Abstract
Black widow spiders (Latrodectus mactans) are found throughout the US. Though bites are relatively uncommon, they pose a significant health problem with over 2500 reported to American poison control centers annually. Black widow spider bites cause a characteristic envenomation syndrome consisting of severe pain, muscle cramping, abdominal pain, and back pain. The significant pain associated with envenomation is often refractory to traditional analgesics. Antivenom (Antivenin Latrodectus mactans) is available and effective, but is often withheld because of a fear of acute hypersensitivity reactions. We report four cases of symptomatic black widow spider envenomation. One of the reported cases was managed without antivenom, and, in contrast, three were treated successfully with Antivenin Latrodectus mactans. We believe that these cases demonstrate safe and effective use of black widow antivenom. This article presents the rationale for use of antivenom in these cases, and a nonsystematic review of the pertinent literature.
Background
Latrodectus species are found throughout the world. Five species of widow spiders occur in the US: the southern black widow (L mactans), the northern black widow (L variolus), the Western black widow (L hesperus), the brown widow (L geometricus), and the red widow (L bishopi). In North America, the most widely distributed native spider is L mactans, known as the black widow spider.1,2 Although most spiders produce venom, the vast majority lack mouthpieces (chelicerae) capable of delivering their venom through human skin.3–5 Black widow spiders are one of only a few spiders with the ability to cause a poisonous bite to humans.3,4 Only female widow spiders are dangerous. They can be identified by the hourglass pattern (red or orange in color) on the ventral aspect of their shiny, black abdomen (Figure 1). Male widow spiders are much smaller and lighter in color, and they lack the ability to deliver venom. Black widow spiders are commonly found in garages, trash heaps, and outbuildings but are uncommon in occupied dwellings. Bites are usually defensive, occurring when the spider is accidentally disturbed.4
Figure 1.

Female black widow spider.
Black widow spider envenomation remains a significant health problem in the US, being reported over 2500 times annually to US poison-control centers.1,2 The actual number of envenomations is probably much higher, because poison-center estimates tend to underreport exposures.6 Black widow spider envenomation frequently results in severe pain, muscle cramps, abdominal pain, back pain, and hypertension. These symptoms may be refractory to traditional therapies. However, envenomation is associated with low mortality.4,7 Only three cases of deaths associated with widow spiders have been reported in the world medical literature. Two were patients from Madagascar bitten by L geometricus species, and the third was a young Greek woman who died of myocarditis after being bitten by an L tredecimguttatus spider.8,9 There are no known cases of death resulting from envenomation by the widow species found in the US.
Antivenin Latrodectus mactans (Merck & Co, Inc, Whitehouse Station, NJ) is the only antivenom currently available in the US for treatment of black widow spider envenomation.10 Despite the significant symptoms that may develop after envenomation, the use of antivenom is a subject of debate within the toxicology community. This controversy stems primarily from a single reported case of fatal hypersensitivity related to spider antivenom administration. We describe here one case in which envenomation was treated without antivenom and three cases in which Antivenin Latrodectus mactans was used safely and effectively.
Case Presentations
Case 1
A previously healthy boy, age 3 years, arrived in the Emergency Department (ED) 1.5 hours after suffering a black widow spider bite to the top of his right foot while putting on his boots. The parents brought the spider to the ED, where it was identified as a female black widow. There was a 2-by-2-cm area of mild erythema to the top of the boy's foot. Over the next hour, the boy developed severe foot, leg, groin, and abdominal pain. His vital signs were as follows: blood pressure, 111/68 mmHg; respiratory rate, 20 to 30 breaths/min; heart rate, 103 beats/min; temperature, 98.4°F; pulse oxygen saturation, 99% on room air. His lungs were clear, and findings on his cardiac and abdominal examinations were normal. He cried constantly and complained of severe pain.
The patient was treated with morphine and lorazepam in the ED, which did not provide relief. Because of concern about a hypersensitivity reaction, he was not given Antivenin Latrodectus mactans. He was eventually admitted to the pediatric ward for further pain control. In the hospital, he received ketorolac every 6 hours and hydromorphone every 4 hours for 2 days. A consultation with the Medical Toxicology Service was not obtained. On the third hospital day, the boy began to feel better and was discharged to his home that afternoon. After discharge, his symptoms resolved completely, and he had experienced no further sequelae when evaluated 6 months later.
Case 2
A previously healthy man, age 35 years, arrived in the ED approximately 1 hour after sustaining a bite to his left middle toe from what he described as a “black spider.” He was doing yard work, wearing boots that were “open at the top,” when he felt a sudden pain in his toe. When he removed the boot to investigate, a black spider ran out. Within 5 minutes of the incident, he began feeling severe pain, cramping, and paresthesias in his left leg. The pain progressed to include his abdomen, low back, and chest. In the ED, the patient complained that the pain was so severe that it was difficult to sit or lie down. Because the patient's description of the spider that bit him and the classic clinical syndrome, his symptoms were believed to be caused by Latrodectus envenomation.
His vital signs were as follows: blood pressure, 146/72 mmHg; respiratory rate, 18 breaths/min; heart rate, 71 beats/min; temperature, 97.8°F; pulse oxygen saturation, 99% on room air. He appeared uncomfortable and was treated with intravenous diazepam and ketorolac, which did not provide relief. During his ED stay, his pain became more severe, requiring multiple doses of hydromorphone for control. The patient stood bent over the gurney and appearing very uncomfortable. His lungs were clear, and findings on his cardiac and abdominal examinations were normal. His left middle toe showed no discernible bite marks, swelling, or erythema.
Because of the patient's severe pain, the medical toxicologist thought that Latrodectus antivenom would be appropriate for treatment. The benefits and risks of treatment were discussed, and then the patient stated, “I would rather die taking the medicine than feel the pain the way I do.” One vial of Antivenin Latrodectus mactans (2.5 mL) was infused intravenously during a 30-minute period. Within 15 minutes of infusion completion, he began experiencing relief. No further hydromorphone was required. He was observed in the ED for 2 hours and then discharged to his home. A follow-up appointment was scheduled for 48 hours later, but he did not keep it. A review of the medical records showed no return visits to the ED and no further clinic visits by the patient. He was not available for long-term follow-up assessment.
Case 3
A woman, age 24 years, arrived in the ED and said that she had sustained a black widow spider bite on her right shoulder. The spider was on a shirt that she put on. The patient had mild erythema without swelling at the bite site. She complained of severe pain and muscle cramps in the shoulder, neck, and back. Her vital signs were as follows: blood pressure, 143/94 mmHg; respiratory rate, 18 breaths/min; heart rate, 101 beats/min; temperature, 97.8°F; pulse oxygen saturation, 99% on room air. She appeared extremely uncomfortable. Her lungs were clear, and findings on her cardiac and abdominal examinations were normal. She was treated with hydromorphone, ketorolac, metoclopramide, and lorazepam, which provided minimal relief.
Latrodectus antivenom therapy was recommended by the medical toxicologist because of her severe pain. After intravenous infusion of a single vial (2.5 mL) of Antivenin Latrodectus mactans, the patient experienced significant relief and required no further pain medication. She was discharged to her home after 2.5 hours of observation. She did not return to the ED or to her primary physician for further treatment. At a follow-up evaluation more than 1 year after the incident, she reported having no further sequelae after leaving the ED and no symptoms of serum sickness.
Case 4
A boy, age 8 years, was brought to the ED by his mother approximately 3 hours after sustaining a black widow spider bite to his right second toe. The spider was in a shoe that the boy put on. The mother had brought the spider to the ED, and it was clearly identifiable as a female black widow. The patient complained of severe pain that began in his foot and then progressed to his leg, low back, abdomen, and chest.
At presentation, his vital signs were as follows: blood pressure, 134/92 mmHg; respiratory rate, 26 breaths/min; heart rate, 96 beats/min; temperature, 97.8°F; pulse oxygen saturation, 96% on room air. He appeared to be in distress. He was diaphoretic. His abdomen was tight, and he exhibited diffuse guarding. His lungs were clear, and findings on his cardiac examination were normal. There was mild erythema of his right second toe, but there were no identifiable puncture marks. While in the ED, the patient began to complain of difficulty breathing. He was treated with morphine and diazepam, which did not provide relief.
Latrodectus antivenom was recommended by the on-call toxicologist for treatment of his severe pain. A single vial (2.5 mL) of Antivenin Latrodectus mactans was infused intravenously during a 20-minute period. During infusion, he began experiencing relief of his symptoms. Within 20 minutes, he was feeling better and described his pain as being at a level of 1 on a scale of 1 to 10. After 1.5 hours of observation in the ED, he was released to his home. He was seen for a follow-up evaluation 2 days later and reported no further pain and had required no oral pain medication. At a follow-up evaluation more than 1 year later, he reported no further sequelae and no symptoms of serum sickness.
Discussion
Of the four cases discussed here, three involved bites to the feet and one to the right shoulder. One patient was treated without antivenom, and the other three patients were successfully and safely treated with Antivenin Latrodectus mactans. We believe that the rapid symptomatic improvement and favorable outcomes we observed in these cases were directly attributable to the use of spider antivenom. Antivenom provides rapid pain relief and may help to avoid hospital admissions and/or repeat ED visits.
Latrodectus venom is one of the most potent poisons by volume, containing at least five insecticidal toxins, a vertebrate-specific neuro-toxin (α-latrotoxin), and one toxin affecting crustaceans. The primary toxin responsible for the envenomation syndrome in humans is α-latrotoxin. The neurotoxin binds to specific presynaptic receptors (neurexin 1a and CIRL) that precipitate neurotransmitter release, particularly norepinephrine and acetylcholine.4 Release of these neurotransmitters is responsible for the classic envenomation syndrome seen with these bites.
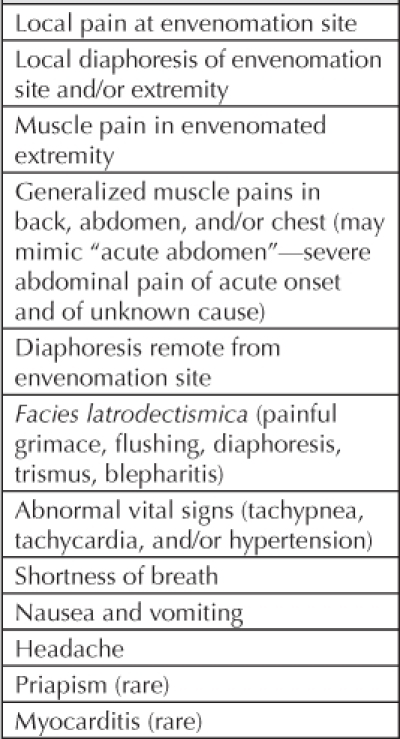
Black widow spider bites occur most commonly to the lower extremities, followed by the upper extremities and then the trunk.3,11,12 Interestingly, reports of early series noted higher numbers of bites to the trunk (ie, the buttocks and genitalia) related to outhouse exposures.13 No association between bite location and envenomation severity has been found.7 Local bite site findings are variable, including tiny puncture marks, mild erythema, and an erythematous target-like lesion11,14 (Figure 2). Symptoms of envenomation include diaphoresis, hypertension, muscle cramping, weakness, and pain either near or distant from the site of envenomation. The most common presenting symptoms are abdominal and/or back pain that may be very severe and difficult to treat (Table 1). Severe abdominal pain mimicking “acute abdomen” has even been reported.15 Although these symptoms can be extremely uncomfortable, permanent disability and death are rare.4,7 Treatment of black widow spider envenomation can be challenging, often necessitating large doses of pain medication and/or hospital admission. In one study, 52% (39 of 76) of patients with black widow bites who did not receive antivenom required hospital admission for further treatment.3
Figure 2.

Example of local appearance of Latrodectus mactans bite to the neck. (This photograph is not from any of the presented cases.)
Table 1.
The traditional therapies for black widow spider envenomation are aimed at providing symptomatic relief while venom effects resolve. These include primarily opioid analgesics and muscle relaxants. Past trials involving these therapies have shown partial success at best.3,4,6,16 In addition, calcium therapy was once considered to be an antidote for black widow envenomation.17 Calcium was thought to stabilize nerve membrane permeability, resulting in decreased neurotransmitter release.16,17 Although this effect was demonstrated in vitro and reported in some early clinical series,13,16–18 subsequent experience has not shown effectiveness. Therefore, calcium therapy has lost favor in the medical toxicology community.3–6
The only therapies with proven effectiveness are opioid analgesics and black widow spider antivenom. Antivenin Latrodectus mactans is an equine-derived antivenom based on immunoglobulin G.4,10,19,20 The proposed pharmacologic mechanism is binding of venom toxic constituents by the antivenom antibodies. A single vial (2.5 mL) generally provides adequate relief in human (adult or pediatric) poisoning cases.3–5,14,19,21 The Kaiser Permanente (KP) acquisition cost for one vial of Antivenin Latrodectus mactans was $27.71 in 2011. In the largest series reported to date of moderate to severe black widow spider envenomation (n = 163), patients treated with antivenom experienced a much shorter duration of symptoms and were less likely to be admitted to the hospital than those who did not receive antivenom.3 Relief of symptoms occurred within an average of 31 minutes of antivenom infusion.3 Administration of antivenom even late in the course of envenomation has been reported to be effective.21,22 In one reported case, antivenom was used effectively for the treatment of symptoms 90 hours after a black widow spider bite.22
Acute hypersensitivity reactions are the most feared complication associated with Antivenin Latrodectus mactans administration. Although these reactions do occur, relatively few minor reactions have been reported,3,6,14 and only one report of a severe reaction can be found in the medical literature.3 Unfortunately, that one case is frequently cited as the reason to avoid administering antivenom to symptomatic patients.3,6 Critics believe that because black widow spider envenomation is generally a nonfatal condition, it is too risky to administer such treatment with even a single reported fatality reported in the medical literature. The case at the heart of controversy, however, involved a young woman with history of asthma and multiple medication allergies who received a rapid, undiluted bolus of antivenom. She had a severe hypersensitivity reaction. Unfortunately, her resuscitation was complicated by a pneumothorax and a protracted hospital stay, and she eventually died.2,3,6 Although that case was tragic, we do not believe that it represents sufficient evidence for abandoning antivenom use on the grounds that it is unsafe. The current package insert for Antivenin Latrodectus mactans calls for infusion of diluted antivenom during a period of 15 to 30 minutes.10 At these slower infusion rates, immediate hypersensitivity appears to be extremely rare.6
We believe that antivenom, when given correctly, is safe and should be considered in cases of envenomation with systemic symptoms or severe local symptoms. Though it is not mentioned on the package insert for Antivenin Latrodectus mactans, patients may be pretreated with diphenhydramine and/or steroids in an attempt to blunt a hypersensitivity response.5,6 Multiple allergies, asthma, or past reactions to equine-based products should be considered contraindications.10
Black widow spider envenomation in pregnancy has been recommended as an indication for antivenom because of the risk of venom-induced abortion or other possible harm to the fetus4,23; however, the actual risk is not known. In one report of a poison-center study of 97 black widow spider bites in pregnant females, there were no miscarriages.24 Although Antivenin Latrodectus mactans is a category C drug, it has been given in pregnancy without consequence.25,26 Even though absolute safety is impossible to prove, there is nothing currently to suggest that spider antivenom is unsafe in pregnancy. Antivenin Latrodectus mactans does contain the preservative thimerosal, but the amount of mercury associated with an antivenom dose would not be expected to cause fetal harm.24
The package insert for Antivenin Latrodectus mactans does warn of the potential for (delayed) serum sickness after antivenom administration. In contrast to equine-based snake antivenom (Antivenin Crotalidae Polyvalent [Wyeth-Ayerst, West Greenwich, RI]), which required much larger doses and was associated with serum sickness in the majority of patients, Latrodectus antivenom usually requires only a single vial, and there are few reports of serum sickness from it.5,6,14 Although the exact rate of serum sickness after black widow spider antivenom is unknown, our review of the literature leads us to believe that it is low. In one study of Australian red-back spider antivenom (a similar antivenom product, Antivenin Latrodectus hasselti [CSL Limited, Parkville, Victoria, Australia]), the incidence of serum sickness was 1.7%.11
Antivenin Latrodectus mactans has been used for more than 70 years. A new Fab antibody-based antivenom is currently in development and in phase 3 trials. The hope is that this product will be equally effective but carry a lower risk of hypersensitivity reactions.
KP Northern California has a regional on-call Medical Toxicology consultation service offering assistance in treating poisoned patients.
Conclusion
In three of four cases of symptomatic black widow spider envenomation, we administered Antivenin Latrodectus mactans and observed rapid and complete resolution of symptoms. These cases demonstrate the safe and effective use of spider antivenom. Our review of the literature suggests that the witnessed effects of antivenom are usual, which leads us to believe that Antivenin Latrodectus mactans is safe when given correctly.
Disclosure Statement
This study received no funding. The author(s) have no conflicts of interest to disclose.
Acknowledgments
Katharine O'Moore-Klopf, ELS, of KOK Edit provided editorial assistance.
References
- Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Giffin SL. 2008 Annual report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 26th annual report. Clin Toxicol (Phila) 2009 Dec;47(10):911–1084. doi: 10.3109/15563650903438566. [DOI] [PubMed] [Google Scholar]
- Daly FFS, White J. Widow and related Latrodectus spiders. In: Brent J, Wallace K, Burkhart K, Phillips S, Donovan J, editors. Critical care toxicology: diagnosis and management of the critically poisoned patient. Philadelphia, PA: Elsevier Mosby; 2005. pp. 1187–93. p. [Google Scholar]
- Clark RF, Wethern-Kestner S, Vance MV, Gerkin R. Clinical presentation and treatment of black widow spider envenomation: a review of 163 cases. Ann Emerg Med. 1992 Jul;21(7):782–7. doi: 10.1016/s0196-0644(05)81021-2. [DOI] [PubMed] [Google Scholar]
- Hahn IH, Lewin NA. Arthropods. In: Flomenbaum NE, Goldfrank L, Hoffman R, Howland MA, Lewin N, Nelson L., editors. Goldfrank' s toxicologic emergencies. 8th ed. New York: McGraw-Hill Professional; 2006. pp. 1603–22. p. [Google Scholar]
- Peterson ME. Black widow spider envenomation. Clin Tech Small Anim Pract. 2006 Nov;21(4):187–90. doi: 10.1053/j.ctsap.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Clark RF. The safety and efficacy of antivenin Latrodectus mactans. J Toxicol Clin Toxicol. 2001;39(2):125–7. doi: 10.1081/clt-100103827. [DOI] [PubMed] [Google Scholar]
- Moss HS, Binder LS. A retrospective review of black widow spider envenomation. Ann Emerg Med. 1987 Feb;16(2):188–92. doi: 10.1016/s0196-0644(87)80014-8. [DOI] [PubMed] [Google Scholar]
- Ramialiharisoa A, de Haro L, Jouglard J, Goyffon M. [Latrodectism in Madagascar]. [Article in French] Med Trop (Mars) 1994;54(2):127–30. [PubMed] [Google Scholar]
- Pneumatikos IA, Galiatsou E, Goe D, Kitsakos A, Nakos G, Vougiouklakis TG. Acute fatal toxic myocarditis after black widow spider envenomation. Ann Emerg Med. 2003 Jan;41(1):158. doi: 10.1067/mem.2003.32. [DOI] [PubMed] [Google Scholar]
- Antivenin Latrodectus mactans [package insert] Whitehouse Station, NJ: Merck & Co, Inc; 2005. [Google Scholar]
- Sutherland SK, Trinca JC. Survey of 2144 cases of red-back spider bites: Australia and New Zealand, 1963– 1976. Med J Aust. 1978 Dec 30;2(14):620–3. doi: 10.5694/j.1326-5377.1978.tb131783.x. [DOI] [PubMed] [Google Scholar]
- Isbister GK, Gray MR. Latrodectism: a prospective cohort study of bites by formally identified redback spiders. Med J Aust. 2003 Jul 21;179(2):88–91. doi: 10.5694/j.1326-5377.2003.tb05442.x. [DOI] [PubMed] [Google Scholar]
- Kirby-Smith HT. Black widow spider bite. Ann Surg. 1942 Feb;115(2):249–57. doi: 10.1097/00000658-194202000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordt SP, Lee A, Sasaki K, Clark RF, Cantrell FL. Retrospective review of black widow spider antivenom use [abstract 110] Clin Toxicol. 2010;48(6):627. Available from: www.eapcct.org/publicfile.php?folder=congress&file=Abstracts_Denver.pdf. [Google Scholar]
- Bush SP. Black widow spider envenomation mimicking cholecystitis. Am J Emerg Med. 1999 May;17(3):315. doi: 10.1016/s0735-6757(99)90137-7. [DOI] [PubMed] [Google Scholar]
- Key GF. A comparison of calcium gluconate and methocarbamol (Robaxin) in the treatment of Latrodectism (black widow spider envenomation) Am J Trop Med Hyg. 1981 Jan;30(1):273–7. doi: 10.4269/ajtmh.1981.30.273. [DOI] [PubMed] [Google Scholar]
- Gilbert EW, Stewart CM. Effective treatment of arachnidism by calcium salts: a preliminary report. Am J Med Sci. 1935;189(4):532–6. [Google Scholar]
- Timms PK, Gibbons RB. Latro-dectism—effects of the black widow spider bite. West J Med. 1986 Mar;144(3):315–7. [PMC free article] [PubMed] [Google Scholar]
- Bronstein NA. Antidotes in depth: antivenom (scorpion and spider) In: Flomenbaum NE, Goldfrank L, Hoffman R, Howland MA, Lewin N, Nelson L., editors. Goldfrank' s toxicologic emergencies. 8th ed. New York: McGraw-Hill Professional; 2006. pp. 1623–8. p. [Google Scholar]
- Heard K, O'Malley GF, Dart RC. Antivenom therapy in the Americas. Drugs. 1999 Jul;58(1):5–15. doi: 10.2165/00003495-199958010-00002. [DOI] [PubMed] [Google Scholar]
- Suntorntham S, Roberts JR, Nilsen GJ. Dramatic clinical response to the delayed administration of black widow spider antivenin. Ann Emerg Med. 1994 Dec;24(6):1198–9. doi: 10.1016/s0196-0644(94)70259-4. [DOI] [PubMed] [Google Scholar]
- O'Malley GF, Dart RC, Kuffner EF. Successful treatment of latrodectism with antivenin after 90 hours. N Engl J Med. 1999 Feb 25;340(8):657. doi: 10.1056/NEJM199902253400816. [DOI] [PubMed] [Google Scholar]
- Russell FE, Marcus P, Streng JA. Black widow spider envenomation during pregnancy. Report of a case. Toxicon. 1979;17(2):188–9. doi: 10.1016/0041-0101(79)90302-7. [DOI] [PubMed] [Google Scholar]
- Wolfe MD, Meyers O, Carvati EM, Rayburn WF, Seifert SA. Black widow spider envenomation in pregnancy. J Matern Fetal Neonatal Med. 2011 Jan;24(1):122–6. doi: 10.3109/14767058.2010.481317. [DOI] [PubMed] [Google Scholar]
- Sherman RP, Groll JM, Gonzalez DI, Aerts MA. Black widow spider (Latrodectus mactans) envenomation in a term pregnancy. Curr Surg. 2000 Jul 1;57(4):346–8. doi: 10.1016/s0149-7944(00)00276-2. [DOI] [PubMed] [Google Scholar]
- Handel CC, Izquierdo LA, Curet LB. Black widow spider (Latrodectus mactans) bite during pregnancy. West J Med. 1994 Mar;160(3):261–2. [PMC free article] [PubMed] [Google Scholar]
- Quan D, Ruha AM. Priapism associated with Latrodectus mactans envenomation. Am J Emerg Med. 2009 Jul;27(6):759.e1–2. doi: 10.1016/j.ajem.2008.10.033. [DOI] [PubMed] [Google Scholar]
- Sari I, Zengin S, Davutoglu V, Yildirim C, Gunay N. Myocarditis after black widow spider envenomation. Am J Emerg Med. 2008 Jun;26(5):630. e1–3. doi: 10.1016/j.ajem.2007.09.012. [DOI] [PubMed] [Google Scholar]
- Hoover NG, Fortenberry JD. Use of antivenin to treat priapism after a black widow spider bite. Pediatrics. 2004 Jul;114(1):e128–9. doi: 10.1542/peds.114.1.e128. [DOI] [PubMed] [Google Scholar]


