Abstract
Objective
The identification of older adults who are at increased risk of future cognitive decline is often difficult, particularly in individuals of an ethnic minority. This study evaluated which baseline demographic, neuropsychological and functional variables were most strongly associated with future longitudinal decline in global cognitive function.
Design/setting
Participants were part of a community-based prospective longitudinal study of 1789 older Hispanics (Sacramento Area Latino Study on Aging (SALSA)).
Participants
A subsample of 639 individuals were evaluated, comprising cognitively normal, mildly impaired, and dementia cases, and were followed longitudinally for up to seven years. Sixty-three percent were tested in Spanish.
Measurements
Latent growth curve modeling of longitudinal data was used to assess the effects of age, gender, education, language of test administration (Spanish or English), acculturation, baseline measures of neuropsychological function (i.e. verbal memory and confrontation naming) and baseline everyday functioning (as measured by the IQCODE) on rate of change in global cognitive impairment (measured by the 3MS).
Results
Less education, being tested in English, and poorer scores on the neuropsychological tests were all cross-sectionally associated with lower baseline 3MS scores. However, longitudinal decline in global cognition over time was primarily associated with older age and poorer everyday function at baseline.
Conclusions
Informant-based ratings of functional impairment, which are easy to collect in a clinical setting, have significant utility in identifying Hispanic older adults at increased risk for future cognitive decline.
Keywords: Cognitive decline, Hispanic population
There has been a dramatic increase in the numbers of older persons in the U.S. who belong to an ethnic minority. Hispanic elderly are among the most rapidly growing aging minorities in the U.S. [1]. Several studies have suggested that the prevalence of cognitive impairment and dementia in older Hispanics is similar to, or higher than in non-Hispanic whites [2-5]. Such findings highlight the need for culturally appropriate methods to identify risk factors for cognitive decline and dementia in elderly Hispanics. Better identification of Hispanic older adults at risk for cognitive decline and dementia will, in turn, lead to the improved provision of healthcare services to this underserved population.
Cognitive testing, whether in the form of brief screening measures or more comprehensive neuropsychological testing, is typically an important part of the standard work-up for neurodegenerative diseases of aging. However, demographic factors including cultural background, being tested in a language other than one's first/primary language, and having low levels of education can adversely affect performance on cognitive tests. In these situations, cross-sectional cognitive testing can lead to erroneous conclusions about the presence of an underlying neurodegenerative disease [6-8]. That is, low cognitive test scores are misattributed to disease rather than being a result of background factors. As such, it can be difficult for clinicians to identify those older individuals of an ethnic minority or with low education who are declining and at risk for the development of dementia.
Early signs of neurodegenerative diseases such as Alzheimer's disease manifest not only as cognitive impairments but also as changes in one's ability to function independently in daily life. In fact, significant disability in daily function is a required criterion for a dementia syndrome [9]. More subtle changes in daily function have been shown to be evident well before frank dementia develops [10-12]. Thus, another approach to evaluating the presence of an underlying neurodegenerative disease, or predicting risk of future disease progression, is to evaluate changes in functional status. Several studies have suggested that measures of everyday function tend to be much less correlated with demographic variables such as education, than neuropsychological tests [13-16]. Therefore, the measurement of functional impairment may provide a particularly good way to identify those who are on a ‘downward trajectory’ (verses those who will remain stable) in individuals of an ethnic minority whose cognitive test scores can be difficult to interpret due to the confounding effects of education and cultural background.
This study prospectively followed a large group of elderly Hispanic individuals living in the community. Participants were evaluated on an annual basis for up to seven years. The goal of the present study was to determine which variables help identify who is on a trajectory of decline using a continuous measure of global cognition. More specifically, we examined which demographic and baseline neuropsychological and functional variables are most strongly associated with longitudinal decline in global cognitive functioning in Hispanic older adults. It was hypothesized that informant reports of functional status at baseline would be a better predictor of future cognitive decline than baseline neuropsychological performance after controlling for background variables such as age, years of education, language of test administration, and level of acculturation.
Methods
Participant Sample
Participants in this study were all part of the Sacramento Area Latino Study on Aging (SALSA). The SALSA project is an epidemiological, longitudinal study of cognitive and functional impairment in older Hispanics. Recruitment methods have been extensively described previously [17-19]. Briefly, SALSA recruitment targeted Census tracts of Sacramento County and neighboring counties with proportional densities of Hispanics greater than 5% based on 1990 and 1998 U.S. Census information. The recruitment method was designed to enumerate all Hispanic households within the targeted Census tracts. Individuals eligible for the study were (1) self-identified as Latino or Hispanic, (2) age 60 or above, (3) Spanish or English speakers, and (4) living in a non-institutionalized setting. A multi-tier approach involved mailing Hispanic households information regarding SALSA, which was followed by a telephone call. Households that could not be contacted by telephone or mail were visited by recruiters. The overall response rate in those contacted was 85%. Approximately 22% of the total eligible population of Sacramento County, CA was recruited. At baseline a total of 1,789 Hispanics age 60 and over were enrolled in the SALSA study.
Of the 1,789 individuals recruited into SALSA a subsample underwent further testing and this subsample is the focus of the present study. Two screening tests were used to determine who received further neuropsychological testing. These were the 3MSE [20] and Spanish and English Verbal Learning Test (SEVLT, [17]). The 3MSE is a measure of global cognitive functioning. The delayed recall trial from the SEVLT was used with the 3MSE to screen for cognitive impairment. Those individuals who fell below the 20th percentile on either of these instruments received additional neuropsychological testing. In addition, a 20% random subset of the entire sample was referred for neuropsychological testing. Neuropsychological testing was completed by 82.6% of SALSA participants referred for testing. The sampling procedure described above was used to ensure a diverse sample was captured in terms of range of cognitive function. The initial period of recruitment for the study occurred between 1998 and 1999 and follow-up evaluations continued through 2006. Follow-ups were done on approximately an annual basis.
Outcome measure
Global Cognitive Function
The Modified Mini Mental State Exam (3MS; [20]) was used to measure global cognitive functioning because it is an efficient but sensitive instrument that has been widely used in epidemiological research on cognition. It is an expanded version of the MMSE [21] that was designed to increase the sensitivity and reliability of the original MMSE. The 3MS is a 100-point scale that includes additional items to assess a wider variety of abilities than the original MMSE (i.e. abstract reasoning, verbal fluency) and expanded scoring schemes for some items (e.g. pentagon drawing, spelling ‘world’ backwards) [20,22, 23]. The 3MS was translated and back translated from English to Spanish. A consensus group of Spanish speakers reviewed these translations. When applicable, linguistic equivalents of some items were used instead of the exact translation. This mainly applied to the phrase ‘no ifs ands or buts’ which was replaced with ‘si no sube baja’ in the Spanish version. Evidence of its validity as a measure of cognitive function in this population comes from a number of studies that show that the 3MS is related to a diagnosis of dementia [19] to structural and functional brain imaging [24], to the presence of a metabolic syndrome [25] and to folate deficiency [26].
Baseline predictor variables
Demographic and linguistic variables
Gender, age, and education were included as basic demographic variables. Participants were allowed to decide whether they wanted to be tested in English or Spanish. Cultural orientation was measured using the Acculturation Rating Scale for Mexican Americans – Version II (ARSMA-II; [27]). This instrument assesses such information as whether an individual prefers Spanish or English media, and about contacts with their country of origin and with people of Latino and Anglo backgrounds. It is widely used to assess degree of cultural adaptation of Mexican Americans into the Anglo culture. The scale was formed so that the least affiliation with Anglo cultured was scored as 0, and the items were summed to form a scale from 0 – 63.
Functional assessment
Problems in everyday abilities were measured at baseline using the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE; [13, 28, 29]. This is a 26-item interview-based questionnaire completed by an informant familiar with the participant. Each informant is asked to compare the participant's current level of everyday functioning with how he or she was functioning 10 years earlier. Each of the 26 items assesses specific, day-to-day activities dependent upon memory and cognitive functions which are rated according to a five-point scale: 1 = much better than 10 years earlier, 2 = somewhat better, 3 = no change, 4 = somewhat worse, 5 = much worse. A total score was derived from averaging the ratings over the total number of completed items and ranges from 1.0 to 5.0 with higher scores indicating worse functional impairment. Both English and Spanish versions of the IQCODE are available [30, 31]. Since the original Spanish language version of the IQCODE was developed in Spain, a consensus group of local Spanish speakers (bilingual, bicultural researchers and psychometrists) reviewed this original Spanish version and when applicable, linguistic equivalents of some items were used when deemed appropriate to the local Hispanic population. The IQCODE has been shown to have high internal consistency and good test-retest reliability [13]. The IQCODE also has limited association with education [13,14]. Examples of IQCODE items are included in the Appendix. In a previous paper we have shown that the relationship between the IQCODE and cognitive and neuroimaging variables does not differ as a function of language status (English or Spanish) [32].
Cognitive measures
Cognitive tests were taken from the Spanish and English Neuropsychological Assessment Scales (SENAS; [33-35]. This is a neuropsychological test battery developed using psychometric methods associated with item response theory (IRT) [36-38]. The overriding goal for the SENAS project was to construct a battery of psychometrically matched tests that are clinically relevant for the neuropsychological evaluation of older English and Spanish speaking persons. The goal of psychometric matching called for highly similar measurement properties of the English and Spanish versions of the same scale, but also for similar measurement properties of all scales within each language version.
Two separate measures of cognitive ability were derived from the SENAS for the purposes of this study: 1) Verbal Memory, 2) Object Naming. The Verbal Memory measure was derived from the Spanish and English Verbal Learning Test (SEVLT; [17]). The SEVLT uses a 15 word list that is presented for five learning trials in a standard word-list learning test format, followed by presentation of a distractor task, and then by free recall of the initial list. The Verbal Memory measure was a composite measure combining scores from the learning trials and delayed recall trials. Object Naming is a confrontation naming task that assesses ability to name objects depicted in colored pictures and drawings. The current study focused on episodic memory and confrontation naming as possible predictors of future decline because these two variables from the SENAS have been previously shown to independently and incrementally discriminate between clinical groups in cross-sectional analysis [34]. Raw scores were used in the analysis and demographic variables (i.e. education) were added to various models as covariates.
Data Analysis
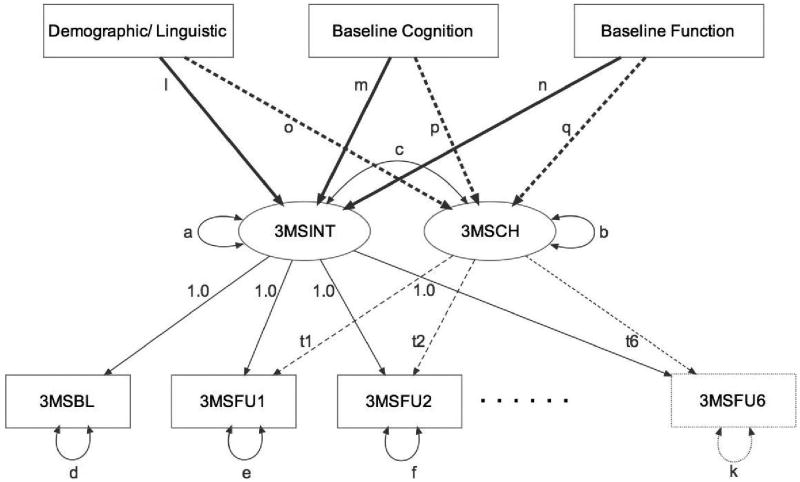
A latent variable modeling approach was used to estimate relationships of demographic variables and baseline measures of cognition and independent function with longitudinal trajectories of cognition, measured by the 3MS. Latent variable models provide a flexible platform for characterizing longitudinal change in relationship to external variables that might account for differences in longitudinal trajectories [39, 40]. In this study, there were seven observation points for the 3MS with varying numbers of observations at each assessment wave. The Mplus application [41] was used to fit a latent growth model with random effects estimates of 3MS baseline status and linear rate of change [41]. Figure 1 shows the overall analytic framework for this model.
Figure 1.
Conceptual and analytic model. Observed variables are indicated by rectangles and latent variables are represented by ovals, one headed arrows correspond to regressions of the variable at the (arrow) end of the line on the variable at the other (non-arrow) end, and two headed arrows represent correlations. Variances are indicated by two headed arrows beginning and ending on the same variables. Fixed model parameters are presented as numbers and freely estimated parameters are depicted by lower case letters. t1-t6 refer to the time in years from the baseline assessment to follow-up assessments 1-6.
The core measurement model in the bottom part of Figure 1 described the varying 3MS trajectories. Latent variables were defined to estimate baseline status (loadings of 1.0 for all seven assessments) and change (loadings corresponding to time of follow-up observation t1 – t6 which were allowed to vary by individual). In this model, the score for any individual at any time is represented by the sum of the 3MSINT latent variable, 3MSCH times the time for that assessment, and residual error (e.g. parameter d for 3MSBL). Model estimated means for 3MSINT and 3MSCH represent the average values in the total sample. Model estimated variances for these latent variables represent variability of of 3MSINT and 3MSCH around the overall means and the correlation between 3MSINT and 3MSCH was freely estimated (parameter c). In the structural part of the model in the upper part of Figure 1, 3MSINT and 3MSCH latent variables were regressed on external variables that included demographic and linguistic characteristics, baseline measures of cognition (Verbal Memory, Object Naming), and baseline independent functioning (IQCODE).
The structural part of the model relating 3MSINT and 3MSCH to external variables was evaluated in several sequential steps. In Step 1, the association of demographic variables with 3MS baseline and change was examined. Effects of baseline neuropsychological variables (Verbal Memory and Object Naming) on 3MS baseline and change were evaluated in Step 2, and then effects of neuropsychological variables in conjunction with demographic variables were evaluated in Step 3. Effects of independent function (IQCODE) were evaluated in Step 4, followed by joint effects of IQCODE and demographic variables in Step 5. A final joint model (Step 6) assessed the independent associations of the demographic factors, baseline neuropsychological function, and functional status with baseline and longitudinal change in global cognitive impairment.
Latent variables models like the model used in this study can be conceptualized as multiple, simultaneously estimated linear regressions, and for example, each path depicted by a line in Figure 1 corresponds to a regression of the variable at the (arrow) end of the line on the variable at the (non-arrow) beginning of the line. The model parameters correspond to regression coefficients, means, intercepts, and variances. These coefficients divided by their standard errors are distributed as standard normal (z) statistics. In subsequent results, the coefficient divided by the standard error generated a z value (based on the sample of 639 in this study) that was compared to the standard normal distribution to determine statistical significance.
Maximum likelihood estimation was performed using the missing value analysis option within Mplus. This approach uses all cases including those with missing observations, and has been shown to provide unbiased estimation of model parameters if the missing data can be considered to be missing completely at random or missing at random [36]. Even under conditions of non-ignorable missingness, the maximum likelihood missing data analysis yields less bias in parameter estimates than an analysis restricted to cases with complete data [36]. In studies of cognitive aging, increasing cognitive impairment leading to inability to complete subsequent evaluations is a major concern that could result in non-ignorable missing data. This would be expected to result in under estimation of rate of cognitive decline in those who drop out, which would decrease statistical power for identifying predictors of cognitive decline. Missing at random is satisfied if patterns of missing data can be explained by observed variables that are explicitly in the model. The inclusion of multiple baseline measures of cognitive and functional status in models would minimize this type of bias since these are direct measures of impairment.
Maximum likelihood estimation is based on an assumption of multivariate normality of data. Because the 3MS was not normally distributed, the total number of errors (out of 100) was log transformed, inverted, and then rescaled to have a mean of 100 and standard deviation of 15 based on the baseline SALSA sample. For example, a score of 100 was at the sample average and a score of 115 corresponded to one standard deviation above the mean. Secondary analyses were performed using a robust distribution free estimator to verify that results were not biased by potential deviations from multivariate normality.
Results
A total of 760 participants were enrolled in the study and had baseline cognitive testing. Of those, 688 individuals completed at least one follow-up evaluation. Forty-one of this 688 had missing data for at least one of the covariates in this study (age, education, gender, acculturation, language of administration), yielding a total sample of 639. Six follow-up evaluations were completed by 217 of the 639, 115 completed five follow-ups, 77 had four follow-ups, 86 had three, 72 had two follow-ups, and 72 had one follow-up. The average age of the sample at baseline was 70.1 (SD = 6.7). Individuals were allowed to decide which language they preferred for testing; 63% were tested in Spanish, the remainder in English. The mean acculturation level was 42 (SD = 12.7). Scores on this scale ranged from 7 (Mexican oriented) to 62 (Anglo-oriented), indicating a wide distribution of acculturation levels. The mean level of education for this sample was quite low (mean = 7.3, SD = 5.5), with more than 50% of the sample having less than a high school education. However, the education level spanned a very wide range from zero years of formal education to post-graduate studies. Mean baseline scores for the cognitive and functional predictor variables are included in Table 1. At baseline, 88% of the sample was cognitively normal and 12% had mild cognitive impairment or dementia.
Table 1.
Baseline cognitive and functional scores.
| Mean score (standard deviation) | Range of scores | |
|---|---|---|
| Episodic Memory | -0.13 (0.80) | -2.83 to 1.81 |
| Confrontation Naming | -0.42 (0.95) | -3.64 to 3.16 |
| IQCODE | 3.21 (0.32) | 2.16 to 5.00 |
Episodic Memory and Confrontation naming are reported as standard z-scores with a mean of 0 and standard deviation of 1. IQCODE scores are reported as raw scores.
Demographic predictors of global cognition
First, we examined baseline demographic variables in association with baseline and change in global cognitive functioning, as measured by the 3MS. In a model that included all the demographic variables (age, education, gender, language of test administration, acculturation), older age (in years; coefficient (standard error) = -0.40 (0.06), z=-6.90, n=639, p <.001), being tested in English (-2.82 (1.21), z=-2.32, n=639, p=.02), and Anglo acculturation (-0.10 (0.05), z=-2.00, n=639, p = .05) were associated with poorerbaseline global cognitive function, while higher education (in years; 1.27 (.09), z=13.87, n=639, p<.001) was associated with better performance. When these same demographic variables were examined in relation to longitudinal change in global cognitive status, older age at baseline (-0.09 (.01), z=-7.67, n=639, p = <.001) was associated with a faster rate of decline on the 3MS over time and male gender (0.30 (.16), z=1.96, n=639, p = .05) was associated with slower decline.
Baseline neuropsychological predictors of global cognition
Next, baseline measures of specific neuropsychological tests were examined in association with baseline and change in global cognitive function. Baseline 3MS was positively related to baseline Verbal Memory (standard score units; 5.84 (0.44), z=13.27, n=639, p<.001) and Object Naming (standard score units; 6.88 (0.37), z=18.88, n=639, p<.001). Furthermore, baseline performance in Verbal Memory (0.36 (0.11), z=3.41, n=639, p=.001) and Object Naming (0.39 (0.09), z=4.55, n=639, p<.001) were independently associated with 3MS change, with lower cognitive scores predicting greater decline. When the demographic variables and the neuropsychological variables were included in a joint model, both neuropsychological variables remained associated with baseline global cognition (Verbal Memory (5.48 (0.46), z=11.92, n=639, p<.001), Object Naming (5.31 (0.46), z=11.48, n=639, p<.001)), along with years of education (0.72 (0.08), z=9.03, n=639, p<.001), and being tested in English (-3.15 (0.97), z=-3.24, n=639, p=.001). However, when predicting longitudinal change in global cognition, baseline Verbal Memory was no longer a significant predictor (0.20 (0.12), z=1.72, n=639, p = .09). Worse Object Naming remained significantly associated with faster decline in global cognition (0.24 (0.11), z=2.14, n=639, p = .03) along with older age (-0.08 (0.01), z=-6.11, n=639, p < .001); male gender (0.32 (0.16), z=2.01, n=639, p = .04) continued to be associated with improving performance.
Baseline functional status (IQCODE) as a predictor of global cognition
Degree of everyday functional impairment at baseline, measured by the IQCODE, was also examined in association with baseline and change in global cognitive status. Poorer baseline functional status was associated with poorer baseline 3MS (-10.98 (1.51), z=-7.30, n=639, p < .001). Greater baseline functional impairment was also strongly associated with a more rapid decline in global cognitive function over time (-1.36 (0.29), z=-4.65, n=639, p < .001). When demographic variables were added to the model, more impaired daily function on the IQCODE remained a strong predictor of longitudinal decline in global cognition (-0.98 (0.27), z=-3.58, n=639, p < .001), along with older age (-0.09 (0.01), z=-7.33, n=639, p < .001); being male was associated with less cognitive decline (0.33(0.15), z=2.18, n=639, p = .03).
Multivariate model: demographic, baseline cognitive and functional measures as predictors of global cognition
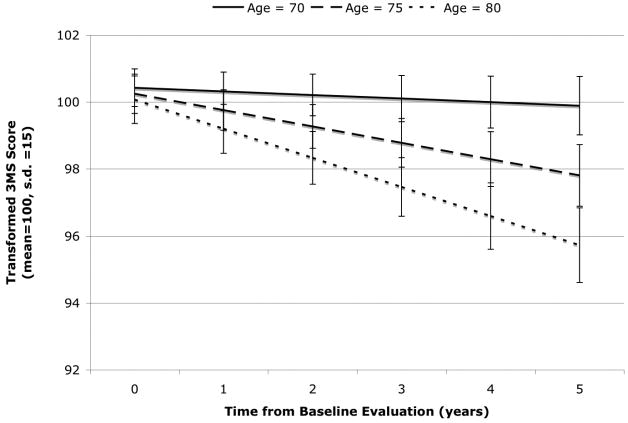
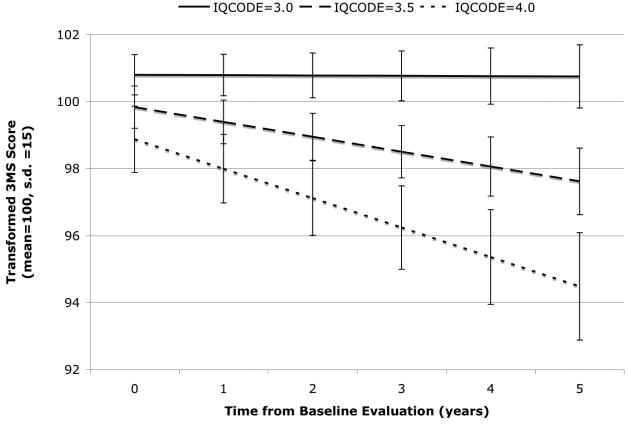
Finally, a joint model, including all of the demographic variables, the neuropsychological variables, and the IQCODE, was used to examine the independent predictors of baseline and change in global cognitive status. Continuous independent variables were standardized so that effect sizes of the various variables could be directly compared; the coefficients in this case show the change in 3MS baseline or change associated with a 1.0 s.d. difference in the independent variable. Lower education, being tested in English, and poorer performance on both Verbal Memory and Object Naming were all independently associated with poorer baseline global cognitive function (Table 2). Older age, being female, having more functional impairment (IQCODE) at baseline, and having poorer Object Naming were independently associated with greater longitudinal decline in global cognitive function over time (Table 3). The significant relationship between older age and progressive cognitive decline on the 3MS is illustrated in Figure 2, which shows expected trajectories in rate of decline for three specific ages. Figure 3 models the predicted longitudinal trajectories in cognitive decline for three different IQCODE scores.
Table 2. Independent effects of baseline demographic, neuropsychological, and functional predictors on estimated baseline global cognitive function.
| Coefficient | S.E. | P values | |
|---|---|---|---|
| Education (standardized) | 4.00 | 0.44 | 0.001 |
| Male | 0.90 | 0.66 | 0.18 |
| English Language | -3.04 | 0.97 | 0.002 |
| Acculturation (standardized) | 0.48 | 0.52 | 0.35 |
| Age (standardized) | -0.24 | 0.34 | 0.47 |
| Object Naming (standardized) | 4.99 | 0.45 | 0.001 |
| Verbal Memory (standardized) | 4.24 | 0.38 | 0.001 |
| IQCODE (standardized) | -0.61 | 0.33 | 0.07 |
Note. Global cognitive function was measured by the transformed 3MS which has a mean of 100 and a standard deviation of 15 in the study sample. Coefficients represent the difference in estimated baseline 3MS associated with a one unit difference in the independent variable. Coefficients divided by their standard errors have a standard normal (z) distribution and were compared to the standard normal table to determine statistical significance (N = 639). Continuous independent variables were standardized based on the study sample, Male (male=1, female=0) and English Language (English=1, Spanish=0) were dichotomous indicator variables.
Table 3. Baseline demographic, neuropsychological, and functional predictors of change in global cognitive function.
| Coefficient | S.E. | P Values. | |
|---|---|---|---|
| Education (standardized) | 0.04 | 0.10 | 0.70 |
| Male | 0.33 | 0.16 | 0.04 |
| English Language | 0.07 | 0.23 | 0.77 |
| Acculturation (standardized) | -0.03 | 0.13 | 0.83 |
| Age (standardized) | -0.52 | 0.09 | 0.001 |
| Object Naming (standardized) | 0.22 | 0.11 | 0.04 |
| Verbal Memory (standardized) | 0.10 | 0.09 | 0.30 |
| IQCODE (standardized) | -0.28 | 0.09 | 0.001 |
Note. Global cognitive function was measured by the transformed 3MS which has a mean of 100 and a standard deviation of 15 in the study sample. Coefficients represent the difference in estimated baseline 3MS associated with a one unit difference in the independent variable. Coefficients divided by their standard errors have a standard normal (z) distribution and were compared to the standard normal table to determine statistical significance (N = 639). Continuous independent variables were standardized based on the study sample, Male (male=1, female=0) and English Language (English=1, Spanish=0) were dichotomous indicator variables.
Figure 2.
Independent effects of age on 3MS baseline and linear rate of change. Results show model derived trajectories for three specific baseline ages (70, 75, and 80 years). The lines correspond to the expected average 3MS score at each time point. Bars show standard errors of the expected means at six time points (0, 1, 2, 3, 4, and 5 years).
Figure 3.
Independent effects of IQCODE on 3MS baseline and linear rate of change. Results show model derived trajectories for three specific baseline IQCODE scores (3.0, 3.5, and 4.0). The lines correspond to the expected average 3MS score at each time point. Bars show standard errors of the expected means at six time points (0, 1, 2, 3, 4, and 5 years).
Conclusions
The aim of the present study was to identify factors that help to determine which individuals are likely to be in the midst of a declining cognitive trajectory. A major finding was that the degree of everyday functional impairment at baseline (as measured by the IQCODE) is a strong predictor of future decline in global cognition and this was independent of demographic factors. Currently, it is not well understood whether impairments in cognition and daily function develop simultaneously, or whether some degree of cognitive loss precedes declines in everyday function. However, reductions in everyday abilities are intuitively expected to be the real-world expression of even early, mild cognitive decline [42]. In fact, a few studies have shown that mild changes in everyday function can be detected in preclinical stages of neurodegenerative disease [10-12] and therefore can predate a diagnosis of dementia. In large part, the detection of functional problems depends on the sensitivity of the functional scale used. The IQCODE, used as an index of informant-reported daily function in this study, not only includes items related to traditional functional domains (i.e. instrumental activities of daily living such as handling money for shopping) but also includes items that assess ‘everyday cognition’ (cognitively based functional abilities such as remembering where things are kept around the house), which have been shown to be particularly sensitive to very early functional problems [15]. Results from the present study help to confirm a few other previous studies showing greater impairment in functional abilities at baseline is associated with greater risk of future cognitive decline and disease progression [43] [42]). The present study expands previous findings by showing that such findings hold true in a sample of Hispanic older adults, many of whom are Spanish speakers for whom comprehensive neuropsychological testing may not be readily available. Furthermore, results suggest that, at least in this population, baseline functional impairment may be a more sensitive indicator of future risk of cognitive decline than neuropsychological tests. This may be partially accounted for by the fact that while neuropsychological test performance can be strongly influenced by background demographic factors such as education and cultural background, measures of everyday function tend to be much less affected by these non-disease factors [14, 15, 28]. In support of this idea, the ability of baseline verbal memory to predict longitudinal cognitive decline was eliminated once demographic variables were included in the model, but the association between baseline IQCODE and longitudinal cognitive decline was independent of demographic factors.
In several of the models, various demographic variables, including education and language of test administration, were associated with baseline global cognition. This finding is consistent with a large body of literature demonstrating that education can have strong influences on cross-sectional cognitive test results. Such relationships can lead to erroneous conclusions about the presence of disease in minority individuals and potential over-diagnosis of cognitive impairment/dementia [6-8]. In the context of low education, low cognitive scores are not synonymous with ‘impairment.’ In a similar vein, but not as intuitively obvious, we found that being testing in English was also associated with poorer baseline cognitive function. We believe the explanation for this finding is that at least one-third of those who chose to be tested in English reported Spanish as their first language. For these participants, being tested in their second language likely put them at a disadvantage in terms of their performance on the cognitive measures. An important point though is that neither education nor language of test administration were associated with a faster rate of change in cognition in any of the models (including the final joint model). Such findings underscore the importance of longitudinal (as compared to cross-sectional) evaluation in educationally and ethnically diverse samples both in clinical and research contexts to better understand disease related effects.
There are a number of limitations to this study that deserve mention. The current study focused on one particular minority group, namely Hispanics primarily of Mexican decent. Hispanics make up a growing minority group and better methods to identify and monitor early signs of a neurodegenerative disease in this group are badly needed. However, the current results may not generalize to other Hispanic/Latino groups and/or to other ethnic minorities, particularly those that are English speaking and/or have higher rates of literacy and/or education.
Additionally, there may be other baseline variables that were not included in the current study that could be important predictors of longitudinal change in cognition. Baseline measures of executive functioning were not include in this study and may be important predictors of decline based on other studies [47]. Additionally, neuropsychiatric symptoms have been associated with longitudinal decline in cognition in some studies. However, when we added a measure of depression (CES-D) to the final joint model, depression was related to baseline global cognition, but not change (results not shown).
The results of this study have important clinical implications. Informant-based ratings of functional impairment have significant utility in identifying those individuals who are more likely to be suffering from a neurodegenerative disease process. While neuropsychological testing can also be helpful in predicting longitudinal decline, it is not always accessible, particularly for non-English speakers. Additionally, representative normative values for neuropsychological tests are often not available for minority individuals. Informant ratings of daily function are relatively easy to acquire in clinical settings and show significant value in identifying individuals at increased risk of future cognitive decline.
Acknowledgments
Sources of support: NIA grants AG 12975, AG 10129, and AG 10220, AG 21511.
Grant support was provided by the National Institutes of Health/National Institute of Aging (NIA grants AG 12975, AG 10129, and AG 10220, AG 21511). The authors would also like to thank the participant volunteers and study partners without whom this research would be impossible.
Appendix. Sample Items of the IQCODE
Recalling a conversation a few days later.
Remembering where things are usually kept.
Remembering the names of family and friends.
Learning to use new machines around the house.
Understanding articles in newspapers or magazines.
Following a story in a book or on TV.
Composing letters to relative or friends or for business purposes.
Handling money for shopping.
Footnotes
No disclosures to report
Previous Presentations: This paper was presented as a poster presentation at the International Conference on Alzheimer's Disease (ICAD) in Chicago, 2008.
References
- 1.Berastein R. US Census Bureau News. Washington, DC: 2005. Hispanic population passes 40 million, Census Bureau reports [press release] [Google Scholar]
- 2.Fitzpatric A, Kuller L, Ives D, Lopez O, Jagust W, Breitner J, Jones B, Lyketsos C, Dullberg C. Incidence and prevalence of demenita in the Cardiovascular Health Study. J Am Geriatr Soc. 2004;52:195–204. doi: 10.1111/j.1532-5415.2004.52058.x. [DOI] [PubMed] [Google Scholar]
- 3.Sandberg G, S W, Smialek J, Troncoso J. The prevalence of the neuropathological lesions of Alzheimer's disease is independent of race and gender. Neurobiol Aging. 2001;22:169–175. doi: 10.1016/s0197-4580(00)00236-0. [DOI] [PubMed] [Google Scholar]
- 4.Tang M, Cross P, Andrews H, Jacobs D, Small S, Bell K, Merchant C, Lantigua R, Costa R, Stern Y, Mayeux R. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology. 2001;56:49–56. doi: 10.1212/wnl.56.1.49. [DOI] [PubMed] [Google Scholar]
- 5.Gurland B, Wilder D, Lantigua R, Stern Y, Chen J, Killeffer E, Mayeux R. Rates of dementia in three ethnoracial groups. Int J Geriatr Psychiatry. 1999;14:481–493. [PubMed] [Google Scholar]
- 6.Ramirez M, Teresi JE, Silver S, Holmes D, Gurland B, Lantigua R. Cognitive assessment among minority elderly: Possible test bias. Journal of Mental Health and Aging. 2001;7:91–118. [Google Scholar]
- 7.Manly J, Jacobs D, Sano M, Bell K, Merchant C, Small S. Cognitive test performance among nondemented elderly African Americans and whites. Neurology. 1998;50:1238–1245. doi: 10.1212/wnl.50.5.1238. [DOI] [PubMed] [Google Scholar]
- 8.Gasquoine P. Variables moderating cultural and ethnic differences in neuropsychological assessment: The case of Hispanic Americans. Clin Neuropsychol. 1999;13:376–383. doi: 10.1076/clin.13.3.376.1735. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Rev. 3rd. Washington DC: American Psychiatric Association; 1987. [Google Scholar]
- 10.Jefferson A, Byerly L, Vanderhill S, Lambe S, Wong S, Ozonoff A, Karlawish J. Characterization of activities of daily living in individuals with mild cognitive impairment. Am J Geriatr Psychiatry. 2008;16:375–383. doi: 10.1097/JGP.0b013e318162f197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tomaszewski Farias S, Mungas D, Reed B, Harvey D, Cahn-Weiner D, DeCarli C. MCI is associated with deficits in everyday functioning. Alzheimer Dis Assoc Disord. 2006;20:217–223. doi: 10.1097/01.wad.0000213849.51495.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tam C, Lam L, Chui H, Lui V. Characteristic profiles of instrumental activities of daily living in Chinese older persons with mild cognitive impairment. Am J Alzheimers Dis other Demen. 2007;22:211–217. doi: 10.1177/1533317507301597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jorm AF, Jacomb PA. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Socio-demographic correlates, reliability, validity and some norms. Psychological Medicine. 1989;19:1015–1022. doi: 10.1017/s0033291700005742. [DOI] [PubMed] [Google Scholar]
- 14.Fur JL, Teng E, Lin KN, Larson EB, Wang SJ, Liu CY, Chou P, Kuo BI, Liu HC. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) as a screening tool for dementia for a predominantly illiterate Chinese popluation. Neurology. 1995;45:92–96. doi: 10.1212/wnl.45.1.92. [DOI] [PubMed] [Google Scholar]
- 15.Tomaszewski Farias S, Mungas D, Reed B, Cahn-Weiner D, Jagust W, Baynes K, DeCarli C. The measurement of everyday cognition (ECog): Scale development and psychometric properties. Neuropsychology. 2008;22:531–544. doi: 10.1037/0894-4105.22.4.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Del-Ser T, Morales JM, Barguero MS, Canton R, Bermejo F. Application of the Spanish version of the “Informant Questionnaire on Cognitive Decline in the Elderly” in the clinical assessment of dementia. Alzheimer Dis Assoc Disord. 1997;11:3–8. doi: 10.1097/00002093-199703000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Gonzales HM, Mungas D, Haan MN. A verbal learning and memory test for English- and Spanish-speaking older Mexican-American adults. The Clinical Neuropsychologist. 2002;16:439–451. doi: 10.1076/clin.16.4.439.13908. [DOI] [PubMed] [Google Scholar]
- 18.Hinton L, Haan MN, Geller S, Mungas D. Neuropsychiatric symptoms in Latino elders with dementia or cognitive impairment without dementia and factors that modify their association with caregiver depression. The Gerontologist. 2003;43:669–677. doi: 10.1093/geront/43.5.669. [DOI] [PubMed] [Google Scholar]
- 19.Haan MN, Mungas D, Gonzales HM, Ortiz TA, Acharya A, Jagust WJ. Prevalence of dementia in older Latinos: The influence of type 2 diabetes mellitus, stroke, and genetic factors. JAGS. 2003;51:169–177. doi: 10.1046/j.1532-5415.2003.51054.x. [DOI] [PubMed] [Google Scholar]
- 20.Teng E, Chui H. The modified Mini-Mental State (3MS) Examination. J Clin Psychiatry. 1987;48:314–318. [PubMed] [Google Scholar]
- 21.Folstein M, Folstein S, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 22.Bland R, Newman S. Mild dementia or cognitive impairment: Yhe Modified Mini-Mental State Examination (3MS) as a screen for dementia. Can J Psychiatry. 2001;46:506–510. doi: 10.1177/070674370104600604. [DOI] [PubMed] [Google Scholar]
- 23.McDowell I, Kristjansson B, Hill G. Community screen for dementia: The Mini-Mental State Exam (MMSE) and Modified Mini Mental State Exam (3MS) compared. J Clin Epidemiol. 1997;50:231–238. doi: 10.1016/s0895-4356(97)00060-7. [DOI] [PubMed] [Google Scholar]
- 24.Jagust W, Gitcho A, Sun F, Kuczynski B, Mungas D, Haan MN. Brain imaging evidence of preclinical Alzheimer's disease in normal aging. Ann Neurol. 2006;59:673–681. doi: 10.1002/ana.20799. [DOI] [PubMed] [Google Scholar]
- 25.Yaffe K, Haan MN, Blackwell T, Cherkasova E, Whitmer RA, West N. Metabolic syndrome and cognitive decline in elderly Lations: findings from the Sacramento Area Latino Study of Aging. J Am Geriatr Soc. 2007;55:758–762. doi: 10.1111/j.1532-5415.2007.01139.x. [DOI] [PubMed] [Google Scholar]
- 26.Ramos MI, Allen LH, Mungas D, Jagust W, Haan MN, Green R, Miller JW. Low folate status is associated wtih impaired cognitive function and dementia in the Sacrameto Area Lation Study on Aging. Am J Clin Nutr. 2005;82:1346–1352. doi: 10.1093/ajcn/82.6.1346. [DOI] [PubMed] [Google Scholar]
- 27.Cuellar I, Arnold B, Maldonado R. Acculturation rating scale for Mexican Americans-II: A revision of the original ARMS scale. Hispanic Journal of Behavioral Sciences. 1995;17:275–304. [Google Scholar]
- 28.Jorm AF, Scott R, Cullen JS, MacKinnon AJ. Performance of the Informant Questionnaire on Cognitive Decline in the Olderly (IQCODE) as a screening test for dementia. Psychological Medicine. 1991;21:785–790. doi: 10.1017/s0033291700022418. [DOI] [PubMed] [Google Scholar]
- 29.Jorm A, Korten E. Assessment of cognitive decline in the elderly by informant interview. British Journal of Psychiatry. 1988;152:209–213. doi: 10.1192/bjp.152.2.209. [DOI] [PubMed] [Google Scholar]
- 30.Morales JM, Gonzalez-Montalvo JI, Bermejo F, Del-ser T. The screening of mild dementia with a shortened Spanish version of the Informant Questionnaire on Cogntive Decline in the Elderly. Alzheimer Dis Assoc Disord. 1995;9:105–111. doi: 10.1097/00002093-199509020-00008. [DOI] [PubMed] [Google Scholar]
- 31.Jorm AF. A short form of the Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): Development and cross-validation. Psychological Medicine. 1994;24:145–153. doi: 10.1017/s003329170002691x. [DOI] [PubMed] [Google Scholar]
- 32.Tomaszewski Farias S, Mungas D, Reed B, Haan MN, Jagust W. Everyday functioning in relation to cognitive functioning and neuroimaging in community dwelling Hispanic and non-Hispanic older adults. J Int Neuropsychol Soc. 2004;10:342–354. doi: 10.1017/S1355617704103020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mungas D, Reed B, Crane P, Hann M, Gonzales H. Spanish and English Neuropsychological Assessment Scales (SENAS): Further development and psychometric characteristics. Psychological Assessment. 2004;16:347–359. doi: 10.1037/1040-3590.16.4.347. [DOI] [PubMed] [Google Scholar]
- 34.Mungas D, Reed B, Farias S, DeCarli C. Criterion-referenced validity of a neuropsychological test battery:Equivalent performance in elderly Hispanic and Non-Hispanic Whites. J Int Neuropsychol Soc. 2005;11:620–630. doi: 10.1017/S1355617705050745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mungas D, Reed B, Marshall S, Gonzales H. Development of psychometrically matched English and Spanish neuropsychological tests for older persons. Neuropsychol. 2000;14:209–223. doi: 10.1037//0894-4105.14.2.209. [DOI] [PubMed] [Google Scholar]
- 36.Baker FB. The basics of item response theory. Prtsmouth, NH: Heineman Publishing; 1985. [Google Scholar]
- 37.Hambleton RK, Swaminathan H. Principles and applications. Boston: Kluwer-Nijhoff Publishing; 1985. Item response theory. [Google Scholar]
- 38.Hambleton RK, Swaminathan H, Rogers HJ. Fundementals of item response theory. Newbury Park: Sage Publications; 1991. [Google Scholar]
- 39.Meredith W, Tiska J. Latent curve analysis. Psuchometrika. 1990;55:107–122. [Google Scholar]
- 40.McArdle JJ. Latent variable modeling of differences and changes with longitudinal data. Ann Rev Psych. 2009;60:577–605. doi: 10.1146/annurev.psych.60.110707.163612. [DOI] [PubMed] [Google Scholar]
- 41.Muthen LK, Muthen BO. MPlus: User's guide. second. Los Angeles: Muthen & Muthen; 2004. [Google Scholar]
- 42.Peres K, Chrysostome V, Fabrigoule C, Orgogozo J, Dartigues J, Bargerger-Gateau P. Restriction in complex activities of daily living in MCI: impact on outcome. Neurology. 2006;67:461–466. doi: 10.1212/01.wnl.0000228228.70065.f1. [DOI] [PubMed] [Google Scholar]
- 43.Purser J, Fillenbaum G, Wallace R. Memory complaint is not necessary for diagnosis of mild cognitive impairment and does not predict 10-year trajectories of functional disability, word recall, or short portable mental status questionnaire limitations. J Am Geriatr Soc. 2006;54:335–338. doi: 10.1111/j.1532-5415.2005.00589.x. [DOI] [PubMed] [Google Scholar]
- 44.Palmer K, Wang HX, Backamn L, Fratiglioni L. Differential evolution of cognitive impairment in nondemented older person: results from the Kungsholmen Project. Am J Psychiatry. 2002;159:435–442. doi: 10.1176/appi.ajp.159.3.436. [DOI] [PubMed] [Google Scholar]
- 45.Ritchie K, Artero S, Touchon J. Classification criteria for mild cognitive impairment: A population-based validation study. Neurology. 2001;56:37–42. doi: 10.1212/wnl.56.1.37. [DOI] [PubMed] [Google Scholar]
- 46.Feldman H, Jacova C. Mild cognitive impairment. Am J Geriatr Psychiatry. 2005;13:645–655. doi: 10.1176/appi.ajgp.13.8.645. [DOI] [PubMed] [Google Scholar]
- 47.Cahn-Weiner D, Tomaszewski Farias S, Julian L, Harvey DJ, Kramer JH, Reed B, Mungas D, Wetzel M, Chui H. Cognitive and neuroimaging predictors of instrumental activities of daily living. J Int Neuropsychol Soc. 2007;13:747–757. doi: 10.1017/S1355617707070853. [DOI] [PMC free article] [PubMed] [Google Scholar]