS, Quraishi MS, Herbert M. A prospective study of the psychological effects of rhinoplasty. Clin Otolaryngol. 1996;21:232–236. doi: 10.1111/j.1365-2273.1996.tb01732.x. [DOI] [PubMed] [Google Scholar]
- 33.Klassen A, Jenkinson C, Fitzpatrick R, Goodacre T. Patients' health related quality of life before and after aesthetic surgery. Br J Plast Surg. 1996;49:433–438. doi: 10.1016/s0007-1226(96)90025-9. [DOI] [PubMed] [Google Scholar]
- 34.Cole RP, Shakespeare V, Shakespeare P, Hobby JA. Measuring outcome in low-priority plastic surgery patients using Quality of Life indices. Br J Plast Surg. 1994;47:117–121. doi: 10.1016/0007-1226(94)90170-8. [DOI] [PubMed] [Google Scholar]
- 35.Pruzinski T, Edgerton MT. Body image change in cosmetic plastic surgery. In: Cash TF, Pruzinsky T, editors. Body images: development, deviance and change. New York: Guilford; 1990. [Google Scholar]
- 36.McKiernan DC, Banfield G, Kumar R, Hinton AE. Patient benefit from functional and cosmetic rhinoplasty. Clin Otolaryngol. 2001;26:50–52. doi: 10.1046/j.1365-2273.2001.00427.x. [DOI] [PubMed] [Google Scholar]
- 37.Sarwer DB, Pertschuk MJ, Wadden TA, Whitaker LA. Psychological investigations in cosmetic surgery: a look back and a look ahead. Plast Reconstr Surg. 1998;101:1136–1142. doi: 10.1097/00006534-199804040-00040. [DOI] [PubMed] [Google Scholar]
- 38.Hill G, Silver AG. Psychodynamic and motivations for plastic surgery. Psychol Med. 1950;12(6):345–355. doi: 10.1097/00006842-195011000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Linn L, Goldman IB. Psychiatric observations concerning rhinoplasty. Psychol Med. 1949;11:307. doi: 10.1097/00006842-194909000-00010. [DOI] [PubMed] [Google Scholar]
- 40.Meyer E, Jacobson WE, Edgerton MT, Canter A. Motivational patterns in patients seeking elective plastic surgery. Psychol Med. 1960;22:193. [Google Scholar]
- 41.Hay GG. Psychiatric aspects of cosmetic nasal operations. Br J Psychiatry. 1970;116:85. doi: 10.1192/bjp.116.530.85. [DOI] [PubMed] [Google Scholar]
- 42.Wright MR, Wright WK. A psychological study of patients undergoing cosmetic surgery. Arch Otolaryngol. 1975;101:145. doi: 10.1001/archotol.1975.00780320003001. [DOI] [PubMed] [Google Scholar]
- 43.Goin MK, Rees TD. A prospective study of patients' psychological reactions to rhinoplasty. Ann Plast Surg. 1991;27:210. doi: 10.1097/00000637-199109000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Meerloo J. The fate of one's face. Psychiatric quarterly. 1956;30:31. doi: 10.1007/BF01564325. [DOI] [PubMed] [Google Scholar]
- 45.Roubichek J. Zur Psychopathologie des kosmetischen Fehlers. Aesthet Med. 1960;9:21. [Google Scholar]
- 46.Edgerton MT, Jacobson WE, Meyer E. Surgical-psychiatric study of patients seeking plastic (cosmetic) surgery. Br J Plast Surg. 1960;13:136. doi: 10.1016/s0007-1226(60)80029-x. [DOI] [PubMed] [Google Scholar]
- 47.Edgerton MT, Langman MW, Pruzinsky T. Plastic surgery and psychotherapy in the treatment of 100 psychologically disturbed patients. Plast Reconstr Surg. 1991;88:594. doi: 10.1097/00006534-199110000-00006. [DOI] [PubMed] [Google Scholar]
- 48.Crerand CE, Phillips KA, Menard W, Fay C. Nonpsychiatric Medical Treatment of Body Dysmorphic Disorder. Psychosomatics. 2005;46(6):549–555. doi: 10.1176/appi.psy.46.6.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Behrbohm H, Tardy ME Jr, editors. Funktionell-ästhetische Chirurgie der Nase. Septorhinoplastik. Stuttgart, New York: Thieme; 2004. [Google Scholar]
- 50.Slator R, Harris DL. Are rhinoplasty patients potentially mad? Br J Plast Surg. 1992;45:301. doi: 10.1016/0007-1226(92)90058-6. [DOI] [PubMed] [Google Scholar]
- 51.Macgregor FC. Social, psychological and cultural dimensions of cosmetic and reconstructive plastic surgery. Aesthetic Plast Surg. 1989;13:1. doi: 10.1007/BF01570318. [DOI] [PubMed] [Google Scholar]
- 52.Gorney M, Martello J. Patient selection criteria. Medical-legal issues in plastic surgery. Clin plast surg. 1999;26:37. [PubMed] [Google Scholar]
- 53.Rohrich RI. Streamlining cosmetic surgery patient selection - just say no. Plast Reconstr Surg. 1999;104:220. [PubMed] [Google Scholar]
- 54.Sheen JH, Sheen AP, editors. Aesthetic Rhinoplasty. 2nd ed. St. Louis: Quality Medical Publishing; 1998. [Google Scholar]
- 55.Powell N, Humphreys B. Proportions of the aesthetic face. New York, NY: Thieme Stratton inc.; 1984. [Google Scholar]
- 56.Becker OJ. Rhinoplasty: Cultural, esthetic and psychological aspects. Chicago Med. 1961;64:15. [PubMed] [Google Scholar]
- 57.Berghaus A. Die Chirurgie der Nasenspitze. Laryngo Rhino Otol. 1997;76:680–681. doi: 10.1055/s-2007-997506. [DOI] [PubMed] [Google Scholar]
- 58.Nolst Trenité GJ. Rhinoplasty; A practical guide to functional and aesthetic surgery of the nose. The Hague, Netherlands: Kugler Publications; 2005. [Google Scholar]
- 59.Tasman AJ, Helbig M. Sonography of nasal tip anatomy and surgical tip refinement. Plast Reconstr Surg. 2000;105(7):2573–2579. doi: 10.1097/00006534-200006000-00045. [DOI] [PubMed] [Google Scholar]
- 60.Briner HR, Simmen D, Jones N. Impaired sense of smell in patients with nasal surgery. Clin Otolaryngol Allied Sci. 2003;28(5):417–419. doi: 10.1046/j.1365-2273.2003.00735.x. [DOI] [PubMed] [Google Scholar]
- 61.Kobal G, Hummel T, Sekinger B, Barz S, Roscher S, Wolf S. "Sniffin' sticks": screening of olfactory performance. Rhinology. 1996;34(4):222–226. [PubMed] [Google Scholar]
- 62.Simmen D, Briner HR, Hess K. Screeningtest des Geruchsinnes mit Riechdisketten. Laryngo Rhino Otol. 1999;78:125–130. doi: 10.1055/s-2007-996844. [DOI] [PubMed] [Google Scholar]
- 63.Galdino GM, DaSilva AD, Gunter JP. Digital photography for rhinoplasty. Plast Reconstr Surg. 2002;109(4):1421–1434. doi: 10.1097/00006534-200204010-00035. [DOI] [PubMed] [Google Scholar]
- 64.Hirche W. Arztrecht kompakt. Juristischer Ratgeber für die Arztpraxis. München: MD-Verlag; 1994. [Google Scholar]
- 65.Gruber RP. Computer imaging and surgical reality in aesthetic rhinoplasty. Plast Reconstr Surg. 2005;116(3):922–923. doi: 10.1097/01.prs.0000181662.94027.3c. [DOI] [PubMed] [Google Scholar]
- 66.Mühlbauer W, Holm C. Computer imaging and surgical reality in aesthetic rhinoplasty. Plast Reconstr Surg. 2005;115(7):2098–2104. doi: 10.1097/01.prs.0000164676.72074.6a. [DOI] [PubMed] [Google Scholar]
- 67.Moses S, Mahler D. After aesthetic rhinoplasty: new looks and psychological outlooks on post-surgical satisfaction. Aesthetic Plast Surg. 1984;8:213. doi: 10.1007/BF01570705. [DOI] [PubMed] [Google Scholar]
- 68.Goin MK, Rees TD. A prospective study of patients' psychological reactions to rhinoplasty. Ann Plast Surg. 1991;27:210. doi: 10.1097/00000637-199109000-00004. [DOI] [PubMed] [Google Scholar]
- 69.Perkins SW, Hamilton MM. Endonasale Zugänge zur Nasenspitze. In: Behrbohm H, Tardy ME Jr, editors. Funktionell-ästhetische Chirurgie der Nase. Stuttgart, New York: Thieme; 2004. [Google Scholar]
- 70.Demirtas Y, Ayhan S, Tulmac M, Findikcioglu F, Ozkose Z, Yalcin R, Atabay K. Hemodynamic effects of perioperative stressor events during rhinoplasty. Plast Reconstr Surg. 2005;115(2):620–626. doi: 10.1097/01.prs.0000150153.16897.d2. [DOI] [PubMed] [Google Scholar]
- 71.Cavallini M, Baruffaldi Preis FW, Casati A. Effects of mild hypothermia on blood coagulation in patients undergoing elective plastic surgery. Plast Reconstr Surg. 2005;116(1):316–321. doi: 10.1097/01.prs.0000170798.45679.7a. [DOI] [PubMed] [Google Scholar]
- 72.Kim DW, Toriumi DM. Rhinoplastik in offener Technik. In: Behrbohm H, Tardy ME Jr, editors. Funktionell-ästhetische Chirurgie der Nase. Septorhinoplastik. Stuttgart, New York: Thieme; 2004. [Google Scholar]
- 73.Huizing EH, de Groot JAM, editors. Functional reconstructive Nasal surgery. Stuttgart, New York: Thieme; 2003. [Google Scholar]
- 74.Rajan GP, Fergie N, Fischer U, Romer M, Radivojevic V, Hee GK. Antibiotic prophylaxis in septorhinoplasty? A prospective, randomized study. Plast Reconstr Surg. 2005;116(7):1995–1998. doi: 10.1097/01.prs.0000191181.73298.b3. [DOI] [PubMed] [Google Scholar]
- 75.Michelson A, Wolf SR, Rettinger G, Zichner M. Antibiotikaprophylaxe in der Rhinochirurgie. HNO. 1993;41(9):421–425. [PubMed] [Google Scholar]
- 76.Tasman AJ, Wallner F, Neumeier R. Antibiotische Imprägnation von Knorpelimplantaten: Diffusionskinetik von Fluorchinolonen. Laryngorhinootologie. 2000;79:30–33. doi: 10.1055/s-2000-8778. [DOI] [PubMed] [Google Scholar]
- 77.Kittel H, Masing H. Corticosteroid therapy in rhinoplasty. Rhinology. 1976;14(4):163–166. [PubMed] [Google Scholar]
- 78.Kara CO, Gokalan I. Effects of single-dose steroid usage on edema, ecchymosis, and intraoperative bleeding in rhinoplasty. Plast Reconstr Surg. 1999;104(7):2213–2218. doi: 10.1097/00006534-199912000-00041. [DOI] [PubMed] [Google Scholar]
- 79.Hanasono MM, Kridel RW, Pastorek NJ, Glasgold MJ, Koch RJ. Correction of the soft tissue pollybeak using triamcinolone injection. Arch Facial Plast Surg. 2002;4(1):26–30. doi: 10.1001/archfaci.4.1.26. [DOI] [PubMed] [Google Scholar]
- 80.Sclafani AP, Romo T, 3rd, Barnett JG, Barnett CR. Adjustment of subtle postoperative nasal defects: managing the "near-miss" rhinoplasty. Facial Plast Surg. 2003;19(4):349–361. doi: 10.1055/s-2004-815655. [DOI] [PubMed] [Google Scholar]
- 81.Guyuron B. Discussion: Changing the Convexity and Concavity of Nasal Cartilages and Cartilage Grafts with Horizontal Mattress Sutures; Part I. Experimental Results and Part II. Clinical Results. Plast Reconstr Surg. 2005;115(2):607–608. doi: 10.1097/01.prs.0000150145.39509.db. [DOI] [PubMed] [Google Scholar]
- 82.Sheen JH. The ideal dorsal graft: A continuing quest. Plast Reconstr Surg. 1998;102:2490. doi: 10.1097/00006534-199812000-00036. [DOI] [PubMed] [Google Scholar]
- 83.Rettinger G. Eingriffe der Nase. In: Theissing J, Rettinger G, Werner J, editors. HNO-Operationslehre. 4. Aufl. Stuttgart, New York: Thieme; 2005. [Google Scholar]
- 84.Gibson T, Davis WB. Distortion of autogenous rib grafts: its cause and prevention. Br J Plast Surg. 1957;10:247–274. [Google Scholar]
- 85.Agaoglu G, Erol OO. In situ split costal cartilage graft harvesting through a small incision using a gouge. Plast Reconstr Surg. 2000;106(4):932–935. [PubMed] [Google Scholar]
- 86.Jackson IT, Yavuzer R. Alloderm for Dorsal Nasal Irregularities. Plast Reconstr Surg. 2001;107:551–558. doi: 10.1097/00006534-200102000-00038. [DOI] [PubMed] [Google Scholar]
- 87.Daniel RK, Calvert JW. Diced cartilage grafts in rhinoplasty surgery. Plast Reconstr Surg. 2004;113(7):2156–2171. doi: 10.1097/01.prs.0000122544.87086.b9. [DOI] [PubMed] [Google Scholar]
- 88.Calvert JW, Brenner K, DaCosta-Iyer M, Evans GR, Daniel RK. Histological analysis of human diced cartilage grafts. Plast Reconstr Surg. 2006;118(1):230–236. doi: 10.1097/01.prs.0000220463.73865.78. [DOI] [PubMed] [Google Scholar]
- 89.Erol OO. The Turkish delight: a pliable graft for rhinoplasty. Plast Reconstr Surg. 2000;105(6):2229–2241. doi: 10.1097/00006534-200005000-00051. [DOI] [PubMed] [Google Scholar]
- 90.Elahi MM, Jackson IT, Moreira-Gonzalez A, Yamini D. Nasal augmentation with Surgicel-wrapped diced cartilage: a review of 67 consecutive cases. Plast Reconstr Surg. 2003;111(3):1309–1318. doi: 10.1097/01.PRS.0000047442.41691.C8. [DOI] [PubMed] [Google Scholar]
- 91.Gurley JM, Pilgram T, Perlyn CA, Marsh JL. Long-term outcome of autogenous rib graft nasal reconstruction. Plast Reconstr Surg. 2001;108(7):1895–1905. doi: 10.1097/00006534-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 92.Reich, J The application of dermis grafts in deformities of the nose. Plast Reconstr Surg. 1983;71:772. doi: 10.1097/00006534-198306000-00005. [DOI] [PubMed] [Google Scholar]
- 93.Erdogan B, Tuncel A, Adanali G, Deren O, Ayhan M. Augmentation rhinoplasty with dermal graft and review of the literature. Plast Reconstr Surg. 2003;111(6):2060–2068. doi: 10.1097/01.PRS.0000056841.23067.0F. [DOI] [PubMed] [Google Scholar]
- 94.Gryskiewicz JM. Waste not, want not: the use of AlloDerm in secondary rhinoplasty. Plast Reconstr Surg. 2005;116(7):1999–2004. doi: 10.1097/01.prs.0000191180.77028.7a. [DOI] [PubMed] [Google Scholar]
- 95.Gryskiewicz JM, Rohrich RJ, Reagan BJ. The use of alloderm for the correction of nasal contour deformities. Plast Reconstr Surg. 2001;107(2):561–570. doi: 10.1097/00006534-200102000-00040. [DOI] [PubMed] [Google Scholar]
- 96.Miller TA. Temporalis fascia grafts for facial and nasal contour augmentation. Plast Reconstr Surg. 1988;81:524. doi: 10.1097/00006534-198804000-00007. [DOI] [PubMed] [Google Scholar]
- 97.Baker TM, Courtiss EH. Temporalis fascia grafts in open secondary rhinoplasty. Plast Reconstr Surg. 1994;93:802. doi: 10.1097/00006534-199404000-00023. [DOI] [PubMed] [Google Scholar]
- 98.Guerrerosantos J. Temporoparietal free fascia grafts in rhinoplasty. Plast Reconstr Surg. 1984;74:465. doi: 10.1097/00006534-198410000-00001. [DOI] [PubMed] [Google Scholar]
- 99.Sheen JH. Temporoparietal free fascia grafts in rhinoplasty (Discussion) Plast Reconstr Surg. 1984;74:475. doi: 10.1097/00006534-198410000-00001. [DOI] [PubMed] [Google Scholar]
- 100.Leaf N. SMAS autografts for the nasal dorsum. Plast Reconstr Surg. 1996;97:1249. doi: 10.1097/00006534-199605000-00025. [DOI] [PubMed] [Google Scholar]
- 101.Koronas TC, Bucky LP, Hurley C, JW The fate of suctioned and surgically removed fat after reimplantation for soft-tissue augmentation: A volumetric and histologic study in the rabbit. Plast Reconstr Surg. 1993;91:763. doi: 10.1097/00006534-199304001-00001. [DOI] [PubMed] [Google Scholar]
- 102.Romo T, 3rd, Sclafani AP, Jacono AA. Nasal reconstruction using porous polyethylene implants. Facial Plast Surg. 2000;16(1):55–61. doi: 10.1055/s-2000-7326. [DOI] [PubMed] [Google Scholar]
- 103.McCurdy JA., Jr The Asian nose: augmentation rhinoplasty with L-shaped silicone implants. Facial Plast Surg. 2002;18(4):245–252. doi: 10.1055/s-2002-36492. [DOI] [PubMed] [Google Scholar]
- 104.Mackay IS. Rhinoplasty. A practical guide to functional and aesthetic surgery of the nose. The Hague, Netherlands: Kugler Publications; 1998. Augmentation rhinoplasty. [Google Scholar]
- 105.Lawson W, Reino AJ, Seidman D. The silicone columellar strut. Plast Reconstr Surg. 1996;97(5):938–943. doi: 10.1097/00006534-199604001-00008. [DOI] [PubMed] [Google Scholar]
- 106.Beekhuis GJ. Silastic alar-columellar prosthesis in conjunction with rhinoplasty. Arch Otolaryngol. 1982;108(7):429–432. doi: 10.1001/archotol.1982.00790550033008. [DOI] [PubMed] [Google Scholar]
- 107.Baran CN, Tiftikcioglu YO, Baran NK. The use of alloplastic materials in secondary rhinoplasties: 32 years of clinical experience. Plast Reconstr Surg. 2005;116(5):1502–1516. doi: 10.1097/01.prs.0000182603.05914.bd. [DOI] [PubMed] [Google Scholar]
- 108.Stoll W. The use of polytetrafluoroethylene for particular augmentation of the nasal dorsum. Aesthetic Plast Surg. 1991;15:233. doi: 10.1007/BF02273864. [DOI] [PubMed] [Google Scholar]
- 109.Waldman SR. Gore-Tex for augmentation of the nasal dorsum: a preliminary report. Ann Plast Surg. 1991;26(6):520–525. doi: 10.1097/00000637-199106000-00005. [DOI] [PubMed] [Google Scholar]
- 110.Zhanqiang L. Carving Gore-Tex reinforced sheets for augmentation rhinoplasty in Chinese patients. Plast Reconstr Surg. 2006;117(1):326–328. doi: 10.1097/01.prs.0000196247.16012.65. [DOI] [PubMed] [Google Scholar]
- 111.Stal S, Hollier L. The use of resorbable spacers for nasal spreader grafts. Plast Reconstr Surg. 2000;106(4):922–928. [PubMed] [Google Scholar]
- 112.Gilmore, J Use of Vicryl mesh in prevention of postrhinoplasty dorsal irregularities. Ann Plast Surg. 1989;22:105. doi: 10.1097/00000637-198902000-00004. [DOI] [PubMed] [Google Scholar]
- 113.Kamer FM, Parkes ML. Gelatin film: A useful adjunct in rhinoplastic surgery. Acta Otolaryngol. 1977;103:667. [PubMed] [Google Scholar]
- 114.Carey JW, Steegmann AT., Jr Human nasal protrusion, latitude, and climate. Am J Phys Anthropol. 1981;56(3):313–319. doi: 10.1002/ajpa.1330560312. [DOI] [PubMed] [Google Scholar]
- 115.Franciscus RG, Trinkaus E. Nasal morphology and the emergence of Homo erectus. Am J Phys Anthropol. 1988;75(4):517–527. doi: 10.1002/ajpa.1330750409. [DOI] [PubMed] [Google Scholar]
- 116.Rubin FF. Two New Instruments for Rhinoplastic Surgery. Arch Otolaryng. 1967;85:698–700. doi: 10.1001/archotol.1967.00760040700021. [DOI] [PubMed] [Google Scholar]
- 117.Rohrich RJ, Muzaffar AR, Janis JE. Component dorsal hump reduction: the importance of maintaining dorsal aesthetic lines in rhinoplasty. Plast Reconstr Surg. 2004;114(5):1298–1308. doi: 10.1097/01.prs.0000135861.45986.cf. [DOI] [PubMed] [Google Scholar]
- 118.Camirand A, Doucet J, Harris J. Nose surgery: how to prevent a middle vault collapse - a review of 50 patients 3 to 21 years after surgery. Plast Reconstr Surg. 2004;114(2):527–534. doi: 10.1097/01.prs.0000128425.01547.45. [DOI] [PubMed] [Google Scholar]
- 119.Guyuron B. Precision rhinoplasty. Part II: prediction. Plast Reconstr Surg. 1988;81:500. doi: 10.1097/00006534-198804000-00002. [DOI] [PubMed] [Google Scholar]
- 120.Huizing EH, de Groot JAM, editors. Functional reconstructive Nasal surgery. Stuttgart, New York: Thieme; 2003. [Google Scholar]
- 121.Peck GC. Rhinoplasty. Stuttgart: Georg Thieme Verlag; 1984. [Google Scholar]
- 122.Trepsat F. A different rasp for rhinoplasty. Plast Reconstr Surg. 1987;79(4):638–639. doi: 10.1097/00006534-198704000-00024. [DOI] [PubMed] [Google Scholar]
- 123.Mang WL. Manual of aesthetic surgery. Berlin, Heidelberg, New York: Springer-Verlag; 2002. [Google Scholar]
- 124.Wright WK. Study on hump removal in rhinoplasty. Laryngoscope. 1967;77:508. doi: 10.1288/lary.1967.000770406. [DOI] [PubMed] [Google Scholar]
- 125.Skoog T. A method of hump reduction in rhinoplasty. Arch Otolaryngol. 1966;83:283–287. doi: 10.1001/archotol.1966.00760020285020. [DOI] [PubMed] [Google Scholar]
- 126.Harshbarger RJ, Sullivan PK. The optimal medial osteotomy: a study of nasal bone thickness and fracture patterns. Plast Reconstr Surg. 2001;108(7):2114–2119. doi: 10.1097/00006534-200112000-00048. [DOI] [PubMed] [Google Scholar]
- 127.Bhatia K, Jones NS, Bull TR. The use of Heanley bone-cutting forceps to reduce the thickened and broad bony dorsum in rhinoplasty. Arch Facial Plast Surg. 2002;4(3):186–189. doi: 10.1001/archfaci.4.3.186. [DOI] [PubMed] [Google Scholar]
- 128.Aiach G. Atlas of Rhinoplasty: Open and endonasal approaches. St. Louis, Missouri: Quality Medical Publishing; 1996. [Google Scholar]
- 129.Byrd HS, Salomon J, Wood J. Correction of the crooked nose. Plast Reconstr Surg. 1998;102:2148. doi: 10.1097/00006534-199811000-00055. [DOI] [PubMed] [Google Scholar]
- 130.Meyer R. Crooked nose. In: Gruber RP, Peck GC, editors. Rhinoplasty: State of the Art. St. Louis: Mosby; 1993. [Google Scholar]
- 131.Denecke H, Meyer R. Plastic Surgery of Head and Neck: Corrective and Reconstructive Rhinoplasty. New York, NY: Springer-Verlag NY Inc; 1967. [Google Scholar]
- 132.Giampapa VC, DiBernardo BE. Nasal osteotomy - utilizing dual plane reciprocating nasal saw blades: a 6-year follow-up. Ann Plast Surg. 1993;30(6):500–502. doi: 10.1097/00000637-199306000-00004. [DOI] [PubMed] [Google Scholar]
- 133.Castro A, Jackson IT, Rademaker B. Rhinoplasty saw: a modified design. Ann Plast Surg. 1991;26(6):600–601. doi: 10.1097/00000637-199106000-00020. [DOI] [PubMed] [Google Scholar]
- 134.Diamond HP. Rhinoplasty technique. Surg Clin North Am. 1971;51:317–331. doi: 10.1016/s0039-6109(16)39379-3. [DOI] [PubMed] [Google Scholar]
- 135.Rees TD. Nasal osteotomies: A clinical comparison of the perforating methods versus the continuous technique. Letters and viewpoints. Plast Reconstr Surg. 2005;115(6):1783–1784. doi: 10.1097/01.prs.0000162108.94263.10. [DOI] [PubMed] [Google Scholar]
- 136.Rohrich RJ, Krueger JK. The lateral osteotomy in rhinoplasty: Clinical and radiographic rationale for osteotome selection (Discussion) Plast Reconst Surg. 2000;105(5):1817–1819. doi: 10.1097/00006534-200004050-00031. [DOI] [PubMed] [Google Scholar]
- 137.Rohrich RJ, Minoli JJ, Adams WP, Hollier LH. The lateral nasal osteotomy in rhinoplasty: An anatomic endoscopic comparison of the external versus the internal approach. Plast Reconstr Surg. 1997;99:1309. doi: 10.1097/00006534-199704001-00015. [DOI] [PubMed] [Google Scholar]
- 138.Hilger JA. The internal lateral osteotomy in rhinoplasty. Arch Otolaryngol. 1968;88:119. doi: 10.1001/archotol.1968.00770010213026. [DOI] [PubMed] [Google Scholar]
- 139.Parkes ML, Kayner F, Morgan WR. Double lateral osteotomy in rhinoplasty. Arch Otolaryngol. 1977;103(6):344–348. doi: 10.1001/archotol.1977.00780230066010. [DOI] [PubMed] [Google Scholar]
- 140.Goldfarb M, Gallups JM, Gensin JM. Perforating osteotomies in rhinoplasty. Arch Otolaryngol Head Neck Surg. 1993;119:624. doi: 10.1001/archotol.1993.01880180038006. [DOI] [PubMed] [Google Scholar]
- 141.Tardy ME, Denneny JC. Micro-osteotomies in rhinoplasty. Facial Plast Surg. 1984;1:137. [Google Scholar]
- 142.Larrabee W. Open rhinoplasty and the upper third of the nose. Facial Plast Surg Clin North Am. 1993;1:23. [Google Scholar]
- 143.Murakami CS, Younger RAL. Managing the postrhinoplasty or post-traumatic crooked nose. Facial plast Surg Clin North Am. 1995;3:421. [Google Scholar]
- 144.Webster RC, Davidson TM, Smith RC. Curved lateral osteotomy for airway protection in rhinoplasty. Arch Otolaryngol. 1977;103:454. doi: 10.1001/archotol.1977.00780250048003. [DOI] [PubMed] [Google Scholar]
- 145.Ford CN, Battaglia DG, Gentry LR. Preservation of periosteal attachment in lateral osteotomy. Ann Plast Surg. 1984;13:107. doi: 10.1097/00000637-198408000-00003. [DOI] [PubMed] [Google Scholar]
- 146.Murakami CS, Larrabee WE. Comparison of osteotomy techniques in the treatment of nasal fractures. Facial Plast Surg. 1992;8:209. doi: 10.1055/s-2008-1064652. [DOI] [PubMed] [Google Scholar]
- 147.Gryskiewicz JM, Gryskiewicz KM. Lateral Osteotomies: A Clinical Comparison of e Perforating Methods versus the conntinuous Technique. Plast Reconstr Surg. 2004;113(5):1445–1456. doi: 10.1097/01.prs.0000113031.67600.b9. [DOI] [PubMed] [Google Scholar]
- 148.Rohrich RJ, Janis JE, Adams WP, Krueger JK. Update on the LateraI Nasal Osteotomy in Rhinoplasty: An Anatomic endoscopic comparison of the External versus the internal Approach. Plast Reconstr Surg. 2003;111(7):2461–2462. doi: 10.1097/01.PRS.0000061005.27994.E3. [DOI] [PubMed] [Google Scholar]
- 149.Gryskiewicz JM. Visible scars from percutaneous osteotomies. Plast Reconstr Surg. 2005;116(6):1771–1775. doi: 10.1097/01.prs.0000186531.98814.30. [DOI] [PubMed] [Google Scholar]
- 150.Minoli JJ. Update on the Lateral Nasal Osteotomy in Rhinoplasty: An Atomic Endoscopic Comparison of the External versus the Approach (Discussion) Plast Reconstr Surg. 2003;111(7):2463. doi: 10.1097/01.PRS.0000061005.27994.E3. [DOI] [PubMed] [Google Scholar]
- 151.Adams WP, Rohrich RJ, Hollier LH, Minoli J, Thornton LK, Gyimesi I. Anatomic basis and clinical implications for nasal tip support in open versus closed rhinoplasty. Plast Reconstr Surg. 1999;103:255–261. doi: 10.1097/00006534-199901000-00040. [DOI] [PubMed] [Google Scholar]
- 152.Becker DG, McLaughlin RB, Jr, Loevner LA, Mang A. The Lateral Osteotomy in Rhinoplasty: Clinical und Radiographic Rationale for Osteotome Selection. Plast Reconstr Surg. 2000;105(5):1806. doi: 10.1097/00006534-200004050-00031. [DOI] [PubMed] [Google Scholar]
- 153.Kuran I, Ozcan H, lista A, Bos L. Comparison of four different types of osteotomes for lateral os-teotomy: A cadaver study. Aesthetic Plast Surg. 1996;20:323. doi: 10.1007/BF00228464. [DOI] [PubMed] [Google Scholar]
- 154.Thomas JR, Griner NR, Remmler DJ. Steps for a safer method of osteotomies in rhinoplasty. Laryngoscope. 1987;97:746. doi: 10.1288/00005537-198706000-00021. [DOI] [PubMed] [Google Scholar]
- 155.Rohrich RJ, Gunter JP, Deuber MA, Adams WP., Jr The deviated nose: optimizing results using a simplified classification and algorithmic approach. Plast Reconstr Surg. 2002;110(6):1509–1523. doi: 10.1097/01.PRS.0000029975.08760.25. [DOI] [PubMed] [Google Scholar]
- 156.Smith RA, Smith ET. A new technique in nasal-tip reduction surgery. Plast Reconstr Surg. 2001;108(6):1798–1804. doi: 10.1097/00006534-200111000-00059. [DOI] [PubMed] [Google Scholar]
- 157.Guyuron B, Behmand RA. Caudal nasal deviation. Plast Reconstr Surg. 2003;111(7):2449–2457. doi: 10.1097/01.PRS.0000060802.70218.FE. [DOI] [PubMed] [Google Scholar]
- 158.Pontius AT, Williams EF., 3rd Endonasal placement of spreader grafts in rhinoplasty. Ear Nose Throat J. 2005;84(3):135–136. [PubMed] [Google Scholar]
- 159.Rohrich RJ, Griffin JR. Correction of intrinsic nasal tip asymmetries in primary rhinoplasty. Plast Reconstr Surg. 2003;112(6):1699–1712. doi: 10.1097/01.PRS.0000086367.74899.3F. [DOI] [PubMed] [Google Scholar]
- 160.Riechelmann H, Rettinger G. Three-step reconstruction of complex saddle nose deformities. Arch Otolaryngol Head Neck Surg. 2004;130(3):334–338. doi: 10.1001/archotol.130.3.334. [DOI] [PubMed] [Google Scholar]
- 161.Gunter JR, Clark CR, Friedman RM. Internal stabilization of autogenous rib cartilage: A barrier to cartilage warping. Plast Reconstr Surg. 1997;100:161. doi: 10.1097/00006534-199707000-00026. [DOI] [PubMed] [Google Scholar]
- 162.Constantian MB. The two essential elements for planning tip surgery in primary and secondary rhinoplasty: observations based on review of 100 consecutive patients. Plast Reconstr Surg. 2004;114(6):1571–1581. doi: 10.1097/01.prs.0000138755.00167.f5. [DOI] [PubMed] [Google Scholar]
- 163.Kuran I, Tumerdem B, Tosun U, Yildiz K. Evaluation of the effects of tip-binding sutures and cartilaginous grafts on tip projection and rotation. Plast Reconstr Surg. 2005;116(1):282–288. doi: 10.1097/01.prs.0000169959.73447.90. [DOI] [PubMed] [Google Scholar]
- 164.Tasman AJ. Der infrakartilaginäre Zugang zur Nasenspitze. Laryngorhinootologie. 2004;84:234–238. [Google Scholar]
- 165.Adamson PA, Galli SK. Rhinoplasty approaches: current state of the art. Arch Facial Plast Surg. 2005;7(1):32–37. doi: 10.1001/archfaci.7.1.32. [DOI] [PubMed] [Google Scholar]
- 166.Teichgraeber JF, Riley WB, Russo RC. External rhinoplasties: indications for use. Br J Plast Surg. 1992;45:47–54. doi: 10.1016/0007-1226(92)90116-f. [DOI] [PubMed] [Google Scholar]
- 167.Stoll W. 5 years experience with "open septorhinoplasty". Laryngorhinootologie. 1991;70:171–176. doi: 10.1055/s-2007-998015. [DOI] [PubMed] [Google Scholar]
- 168.Adant JP, Bluth F, Fisette J. External rhinoplasty: a useful approach for a young plastic surgeon. Ann Chir Plast Esthet. 1998;43:635–648. [PubMed] [Google Scholar]
- 169.Smith O, Goodman W. Open rhinoplasty: its past and future. J Otolaryngol. 1993;22:21–25. [PubMed] [Google Scholar]
- 170.Gruber RP, Friedman GD. Suture algorithm for the broad or bulbous nasal tip. Plast Reconstr Surg. 2002;110:1752–1764. doi: 10.1097/01.PRS.0000033873.20163.61. [DOI] [PubMed] [Google Scholar]
- 171.Adamson PA. Incision and scar analysis in open (external) rhinoplasty. Arch Otolaryngol Head Neck Surg. 1990;116:671–675. doi: 10.1001/archotol.1990.01870060029003. [DOI] [PubMed] [Google Scholar]
- 172.Foda HM. External rhinoplasty: a critical analysis of 500 cases. J Laryngol Otol. 2003;117(6):473–477. doi: 10.1258/002221503321892325. [DOI] [PubMed] [Google Scholar]
- 173.Guerrerosantos J. Open rhinoplasty without skin-columella incision. Plast Reconstr Surg. 1990;85:955–960. doi: 10.1097/00006534-199006000-00022. [DOI] [PubMed] [Google Scholar]
- 174.Bafaqeeh SA, al-Qattan MM. Alterations in nasal sensibility following open rhinoplasty. Br J Plast Surg. 1998;51:508. doi: 10.1054/bjps.1997.0296. [DOI] [PubMed] [Google Scholar]
- 175.Kastenbauer E. Was hat sich geändert in der funktionell-ästhetischen Rhinochirurgie? Laryngorhinootologie. 1989;68(1):4–11. doi: 10.1055/s-2007-998276. [DOI] [PubMed] [Google Scholar]
- 176.Aiach G. Mini-forum: rhinoplasty by external approach. External or endonasal approach for rhinoplasty? Ann Chir Plast Esthet. 1992;37:498–509. [PubMed] [Google Scholar]
- 177.Draf W, Schauss F. External rhinoplasty: its role in aesthetic and functional surgery of the nose. Facial Plast Surg. 1995;11:228–236. doi: 10.1055/s-2008-1064537. [DOI] [PubMed] [Google Scholar]
- 178.Cardenas-Camarena L, Guerrero MT. Improving nasal tip projection and definition using interdomal sutures and open approach without transcolumellar incision. Aesthetic Plast Surg. 2002;26:161–166. doi: 10.1007/s00266-002-1488-x. [DOI] [PubMed] [Google Scholar]
- 179.Sheen JH. Closed versus open rhinoplasty - and the debate goes on. Plast Reconstr Surg. 1997;99:859–862. doi: 10.1097/00006534-199703000-00039. [DOI] [PubMed] [Google Scholar]
- 180.Anderson JR. A reasoned approach to nasal base surgery. Arch Otolaryngol. 1984;110(6):349–358. doi: 10.1001/archotol.1984.00800320003001. [DOI] [PubMed] [Google Scholar]
- 181.Beaty MM, Dyer WK, 2nd, Shawl MW. The quantification of surgical changes in nasal tip support. Arch Facial Plast Surg. 2002;4(2):82–91. doi: 10.1001/archfaci.4.2.82. [DOI] [PubMed] [Google Scholar]
- 182.Rohrich RJ, Adams WP. The boxy nasal tip: Classification and management based on alar cartilage suturing techniques. Plast Reconstr Surg. 2001;107:1849. [PubMed] [Google Scholar]
- 183.Daniel RK. Rhinoplasty: A simplified, three-stitch, open tip suture technique. Part I: Primary rhinoplasty. Plast Reconstr Surg. 1999;103:1491. doi: 10.1097/00006534-199904050-00022. [DOI] [PubMed] [Google Scholar]
- 184.Tebbetts JB. Shaping and positioning the nasal tip without structural disruption: A new, Systematic approach. Plast Reconstr Surg. 1994;94:61. doi: 10.1097/00006534-199407000-00006. [DOI] [PubMed] [Google Scholar]
- 185.Behmand RA, Ghavami A, Guyuron B. Nasal tip sutures: Part I. The evolution. Plast Reconstr Surg. 2003;112:1125. doi: 10.1097/01.PRS.0000076503.78510.1C. [DOI] [PubMed] [Google Scholar]
- 186.Guyuron B, Behmand RA. Nasal tip sutures. part II. The interplays. Plast Reconstr Surg. 2003;112:1130. doi: 10.1097/01.PRS.0000076505.83375.74. [DOI] [PubMed] [Google Scholar]
- 187.Tebbetts JB. Rethinking the logic and techniques of primary tip rhinoplasty. A perspective of the evolution of surgery of the nasal tip. Clin Plast Surg. 1996;23(2):245–253. [PubMed] [Google Scholar]
- 188.Calderon-Cuellar LT, Trujillo-Hernandez B, Vasquez C, Padilla-Acero J, Cisneros-Preciado H. Modified mattress suture technique to correct anterior septal deviation. Plast Reconstr Surg. 2004;114(6):1436–1441. doi: 10.1097/01.prs.0000138816.48312.ad. [DOI] [PubMed] [Google Scholar]
- 189.Gruber RP, Nahai F, Bogdan MA, Friedman GD. Changing the Convexity and Concavity of Nasal cartilages and cartilage grafts with horizontal mattress sutures: Part II. Clinical Results. Plast Reconstr Surg. 2005;115(2):595–606. doi: 10.1097/01.prs.0000150146.04465.81. [DOI] [PubMed] [Google Scholar]
- 190.Rohrich RJ, Friedman RM, Liland DL. Comparison of otoplasty techniques in the rabbit model. Ann Plast Surg. 1995;34:43. doi: 10.1097/00000637-199501000-00009. [DOI] [PubMed] [Google Scholar]
- 191.Gruber RP, Nahai F, Bogdan MA, Friedman GD. Changing the convexity and concavity of nasal cartilages and cartilage grafts with horizontal mattress sutures: part I. Experimental results. Plast Reconstr Surg. 2005;115(2):589–594. doi: 10.1097/01.prs.0000150145.39509.db. [DOI] [PubMed] [Google Scholar]
- 192.Meyer R, Jovanovic B, Derder S. All about nasal valve collapse. Aesthetic Plast Surg. 1996;20:141. doi: 10.1007/BF02275534. [DOI] [PubMed] [Google Scholar]
- 193.Schlosser RJ, Park SS. Functional nasal surgery. Otolaryngol Clin North Am. 1999;32:37. doi: 10.1016/s0030-6665(05)70114-6. [DOI] [PubMed] [Google Scholar]
- 194.Ozturan O, Miman MC, Kizilay A. Bending of the upper lateral cartilages for nasal valve collapse. Arch Facial Plast Surg. 2002;4:258. doi: 10.1001/archfaci.4.4.258. [DOI] [PubMed] [Google Scholar]
- 195.Park SS. The flaring suture to augment the repair of the dysfunctional nasal valve. Plast Reconstr Surg. 1998;101:1120. doi: 10.1097/00006534-199804040-00036. [DOI] [PubMed] [Google Scholar]
- 196.Cardenas JC, Carvajal J, Ruiz A. Securing nasal tip rotation through suspension suture technique. Plast Reconstr Surg. 2006;117(6):1750–1755. doi: 10.1097/01.prs.0000210029.58404.51. [DOI] [PubMed] [Google Scholar]
- 197.Goldman IB. Surgical tips on the nasal tip. Eye Ear Nose Throat Mon. 1954;33:583–591. [PubMed] [Google Scholar]
- 198.Davis AM, Simons RL, Rhee JS. Evaluation of the Goldman Tip Procedure in Modern-Day Rhinoplasty. Arch Facial Plast Surg. 2004;6:301–308. doi: 10.1001/archfaci.6.5.301. [DOI] [PubMed] [Google Scholar]
- 199.Foda HM, Kridel RW. Lateral crural steal and lateral crural overlay: an objective evaluation. Arch Otolaryngol Head Neck Surg. 1999;125(12):1365–1370. doi: 10.1001/archotol.125.12.1365. [DOI] [PubMed] [Google Scholar]
- 200.Pastorek NJ, Bustillo A, Murphy MR, Becker DG. The extended columellar strut-tip graft. Arch Facial Plast Surg. 2005;7(3):176–184. doi: 10.1001/archfaci.7.3.176. [DOI] [PubMed] [Google Scholar]
- 201.Rohrich RJ, Raniere J, Jr, Ha RY. The alar contour graft: correction and prevention of alar rim deformities in rhinoplasty. Plast Reconstr Surg. 2002;109(7):2495–2505. doi: 10.1097/00006534-200206000-00050. [DOI] [PubMed] [Google Scholar]
- 202.Collawn SS, Fix RJ, Moore JR, Vasconez LO. Nasal cartilage grafts: more than a decade of experience. Plast Reconstr Surg. 1997;100:1547. doi: 10.1097/00006534-199711000-00027. [DOI] [PubMed] [Google Scholar]
- 203.Constantian MB. Functional effects of alar cartilage malposition. Ann Plast Surg. 1993;30:487. doi: 10.1097/00000637-199306000-00003. [DOI] [PubMed] [Google Scholar]
- 204.Foda HM. Management of the droopy tip: a comparison of three alar cartilage-modifying techniques. Plast Reconstr Surg. 2003;112(5):1408–1417. doi: 10.1097/01.PRS.0000081065.48569.43. [DOI] [PubMed] [Google Scholar]
- 205.Gruber RP. Primary open rhinoplasty. In: Gruber RP, Peck GC, editors. Rhinoplasty State of the Art. St. Louis: Mosby-Year Book; 1993. [Google Scholar]
- 206.Walter C. Plastisch-chirurgische Eingriffe im Kopf-Halsbereich. Stuttgart: Thieme; 1997. [Google Scholar]
- 207.Boccieri A. Mini spreader grafts: a new technique associated with reshaping of the nasal tip. Plast Reconstr Surg. 2005;116(5):1525–1534. doi: 10.1097/01.prs.0000182787.99210.10. [DOI] [PubMed] [Google Scholar]
- 208.Gruber RP. The short nose. Clin Plast Surg. 1996;23(2):297–313. [PubMed] [Google Scholar]
- 209.Peck GC. The onlay graft for nasal tip projection. Plast Reconstr Surg. 1983;71:27. doi: 10.1097/00006534-198301000-00007. [DOI] [PubMed] [Google Scholar]
- 210.Sheen JH. Secondary rhinoplasty. Plast Reconstr Surg. 1975;56:137. doi: 10.1097/00006534-197508000-00003. [DOI] [PubMed] [Google Scholar]
- 211.Hamra ST. Lengthening the foreshortened nose. Plast Reconstr Surg. 2001;108(2):547–549. doi: 10.1097/00006534-200108000-00042. [DOI] [PubMed] [Google Scholar]
- 212.Guyuron B, Varghai A. Lengthening the nose with a tongue-and-groove technique. Plast Reconstr Surg. 2003;111(4):1533–1539. doi: 10.1097/01.PRS.0000049637.42449.80. [DOI] [PubMed] [Google Scholar]
- 213.Constantian MB. The boxy nasal tip, the ball tip, and alar cartilage malposition: variations on a theme - a study in 200 consecutive primary and secondary rhinoplasty patients. Plast Reconstr Surg. 2005;116(1):268–281. doi: 10.1097/01.prs.0000169958.83870.e1. [DOI] [PubMed] [Google Scholar]
- 214.Oxford Centre for Evidence-based Medicine. 2001. [Download vom 10.08.2006]. Available from: http://www.cebm.net.
- 215.Ching S, Thoma A, McCabe RE, Antony MM. Measuring outcomes in aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg. 2003;111(1):469–480. doi: 10.1097/01.PRS.0000036041.67101.48. [DOI] [PubMed] [Google Scholar]


