Abstract
Purpose:
To assess the knowledge of obstetricians about concerns of women with epilepsy.
Materials and Methods:
We surveyed 97 obstetricians (teaching hospitals—43, private hospitals—32, and community health centers–21) using knowledge of women's issues and epilepsy (KOWIE) questionnaire II with additional questions.
Results:
The mean duration of practice of the surveyed obstetricians was 12.4 ± 10.7 years and 94% were female doctors. Most of them were well informed about the teratogenic effects of AEDs (91%), need to continue antiepileptic drugs (AEDs) during pregnancy (95%), and the role of folic acid and vitamin K during pregnancy (95%). They agreed AEDs decrease the efficacy of oral contraception and it was safe for the woman to breast-feed the baby while on AEDs. Only 1/3rd of them knew that steroid hormones could alter seizure threshold or that AEDs could predispose to osteomalacia. Fewer doctors knew that WWE could have increased sexual dysfunction (29.9%) or infertility (26.8%). The knowledge did not vary according to years of practice or practice settings.
Conclusions:
Obstetricians were well informed about the fetal complications of antenatal AED exposure, but were under informed of other complications such as osteomalacia, sexual dysfunction, and infertility.
Keywords: Knowledge, obstetricians, survey, women with epilepsy
Introduction
Women with epilepsy (WWE) face many gender-related issues. This is because of the effect of epilepsy and antiepileptic drugs (AEDs) on fertility, contraception, pregnancy, breast-feeding, and fetus.[1–3] The American Academy of Neurology and the American College of Obstetricians and Gynecologists issued practice parameters on various medical issues of WWE.[4–6] The various studies published in last two decades have consistently demonstrated a substantial lack of knowledge by both health professionals and patients in the areas of health of WWE.[7–10] In a study conducted by the American Epilepsy Foundation, out of a total of around 3500 participants, only 5% of health care providers could correctly answer two-thirds of the questions on various issues of WWE.[7] Empathetic consideration, patient counseling especially in the prepregnancy period, diagnostic watchfulness, and the use of supplemental medications can successfully overcome the challenges in most cases.[10,11] As is evident, the deficiency of quality care and the lacunae of awareness among health care providers go hand in hand.
The majority of studies done so far to assess the knowledge and awareness of health care workers included a heterogeneous population.[7,11,12] Obstetricians significantly contribute as one of the primary care providers for WWE during pregnancy and childbirth. Therefore, we undertook this study to assess the knowledge of obstetricians about the relevant topics and concerns of WWE in Kerala, a state in Southern India. We also aimed to compare the knowledge of obstetricians working in different hospital set-ups.
Materials and Methods
To assess the awareness of issues specific to women with epilepsy, obstetricians attending a local state level conference were asked to complete a questionnaire. The study group consisted of obstetricians working in three different hospital settings, i.e., small community health centers, the private hospitals, and the government teaching institutes. The questionnaire included the knowledge of women's issues and epilepsy (KOWIE) II questionnaire[11] along with additional questions regarding their demography, clinical practice, and AED preferences.
Long et al. developed the KOWIE I and II questionnaires to ascertain what women (KOWIE- I) and healthcare professionals (KOWIE-II) knew about issues pertaining to WWE.[11,13] The items for emphasis for both tools are consistent, and include questions pertaining to the effect of seizures and antiepileptic drugs on oral contraception, bone health, sexual function, hormones, pregnancy, and breast-feeding. The validity and reliability of both tools have been previously established.[13] We took the author's prior permission to use the KOWIE-II questionnaire in our study.
For statistical analysis, the questionnaire was evaluated and scored as zero (incorrect response) or one (correct response) for each question. Mann-Whitney test was used for the univariate analysis, for the comparison of awareness of obstetricians working in different health set-ups and with different years of experiences.
Results
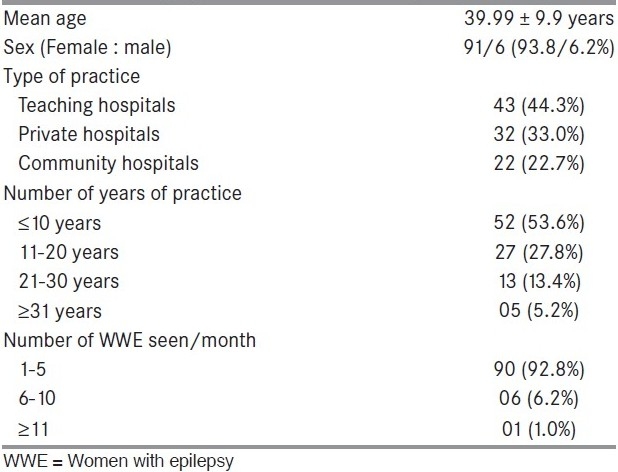
We approached a total of 100 obstetricians (teaching hospitals—46, private hospitals—32, and community health centers—22) using the questionnaire. Three obstetricians from teaching hospital declined to take part. Their demographic data and type of practice are summarized in Table 1. While 93 (96%) of them were interested in treating WWE, majority (80, 82.5%) were treating WWE in cooperation with the neurologist. Most of them were using first line AEDs (carbamazepine-54, phenobarbitone-28, phenytoin-18, sodium valproate-14, and newer AEDs-4) for WWE. According to participants, the highest incidence of congenital anomaly was with valproate (60), followed by phenytoin (32), carbamazepine (6), and phenobarbitone (1).
Table 1.
Demographic details of surveyed obstetricians
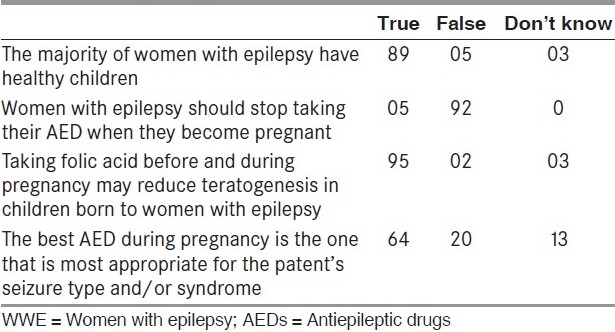
A common knowledge was that the majority of the WWE have healthy children (91%). A significant percentage of obstetricians (n = 95, 97%) considered that teratogenesis could be prevented by using folic acid during pregnancy. WWE were advised to continue AEDs during pregnancy by 92 (95%) doctors. The AED most suited for the seizure type/epilepsy syndrome was considered to be the best during pregnancy by 64 (65.9%) of the obstetricians [Table 2].
Table 2.
Pregnancy related issues in WWE
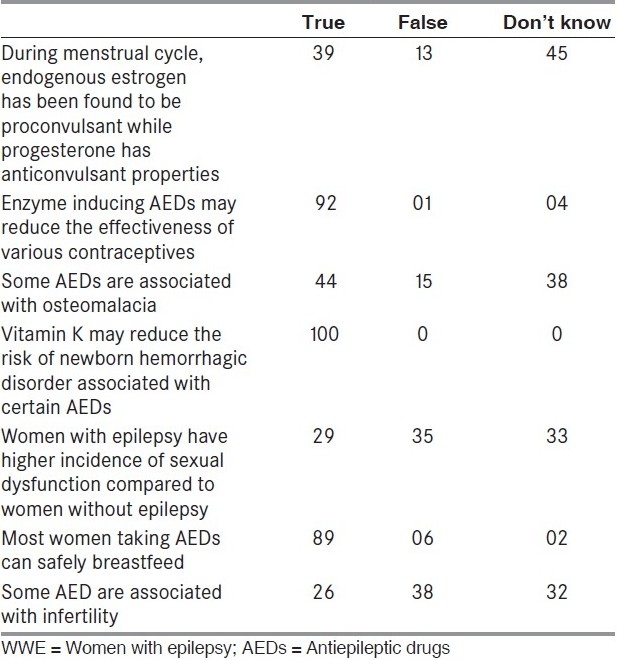
All participants believed that vitamin K may reduce the risk of hemorrhagic disorder in the fetus associated with AED exposure. The reduction of efficacy of oral contraceptive pills on AED usage was understood by 92 (94.8%) of the obstetricians. Similarly, the safety of breast-feeding was widely known (91.7%). Nevertheless, less than 30% of the participants only correctly understood the higher incidence of sexual dysfunction (n = 29) and infertility (n = 26) in WWE. About half of them (n = 44) knew about the association of AEDs and osteomalacia. Around a third of the participants (n = 39) knew that estrogen has a proconvulsant effect whereas progesterone has an anticonvulsant effect [Table 3].
Table 3.
The issues other than pregnancy in WWE
When comparison was made using the scoring system, there was no significant difference between the obstetricians working in the different health set-ups (mean score 7.98 vs 7.67, P = 0.32). Also, no significant difference was found when comparison was made according to years of practice (≤10 years = 7.75 vs ≥11 years = 7.87, P = 0.99).
Discussion
WWE need more attention and special care as compared to men with epilepsy, especially during pregnancy and childbirth. This is the first study from India to survey the knowledge of the obstetricians regarding the issues of WWE. A better awareness among the health care professionals and improved understanding in woman herself and her family members can indeed help to alleviate the anxiety and thus, in turn improve the outcome.
The majority of the findings of the nonobstetric effect of AEDs and epilepsy in WWE were similar to previous studies.[7,11,14] However, the earlier studies included health care providers working in different specialties. The difference was observed in the following three areas: Majority of the participants in our study knew the safety of the breast feeding and usefulness of vitamin K in preventing hemorrhagic diseases in the newborn. In contrast, only 47% and 68% of the health professionals in a study done in USA knew them correctly.[11] A similar study among obstetricians in Scotland observed that 13% of the obstetricians discouraged breast-feeding and 56% of them never gave vitamin K during pregnancy.[10] However, only 44% of the Indian obstetrician knew the relationship between AEDs and osteomalacia as against 77% of the US health professionals. This might be explained by the fact of higher prevalence of osteomalacia related to AEDs exposure in temperate countries compared to tropical countries such as India. In our study, majority knew about the enzyme inducing effect of AEDs on OCPs whereas only 1/4th of the study population including neurologists and gynecologists understood this interaction in a study done in the USA in 1996. Studies have shown that hiking up the dose of OCPs will prevent unplanned pregnancies in WWE in the presence of enzyme inducing AEDs.[4]
There was a good correlation between the awareness on side effects profile of first line AEDs on fetus and their usage in clinical practice among the participants in our study. In a study by Long et al.,[11] there was a better understanding of the issues of WWE with more years of practice. However, on comparing the different working setups and years of experience, significant difference was found among the obstetricians in our study. This could possibly be accounted for by the smaller sample size.
In conclusion, majority of the obstetricians were well informed about the maternal and fetal aspects of WWE, but were relatively under informed of other related issues such as osteomalacia, sexual dysfunction and infertility. A well-planned education in this area to all health care professionals is essential to improve the understanding and care of WWE. It is highly recommended to organize sessions in order to dissipate knowledge about matters concerning WWE. This will not only improve the level of quality care provided by heterogeneous population of obstetricians, rather, will be step towards a good teamwork between the teaching and nonteaching health sectors.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
References
- 1.Zahn CA, Morrell MJ, Collins SD, Labiner DM, Yerby MS. Management issues for women with epilepsy.A review of the literature. Neurology. 1998;51:949–56. doi: 10.1212/wnl.51.4.949. [DOI] [PubMed] [Google Scholar]
- 2.Morrell MJ. Reproductive and metabolic disorders in women with epilepsy. Epilepsia. 2003;44(Suppl 4):11–20. doi: 10.1046/j.1528-1157.44.s4.2.x. [DOI] [PubMed] [Google Scholar]
- 3.Mawer G, Briggs M, Baker GA, Bromley R, Coyle H, Eatock J, et al. Pregnancy with epilepsy: Obstetric and neonatal outcome of a controlled study. Seizure. 2010;9:112–9. doi: 10.1016/j.seizure.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Quality Standards subcommittee of the American Academy of Neurology. Practice parameter: Management issues for women with epilepsy (summary statement) Neurology. 1998;51:944. doi: 10.1212/wnl.51.4.944. [DOI] [PubMed] [Google Scholar]
- 5.Practice Parameter update: Management issues for women with epilepsy—Focus on pregnancy (an evidence-based review): Teratogenesis and perinatal outcomes. Report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology. 2009;73:133–41. doi: 10.1212/WNL.0b013e3181a6b312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Practice Parameter update: Management issues for women with epilepsy—Focus on pregnancy (an evidence-based review): Obstetrical complications and change in seizure frequency. Report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology. 2009;73:126–32. doi: 10.1212/WNL.0b013e3181a6b2f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrell MJ, Sarto GE, Shafer PO, Borda EA, Herzog A, Callanan M. Health issues for women with epilepsy: A descriptive survey to assess knowledge and awareness among health care providers. J Womens Health Gend Based Med. 2000;9:959–65. doi: 10.1089/15246090050199982. [DOI] [PubMed] [Google Scholar]
- 8.Vazquez B, Gibson P, Kustra R. Epilepsy and women's health issues: Unmet needs-survey results from women with epilepsy. Epilepsy Behav. 2007;10:163–9. doi: 10.1016/j.yebeh.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Crawford P, Hudson S. Understanding the information needs of women with epilepsy at different life stages: Results of the ‘Ideal World’ survey. Seizure. 2003;12:502–7. doi: 10.1016/s1059-1311(03)00085-2. [DOI] [PubMed] [Google Scholar]
- 10.Russell AJ, Macpherson H, Cairnie V, Brodie MJ. The care of pregnant women with epilepsy- a survey of obstetricians in Scotland. Seizure. 1996;5:271–7. doi: 10.1016/s1059-1311(96)80020-3. [DOI] [PubMed] [Google Scholar]
- 11.Long L, Montouris G. Knowledge of women's issues and epilepsy (KOWIE-II): A survey of health care professionals. Epilepsy Behav. 2005;6:90–3. doi: 10.1016/j.yebeh.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Krauss GL, Brandt J, Campbell M, Plate C, Summerfield M. Antiepileptic medications and oral contraceptive interactions: A national survey of neurologists and obstetricians. Neurology. 1996;46:1534–9. doi: 10.1212/wnl.46.6.1534. [DOI] [PubMed] [Google Scholar]
- 13.Long L, McAuley JW, Shneker B, Moore JL. The validity and reliability of the knowledge of women's issues and epilepsy (KOWIE) questionnaires I and II. J Neurosci Nurs. 2005;37:88–91. [PubMed] [Google Scholar]
- 14.McAuley JW, Casey J, Long L. An evaluation of pharmacists’ knowledge of women's issues in epilepsy. Epilepsy Behav. 2009;14:243–6. doi: 10.1016/j.yebeh.2008.10.018. [DOI] [PubMed] [Google Scholar]


