Abstract
Introduction: Globally about 8% to 10% of newborns require neonatal intensive care (NICU) care. Families face emotional and financial difficulties when their sick newborns are hospitalized for prolonged periods in a NICU.
Methods: We conducted a study to assess the feasibility and acceptance of an Internet-based telemedicine program in an intensive care setting and to evaluate its impact on newborns' length of stay (LOS) in hospitals. We identified eligible newborns and obtained their parents' written consent before installing a Web camera by the babies' beds. Using child-specific, confidential passwords, families viewed real-time video images of their newborns through a secure portal via an Internet browser or 3G (third-generation) cell phone. Parents of study subjects completed a survey that detailed the performance of the system. Frequency of parental visits and LOS of babies were tracked and compared with the same data for similar high-risk newborns matched for gestation and birth weight.
Results: Parents responded favorably to the stability of the system and clarity of the image. Eighty percent requested a larger image frame. Frequencies of hospital visits made by parents of newborns in the study group and of those made by parents in the control group were not statistically different. LOS and postmenstrual age on discharge of study infants were not statistically different compared with infants in the control group.
Conclusion: Virtual visitation is well accepted by families with sick newborns requiring prolonged hospitalization. Inclusion of information technology to optimize NICU visitation resulted in no significant decrease in duration of hospitalization; however, its role in improving post-discharge transition care must be evaluated further.
Introduction
Telemedicine has been used to facilitate patient care delivery, to improve accessibility of health care services, and to optimize compliance with treatment plans, reducing the need for hospital visits, thereby reducing cost of health care.1–3 It is estimated that globally about 8% to 10% of babies delivered in the hospital require care in a neonatal intensive care unit (NICU).4 Fifty percent of these high-risk babies spend a significant portion of their stay in the NICU and subsequently continue to require a prolonged hospital stay. Families face financial and emotional difficulties when a newborn is not medically stable and has to stay in a NICU for a prolonged period of time. As part of infection-control measures in NICUs, only parents are granted visitation rights. Given the threats to these infants from infectious diseases, parents' visits to the NICU may be further restricted, thus compounding their anxiety. With globalization and the demands of jobs, parents may not be together to support each other throughout the baby's NICU stay. This is especially difficult for first-time parents when faced with the need to make critical decisions about the care of their sick newborns. Very often, when such babies are medically stable and able to go home, parents frequently have little confidence in their own ability to look after their babies, thus prolonging their stay in the hospital further.
We hypothesized that parents are receptive to the use of the Internet and telemedicine technology in an acute NICU setting and that its availability may lower health care costs through reduction in avoidable readmissions after discharge from primary hospitalization. In this article, we describe our study design and our high-tech approach to providing individualized support to the families of very-low-birth-weight infants.
Methods
To facilitate Internet access, we installed three broadband points and three cameras in the NICU at our institution. The connections were linked to a centralized computer located at the central nursing station. Installation of the cameras and technical connections were sponsored by our local telecommunication company, SingTel. The institution initiated the broadband subscription and maintained the service contract throughout the study period.
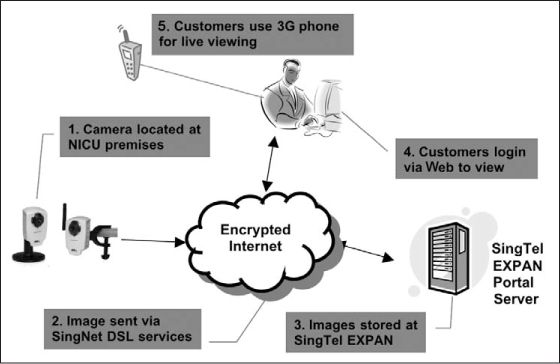
Very-low-birth-weight infants with an expected length of stay (LOS) of more than three weeks in the NICU were eligible for study enrollment. Parents of eligible infants were informed of the availability of Web camera service before the mother's discharge from the maternity ward. Parents with knowledge of Internet use and access to Internet service who agreed to abide by the access guidelines were enrolled in our study. Enrolled families were required to stop using their user identification number and password when their babies were discharged to step-down care or when their newborns were discharged from the hospital, whichever happened first. We obtained written consent from the parents before installing a Web camera by their babies' beds. Each enrolled family was issued a child-specific, confidential password that enabled them to view real-time video images of their newborns through a secure portal via an Internet browser or 3G (third-generation) cell phone (Figures 1 and 2). A security number for each newborn, which included a user identification number and a password, was released on confirmation of agreement in writing. The same security number remained in place for the newborn for the entire NICU stay.
Figure 1.

Picture of cot-side Web camera and Web image on cell phone.
(Permission for publication granted by parents.)
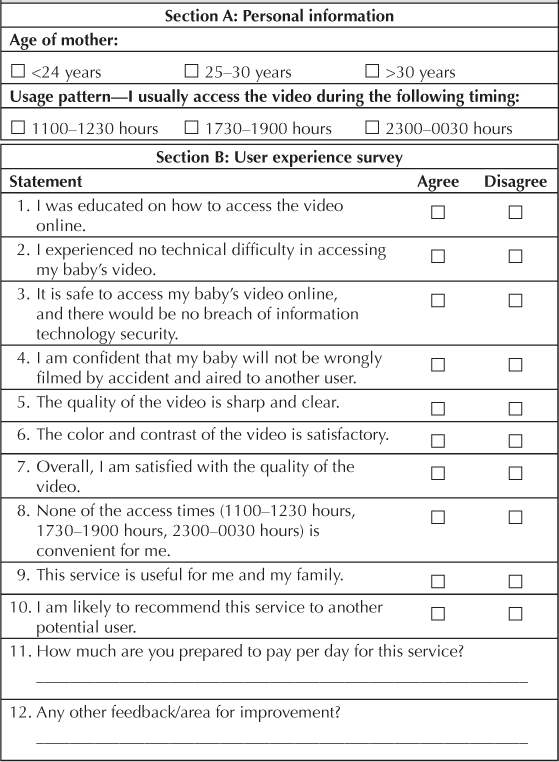
Figure 2.
How the newborn-viewing Web camera system works. (SingTel EXPAN is an Internet service provider for businesses.)
DSL = digital subscriber line
100% of the parents with Internet access found it useful for them and their family members. … and expressed interest in recommending the service to potential users.
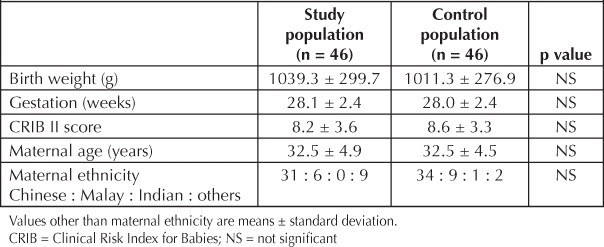
At every shift, the nurse in charge would check that the assigned camera focused on and was filming the correct baby. The system had a visual indicator to alert the staff when the camera was in action. Cameras were activated at scheduled times identified as infants' rest time: 1100 to 1230 hours, 1730 to 1900 hours, and 2300 to 0030 hours. During an emergency, the nursing and medical teams in charge were responsible for switching off the camera. Characteristics of enrolled babies, severity of their illness, and the mothers' ages and ethnicities were collected and compared with randomly selected high-risk newborns matched for gestation and birth weight. Study control-group members were newborns treated in the NICU in the preceding year. LOS, postmenstrual age at discharge, and readmission within 15 days after discharge were tracked for both cohorts of infants. Parental perceptions of the system's stability and feasibility were evaluated through a set of survey questions (Table 1). The cost of implementing this Internet service was computed.
Table 1.
Survey of parental perceptions of Internet viewing service
Statistical Analysis
Statistical analysis was performed using SPSS Statistics (version 18.0; SPSS Inc, Chicago, IL, USA). The data are shown here as means ± standard deviation. Analysis of the study versus control cohorts was performed using the Fisher exact test and the independent sample t-test where appropriate. A p value of <0.05 was considered significant.
Ethics Approval
Our study was approved by our institution's review board and supported by our institution's legal advisor.
Results
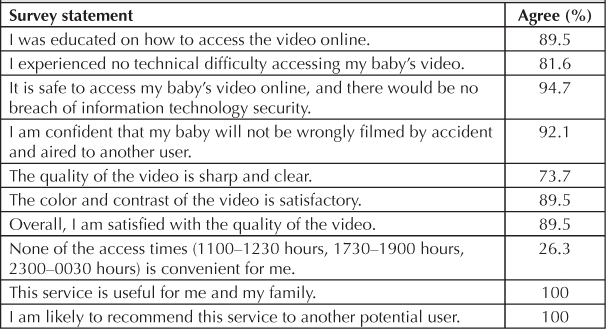
A total of 46 study participants were recruited for the Internet viewing service between 2005 and 2007. Forty-six infants were identified from the patient database maintained by the NICU to serve as a study control group. Data were controlled for gestation and birth weight. Study participants and control-group members were not significantly different regarding birth weight, duration of gestation, or severity of illness as measured on the Clinical Risk Index for Babies (CRIB) II score.5 Infants in both groups were born to mothers with a mean age of 32.5 years. Infants in both groups were equally distributed among ethnicities (Table 2).
Table 2.
Characteristics of study and control-group populations
The mean LOS of study participants was 68.3 ± 25.5 days, compared with 74.3 ± 29.0 days in control-group members. Study participants were discharged at a mean postmenstrual age of 38.1 ± 2.3 weeks compared with 38.4 ± 2.6 weeks for control-group members. These trends did not amount to a statistical significant difference between both groups. One control-group infant was readmitted within 15 days of primary hospital discharge, in contrast with no infants from the study group.
Parents of study participants reported confidence in the Internet viewing service. Ninety-seven percent of families expressed confidence in the safety and security of online video access, and 100% of the parents with Internet access found it useful for them and their family members. All parents of the study cohort expressed interest in recommending the service to potential users (Table 3).
Table 3.
Distribution of parents' responses to survey questions
The service required 3 broadband accounts; the cost for maintaining the 3 accounts and the wireless modem was 7500 SGD (Singapore dollars) per year. For the 3-year study period, our institution incurred a total cost of 22,500 SGD to maintain the service.
Discussion
Our study confirmed the feasibility of integrating communication technologies, using the Internet, in the NICU environment. The technology was readily accepted and enthusiastically embraced by parents. Parents used the system to watch their newborn several times each day. With this viewing service, families remained connected with their child and receive second-by-second updates on their child throughout the access period.
The immense interest among parents of our NICU babies in using the service to gather information on their child's care in the NICU parallels the experience reported from several other studies. The study by Bass et al of patients with Alzheimer disease found that computer support networks were heavily used by patients' family caregivers and significantly reduced stress among caregivers.6 The study by Gray et al of the use of Internet and telecommunication to improve care of high-risk infants demonstrated a high Internet-use rate, with the majority initiating viewing sessions from home.2,7 Other studies have also identified valuable success with the use of telemedicine technologies in the care of pediatric patients. Karp et al, in their study of a population of children with special health care needs, found the telemedicine system to be well received and well used in providing distance consultation within the US state of Georgia.8 Miyasaka et al, in their study on use of telemedicine to provide home monitoring and care after a stay in an intensive care unit, documented a reduced need for physician home visits, unscheduled hospital visits, and days of hospitalization.9
Despite reported successes, several issues have been raised as hindrance to routine implementation of the system, including the ability of providers to recoup costs associated with providing Internet access, telemedicine consultations, and medicolegal concerns.10,11 Similarly, costs of maintaining Internet access restricted our ability to extend the service to all families with newborns at high risk requiring NICU care.
We selected only families with Internet access and with knowledge of how to use the Internet for our study, but it has been shown that families without traditional access to health care derive more benefits from computer-assisted support than do Internet-savvy families.12 Our study was limited by the small size of our study group. Although LOS was shorter among study participants than among control-group infants, the difference was not statistically significant. Infants in our study cohort were discharged earlier than control-group infants; however, this difference also was not statistically significant. Our small study population possibly limits the power of our analyses to detect differences. Extending Internet service in the postdischarge period may potentially improve the efficiency of care coordination for these infants, but further work is required to confirm and demonstrate its impact.
Conclusion
With advances in neonatal practices, NICU care and support for extremely preterm babies has increased, this translates into an increased emotional toll on families. Our study findings confirm that parents respond favorably to the availability of telemedicine in a NICU and that well-designed virtual access may assist in addressing the emotional and educational needs of families, thereby improving family comfort and providing emotional reassurance to parents of neonates at high risk.
Disclosure Statement
This study was partially funded by SingTel, Singapore. The author(s) have no conflicts of interest to disclose.
Acknowledgments
We thank the staff from the Department of Information Technology, Singapore Health Services, for their guidance during the course of our study as well as the NICU nurses and physicians for their support.
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
References
- Field MJ, editor. Telemedicine: a guide to assessing telecommunications for health care. Washington, DC: National Academies Press; 1996. editor. [PubMed] [Google Scholar]
- Gray J, Pompilio-Weitzner G, Jones PC, Wang Q, Coriat M, Safran C. Baby CareLink: development and implementation of a WWW-based system for neonatal home telemedicine. Proc AMIA Symp. 1998:351–5. [PMC free article] [PubMed] [Google Scholar]
- Pompilio-Weitzner G, Gray J, Jones PC, Levy A, Scholz S, Sturges E, Safran C. Baby CareLink: Home telemedicine for families of NICU patients [poster abstract on the Internet] Proc AMIA Symp. 1998. [cited 2011 Jul 17];1055. Available from: http://proceedings.amia.org/1al9ai/1.
- Martin JA, Hamilton BE, Sutton PD, et al. Division of Vital Statistics Births: Final data for 2006. National Vital Statistics Reports. 2009 Jan;57(7) [Google Scholar]
- Parry G, tucker J, Tamow-Mordi W, UK Neonatal Staffing Study Collaborative Group CRIB II: an update of the clinical risk index for babies score. Lancet. 2003 May;361(9371):1789–91. doi: 10.1016/S0140-6736(03)13397-1. [DOI] [PubMed] [Google Scholar]
- Bass DM, McClendon MJ, Brennan PF, McCarthy C. The buffering effect of a computer support network on caregiver strain. J Aging Health. 1998;10(1):20–43. doi: 10.1177/089826439801000102. [DOI] [PubMed] [Google Scholar]
- Gray JE, Safran C, Davis RB, et al. Baby CareLink: using the Internet and telemedicine to improve care for high-risk infants. Pediatrics. 2000 Dec;106(6):1318–24. doi: 10.1542/peds.106.6.1318. [DOI] [PubMed] [Google Scholar]
- Karp WB, Grigsby K, McSwiggan-Hardin M, et al. Use of telemedicine for children with special health care needs. Pediatrics. 2000 Apr;105(4 Pt 1):843–7. doi: 10.1542/peds.105.4.843. [DOI] [PubMed] [Google Scholar]
- Miyasaka K, Suzuki Y, Sakai H, Kondo Y. Interactive communication in high-technology home care: videophones for pediatric ventilatory care. Pediatrics. 1997 Jan;99(1):E1. doi: 10.1542/peds.99.1.e1. [DOI] [PubMed] [Google Scholar]
- Rind DM, Kohane IS, Szolovits P, Safran C, Chueh HC, Barnett GO. Maintaining the confidentiality of medical records shared over the Internet and the World Wide Web. Ann Intern Med. 1997 Jul 15;127(2):138–41. doi: 10.7326/0003-4819-127-2-199707150-00008. [DOI] [PubMed] [Google Scholar]
- Sorum PC, Mallick R. Physicians' opinions on compensation for telephone calls. Pediatrics. 1997 Apr;99(4):E3. doi: 10.1542/peds.99.4.e3. [DOI] [PubMed] [Google Scholar]
- DuBenske LL, Gustafson DH, Shaw BR, Cleary JF. Web-based cancer communication and decision making systems: connecting patients, care-givers, and clinicians for improved health outcomes. Med Decis Making. 2010 Nov–Dec;30(6):732–44. doi: 10.1177/0272989X10386382. [DOI] [PMC free article] [PubMed] [Google Scholar]


