Abstract
Purpose
It has been shown that a cumulative dose of ⩾87 Gy (EQD2) of external beam radiotherapy (EBRT) and image guided adaptive brachytherapy (IGABT) to the high risk clinical target volume (HR CTV) confer a local control rate >95% in locally advanced cervical cancer. This study examines the dose distribution within the HR CTV and intermediate (IR) CTV in patients with cervical cancer treated with definitive EBRT +/− concomitant chemotherapy and MRI-based IGABT between patients with local recurrence (LR) and patients in continuous complete local remission (CCLR).
Material and methods
From 1998 to 2010, 265 patients were treated with definitive EBRT +/− concomitant chemotherapy and IGABT. Twenty-four LRs were documented. For the statistical analysis all patients with LR were matched to patients in CCLR from our database according to the following criteria: FIGO stage, histology, lymph node status, tumour size and chemotherapy.
DVH parameters (D50, D90, D98, D100) were reported for HR CTV and IR CTV. In order to report the minimum dose in the region where the recurrence occurred, the HR CTV/IR CTV were divided into four quadrants on transversal planes. The minimum dose at the HR CTV/IR CTV contour was measured (within the corresponding quadrant closest to the LR) in the treatment planning system. A mean minimum point dose (MPD) was calculated by averaging these measurements on four consecutive slices at the level of the recurrence for each of the 4 brachytherapy fractions. EQD2 doses were calculated by summation of all BT and external beam therapy fractions.
For each matched patient in the control group the measurements were performed on the same quadrant and at the same level.
Results
Sufficient image data were available for 21 LRs. Eight central failures and 13 non-central failures were observed. The mean D90 and D100 for HR CTV were 77 Gy and 61 Gy for patients with LR and 95 Gy and 71 Gy for patients in CCLR, respectively (p < 0.01). The MPD for HR CTV was 72 Gy for patients in the LR arm and 99 Gy for patients in the CCLR arm (p < 0.01). In the LR arm seven patients had a D90 for HR CTV ⩾87 Gy, however, in only three patients the MPD was ⩾87 Gy.
Conclusion
This study demonstrated significant differences in local outcome according to the delivered dose. In 85% of the LRs systematic low dose regions with less than 87 Gy were found at HR CTV contour. Systematic low dose regions leading to local recurrence could be detected even if a D90 HR CTV ⩾87 Gy was applied. In addition to DVH parameters, inspection of the spatial dose distribution remains a key point in dose prescription.
Keywords: Cervical cancer, Image-guided adaptive brachytherapy, Local recurrences, DVH
Local tumour control is the major endpoint in image-guided adaptive brachytherapy (IGABT) [1]. Since the publication of the GEC-ESTRO recommendations [2,3] IGABT is becoming increasingly introduced into clinical practice. First monoinstitutional series demonstrated an increased therapeutic ratio when compared to conventional 2D X-ray based brachytherapy [4–7]. Previous reports from our group described a significant dependence of local tumour control on D90 and D100 for HR CTV. Especially the D90 for HR CTV seems to be a reliable parameter for predicting local tumour control and can be used in clinical practice. It was shown that if a D90 ⩾ 87 Gy is applied, a local tumour control rate greater than 95% is achievable. The D100 appears to be also an indicator for local tumour control but is highly dependent on uncertainties [8,9].
However, DVH parameters like the D90 and D100 for HR CTV always refer to the whole contoured volume irrespective of dose variations. This means that clinically relevant topographic (sub-)areas within the HR CTV such as lateral tumour extension in the parametrial space could be underrepresented or even not reflected by DVH parameters due to the heterogeneous dose profile in brachytherapy. It may be assumed that such short comings in the spatial dose distribution will impact on local tumour control.
The primary goal of the study is to retrospectively investigate the dose in the area where the local recurrence occurred and to determine whether a low dose detected by the DVH parameters is topographically related to the area of the LR and reflected by the regional dose in the area of LR. The regional dose in the area of the local recurrence will be compared to the dose delivered in a similar region in patients with complete continuous local remission (CCLR) within a matched pair analysis. The secondary goal is to report patterns of failure and clinical outcome. The tertiary goal is to analyse the feasibility and clinical relevance of the D50 and D98.
Material and methods
Patients and treatment
From 1998 to 2010, 265 patients with uterine cervical cancer were treated at the Medical University of Vienna with EBRT (+/− chemotherapy) and IGABT in curative intent. Until the end of 2010 24 LRs were documented. Inclusion criteria for this study were the availability of complete MRI or CT datasets at the time of diagnosis, at the time of each brachytherapy fraction and at the time of LR.
Intended treatment consisted of 45–50 Gy EBRT delivered in 25–28 fractions with or without concomitant cisplatin based chemotherapy (40 mg/m2 of body surface per week for five weeks) and three to six fractions of 5–7 Gy HDR brachytherapy using tandem ring applicators +/− interstitial needles and/or a combination of tandem and vaginal cylinders +/− interstitial needles. MRI imaging, contouring and treatment planning were performed as described in earlier publications [2,3,10–14]. Follow-up investigations including clinical examination and MRI and/or CT were performed every three months for the first two years and twice annually for the next three years. Hence, all LRs were assessed by clinical examination, imaging studies (MRI and/or CT) and additionally by biopsy, if accessible. If MRI was not available at the time of LR, CT together with clinical examination was accepted for the definition of the area of LR (quadrant and level).
Classification of patterns of failure
LRs were classified as central recurrence (1) if the LR was localized within the uterine cervix, the uterine corpus and/or within the upper vagina or (2) if the LR captured the whole small pelvis and a side-specific attribution was not possible. LRs were described as non-central in case of LR at the parametrial space, the pelvic wall and or distal vagina. Non-central recurrences located at the parametrial space and/or at the pelvic wall were distinguished into ipsilateral and contralateral recurrences. Non-central recurrences were classified as ipsilateral if the main tumour load outside the uterine cervix at the time of diagnosis and the LR were situated on the same side. Non-central recurrences were classified as contralateral if the main tumour load outside the uterine cervix at the time of diagnosis and the LR were situated on opposite sides.
DVH and point dose analysis
DVH parameters (D50, D90, D98, D100) for HR CTV and IR CTV were reported for all patients. In order to report the minimum dose in the region where the recurrence occurred, the target volumes were divided into four quadrants on transversal planes in a way, so that two quadrants covered each one complete parametrial side and the remaining two quadrants covered the spaces anterior and posterior to the cervix (Figs. 1 and 2). The minimum dose at the target volume contour was measured at the corresponding quadrant closest to the LR in the treatment planning system. These measurements were performed on four consecutive slices (the MRI-slice thickness was 0.5 cm) at the level of the recurrence for each brachytherapy fraction separately – for example in case of a non-central recurrence treated with four fractions of HDR brachytherapy, 4 × 4 minimum point doses per target volume were measured. A mean minimum point dose (MPD) was calculated by averaging these measurements. Biologically normalized EQD2 doses were calculated by summation of all four BT fractions and external beam therapy.
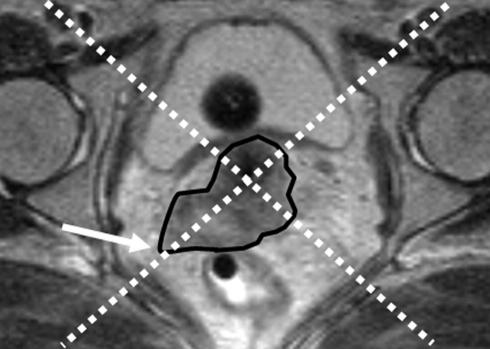
Fig. 1.
Example of the assessment of the minimum point dose based on the case presented in Fig. 2. T2-weighted MR image from the first brachytherapy fraction. The local recurrence was located on the right pelvic wall. The point dose assessment was performed correspondingly in the right quadrant. The white arrow indicates the area of the minimum point dose.
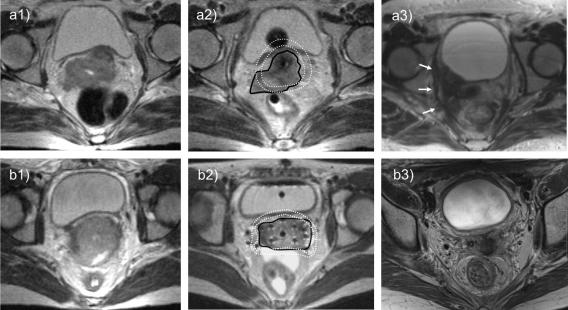
Fig. 2.
Example from the matched-pair analysis. Fig. 2a shows a patient from the local recurrence group and Fig. 2b shows the matched patient from the continuous complete remission group at the time of diagnosis (1), at the time of the first brachytherapy (BT) fraction (2) and with and without local recurrence (3). Both patients had a squamous cell carcinoma, staged as FIGO III with a maximum tumour diameter ⩾5 cm. Pelvic lymph nodes were involved in both cases. Both patients received concomitant cisplatin chemotherapy. The patient from Fig. 2a was treated with 45 Gy external beam radiotherapy (EBRT) and three fractions of intracavitary brachytherapy during the “learning period”. A substantial low dose region occurred in the right parametrial space. The local recurrence was located in the right pelvic wall corresponding to the low dose regions, as indicated by the white arrows. The D90 for HR CTV was 67.5 Gy and the MPD for HR CTV was 56.9 Gy. The patient from Fig. 2b was treated with 45 Gy EBRT and four fractions of combined intracavitary and interstitial BT. The HR CTV was sufficiently covered by the 7 Gy isodose-line. No local recurrence was reported until the time of analysis after a follow up time of 35 months. The D90 for HR CTV was 86 Gy and the MPD for HR CTV was 80 Gy. Black line – HR CTV. Inner white dotted line – 7 Gy isodose. Outer white dotted line – 5 Gy isodose.
In case of a central recurrence the MPD was calculated for both parametrial sides and the lower of these two values was taken as the final MPD – this means that for central recurrences in total eight minimum point doses (four on each parametrial side) were measured per fraction, however, only the MPD with lower dose was used.
Matched-pair analysis
To compare the MPD, DVH parameters and clinical outcome of all patients with LR to a comparable group of patients in CCLR, each patient with LR was matched to one patient in CCLR. The patient database at the Medical University of Vienna consists of 265 patients treated from 1998 to 2010 with definitive EBRT (+/− chemotherapy) and IGABT. Each patient with LR was matched to a specific patient in CCLR treated between 2001 and 2008 according to the following matching criteria: FIGO stage (any tumour stage), histology (any histology), lymph node status (positive vs. negative), tumour size (⩾5 cm vs. <5 cm) at diagnosis, chemotherapy (yes vs. no).
For each matched patient in the CCLR group the MPD was assessed following the same method as for patients with LR. The quadrant and the level for measuring the minimum point doses in patients in CCLR were defined according to the specific situation of the matched patient with LR in regard of the initial tumour spread and the topography of the LR – for example in case of a patient in CCLR matched to a patient with an ipsilateral non-central LR at a pelvic wall the MPD was calculated in the quadrant with the main parametrial involvement (“ipsilateral”).
Endpoints and statistical analysis
Descriptive statistics were performed for patient and treatment characteristics and patterns of failure. Gross tumour volume (GTV) at diagnosis was estimated by the maximum GTV diameters (anterior–posterior, latero-lateral, cranio-caudal) using the ellipsoid-formula (Volume = height × width × thickness × π/6). Mean values for MPD and DVH parameters for both groups were compared. A double-sided two-independent-samples t-test was used to identify any significant differences. Clinical outcome in terms of overall survival (OS) and cancer specific survival (CSS) was measured as previously described by Pötter et al. [4,5]. A p-value of <0.05 was considered statistically significant. All statistical analyses were performed using the SPSS 15.0 software (SPSS, Chicago, IL).
Results
Patient and treatment characteristics from matched-pair analysis
Patient characteristics from both groups are presented in Table 1. Three patients with LR had to be excluded because of insufficient imaging data. Hence, in total 21 patients with LR and 21 patients in CCLR were available for this study. In all patients except one with hip prosthesis at least one MRI-based treatment plan was available. If for some fractions no MRI was available, a CT was used together with the target volume information from the available MRI.
Table 1.
Patient characteristics from matched-pair analysis.
| Characteristic | LR [n = 21] | CCLR [n = 21] | p |
|---|---|---|---|
| Age [years {mean (range)}] | 52 (33–90) | 58 (38–85) | 0.17 |
| Histology [n] | |||
| Squamous cell carcinoma | 17 | 18 | 0.69 |
| Adenocarcinoma | 3 | 3 | 1.00 |
| Others | 1 | 0 | 0.32 |
| FIGO stage [n] | |||
| IB | 0 | 1 | 0.32 |
| IIA | 1 | 0 | 0.32 |
| IIB | 8 | 9 | 0.76 |
| IIIB | 10 | 9 | 0.76 |
| IVA | 2 | 2 | 1.00 |
| Tumour size [n] | |||
| Width < 5 cm | 3 | 3 | 1.00 |
| Width ⩾ 5 cm | 18 | 18 | 1.00 |
| Regional lymphnode involvement [n] | 12 | 12 | 1.00 |
| Concurrent chemotherapy [n] | 12 | 15 | 0.35 |
LR – local recurrence, CCLR – continuous complete remission.
Median follow-up was 17 months in LR-group and 24 months in the CCLR group. The distribution of (matched) prognostic factors was well balanced in both groups. There were no statistically significant differences in age, histology, FIGO stage, tumour size, regional lymph node involvement and delivery of concomitant chemotherapy. The mean volume of GTV at diagnosis was 75 cm3 ± 43 and 71 cm3 ± 79 in the LR and CCLR group, respectively (p = 0.841). The mean volume of HR CTV was 50 cm3 ± 22 and 47 cm3 ± 33 in the LR and CCLR group, respectively (p = 0.78). The total treatment time could not be matched and was significantly longer in the LR group (62 vs. 51 days, p = 0.03). In the LR group the application was performed in 17 patients with a tandem-ring applicator, in three patients with a combination of a tandem and a vaginal cylinder and in one patient with both tandem/vaginal cylinder and tandem-ring applicator. Eleven patients received additional interstitial needles. Overall a mean number of 2.5 ± 3 interstitial needles per application were used in the LR group. In the CCLR group the application was performed in 17 patients with a tandem-ring applicator, in two patients with a combination of a tandem and a vaginal cylinder and two patients with both tandem/vaginal cylinder and tandem-ring applicator. Fourteen patients received additional needles. Overall a mean number of 4.5 ± 4 interstitial needles per application were used in the CCLR group. The difference in the number of the interstitial needles between patients with LR and patients in CCLR was not statistically significant (p = 0.1).
Patterns of failure and clinical outcome
In eight patients a central recurrence and in 13 patients a non-central recurrence were observed. Nine of the non-central recurrences were ipsilateral recurrences and four were contralateral recurrences. Salvage treatment for patients with LR was surgery (n = 4), reirradiation (n = 3), chemotherapy (n = 9) and no treatment (n = 8). At the time of analysis 19/21 patients in the LR group had died due to tumour progression. The median time to LR was 10 months and the median time from LR to death was 7 months. In the CCLR group 6/21 patients died – five due to distant metastasis and one without any evidence of cervical cancer.
DVH-analysis and point dose analysis
All dose parameters are given in Table 2. The MPD for HR CTV was 72 Gy ± 13 Gy for patients in the LR arm and 99 Gy ± 20 Gy for patients in the CCLR arm (p < 0.01). The MPD for IR CTV was 58 Gy ± 6 Gy for patients in the LR arm and 73 Gy ± 6 Gy for patients in the CCLR arm (p < 0.01). The mean D90 and D100 for HR CTV were 77 Gy ± 12 Gy and 61 Gy ± 7 Gy for patients with LR and 95 Gy ± 10 Gy and 71 Gy ± 7 Gy for patients in CCLR, respectively (p < 0.01). The mean D90 and D100 for IR CTV were 64 Gy ± 6 Gy and 54 Gy ± 4 Gy for patients with LR and 76 Gy ± 6 Gy and 60 Gy ± 5 Gy for patients in CCLR, respectively (p < 0.01).
Table 2.
Dose analysis from matched-pair analysis.
| Parameter | LR [n = 21] | CCLR [n = 21] | p |
|---|---|---|---|
| Doses to HR CTV [Gyαβ10 {mean (st. dev.)}] | |||
| MPD | 72 (±13) | 99 (±20) | <0.001 |
| D100 | 61 (±7) | 71 (±7) | <0.001 |
| D98 | 67 (±8) | 80 (±8) | <0.001 |
| D90 | 77 (±12) | 95 (±10) | <0.001 |
| D50 | 121 (±30) | 146 (±20) | <0.001 |
| Doses to IR CTV [Gyαβ10 {mean (st. dev.)}] | |||
| MPD | 58 (±6) | 73 (±6) | <0.001 |
| D100 | 54 (±4) | 60 (±5) | <0.001 |
| D98 | 57 (±5) | 66 (±6) | <0.001 |
| D90 | 64 (±6) | 76 (±6) | <0.001 |
| D50 | 95 (±17) | 115 (±13) | <0.001 |
| D90 for HR CTV ⩾87 Gy [n] | 7 | 17 | – |
| MPD for HR CTV ⩾87 Gy [n] | 3 | 17 | – |
LR – local recurrence, CCLR – continuous complete remission, HR CTV – high risk clinical target volume, IR CTV – intermediate risk clinical target volume, MPD – mean minimum point dose.
In the LR arm 7 patients had a D90 for HR CTV ⩾ 87 Gy, however, in only 3 patients the MPD for HR CTV was ⩾87 Gy. The mean difference between the D90 for HR CTV and the MPD for HR CTV was 6 Gy ranging from −5 to 17 Gy.
The mean MPD of HR CTV was 83 Gy ± 10 Gy for true central recurrences and 65 Gy ± 5 Gy for whole small pelvis recurrences. The mean MPD of the HR CTV for ipsilateral LR (n = 9) was 66 Gy ± 9 Gy, however, for contralateral LR (n = 4) 91 Gy ± 7 Gy (Table 3).
Table 3.
Patterns of failure.
| No. of patients | MPD [Gyαβ10 {mean (st. dev.)}] | |
|---|---|---|
| Central recurrence | 8 | 69.5 (±9.9) |
| True central | 2 | 83.3 (±9.3) |
| Whole small pelvis | 6 | 65.0 (±4.5) |
| Non-central recurrence | 13 | 73.5 (±14.8) |
| Ipsilateral | 9 | 65.6 (±9.2) |
| Contralateral | 4 | 91.2 (±7.1) |
MPD – mean minimum point dose.
Discussion
The heterogeneous dose distribution and the steep dose fall off make dose reporting a critical issue in brachytherapy. For cervical cancer it was shown that the use of DVH parameters related to the individual target volume (D90, D100 for HR CTV) is more appropriate in predicting local control than the use of point doses (Point A + B) related to the applicator [15,16]. However, these DVH parameters have limitations: The D100 for HR CTV reflecting the minimum dose within the target is known to be highly influenced by uncertainties [8,9]. Any part/voxel of the target volume contributes to the D100 independently of its clinical relevance. Further on, the localization of the minimum dose may vary in the target especially if multiple applications with different implants are necessary. The D90 for HR CTV reflecting the minimum dose of the most irradiated 90% of the target was reported to be a clinically more reliable parameter. However, since the D90 does not refer to the whole target, low dose regions within the target representing major residual tumour may be hidden. Based on this background the study was initiated to investigate for the first time the local dose in the area of recurrence in patients with locally relapsed cervical cancer treated by EBRT (+/− chemotherapy) and IGABT. The dose in the area of LR was assessed using a newly introduced methodology and was compared to the dose derived from patients in CCLR within a matched pair analysis. Additionally several DVH parameters were analysed. It has to be stated that the MPD is rather an approximation representing a surrogate than a precise value. No information in regard of the volume the low dose region can be derived from the MPD. The mean MPD in the area of the LR was 72 Gy for HR CTV and 58 Gy for IR CTV. In contrast, the mean MPD for patients in CCLR was 99 Gy for HR CTV and 73 Gy for IR CTV. This difference in dose between patients in LR and CCLR was statistically significant. The value of 99 Gy for HR CTV in patients in CCLR was high, which was mainly related to loaded interstitial needles at or close to the HR CTV border, resulting in high physical doses and even higher biologically normalized doses.
In accordance to the MPD statistically significant differences between the LR and CCLR group were found for all investigated DVH parameters for both HR CTV and IR CTV. The differences were most pronounced for the D50 – with correspondingly very high standard deviations – whereas the least difference was found for the D100. The intention to investigate the D50 was based on the assumption that high dose regions within the target may have an additional impact on the local outcome. However, in this limited material it was not possible to detect an independent importance of the D50. The D98 seems to be an interesting alternative to the D100 since uncertainties in the DVH sampling might be less influencing. Further investigations will be necessary to determine the role of the D98. Regarding the various DVH parameters it seems that currently the D90 remains the most reliable indicator for predicting local tumour control.
All of the 13 patients in the LR group with a D90 for HR CTV <87 Gy showed a MPD of <87 Gy. According to this agreement, in these patients, it seems that the low dose detected by the DVH parameter could also be topographically related to the area of LR. Subsequently the remaining seven patients with LR showed a D90 for HR CTV ⩾ 87 Gy. However, in four out of these seven patients with a D90 for HR CTV ⩾ 87 Gy the MPD for HR CTV was <87 Gy. This indicates that areas with a low dose can occur even with high values of the D90 for HR CTV, if these low dose regions are systematically located in the missing 10% of the target volume. In total, differences of up to 17 Gy were found between the D90 for HR CTV and the MPD for HR CTV in the LR group. In contrast, 17 patients in the CCLR arm had a D90 and MPD for the HR CTV ⩾ 87 Gy.
Thirteen of 21 patients from the LR group were treated in the “learning period” as described by Pötter et al. [4,5] from 1998 to 2001. In this period – even though MRI based treatment planning was performed – patients were treated without prospective contouring using a standardized target definition and only with very limited dwell time optimization for increasing the target coverage. The use of additional interstitial needles in order to increase and shape the treated volume was limited. Although sometimes high D90 have been achieved, the spatial dose distribution was not optimized appropriately to the target volume. The nonstandardized fractionation scheme varied in this period and caused for several cases a prolonged treatment time. Therefore, the total treatment time could not be matched to patients treated within the “protocol period” [4,5] and was statistically significantly longer in LR group than in the CCLR group. This is a limitation of the study, however, this means that the differences in delivered dose in time for the two patient groups are probably even more pronounced due to radiobiological effects.
The analysis of the different patterns of failure revealed that whole small pelvis recurrences and non-central ipsilateral recurrences had a mean MPD of ∼65 Gy. In these patients it seems that the occurrence of the local failure was mainly related to low dose regions within the target. In contrast, true central recurrences and non-central contralateral recurrences had a mean MPD ranging from 83 Gy to 91 Gy. No substantial low dose regions could be found in these patients. It can be assumed that in these cases other (biological?) factors than dose may be predominant, which would be in accordance with the literature about cervical cancer indicating radioresistance [17].
In regard of the similar volume of the HR CTV in the LR and CCLR groups, the main reasons for the differences in dose between the two groups can be found in the systematic and optimized application of interstitial needles in the CCLR group leading to better coverage of the target volume in patients with large target volumes and/or unfavourable topography of the target.
Conclusions
This study demonstrated significant differences in local outcome according to the delivered dose. In 85% of the LRs systematic low dose regions with less than 87 Gy were found at the HR CTV contour. Systematic low dose regions leading to LR could be detected even if a D90 for HR CTV ⩾ 87 Gy was applied. However, regarding the various DVH parameters the D90 remains the most reliable predictor for local tumour control. In addition to DVH parameters, inspection of the spatial dose distribution remains a key point in dose prescription.
Conflict of interest notification
The Department of Radiotherapy at the Medical University of Vienna receives/received financial and/or equipment support for research and educational purposes from Nucletron B.V., Varian Medical Systems, Inc., and Isodose Control B.V.
Acknowledgement
This study was partly supported by the FWF Grant No. L562.
References
- 1.Pötter R., Kirisits C., Fidarova E.F. Present status and future of high-precision image guided adaptive brachytherapy for cervix carcinoma. Acta Oncol. 2008;47:1325–1336. doi: 10.1080/02841860802282794. [DOI] [PubMed] [Google Scholar]
- 2.Haie-Meder C., Pötter R., van Limbergen E. Recommendations from the Gynaecological (GYN) GEC ESTRO Working Group: concepts and terms in 3D-image based 3D-treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2004;74:235–245. doi: 10.1016/j.radonc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 3.Pötter R., Haie-Meder C., van Limbergen E. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose–volume parameters and aspects of 3D-image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78:67–77. doi: 10.1016/j.radonc.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 4.Pötter R., Dimopoulos J., Georg P. Clinical impact of MRI assisted dose volume adaptation and dose escalation in brachytherapy of locally advanced cervix cancer. Radiother Oncol. 2007;83:148–155. doi: 10.1016/j.radonc.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 5.Pötter R., Georg P., Dimopoulos J. Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol. 2011;100:116–123. doi: 10.1016/j.radonc.2011.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haie-Meder C., Chargari C., Rey A. MRI-based low dose-rate brachytherapy experience in locally advanced cervical cancer patients initially treated by concomitant chemoradiotherapy. Radiother Oncol. 2010;96:161–165. doi: 10.1016/j.radonc.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 7.Chargari C., Magné N., Dumas I. Physics contributions and clinical outcome with 3D-MRI-based pulsed-dose-rate intracavitary brachytherapy in cervical cancer patients. Int J Radiat Oncol Biol Phys. 2009;74:133–139. doi: 10.1016/j.ijrobp.2008.06.1912. [DOI] [PubMed] [Google Scholar]
- 8.Dimopoulos J., Pötter R., Lang S. Dose–effect relationship for local control of cervical cancer by magnetic resonance image-guided brachytherapy. Radiother Oncol. 2009;93:311–315. doi: 10.1016/j.radonc.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Dimopoulos J., Lang S., Kirisits C. Dose–volume histogram parameters and local tumor control in magnetic resonance image-guided cervical cancer brachytherapy. Int J Radiat Oncol Biol Phys. 2009;75:56–63. doi: 10.1016/j.ijrobp.2008.10.033. [DOI] [PubMed] [Google Scholar]
- 10.Dimopoulos J., Kirisits C., Petric P. The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: clinical feasibility and preliminary results. Int J Radiat Oncol Biol Phys. 2006;66:83–90. doi: 10.1016/j.ijrobp.2006.04.041. [DOI] [PubMed] [Google Scholar]
- 11.Kirisits C., Pötter R., Lang S. Dose volume parameters for MRI-based treatment planning in intracavitary brachytherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2005;62:901–911. doi: 10.1016/j.ijrobp.2005.02.040. [DOI] [PubMed] [Google Scholar]
- 12.Trnkova P., Pötter R., Baltas D. New inverse planning technology for image-guided cervical cancer brachytherapy: description and evaluation within a clinical frame. Radiother Oncol. 2009;93:331–340. doi: 10.1016/j.radonc.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 13.Dimopoulos J.C., De Vos V., Berger D. Inter-observer comparison of target delineation for MRI-assisted cervical cancer brachytherapy: application of the GYN GEC-ESTRO recommendations. Radiother Oncol. 2009;91:166–172. doi: 10.1016/j.radonc.2008.10.023. [DOI] [PubMed] [Google Scholar]
- 14.Hellebust T.P., Kirisits C., Berger D. Recommendations from Gynaecological (GYN) GEC-ESTRO Working group: considerations and pitfalls in commissioning and applicator reconstruction in 3D image-based treatment planning of cervix cancer brachytherapy. Radiother Oncol. 2010;96:153–160. doi: 10.1016/j.radonc.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Tanderup K., Nielsen S.K., Nyvang G.B. From point A to the sculpted pear: MR image guidance significantly improves tumour dose and sparing of organ at risk in brachytherapy of cervical cancer. Radiother Oncol. 2010;94:173–180. doi: 10.1016/j.radonc.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Jürgenliemk-Schulz I.M., Lang S., Tanderup K. Variation of treatment planning parameters (D90 HR-CTV, D2cc for OAR) for cervical cancer tandem ring brachytherapy in a multicentre setting: comparison of standard planning and 3D image guided optimisation based on a joint protocol for dose-volume constraints. Radiother Oncol. 2010;94:339–345. doi: 10.1016/j.radonc.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 17.Hockel M., Schlenger K., Aral B. Association between tumor hypoxia and malignant progression in advanced cancer of the uterine cervix. Cancer Res. 1996;56:4509–4515. [PubMed] [Google Scholar]