Abstract
Background:
The aim of the study was to evaluate the relationship between obesity and periodontitis.
Materials and Methods:
A total of 300 subjects aged 20 years and above suffering from generalized periodontitis were recruited from Department of Periodontics, Pacific Dental College and Hospital, Udaipur. Periodontal status of the subjects was recorded. Body mass index and waist circumference were used as measure to assess obesity. Other variables like age, gender, oral hygiene index were also recorded.
Results:
When evaluation was done for prevalence of periodontal disease according to BMI in obese and non-obese, the prevalence of periodontal disease was significantly (P=0.03) more in obese (88%) than in non-obese (74.4%) individuals. [OR=−20.4 and 95% confidence interval (CI) 1.3-1.3].
Conclusion:
The prevalence of periodontal disease is higher among obese subjects. Obesity could be a potential risk factor for periodontal disease in all age groups.
Keywords: Body mass index, obesity, periodontal disease, waist circumference
INTRODUCTION
The global obesity epidemic has been described by the World Health Organization (2002) as one of the most blatantly visible but yet most neglected, public health problems that threatens to overwhelm both more and less developed countries. There is a concern for public health, as excess bodyweight is now the sixth important risk factor contributing to disease worldwide and increased level of obesity may result in a decline in life expectancy in the future.[1]
Obesity, one of the most significant health risks of modern society, is now recognized as a chronic disease with a multifactorial etiology.[2] It has reached an alarming stage, current figures in New Delhi indicate that every second person fulfils the criteria of obesity or has excess abdominal fat.[3] Besides being a risk factor for cardiovascular disease, certain cancers and type II diabetes, obesity has also been suggested to be a risk factor for periodontitis. Investigation from the United States, using the large NHANES III database, supported association between body fat and periodontal disease.[1]
Obesity may be considered as a low-grade systemic inflammatory disease. Obese children and adults have elevated serum levels of C-reactive proteins, interleukin-6, tumor necrosis factor-α and leptin which are known as markers of inflammation and are closely associated with chronic inflammatory diseases.[4] Therefore, these findings indicate rationalized bases for association between obesity and periodontal disease, which is also an inflammatory disease resulting from complex interaction between pathogenic microbes and host immune response.[5]
It has been observed that the incidence of obesity and related health hazards is continuously increasing in the urban population. Many recent studies have indicated that there is a positive correlation between obesity and periodontal disease.
Several studies have shown association between obesity and periodontal disease in different populations. 3rd National Family Health Survey (NFHS-3) has reported that there is an increasing tendency of obesity in Indian population. Hence, this study was undertaken to examine the relation between obesity and periodontal disease among the patient coming to department of Periodontology, Pacific Dental College and Hospital, Udaipur.
MATERIALS AND METHODS
The study population consisted of convenience and judgment sample of 300 subjects. All the subjects were included from the Outpatient Department of Periodontics, Pacific Dental College and Hospital, Udaipur, Rajasthan.
Inclusion criteria
Dentate persons, 20 years of age and above
Obese patients with and without diabetes, hypertension, osteoarthritis were included in the study.
Exclusion criteria
Patients who had received periodontal treatment or antibiotics for at least 3 months prior to study
Chronic usage of anti-inflammatory drugs and pre-medication within 3 months prior to study
Physically and mentally challenged patients
Pregnant women and lactating mothers
All potential participants were explained the need and design of the study. Only those subjects who gave consent for the study were included in the study.
Collection of data
Subjects reporting to the Department of Periodontics, Pacific Dental College, Udaipur, were screened for their periodontal status. Each subject was examined by a single examiner on a dental chair under proper illumination. The observations were recorded on a printed performa.
Variables like age and sex which could act as covariants for the periodontal disease were recorded. The patients were stratified according to age to three different age group.[1]
Younger age (20-34 years)
Middle age (35-59 years)
Older adults (60 years and above)
A complete intraoral examination was done and the oral hygiene was assessed and recorded using, oral hygiene index-simplified[2] and the periodontal status of each patient was evaluated by measuring the periodontal pocket depth.
Height (in meters) and weight (in kg) of each patient was recorded and the body mass index (BMI) was calculated. Further, the waist circumference (WC) (in centimeter) of each patient was recorded. The WC was measured (in centimeter) at midpoint between lower border of ribs and upper border of pelvis and was divided into two categories using the cutoff points 102 cm for men and 88 cm for women.[1,6] All the above measurements were recorded in centimeters using a measuring tape. The tape measures should be snug, but should not cause compression on skin.
Anthropometric data collection
The definition of obesity is based on the BMI, which is the ratio of body weight to body height squared. So the status of obesity was recorded using the BMI and WC measurement.
Hence, an individual was categorized as obese if the BMI was ≥30 and nonobese if the BMI was <30.[7]
The data obtained was statistically analyzed and the data was described as number and percentage.
RESULTS
Prevalence of periodontal disease according to age and gender
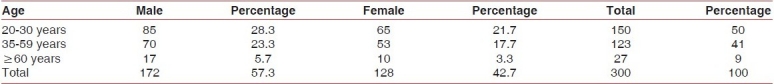
Out of 300 subjects, were divided into three groups according to age, 240 subjects (80%) had periodontal disease. The prevalence of periodontitis was 60.7% (91 out of 150 individual) in younger age group, 99.2% (122 out of 123 individual) in middle-age group and 100% (27 individuals) in older age group which is statistically significant (P=0.00), This implies an increase in prevalence of periodontal disease with increase in age [Table 1]. Whereas, when gender evaluation was done prevalence of periodontal disease was significantly higher (P=0.00) among female compared to males. Out of 128 females included in the study 125 subjects (97.7%) were affected by periodontal disease as compared to 115 out of 172 males (66%) [Tables 1–3].
Table 1.
Prevalence of periodontal disease according to age group
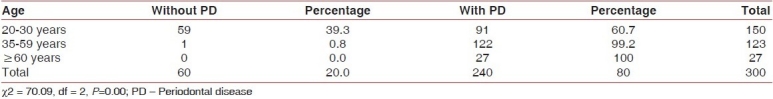
Table 3.
Prevalence of periodontal disease according to gender
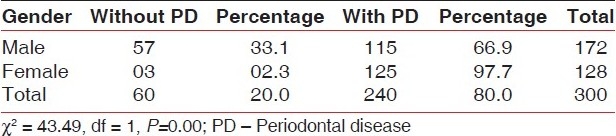
Table 2.
Distribution of study subjects according to age group and gender
So, according to age and gender the prevalence of periodontal disease was significantly higher in older age group compared to younger age group [OR = 22.6 and 95% confidence interval (CI) 5.0-8.8] and the prevalence of periodontal disease was lower in males as compared to females. [OR = 22.6 and 95% confidence interval (CI) 5.0-8.8], respectively.
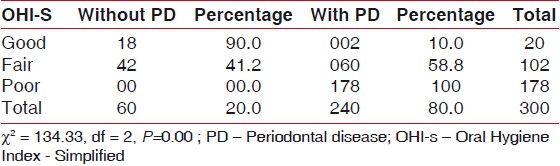
Prevalence of periodontal disease according to oral hygiene status
In the present study 20 subjects had good oral hygiene, 102 had fair and 172 had poor oral hygiene according to OHI-S score. The prevalence of periodontal status was 10% in good oral hygiene group, 58.8% in fair oral hygiene group and 100% in poor oral hygiene group. The association between oral hygiene status and periodontal disease is statistically significant (0.00) and according to oral hygiene status the prevalence of periodontal disease was significantly higher in poor oral hygiene group as compared to good oral hygiene. [OR = 21.8 and 95% confidence interval (CL) 3.0-3.0] [Table 4].
Table 4.
Prevalence of periodontal disease according to OHI-S
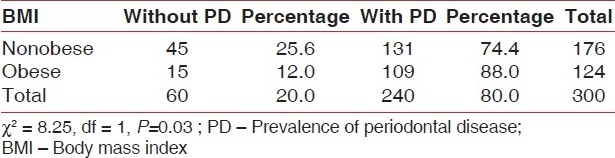
Prevalence of periodontal disease according to BMI
When evaluation was done for prevalence of periodontal disease according to BMI in obese and non-obese, the prevalence of periodontal disease was significantly (P=0.03) more in obese (88%) then in nonobese (74.4%) individuals. [OR = -20.4 and 95% confidence interval (CI) 1.3-1.3] [Table 5].
Table 5.
Prevalence of periodontal disease according to body mass index
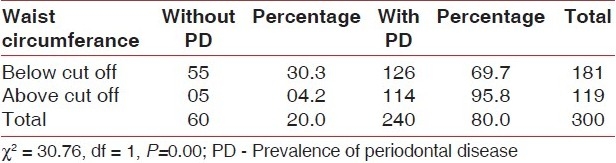
Prevalence of periodontal disease according to WC
According to WC, the prevalence of periodontal disease was significantly higher in above cut-off group compared to below cut-off group. [OR = 2.13 and 95% confidence interval (CL) 1.3 to 5.3] [Table 6].
Table 6.
Prevalence of periodontal disease according to waist circumference
DISCUSSION
Besides being a risk factor for cardio-vascular disease, certain cancers and type II diabetes, obesity has been suggested to be a risk factor for periodontitis. Currently the mechanism of obesity affecting the periodontium is poorly understood, but what is known is that obesity has several harmful biological effect that might be related to pathogenesis of periodontitis. According to current knowledge, the adverse effect of obesity on the periodontium might be mediated through impaired glucose tolerance, dyslipidaemia or through increased levels of various bioactive substances secreted by the adipose tissues.[3]
Tumor necrosis factor-α mediates the endotoxin induced injury in various organs and periodontal tissues. Recently, adipose tissue was shown to secrete TNF- α which causes liver injury in obese rodents. Moreover, TNF- α from adipose tissue was reported to be directly associated with insulin resistance.[3]
Overweight and obesity as assessed by BMI using WHO criteria were evaluated as risk indicators for periodontal disease (Vichea et al.). Findings in a recent 3rd National Health and Nutrition Examination Survey in USA (US NHANES III) suggested that obesity is significantly associated with periodontitis.[1,4]
No-one is immune to obesity, but those with a family history of obesity, or those who have in the past lost weight, are particularly liable to excessive weight gain. According to Garrow et al.;[8] there is no useful way of identifying that portion of the population which is at particularly high risk of obesity so that preventive measures can be focused on that subgroup. Prevention of obesity therefore requires early detection and treatment of excessive weight gain. The most difficult problem in preventing adult obesity is to ensure that excess weight which has been lost is not regained.
A recent study by Brownell et al.,[9] points to the fact that record levels of obesity in children and adolescents are predictable in light of powerful conditions that promote high consumption of calorie-dense, nutrient-poor foods and discourage physical activity. They list five issues as examples: framing of the obesity issue, treating versus preventing obesity, nutrition in schools, marketing and addressing weight bias and discrimination. By adopting a public health approach that addresses the conditions causing obesity, there is hope of reversing troubling trends in prevalence. The current obesity epidemic is fuelled by the availability of highly palatable, calorie-dense food, and the low requirement for physical activity in our modern environment.[10] Center for Disease Control and Health assesses the benefits of physical activity and good nutrition on chronic disease.[11]
Recently Rimm et al.,[12] has shown that the location of body fat is not only associated with morbidity but that this relationship is independent of the total amount of adipose tissue and adipocyte size, location and metabolism are related to fat distribution. Their study of 44,820 women presented easy to read graphs, derived from the multiple logistic model, which will permit practicing physicians to estimate visually the combined risks associated with relative weight and body fat location. Also; the location of body fat has been used to delineate three body types:
Gynoid (pear shape)
Intermediate, and
Android (apple shape)
Rimm et al. used waist girth divided by hip girth for scaling body shape (WHR) and found that it is associated with morbidity after adjustment for relative weight. The use of relative weight and body shape simultaneously gives a better estimate of risk of morbidity than either alone. Another study by Egger et al.,[13] provided a rationale for using waist: Hip ratio (WHR) measurements in clinical practice. Abdominal fat measured by a WHR may be a better single predictor of many diseases. The association between WHR and risk indicators appeared to be “dose” related, and independent of sex, race and age. High WHRs, however, were more characteristic of men with lower socioeconomic status, whereas weight control programs were more commonly developed for women. A reorientation of weight control initiatives based on health rather than aesthetic priorities was proposed and measurement of WHR is advised to be a routine part of clinical assessments. Predictability of WHR measure was seen to be improved by combining it with a measure of body mass.
The study samples were stratified in three age groups (younger age, middle and older age) and the main focus of the study was to evaluate the correlation of BMI and WC with periodontal disease along with role of other confounding factors like age, gender, oral hygiene status, etc.
Although, there are several methods to assess obesity, BMI is commonest of all. However, BMI is a determinant of overweight but does not truly reflect the body fat as it takes height into consideration which confounds the assessment of total body fat.[5]
In our study, we utilized WC to be the determinant of obesity which measured the abdominal obesity. Upper body obesity (abdominal adiposity) is believed to have greater ill-effects on general health than the lower body obesity.[3]
In the present study, the prevalence of periodontal disease was higher in obese subjects (88%) when compared to nonobese subjects (74.4%).This result was in agreement with the studies published by AI-Zahrani et al.
Obesity was significantly associated with the prevalence of periodontal disease in all the three age groups (young, middle-age and old). This finding is not in agreement with the study conducted by AI-Zaharni et al., who found a significant association between measures of body fat and periodontal disease among younger adults, but not in middle age and older adults.
WC above cut-off (95.8%) was associated significantly with the higher prevalence of periodontal disease compared to below cut-off group (69.7%). This finding is consistent with the study conducted by Al-Zahrani et al.
In the present study prevalence of periodontal disease was lower in males (66.9%) as compared to females (97.7%) and this finding is not consistent with previously reported gender differences.
The prevalence of periodontal disease was significantly higher in poor oral hygiene group compared to good oral hygiene group. This finding is consistent with previously reported differences with oral hygiene by Al-Zahrani et al.
Proinflammatory cytokines may play a crucial role in the close relationship among periodontitis, obesity and chronic disease. In fact association may be multidirectional as described in Figure 1.[14]
Figure 1.
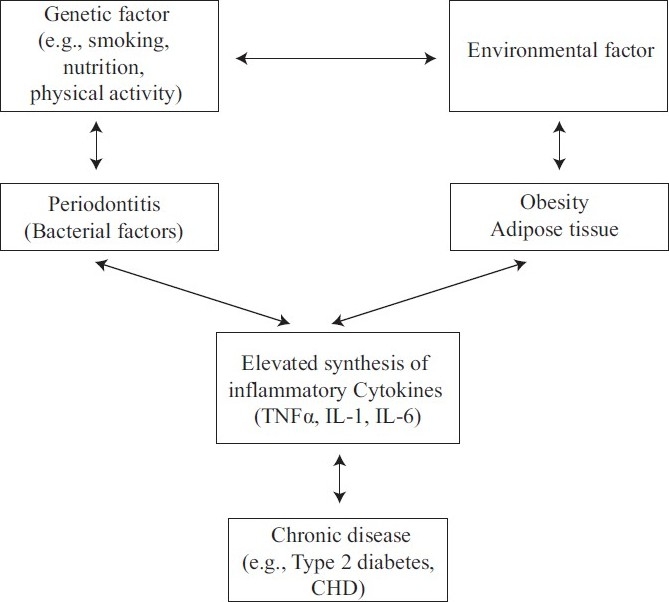
Multidirectional relationship
At the cellular level adipocytes appear to secrete proinflammatory cytokines which may be the molecules linking pathogenesis of periodontal infection. BMI of a person is positively related to severity of periodontal attachment loss and a high level of TNF-α and its soluble receptors (sTNF-α) were found in those individuals with the highest BMI. Hence a positive correlation of TNF-α levels with periodontal disease together with high plasma level of TNF-α and its soluble receptors, which in turn may lead to hyperinflammatory state increasing the risk of periodontal disease, was found in obese patients thereby proving a significant relation between obesity and periodontitis.
CONCLUSIONS
Obesity is one of the major health concerns in both developed and developing countries. It has been implicated as a significant risk factor for several systemic conditions like diabetes, cardiovascular diseases, hypertension, stroke and osteoarthritis.
Because adipose tissue secretes proinflammatory cytokines and tumor necrosis factor (Baumann and Gauldie 1994), it means that obesity could also be a potential cofounder in the association between periodontitis and pro-inflammatory mediators. Tumor necrosis factor-a mediates the endotoxins induced injury in various organs as well as periodontal tissue and may mediate periodontal destruction.
Within the scope and limitations of this study, the following observations were made:
The prevalence of periodontal disease was significantly (P=0.003) higher in patients in obese category (88.0%) compared to patients in nonobese category (74.4%)
Among subjects with WC above cut-off, 95.8% were affected by periodontal disease compared to 69.7% of total subjects with WC below cut-off. WC above cut-off was significantly associated with periodontal disease (P=0.000)
The prevalence of periodontitis was significantly higher in females, in old age and in those with poor oral hygiene.
Although the relationship between obesity and periodontitis needs further investigation, periodontist should counsel obese persons regarding the possible oral complications of obesity, to diminish morbidity for these individuals. Weight screening should be an integral part of periodontal risk assessment on regular basis. This will reduce the patient's risk of developing chronic diseases including periodontitis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Al-zaharani MS, Bissada NF, Borawskit EA. Obesity and periodontal disease in young, middle aged and older adults. J Periodontal. 2003;74:610–5. doi: 10.1902/jop.2003.74.5.610. [DOI] [PubMed] [Google Scholar]
- 2.Soben Peter. 3rd ed. New Delhi: Arya Publishing house; 2004. Indices in dental epidemiology. Essentials of preventive and community dentistry; pp. 123–231. [Google Scholar]
- 3.Saito T, Shimazaki Y, Koga T, Tsuzuki M, Ohshima A. Relationship between upper body obesity and periodontitis. J Dent Res. 2001;80:1631–6. doi: 10.1177/00220345010800070701. [DOI] [PubMed] [Google Scholar]
- 4.Wood N, Johonson RB, Stereckfus CF. Comparision of body composition and periodontal disease using nutritional assessment technique: Third national health and nutritional examination survey(NHANES III) J Clin Periodontol. 2003;30:321–7. doi: 10.1034/j.1600-051x.2003.00353.x. [DOI] [PubMed] [Google Scholar]
- 5.Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635–43. doi: 10.1038/35007508. [DOI] [PubMed] [Google Scholar]
- 6.Karels, Cooper A. Obesity and its role in oral health. Internet J Health Sci Pract. 2007;7:1–5. [Google Scholar]
- 7.Linden G, Patterson C, Evans A, Kee F. Obesity and periodontitis in 60-70 year old men. J Clin Periodontol. 2007;34:461–6. doi: 10.1111/j.1600-051X.2007.01075.x. [DOI] [PubMed] [Google Scholar]
- 8.Garrow J. S. Is it possible to prevent obesity? Infusionstherapie. 1990;17:28–31. doi: 10.1159/000222437. [DOI] [PubMed] [Google Scholar]
- 9.Brownell KD, Schwartz MB, Puhl RM, Henderson KE, Harris JL. The need for bold action to prevent adolescent obesity. J Adolesc Health. 2009;45(3 Suppl):8–17. doi: 10.1016/j.jadohealth.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Chaudhri OB, Wynne K, Bloom SR. Can gut hormones control appetite and prevent obesity. Diabetes Care. 2008;31(Suppl 2):284–9. doi: 10.2337/dc08-s269. [DOI] [PubMed] [Google Scholar]
- 11.Physical activity and good nutrition: Essential elements to prevent chronic diseases and obesity 2003. Nutr Clin Care. 2003;6:135–8. [PubMed] [Google Scholar]
- 12.Rimm AA, Hartz AJ, Fischer ME. A weight shape index for assessing risk of disease in 44,820 women. J Clin Epidemiol. 1988;41:459–65. doi: 10.1016/0895-4356(88)90047-9. [DOI] [PubMed] [Google Scholar]
- 13.Egger G. The case for using waist to hip ratio measurements in routine medical checks. Med J Aust. 1992;156:280–5. doi: 10.5694/j.1326-5377.1992.tb139751.x. [DOI] [PubMed] [Google Scholar]
- 14.Pischon N, Heng N, Bernimoulin JP, Kleber BM, Willich SN, Pischon T. Obesity, inflammation, and periodontal disease. J Dent Res. 2007;86:400–9. doi: 10.1177/154405910708600503. [DOI] [PubMed] [Google Scholar]


