Abstract
Background
Previous studies have shown the usefulness of combining information from different data sources to identify and analyse variations in transfusion practices. Good knowledge of the conditions leading to blood use is a fundamental requirement for the assessment of the appropriateness of blood transfusion.
Materials and methods
In this study we combined blood transfusion data obtained from the Blood Bank information system with patients’ data from the Hospital Discharge Database, based on the ICD9 classification system, from 1,827 surgical procedures performed in seven different orthopaedic divisions in the Ravenna area between January and December 2009. Hip and knee replacement surgery (primary or revision) and operations following femoral fractures (partial hip replacement and reduction with internal fixation) were considered. For a subgroup of patients clinical and transfusion data were also combined with haemoglobin values obtained from the laboratory information system.
Results
Of the 1,827 surgical procedures, 1,038 (56.8%) were followed by transfusion of red cells. The likelihood of receiving a transfusion varied depending on the patient’s sex (49% for males, 60% for females), age, and on the surgical procedure, being higher for interventions following femoral fractures and for revisions of hip replacement: about 70% of patients undergoing these interventions required transfusion. A large variability in transfusion rates was observed between the seven divisions, which was only partially explained by the different types of surgery (post-traumatic or elective) performed by any of them: relevant variations were also observed for the same type of intervention.
Discussion
Combining information from different data sources could be a time-sparing way to gain useful information about transfusion practices, so contributing to optimising blood usage.
Keywords: blood transfusion, orthopaedics, surgery, benchmark, ICD9
Introduction
Assessment of the appropriateness of blood transfusion is a complex issue. Among the strategies available to improve the “right” use of blood components, “audit and feedback” is one of the most widely used1–4: this consists of periodic reviews of blood transfusion practices which are performed and discussed with clinicians in order to identify behaviours in contrast with the accepted guidelines.
Some reports have shown considerable differences in transfusion rates in surgical patients5,6: the analysis of these differences could help clinicians to improve their “transfusion behaviour”.
To obtain a useful comparison of transfusion rates, the groups of patients need to be homogeneous. Unfortunately, poor documentation of patients’ characteristics is often a major obstacle to a useful evaluation7–9. Studies investigating associations between defined surgical procedures (based on the ICD classification system) and blood component transfusions could help to clarify different transfusion behaviours10,11. In this study we analyse red cell use in patients who underwent surgery in seven different orthopaedic divisions in the Ravenna area.
Materials and methods
The Hospital Discharge Database was queried to identify patients undergoing surgery in one of the seven orthopaedic divisions operating in the Ravenna area (4 in public hospitals, 3 in private hospitals) between 1/1/2009 and 31/12/2009. The research was performed for the surgical procedures reported in Table I.
Table I.
Procedures.
| Procedure | ICD9-CM code |
|---|---|
| Partial hip replacement | 81.52 |
| Open reduction of fracture with internal fixation, femur | 79.35 |
| Total hip replacement | 81.51 |
| Revision of hip replacement | 00.70, 00.71, 00.72, 00.73, 00.76, 81.53 |
| Total knee replacement | 81.54 |
| Revision of knee replacement | 81.55 |
To calculate the transfusion rate for each procedure, the records retrieved were matched by surname, name and date of birth with the corresponding data of patients in the Blood Bank Database (Eliot Engineering, Cesena Italy) transfused with red cells concentrates, on the condition that the date of transfusion, for each patient, was between the day of surgery and 30 days later. Patients receiving autologous blood were excluded from the study. Patients undergoing revision of hip replacement, although registered with different ICD9 codes, were considered as a single group.
Statistical analyses were performed using computer software SPSS (SPSS Inc., Chicago, IL, USA) and SAS (SAS Institute Inc., Cary, NC, USA). Differences between categorical variables were analysed using the chi-square test whereas differences between numerical variables were analysed by Student’s t-test or analysis of variance. Statistical significances are shown for informational purposes only, given the observational nature of the study.
The associations between red cell transfusion and sex, age, type of intervention and facility in which the surgery was performed were tested by stepwise logistic regression analysis to calculate odds ratios and 95% confidence intervals. Total knee replacement was selected as the reference intervention as it was associated with the lowest transfusion rate and an adequate number of observations: revision of knee replacement, for which the transfusion rate was similar, was not selected as the reference because of the small number of cases. The same criterion was followed in selecting hospital A as the reference facility.
Results
In the period considered, 1,827 surgical procedures were performed in 1,787 patients (572 males and 1,215 females). The mean age of the patients was 74.4 years (range, 9–102 years): 70.1 years for males (range, 9–97) and 76.2 years (range, 15–102) for females. Overall, 1,038/1,827 (56.8%) interventions were followed by a red cell transfusion.
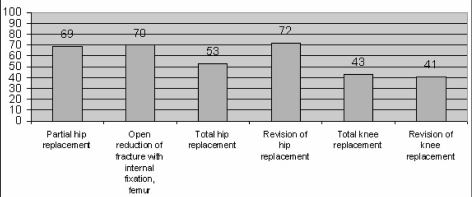
The percentage of transfused patients (shown in Figure 1 and subdivided for each procedure and for each hospital in Table II) varied according to the type of surgery: 69% for partial hip replacement (73% for males, 68% for females), 70% for open reduction of femoral fracture with internal fixation (61% for males, 73% for females), 53% for total hip replacement (41% for males, 63% for females), 72% for revision of hip replacement (67% for males, 76% for females), 43% for total knee replacement (36% for males, 46% for females), 41% for revision of knee replacement (56% for males, 31% for females). The overall percentage of patients requiring red cell transfusion varied greatly between hospitals, ranging from 28% to 74%. Similar between-hospital variations were observed analysing each intervention separately: 54%–77% for partial hip replacement, 50%–100% for internal fixation of femoral fracture, 26%–88% for total hip replacement, 50%–87% for revision of hip replacement, 12%–65% for knee replacement and 22%–100% for revision of knee replacement.
Figure 1.
Percentages of interventions followed by red cell transfusion.
Table II.
Interventions performed and followed by transfusion: distribution among hospitals.
| Hospitals (public-private): transfused/performed (percentage transfused) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Procedure | A(pri) | B(pub) | C(pub) | D(pub) | E(pub) | F(pri) | G(pri) | Total |
| Partial hip replacement | Not performed | 49/65 (75) | 47/87 (54) | 2/3 (67) | 87/113 (77) | Not performed | Not performed | 185/268 (69) |
| Open reduction of fracture with internal fixation, femur | 1/2 (50) | 81/110 (74) | 79/120 (66) | 2/2 (100) | 117/167 (70) | Not performed | Not performed | 280/401 (70) |
| Total hip replacement | 21/37 (57) | 31/37 (84) | 54/138 (39) | 24/50 (48) | 50/93 (54) | 64/73 (88) | 18/69 (26) | 262/497 (53) |
| Revision of hip replacement | 3/6 (50) | 3/4 (75) | 29/43 (67) | 5/7 (71) | 13/15 (87) | 15/18 (83) | 3/5 (60) | 71/98 (72) |
| Total knee replacement | 8/67 (12) | 16/29 (55) | 17/63 (27) | 15/23 (65) | 13/23 (56) | 120/195 (61) | 42/141 (30) | 231/541 (43) |
| Revision of knee replacement | 0/4 (0) | 3/3 (100) | 0/1 (0) | 0/1 (0) | 1/1 (100) | 3/3 (100) | 2/9 (22) | 9/22 (41) |
| Total | 33/116 (28) | 183/248 (74) | 226/452 (50) | 48/86 (56) | 281/412 (68) | 202/289 (70) | 65/224 (29) | 1,038/1,827 (57) |
With regards to total hip replacement the percentage of transfused patients was higher among patients undergoing the operation following a fracture(57/93, 61%) than among arthritic patients (205/404, 51%), although the difference was not statistically significant (p=0.08).
Patients were transfused more frequently in public than in private hospitals (62% versus 48%, p=0.0001), but this difference was no longer observed (52% versus 48%, p=0.2) when the interventions essentially performed only in public facilities (partial hip replacement and open reduction of femoral fracture with internal fixation) were excluded from the analysis.
Surgery in females patients was followed by red cell transfusion significantly more frequently than surgery in male patients: 751/1,243 (60%) versus 287/584 (49%), p=0.0001. The mean age of the transfused patients was higher than that of the patients who were not transfused (77.1 years versus 70.7 years, respectively; p=0.0001).
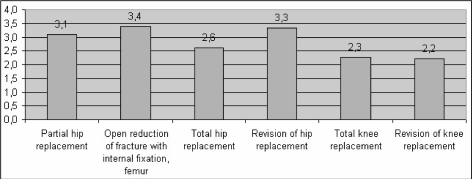
Overall, 2,993 units of red cell concentrate were transfused (mean 2.9 units, min. 1 - max. 18), with no differences for males and females. Figure 2 shows the mean number of units transfused for each intervention.
Figure 2.
Mean number of units transfused.
Results of the logistic regression analysis are reported in Table III: the dependent variable is transfusion status (transfused/not transfused), and the independent variables age, sex, intervention and hospital significantly improve the model fit.
Table III.
Transfusion likelihood - logistic regression analysis.
| Odds Ratio | 95% C.I. | p | |
|---|---|---|---|
| Age | 1.038 | 1.028 – 1.048 | 0.0001 |
| Sex | 0.0064 | ||
| Males | 1 | Reference | |
| Females | 1.361 | 1.090 – 1.699 | |
| Intervention | 0.0001 | ||
| • Total knee replacement | 1 | Reference | |
| • Revision of knee replacement | 1.359 | 0.546 – 3.336 | |
| • Total hip replacement | 2.044 | 1.527 – 2.735 | |
| • Partial hip replacement | 2.086 | 1.394 – 3.121 | |
| • Open reduction of fracture with internal fixation, femur | 2.958 | 2.050 – 4.268 | |
| • Revision of hip replacement | 4.776 | 2.832 – 8.054 | |
| Hospital | 0.0001 | ||
| • A | 1 | Reference | |
| • G | 1.214 | 0.724 – 2.036 | |
| • C | 1.325 | 0.816 – 2.152 | |
| • D | 2.511 | 1.361 – 4.634 | |
| • E | 2.839 | 1.709 – 4.715 | |
| • B | 3.754 | 2.181 – 6.462 | |
| • F | 6.869 | 4.173 – 11.306 |
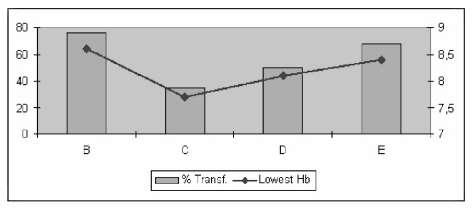
For a subgroup of 154 interventions performed in four public hospitals we retrieved information regarding haemoglobin values during hospital stay from the laboratory database. Eighty-four patients (54%) were transfused. Figure 3 shows the mean lowest haemoglobin values during hospital stay and the transfusion rate for each institution.
Figure 3.
Correlation between mean lowest haemoglobin values during hospital stay and percentage of patients receiving red cell transfusions.
Mean haemoglobin values at discharge were similar for the four institutions, ranging from 10.1 to 10.4 g/dL, and for transfused and not transfused patients (10.3 g/dL for both). No significant difference in the mean number of transfused units was observed between the hospitals (3, 2.8, 2.1 and 3.1 units for hospitals B, C, D and E, respectively, p=0.63).
Discussion and conclusions
As observed in previous studies, our data show relevant differences in red cell transfusion rates for patients undergoing orthopaedic surgery in different institutions. It is obvious that in order to be able to analyse these differences, a unique classification of diagnosis and interventions is needed. The Hospital Discharge Database, containing a standardised set of information based on the ICD system which must be entered for every patient discharged from public and private hospitals, seems to be of great help in minimising the difficulties deriving from the frequently poor documentation of transfusion episodes.
In this observational study, female patients were transfused more frequently than males and the likelihood of receiving a red cell transfusion rose with patients’ age, increasing nearly 4% per year of age.
Red cell transfusions were required more frequently in hip surgery than in knee surgery. The interventions performed following fractures (partial hip replacement and internal fixation of the femur) required transfusion more frequently than those performed in elective conditions: patients in the former group were, however, significantly older (80.5 years versus 70.8 years, p=0.0001) and more frequently females (74% versus 65%, p= 0.0001).
Patients undergoing surgery in public facilities were transfused more than those in private hospitals, probably because private hospitals perform only elective surgery. When the analysis was limited to the interventions performed in both type of facilities, the transfusion rate was similar despite the older age of patients in public facilities (72.1 years versus 69.7 years, p=0.0001).
Relevant differences in transfusion rates were observed for each intervention between the different institutions, and this is the main aspect to be discussed with involved clinicians: in particular, different “transfusion behaviours” should be analysed to exclude the possibility of a too liberal transfusion strategy. For this purpose, a further linkage with the laboratory information system could be of great help. To test this possibility, we retrieved data regarding haemoglobin values during hospital stay from the laboratory database for a small sample of the patients in the study. Interestingly, there seems to be a correlation between the mean of lowest value of haemoglobin concentration observed in transfused patients during hospital stay (which probably represented the transfusion trigger) and the transfusion rate: institutions in which the lower mean values were observed (that is, where clinicians waited for lower values before deciding to transfuse), seemed to have lower transfusion rates. Haemoglobin level at discharge was, however, similar between the hospitals and for transfused and non-transfused patients, seeming to suggest differences in blood loss rather than different transfusion behaviours.
In conclusion, combining data regarding transfusion from different electronic sources seems to be a useful and time-sparing way to evaluate the appropriateness of blood transfusion.
References
- 1.Jamtvedt G, Young JM, Kristoffersen DT, et al. Audit and feedback: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2006;(2):CD000259. doi: 10.1002/14651858.CD000259.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Bero LA, Grilli R, Grimshaw JM, et al. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. BMJ. 1998;317:465–8. doi: 10.1136/bmj.317.7156.465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grimshaw JM, Thomas RE, MacLennan G, et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess. 2004;8:1–72. doi: 10.3310/hta8060. [DOI] [PubMed] [Google Scholar]
- 4.Scott I. What are the most effective strategies for improving quality and safety of health care? Intern Med J. 2009;39:389–400. doi: 10.1111/j.1445-5994.2008.01798.x. [DOI] [PubMed] [Google Scholar]
- 5.Gombotz H, Rehak PH, Shander A, Hofmann A. Blood use in elective surgery: The Austrian benchmark study. Transfusion. 2007;47:1468–1480. doi: 10.1111/j.1537-2995.2007.01286.x. [DOI] [PubMed] [Google Scholar]
- 6.Maki T. Optimizing blood usage through benchmarking. Transfusion. 2007;47:145S–148S. doi: 10.1111/j.1537-2995.2007.01372.x. [DOI] [PubMed] [Google Scholar]
- 7.Friedman MT, Amber Ebrahim A. Adequacy of physician documentation of red blood cell transfusion and correlation with assessment of transfusion appropriateness. Arch Pathol Lab Med. 2006;130:474–9. doi: 10.5858/2006-130-474-AOPDOR. [DOI] [PubMed] [Google Scholar]
- 8.Moylan S, Szabo F, Scott H, Kwok G. Use of fresh-frozen plasma at Royal Darwin Hospital: a retrospective audit. Intern Med J. 2008;38:686–91. doi: 10.1111/j.1445-5994.2008.01730.x. [DOI] [PubMed] [Google Scholar]
- 9.Iorio A, Basile M, Marchesini M, et al. Audit of the clinical use of fresh-frozen plasma in Umbria: study design and results of the pilot phase. Blood Transfus. 2008;6:211–9. doi: 10.2450/2008.0042-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grazzini G. Clinical appropriateness of blood component transfusion: regulatory requirements and standards set by the Scientific Society in Italy. Blood Transfus. 2008;6:186–90. doi: 10.2450/2008.0049-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McClelland B. Clinical quality improvement information for transfusion practice. Transfusion. 2007;47:137S–141S. doi: 10.1111/j.1537-2995.2007.01370.x. [DOI] [PubMed] [Google Scholar]