Dear Editor,
Hepatitis B virus infection is highly endemic in Madagascar1. The last data about blood donation safety and hepatitis B were obtained in the late 1990s2, so it is important to update these data in order to determine the evolution in this viral infection and to estimate the current safety of blood donation in Madagascan healthcare structures.
The aim of this study was to determine the prevalence of hepatitis B surface antigen (HBsAg) among Antananarivo blood donors between 2003 and 2009. We did this by retrospectively examining all recorded data of blood donor candidates at the National Transfusion Centre (NTC) located in Antananarivo, the capital of Madagascar, from 2003 to May 2009. The reason why 2003 was chosen as the beginning of this study is that before this data screening for hepatitis B virus was performed using an enzyme linked immunosorbent assay (ELISA); in 2003, immunochromatographic testing was introduced, so the data from 2003 onwards are homogenous.
We included all first time blood donors (both new volunteer and replacement blood donors). The data considered included the age and sex of each donor and the results of blood serology screening.
Donor selection in the NTC was performed by physicians. The first step of blood donation consisted of interviewing each candidate using a predefined questionnaire with the aim of excluding candidates who had a potential risk of having an infectious diseases because of their behaviour and sexual attitudes and would, therefore, be at risk of transmitting such diseases through donated blood. Those who did not know anything about human immunodeficiency virus/acquired immune deficiency syndrome were counselled by the physicians.
A physical examination was then performed and, at this step, candidate donors were deferred if they had a systolic blood pressure higher than 180 mmHg, a heart rate faster than 120 bpm, a weight less than 48 kg or any clinical symptoms of dermatosis or anaemia (haemoglobin levels were not routinely assessed by biochemical or other techniques). Some donors were temporarily excluded on the basis of other criteria: women during menstrual bleeding, a person who had slept less than 4 hours prior to the proposed donation, recent alcohol drinking (within the preceding 72 hours), dental care within the last 6 months, and if the donor’s blood pressure was measured just after a physical effort.
For this study, a first time blood donor was identified as a donor who donated for first time.
Serum samples were screened for blood-borne infectious agents. Screening for HBsAg was performed using a rapid test (Virucheck® - Orchid Biomedical System, India) which had a sensitivity of 95.6% and specificity of 98.2%3. Virucheck is an immunochromatographic test which can be stored at 4 °C–30 °C and requires 100 μL of serum. The test result can be read in 15 minutes. The definitive result was obtained after a double readout, the first by the laboratory technician who performed the test, and the second by the physician. The national policy for blood donations does not involve either confirmatory tests or additional tests, so all reactive donations were excluded.
Prevalence rates were calculated using univariate analyses, and then bivariate analyses, using chi square testing, were performed with Excel and Epiinfo 2000 ver. 3.5.1 software (CDC, Atlanta, USA). Results with a p value less than 0.05 were retained as statistically significant.
Given the nature of the study, a retrospective review of blood donors, no informed consent of individuals included in the study was needed.
Results
About two-thirds of all donors who came to the NTS during the period of our study were first time blood donors. Overall, there were 47,636 first time donors from among whom we retained 47,597 individuals for this study. The others were excluded because of incomplete information on gender, age or serum screening. The mean age of our donors was 33.3±10.4 years (35.8±11.0 for males, and 32.6±10.1 for females) (p<0.05) and 62.38% of all donors were aged between 20 and 35 years. Most of the donors were male (38,299/47,597; 80.47%).
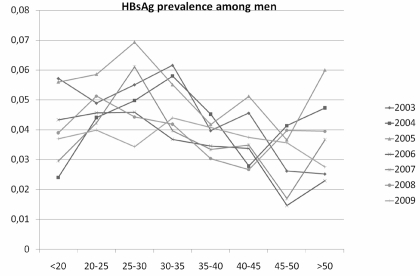
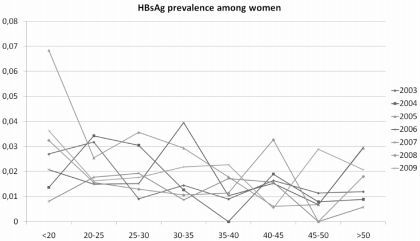
Throughout the whole study period 1,810 of the 47,597 first-time donors were found to be positive for HBsAg, for a prevalence of 3.84% (95% CI, 3.7 – 4.0). There was a significant relationship between age and HBsAg seropositivity (p<0.05 ), which, overall, decreased with age. In detail, HBsAg positivity increased with age up to 35 years, then decreased until 50 years of age, before increasing again after this age in both male and female donors (Figures 1 and 2).
Figure 1.
Prevalence of HBsAg among first time male donors in Antananarivo, Madagascar between 2003 and 2009.
Figure 2.
Prevalence of HBsAg among first time female donors in Antananarivo, Madagascar between 2003 and 2009.
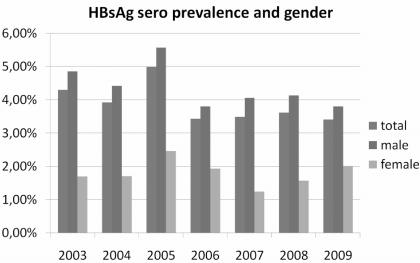
HBsAg-positive candidate donors were younger than HBsAg-negative ones (mean age: 31.7±9.7 versus 33.3±10.3 years) (p< 0.05). The prevalence of HbsAg positivity was higher among male candidate donors than among female ones (4.54% versus 1.80%, respectively) (p<0.05). The prevalence of HBsAg positivity in male donors appeared to decrease over time, whereas that in women remained relatively stable (Figure 3).
Figure 3.
Prevalence of HBsAg among all first time donors and male and female donors in Antananarivo, Madagascar between 2003 and 2009.
Discussion
Data are scarce about hepatitis B infection in Madagascar. In 1972, the prevalence of HBsAg was estimated to be 3%4. In 1996, the prevalence ranged from 5.3% in urban areas to 26.0% in rural areas in Madagascar2. The prevalence of HBV carriers was estimated to be less than 5% in the capital and about 23% in the general population and it was supposed that transmission during childhood and infancy are very high, with estimates of 10 to 35% in children less than 5 years old4.
Even though about two-thirds of our donors were replacement blood donors, the prevalence of HBsAg we found is not as high as that seen in other countries in West Africa where reported HBsAg prevalence rates ranged from 13.8 to 14.9% after the first step of screening5. Furthermore, the prevalence in our country has decreased slightly compared with previous data.
Our data showed that HBsAg positivity decreased with age. We thought that a possible reason for this was an inability of the immunochromatographic technique to detect occult hepatitis B infection and HBV carriers who had undetectable viral loads even if they were still infected.
Finally, we found that being male is a strong risk factor for hepatitis B virus infection among Madagascans, as usual in this particular population.
Our study has some potential limitations. First, we did not separate replacement donors from volunteer blood donors, so it was not possible to determine whether the prevalence of the HBsAg was the same within these two categories, or to show trends of HBV positivity among them. Secondly, the immunochromatographic technique used for screening HBsAg is not as sensitive as ELISA at detecting HBsAg mutants and it cannot detect very low HBsAg levels in the blood and can, therefore, give false negative results. Our hepatitis B virus screening using rapid testing may not, therefore, reveal the true prevalence of this disease. However, due to financial constraints and a lack of means, other tests for hepatitis B virus, such as anti-HBc and anti-HBs, are not available for routine screening of donors. The apparently negative donors may, therefore, have included some truly infected donors who were in the window period or in an early phase of acute infection.
Conclusion
Hepatitis B envelop surface HBsAg was found in 3.84% of first time blood donors in Antananarivo. The prevalence was highest in young people aged less than 35 years. It then decreased, probably due to occult hepatitis B infection and undetectable viral loads among HBV carriers. It is, therefore, essential to find other ways to improve blood safety by adding another test, such as anti-HBc testing, because there is currently no possibility of using a molecular technique in public health centres in Antananarivo.
Many campaigns also need to be carried out in Madagascar in order to sensitise the population about the importance of blood donation, especially volunteer donation instead of replacement donation, as recommended by the World Health Organization. Worldwide data indicate that volunteer donations are safer than replacement ones. Volunteer and non-remunerated blood donors currently account for about one-third of all donations and, although the total number of donors is increasing year by year, this only reflects the increasing need for blood transfusions, while new volunteer donors are rare.
References
- 1.Liaw YF, Chu CM. Hepatitis B virus infection. Lancet. 2009;373:582–92. doi: 10.1016/S0140-6736(09)60207-5. [DOI] [PubMed] [Google Scholar]
- 2.Boisier P, Rabarijaona L, Piollet M, et al. Hepatitis B virus infection in general population in Madagascar: evidence for different epidemiological patterns in urban and in rural areas. Epidemiol Infect. 1996;117:133–7. doi: 10.1017/s0950268800001229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Randrianirina F, Carod JF, Ratsima E, et al. Evaluation of the performance of four rapid tests for detection of hepatitis B surface antigen in Antananarivo, Madagascar. J Virol Methods. 2008;151:294–7. doi: 10.1016/j.jviromet.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 4.Migliani R, Rousset D, Rakoto-Andrianarivelo M, et al. Hepatitis B virus infection: a public health problem in Madagascar. Arch Inst Pasteur Madagascar. 2000;66:50–4. [PubMed] [Google Scholar]
- 5.Allain JP, Sarkodie F, Asenso-Mensah K, Owusu-Ofori S. Relative safety of first-time volunteer and replacement donors in West Africa. Transfusion. 2010;50:340–3. doi: 10.1111/j.1537-2995.2009.02444.x. [DOI] [PubMed] [Google Scholar]