Abstract
Odontogenic tumors mainly occur as intraosseous growths but sometimes may present in a peripheral location on the gingiva where they are referred to as peripheral odontogenic tumors (POTs) which are a rare entity, the most common of them being the peripheral odontogenic fibroma that is an otherwise uncommon, slowly growing, benign odontogenic neoplasm of the periodontal soft tissues. In fact, peripheral odontogenic fibroma is the only POT that is more frequent than its central counterpart. Although considered to be with a potential to recur after excision, the actual recurrence rate is not known due to paucity of literature. This paper presents a case report along with review of the available literature and reinforces the importance of patient follow-up in addition to radiographic and histological examination of seemingly innocuous gingival exophytic lesions.
Keywords: Localized gingival enlargement, peripheral odontogenic fibroma, odontogenic tumors
INTRODUCTION
The odontogenic fibroma is a benign neoplasm of odontogenic ectomesenchymal origin, characterized by relatively mature collagenous fibrous tissue with varying amount of odontogenic epithelium. It can occur in central or peripheral location, the latter being more common by a 1.4:1 ratio.[1] A slight female predominance has been seen in a literature review by Daley et al.[2] Age at diagnosis varies widely with a peak in the third and fourth decades of life.[1,2]
The World Health Organization (WHO) defined[3] it as “a benign odontogenic neoplasm of fibroblastic origin characterized by relatively mature collagenous fibrous tissue and varying amounts of odontogenic epithelium with potential to occur in either a central or an extraosseous location. The extraosseous counterpart is designated as peripheral odontogenic fibroma”.
It appears as a firm, slow-growing and usually sessile gingival mass covered by normal appearing mucosa.[4] Clinically, it cannot be distinguished from common fibrous gingival lesions. Encountered mainly on facial gingiva of mandible, with incisor-canine and premolar area being the most common sites, they seldom cause displacement of teeth. Rarely, multifocal or diffuse lesions have also been described.[5]
The lesion is generally elevated and nonulcerated clinically and nonencapsulated microscopically. The histologic spectrum of this lesion is wide. Connective tissue ranges from loose (almost myxomatous) to markedly cellular or to relatively acellular and well organized.[4] Islands/strands of odontogenic epithelium are scattered throughout connective tissue, which may be prominent/scarce. Dysplastic dentin, amorphous ovoid cementum like calcifications and trabeculae of osteoid may also be present. The peripheral odontogenic fibroma shows histopathologic features similar to those of the central odontogenic fibroma (WHO) type.[5]
Review
In the past, some authors had designated clinically and histopathologically lesions similar to peripheral odontogenic fibroma as odontogenic gingival epithelial hamartoma[6]/peripheral fibroblastic dentinoma,[7] odontogenic epithelial hamartoma.[8] The reason for it being referred to as odontogenic gingival epithelial hamartoma[6] in the past is a reflection of the authors placing more emphasis on the epithelial component rather than the fibroblastic component. It does not appear to be a hamartoma because hamartomas are developmental,[9] while in this particular study by Baden,[5] lesions reported as hamartomas appeared only in sixth and seventh decades of life rather than during the development of dentition, which means that they were not hamartomas.
At one time, the terms peripheral ossifying fibroma and peripheral odontogenic fibroma were used quite interchangeably till Gardener[9] published a clarification in terminology. While the former one is a commonly found reactive lesion with well-formed bone, numerous giant cells and only rarely, if present, odontogenic epithelial rests, the latter one, which is quite rare, has extensive odontogenic epithelium with occasionally found dysplastic dentin/cementum like calcifications and only rarely, giant cells are present. The origin of both the lesions is quite different and so is the biologic behavior. The former is a benign tumor of connective tissue origin with a marked tendency to recur, while the latter is of odontogenic mesenchymal origin whose recurrence is not known exactly but is reported to vary from very low to as high as 38.9%.[2,9,10]
Buchner et al.[4] presented nine cases of peripheral odontogenic fibroma that illustrate the variety of its histopathologic findings. They also suggested that the term ‘WHO type’ to be used to distinguish it from peripheral ossifying fibroma.
The first detailed clinicopathologic study of peripheral odontogenic fibroma was published by Daley et al.[2] Clinical data from this study indicate that the lesion is more common than reported previously and also that it has a significant recurrence rate.
Another study by Buchner[1] presents the relative frequency of peripheral odontogenic tumors (POTs), in which it was found that peripheral odontogenic fibroma accounted for 51.1% of the total POTs. However, POTs themselves are quite rare, consisting of only 0.05%[1] of all oral biopsy specimens.
Being a rare lesion itself, the literature mostly consists of case reports[3,10–13] of rarer forms or presentations of the same lesion which consist of diffuse, multifocal type[11] and diffuse associated with ocular, skin lesions.[3] Histologic subtypes include granular cell variant[13] and squamous variant.[8]
CASE REPORT
A 30-year-old female presented in the Department of Periodontics, SRCDSR, with a localized gingival swelling in relation to interdental gingiva of mandibular left canine-first premolar region [Figure 1]. It was present since 1 year and had slowly grown to this size, causing displacement of both the teeth and creating a space between them. Patient gave a vague history of presence of similar growth in the same region around 11 years back which she got excised in a government hospital, but no records could be obtained regarding that either from the patient or from the hospital. On examination, the swelling was approximately 0.8 × 1 cm in size [Figure 2], was found to be sessile, nonlobulated, sharply demarcated but otherwise of the same color as the surrounding mucosa. On palpation, it had a fibrotic consistency. Complete full mouth periodontal examination revealed the presence of generalized 3-4 mm deep pockets and subgingival flecks or complete bands of calculus. Patient had a very poor oral hygiene. A clinical diagnosis of generalized mild to moderate chronic periodontitis with focal fibrous hyperplasia/irritation fibroma was made. IOPA Intra oral periapical radiograph (IOPA) of the involved area was taken which revealed a horizontal bone loss [Figure 3]. Excisional biopsy was done along with open flap debridement as the patient was suffering from periodontitis. The growth was removed with an internal bevel incision and root surface was scaled and planed thoroughly. Periodontal pack was placed and the patient was recalled after 7 days for pack and suture removal. At follow-up, the area seemed to heal well. The patient is getting treated for periodontitis now and will remain on a regular follow-up of 3 months in the future. A 5-week follow-up photograph has been shown [Figure 4].
Figure 1.

Pre-operative photograph
Figure 2.

Mesiodistal length of excised lesion
Figure 3.
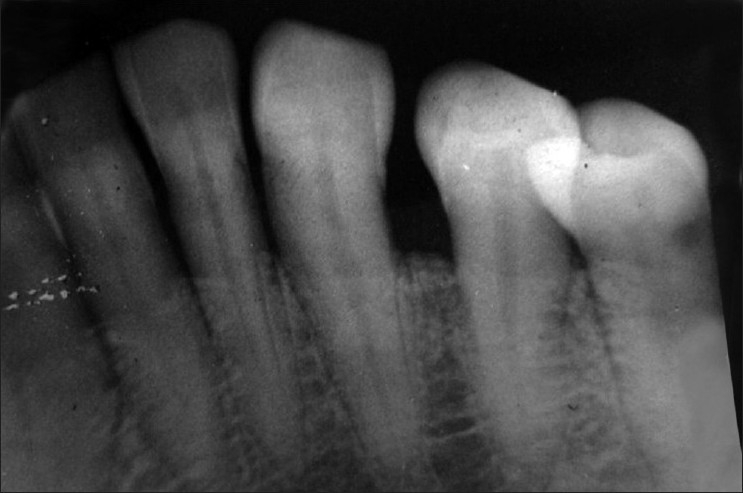
Radiograph of the area
Figure 4.

Post-operative photograph (5-week follow-up)
Microscopically, the lesion showed partially circumscribed tumor mass exhibiting interlacing fascicles of collagen fibers and scattered abundant odontogenic nests and strands [Figure 5]. Intervening connective tissue also consisted of numerous localized areas of chronic inflammatory cells (mainly plasma cells) and few multinucleated giant cells. The overlying epithelium was hyperplastic, parakeratinized stratified squamous epithelium with thin, long rete ridges.
Figure 5.
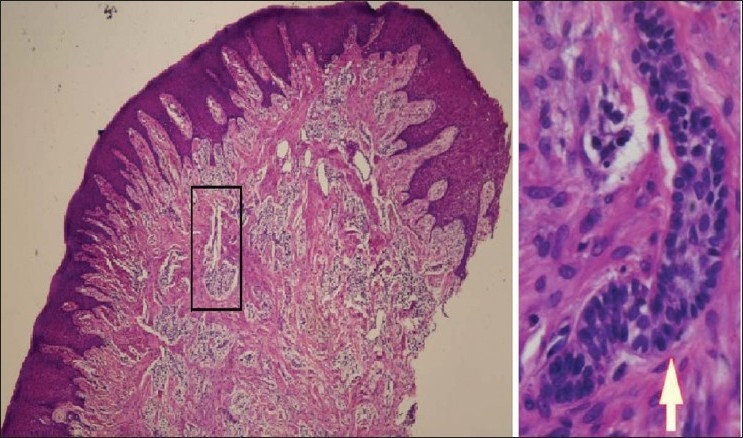
Photomicrograph(×4) of H & E stained section. Inset shows odontogenic epithelial cord (×40)
DISCUSSION
The peripheral odontogenic fibroma is treated by local excision and prognosis is excellent. The differential diagnosis includes inflammatory lesions such as fibrous hyperplasia, fibroma, giant cell fibroma, peripheral ossifying fibroma, POTs, peripheral giant cell granuloma, and pyogenic granuloma.
Peripheral odontogenic fibroma does not involve the underlying bone and only sometimes shows areas of calcification on radiograph.[5] This was not true in our case. The lesion itself showed no calcification, while the reason for interdental bone loss is periodontitis since it is generalized.
Recurrence[2,12] has been documented, so follow-up is mandatory. Armas et al.[12] have published a case report of recurrence of peripheral odontogenic fibroma three times and the last one occurred not only after a gap of 11 years which is the longest reported time of recurrence, but also presented in association with a central odontogenic fibroma although there were no radiographic findings the first two times. This would emphasize the importance of radiographic investigation and follow-up of such type of cases.
Tooth displacement, which is generally not caused by this lesion, was present in this case most likely because of the presence of generalized periodontitis that makes the tooth amenable to pathologic migration. Due to the nonavailability of previous records, we cannot say whether it is a recurrence of the same lesion after a long period of 11 years or another independent lesion. The literature[9] also indicates the presence of another pathological entity, namely fibrous hyperplasia exhibiting odontogenic rests, which was eliminated from differential diagnosis on the basis that the epithelium found in our specimen was actually large in amount as seen in the photomicrograph.
It is further stressed that as far as the excisional part is concerned, mucogingival problem is not created unless and until the attached gingiva is involved, which is not quite usual, or rather it has not been commented upon except in one of the case reports.[10] However, if it is involved, grafting procedures can be done. In our case, attached gingiva was not involved.
To conclude, we stress upon the radiographic and histopathologic investigation of all gingival growths in addition to regular follow-ups of all such patients.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Buchner A, Merrell PW, Carpenter WM. Relative frequency of central odontogenic tumours: A study of 1088 cases from northern California and comparison to studies from other parts of the world. J Oral Maxillofac Surg. 2006;64:1343–52. doi: 10.1016/j.joms.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 2.Daley TD, Wysocki GP. Peripheral odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1994;78:329–36. doi: 10.1016/0030-4220(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 3.Weber A, van Heerden WFP, Ligthelm AJ, Raubenheimer EJ. Diffuse peripheral odontogenic fibroma: Report of 3 cases. J Oral Pathol Med. 1992;21:82–4. doi: 10.1111/j.1600-0714.1992.tb00984.x. [DOI] [PubMed] [Google Scholar]
- 4.Buchner A, Ficarra G, Hansen LS. Peripheral odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1987;64:432–8. doi: 10.1016/0030-4220(87)90148-4. [DOI] [PubMed] [Google Scholar]
- 5.Neville BW, Damm DD, Allen CM, Bouquot JE. 3rd ed. Philadelphia: WB Saunders; 2009. Oral and maxillofacial pathology; pp. 729–9. [Google Scholar]
- 6.Baden E, Moskow BS, Moskow R. Odontogenic gingival epithelial hamartoma. J Oral Surg. 1968;26:702–14. [PubMed] [Google Scholar]
- 7.Mckelvy BD, Cherrick HM. Peripheral ameloblastic fibrodentinoma. J Oral surg. 1976;34:826–9. [PubMed] [Google Scholar]
- 8.Scuibba JJ, Zola MB. Odontogenic epithelial hamartoma. Oral Surg Oral Med Oral Pathol. 1978;45:261–5. doi: 10.1016/0030-4220(78)90093-2. [DOI] [PubMed] [Google Scholar]
- 9.Gardner DG. The peripheral odontogenic fibroma: An attempt at clarification. Oral Surg Oral Med Pathol. 1982;54:40–8. doi: 10.1016/0030-4220(82)90415-7. [DOI] [PubMed] [Google Scholar]
- 10.Michaelides PL. Recurrent peripheral odontogenic fibroma of attached gingiva: A case report. J Periodontol. 1992;63:645–7. doi: 10.1902/jop.1992.63.7.645. [DOI] [PubMed] [Google Scholar]
- 11.Kamal R, Palaskar S, Shetty VP, Bhushan A. Multifocal peripheral odontogenic fibroma. J Oral Maxillofac Pathol. 2008;12:72–4. [Google Scholar]
- 12.Armas JM, Hunter KD, Jenkins W. Odontogenic fibroma: An unusual presentation. J Oral Maxilloial Pathol. 2008;12:68–71. [Google Scholar]
- 13.Lownie JF, Altini M, Shear M. Granular cell peripheral odontogenic fibroma. J Oral Pathol Med. 1976;5:295–304. doi: 10.1111/j.1600-0714.1976.tb01778.x. [DOI] [PubMed] [Google Scholar]


