Abstract
It is essential for a dental surgeon or a periodontist to detect blood glucose level for patients whose signs and symptoms are suggestive of diabetes. Seventy patients in the age group of 40 to 80 years of either sex were selected for the study. The study population included patients with type 1 or type 2 diabetes mellitus. Venous blood was used as a control group, whereas gingival blood and finger-prick blood constituted the study groups I and II, respectively. The percentage deviations of gingival blood glucose level measurements and finger-prick blood glucose level measurements from the standard venous blood glucose level measurements were recorded, which showed that 72.86% of gingival and 68.57% of finger-prick blood glucose level measurements were found to be within ±15% of the standard venous blood glucose level measurements. All values exhibited significant correlations among each other, but correlations between glucose values obtained using venous and gingival blood samples were higher than the correlations between glucose values obtained using venous and finger-prick blood samples.
Keywords: Alternative site testing, diabetes mellitus, glucometer
INTRODUCTION
The periodontist frequently manages diabetic patients using limited information about their blood glucose control. Often, the only information available is from a single laboratory test, which may not reflect their current blood glucose status and diabetologists’ opinions taken earlier. Moreover, even more important is “at that moment” blood glucose level.
This study was undertaken to establish a dentist's role in managing patients with established diabetes mellitus and also in screening patients with undiagnosed diabetes based on their oral clinical manifestations.
This method of analysis was selected because dentists seemingly would be more secure in obtaining blood samples from the gingival tissues than in using venous blood-collection method.
MATERIALS AND METHODS
Seventy patients in the age group of 40 to 80 years of either sex were selected for the study. The study population included patients with type 1 or type 2 diabetes mellitus. Venous blood was used as a control group, whereas gingival blood and finger-prick blood constituted the study groups I and II, respectively. Inclusion criteria (both groups) included patients of either sex, being in the age group 40 to 80 years, and having at least one lower anterior tooth that bled upon probing.[1] Exclusion criteria (both groups) included use of supplemental ascorbic acid (vitamin C)[1] and as in sub acute bacterial endocarditis.[1]
For gingival blood sampling, the most inflamed site in the lower anterior region [Figure 1] was selected and isolated with cotton rolls; Lignocaine gel (2%) was applied. After 1 minute, the gel was wiped off and the selected site was freshly isolated with cotton rolls. The outer surface of the gingiva was pricked with a sterile lancet. Approximately 10 μL of blood was collected using hemoglobin pipette [Figure 2]. The blood was transferred onto a slide. The commercially available strip (placed in the g lucometer) was touched onto this blood drop on the slide and analyzed using a glucometer. After 15 seconds, the reading was obtained for finger-prick blood: the pulp of the fingertip was pricked with a sterile lancet, and a drop of blood was placed on a commercially available glucose oxidase test strip in the self-monitoring device. After 15 seconds, the reading was obtained and recorded [Figures 3 and 4].
Figure 1.

Clinical examination
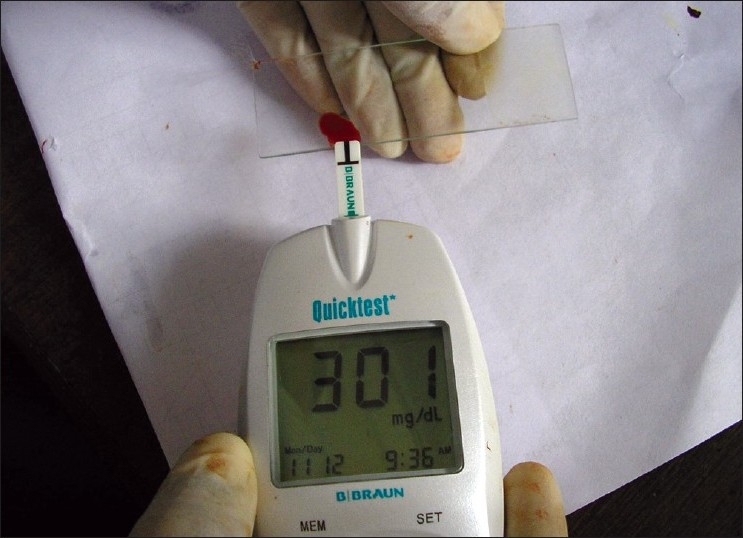
Figure 2.

Gingival blood sampling
Figure 3.
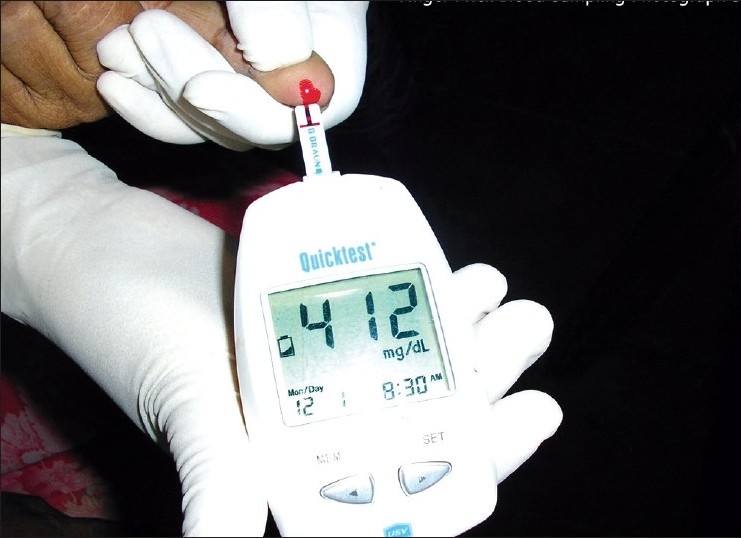
Finger-prick blood sampling
Figure 4.
Glucometer
For venous blood sampling,[1] approximately 1 mL of routine venous blood was drawn from the patient's cubital fosse and analyzed by glucose oxidase method [Figure 5].
Figure 5.

Venous blood sampling
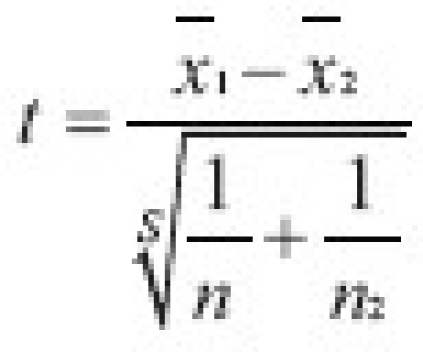
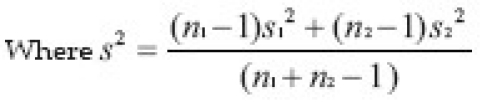
Statistical analysis
RESULTS
The percentage deviations of gingival blood glucose level measurements and finger-prick blood glucose level measurements from the standard venous blood glucose level measurements were recorded, which showed that 72.86% of gingival and 68.57% of finger-prick blood glucose level measurements were found to be within 15% of the standard venous blood glucose level measurements.
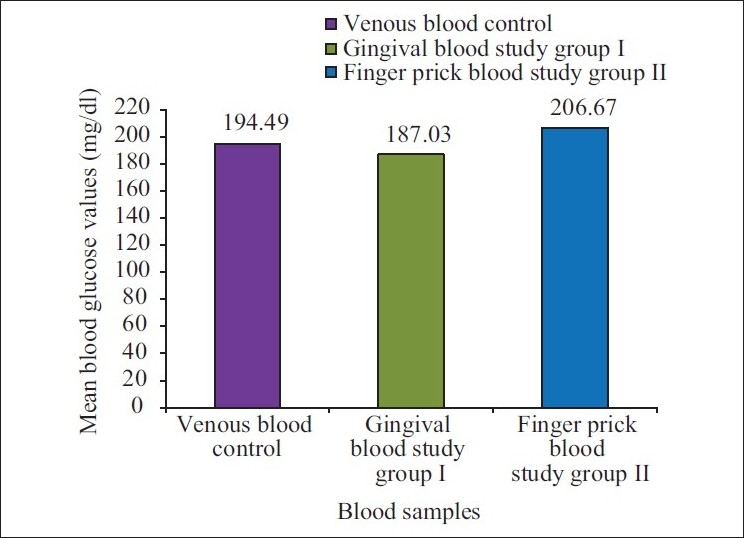
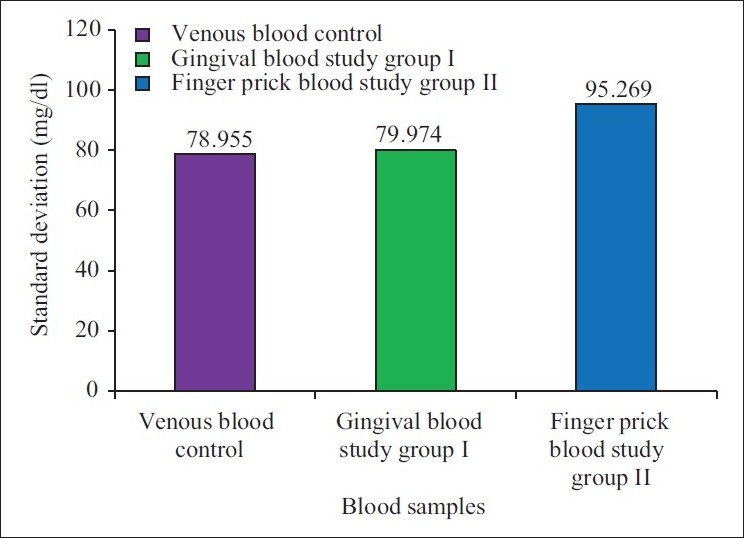
Table 1, Figures 6 and 7 show means and standard deviations of venous, gingival and finger-prick blood glucose level measurements, of which mean and standard deviation of finger-prick blood glucose level measurements were the highest, being 206.67 mg/dL and 95.269 mg/dL, respectively, which indicates that deviations of finger-prick blood glucose level measurements are more than those of gingival blood glucose level measurements when both are compared with venous blood glucose level measurements.
Table 1.
Means and standard deviations of venous, gingival and finger-prick blood glucose level measurements
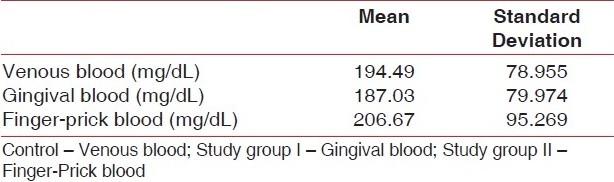
Figure 6.
Mean values of glucose level measurements using venous,gingival and finger-prick blood samples
Figure 7.
Standard deviations of venous, gingival and finger-prickblood glucose level measurements
Figure 8 shows Overlay scatter diagram showing correlations between venous, gingival and finger-prick blood glucose level measurements.
Figure 8.
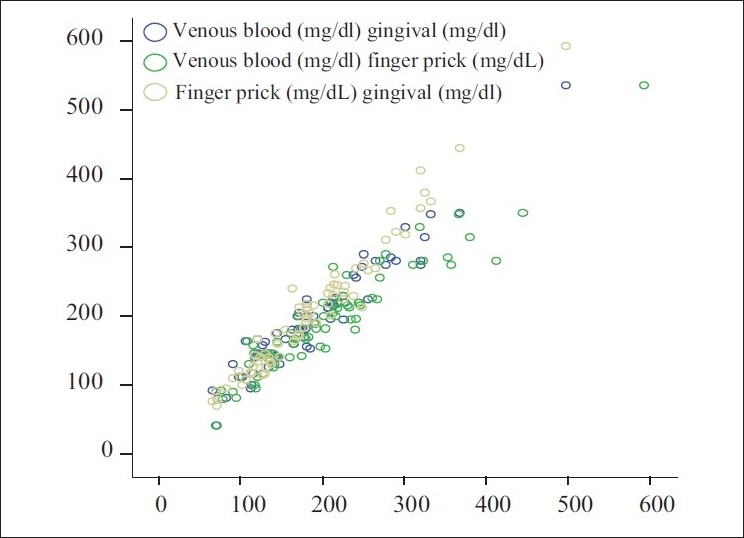
Overlay scatter diagram showing correlations between venous,gingival and finger-prick blood glucose level measurements
DISCUSSION
The term alternative site testing (AST) means the parts of the body other than the fingertips to obtain blood for glucose level testing.[2] This present study uses gingiva as an alternative site. Gingival wound healing is definitely better than finger-prick healing due to the following reasons:
-
a)
Abundant vascular supply to gingiva
-
(b)
High expression of tissue plasminogen activator in gingival fibroblasts. It has been shown that urokinase-type plasminogen activator receptor is able to associate with integrins
-
c)
Unlike skin fibroblasts, adult gingival fibroblasts located in the papillary connective tissue share many properties with fetal fibroblasts, including their growth and response to, cytokines
-
d)
Saliva also helps in healing due to moist environment and salivary factors.
The procedure of determining blood glucose level using glucometer is relatively simple, inexpensive, fast and sufficiently accurate. Acute stress such as that occurring during a dental visit stimulates the sympathetic splanchnic nerves that induce the release of large amount of catecholamine (primarily epinephrine) from the adrenal medulla. Catecholamine release due to stress thus becomes a major counter-regulatory mechanism to the exogenous insulin taken by a diabetic patient. This causes blood glucose level to increase in a patient with stress.[3,4] Depending on the patient's medical history, medication and procedure to be performed, the dentist may need to measure blood glucose level before beginning the procedure. Moreover, in the midst of surgery, blood from surgical site can be used to detect blood glucose level, which avoids a painful prick at the second site. One of the most important reasons also is that dentists feel more secure in collecting blood from gingiva because oral cavity is a dentist's domain, unlike other parts of the body used in conventional blood sampling.[5]
Over and above the glycemic status of the patient in general, local blood glucose concentration in the surgical area is also important as it may affect the outcome of the treatment. The diabetic gingiva is unable to utilize oxygen and thus cannot oxidize glucose as readily (Campbell, 1970).
In this study, 2% Lignocaine jelly was used as a topical anesthetic and was applied 1 minute prior to gingival prick. This makes the gingival prick almost painless. Finger prick produces trauma to fingers, as well as subjective symptoms of pain invariably.
Fingertips are full of nerve endings (receptors) which make finger prick very painful. Gingival blood sampling may be more comfortable in patients because of local anesthesia application.
Quick results are obtained with glucometer; the result may be displayed within 15 to 90 seconds (American Diabetes Association). Because of the quick recordings obtained, glucometer can be used as an educational tool for the patient for easy and quick chair-side counseling.
The main controversial issue is the reliability of glucometer, as they may show large deviations. Future research with larger sample size should be done.
ACKNOWLEDGMENT
I thank Dr. P. K. Saraswathi, M.D.S., and Dr. K. H. Panishankar, M.D.S., Additional Professors, Department of Periodontics, Tamil Nadu Government Dental College and Hospital, Chennai, without whose support this study would not have been possible.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Parker RC, Rapley JW, Isley W, Spencer P, Killoy WJ. Gingival crevicular blood for assessment of blood glucose in diabetic patients. J Periodontol. 1993;64:666–72. doi: 10.1902/jop.1993.64.7.666. [DOI] [PubMed] [Google Scholar]
- 2.Stein GM, Nebbia AA. A chairside method of diabetic screening with gingival blood. Oral Surg Oral Med Oral Pathol. 1969;27:607–12. doi: 10.1016/0030-4220(69)90092-9. [DOI] [PubMed] [Google Scholar]
- 3.Nonogaki K. New insight into the sympathetic regulation of glucose and fat metabolism. Diabetologia. 2000;43:533–49. doi: 10.1007/s001250051341. [DOI] [PubMed] [Google Scholar]
- 4.Berk MA, Clutter WE. Enhanced glycogenic responsiveness to epinephrine in insulin dependent diabetes mellitus is the result of inability to secrete insulin. J Clinical Invest. 1995;75:1842–51. doi: 10.1172/JCI111898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kohad RM, Shetty S. Gingival blood glucose estimation by haemoglucotest reagent strips. A potential chair side screening for diabetes. J Indian Soc Periodontol. 2004;7(2):109–14. [Google Scholar]


