Abstract
Background
Altered ventricular repolarization and cardiovascular mortality are closely correlated and recent novel findings show that a distorted T-wave loop morphology is also strongly correlated with subsequent onset of myocardial infarction among stable angina patients. Therefore, we hypothesized that an abnormal T-wave complexity ratio (CR) can indicate vulnerability to myocardial ischemia in asymptomatic, apparently-healthy adults.
Methods
Healthy firefighters were enrolled in the current investigation where they completed symptom-limited, graded exercise treadmill testing (ETT) and 24-hr Holter ECG recording. The CR was automatically calculated using principal component analysis of the high-resolution Holter ECG signal then averaged over 24 hrs (CR24hrs). Endpoints were manually analyzed from the ETT; recordings revealing horizontal ST-segment depression (≥1mm) in two or more leads for at least 1 min during the peak of exercise were considered indicators of myocardial ischemia.
Results
104 firefighters (age 44±8 years, 96% men) completed both ETT and Holter recording. Firefighters with positive endpoints (n=34, 33%) had higher CR24hrs compared to those with negative endpoints (0.14±0.06 vs 0.09±0.04, p<0.01), there were no demographic differences between the two groups. After controlling for age, smoking status, hypertension, and obesity; an abnormal CR24hrs (≥20%) significantly predicted exercise-induced myocardial ischemia (odds ratio 4.6, p=0.01).
Conclusions
Increased T wave CR24hrs can predict myocardial ischemia in asymptomatic middle age adults; this suggests that the distorted T wave loop morphology can reflect an altered ventricular repolarization caused by prolonged subclinical myocardial ischemia possibly due to early coronary artery disease.
Keywords: Principal Component Analysis, T wave Complexity, Repolarization, Myocardial Ischemia, Firefighters
BACKGROUND
Altered ventricular repolarization plays an essential role in the mechanism of cardiovascular mortality 1. Rooted in the assumption that the T-wave is monophasic and without notches; novel T-wave loop morphology descriptors that simultaneously quantify QT duration, T-wave shape, and ST/T wave morphology, have been previously suggested to quantitatively measure such alterations in ventricular repolarization 2. Obtained from the electrocardiogram (ECG), these novel T-wave loop morphology descriptors have been repeatedly linked to subsequent cardiovascular mortality in different populations 3–8. Recent novel findings 9 have shown that a distorted T-wave loop morphology is strongly correlated with subsequent onset of myocardial infarction among stable angina patients; suggesting that altered repolarization indicates increased vulnerability to myocardial ischemia. Therefore, we hypothesized that a distorted T-wave loop morphology, measured by complexity ratio (CR), can predict myocardial ischemia in asymptomatic, apparently-healthy adults.
METHODS
Healthy on-duty professional firefighters recruited in the parent study, Surveying and Assessing Firefighters Fitness and Electrocardiogram (SAFFE study) 10, were enrolled in the current investigation. All firefighters completed a symptom-limited, graded exercise treadmill testing (ETT) using standard Bruce protocol and a 24-hr Holter 12-lead ECG recording that was analyzed using SuperECG software (Mortara Instrument, Milwaukee, WI). The CR was automatically calculated using principal component analysis (PCA) of the high-resolution Holter ECG signal then averaged over 24 hrs (CR24hrs). A CR24hrs of 20% or more was previously suggested to resemble abnormal repolarization in healthy adults 2 and therefore was used to define the cutoff value for abnormal CR24hrs in the current investigation. A reviewer blinded to all clinical data manually analyzed the endpoints from the ETT using X-Scribe software (Mortara Instrument); recordings revealing horizontal ST-segment depression (≥1mm) and/or T wave inversion in 2 or more adjacent leads for at least 1 min during the peak of exercise were considered indicators of myocardial ischemia 11.
Principal Component Analysis
Instead of analyzing the inhomogenity of T wave morphology from different ECG leads, PCA technique was previously developed to grossly estimate the morphological complexity of the multiple forms required to describe the T-wave using decomposition matrices to estimate the eigenvalues, which makes PCA more consistent due to being less dependent on time domain or precise determination of T wave offset. With the first eigenvalue component accounting for most repolarization energy compared to all 8 eigenvalues components, a calculated ratio between these components, usually referred to complexity ratio (CR), can accurately estimate the heterogeneity of repolarization. In the current investigation, the ratio of the 2nd to 1st eigenvalues of the spatial T-wave vector generated from the digital, minute-by-minute averaged 12-lead ECG was used as a measure of the complexity or heterogeneity of repolarization. CR constitutes the difference between the long and short T wave vectors in a three dimensional loop domain. A large CR (fatter loop) reflects a more dispersed, heterogeneous repolarization compared to a small CR (thinner loop) that reflects a normal, homogenous repolarization. A CR obtained over 24hrs (CR24hrs) allows measuring the diurnal variability of ventricular repolarization 2.
Statistical Analysis
Continuous values are reported as mean ± standard deviation, and categorical variables are reported as frequency (%). Chi-square and independent t-test were used to compare the difference between firefighters with positive and negative endpoints. Step-wise logistic regression was used to predict myocardial ischemia on ETT; selected demographics and clinical data were entered in the first step and CR24hrs was entered in the second step. P <0.05 was considered statistically significant. All statistical analyses were performed with SPSS for Windows (Version 17).
RESULTS
Professional firefighters (n=104, age 44±8 years, 96% men, 81% white) completed both ETT and 24 hour Holter recording. Table 1 shows sample demographics and differences between firefighters with positive (n=34, 33%) and negative endpoints (n=70, 67%). Compared to those with negative endpoints, firefighters with positive endpoints (max ST depression on peak ETT = 2.2±0.6 mm, range 1.3–3.5) had more firefighting experience, had higher systolic blood pressure, achieved faster heart rate and greater exercise tolerance on the ETT, and had larger T wave loop CR24hrs (0.14±0.06 vs 0.09±0.04, p<0.01), there were no differences in age, sex, race, body mass index (BMI), waist circumference, or smoking status between the two groups. The average T wave loop CR24hrs in the whole sample was 10.7±4.9%; a cutoff point of 20% or more approximates 2 standard deviations above the mean. Approximately, 17 firefighters (16.3%) had abnormal T wave loop CR24hrs. Of note, the distorted T wave loop was independent from transient ST/T wave ischemic events documented during Holter recording (χ2=0.005, NS).
Table 1.
Sample Demographics and Clinical Indices
| All Subjects | Myocardial Ischemia on ETT | |||
|---|---|---|---|---|
| Variable | P value | |||
| (n=104) | Negative (n=70) | Positive (n=34) | ||
| Age (yrs) | 43.6±7.7 | 42.8±7.9 | 45.6±5.7 | 0.07 |
| Sex (% men) | 96 | 96 | 97 | NS |
| Race (% white) | 81 | 83 | 79 | NS |
| Firefighting Experience (yrs) | 15.5±7.0 | 14.6±7.2 | 17.5±6.3 | 0.05 |
| BMI (kg/m2) | 29.5±4.1 | 29.7±4.3 | 29.2±4.1 | NS |
| Obesity (BMI≥30, %) | 41 | 46 | 29 | 0.11 |
| Waist Circumference (cm) | 101.3±11.8 | 101.9±12.7 | 100.9±11.2 | NS |
| Systolic BP (mmHg) | 129.3±14.9 | 126.8±14.0 | 133.3±17.1 | 0.04 |
| Diastolic BP (mmHg) | 81.8±10.6 | 81.6±10.5 | 81.9±11.5 | NS |
| HTN (BP≥140/90, %) | 36 | 31 | 44 | NS |
| Smoking Rate (%) | 12 | 13 | 9 | NS |
| Average 24 heart rate (beats) | 76.6±9.9 | 76.9±9.1 | 75.3±10.7 | NS |
| QRS duration (msec) | 98.5±11.1 | 98.9±9.8 | 97.3±13.7 | NS |
| QTc duration (msec) | 409.2±32.9 | 407.8±28.9 | 403.7±29.7 | NS |
| ST ischemic events (%) | 13 | 10 | 15 | NS |
| Max HR on ETT (% target) | 92.7±7.5 | 91.4±7.3 | 96.0±7.1 | 0.01 |
| METs achieved on ETT | 11.8±2.5 | 11.5±2.7 | 12.6±1.8 | 0.01 |
| T wave Loop CR24hrs | 0.11±0.05 | 0.09±0.04 | 0.14±0.06 | 0.01 |
| Abnormal CR24hrs (%) | 16 | 6 | 32 | 0.01 |
All values are mean ± SD; (%): incidence rate; BMI: Body Mass Index; BP: Blood Pressure; HTN: Hypertension; HR: Heart Rate; ETT: Exercise Treadmill Testing; METs: Metabolic Equivalent Tasks; CR24hrs: Average Complexity Ratio over 24 hrs
Using stepwise logistic regression, after controlling for age (years), smoking status (yes/no), hypertension rate (BP≥140/90 mmHg), and obesity rate (BMI≥30 kg/m2), T wave loop CR24hrs was significant in the final model, explaining 18.4% of the predicted myocardial ischemia on ETT (odds ratio 4.6, p=0.01, Table 2). An abnormal CR24hrs (≥20%) has shown 65% positive and 74% negative predictive values; 91% specificity, and 32% sensitivity to predict myocardial ischemia in asymptomatic firefighters. Figure 1 shows subclinical myocardial ischemia during the peak ETT of a firefighter with an abnormal CR24hrs.
Table 2.
Adjusted Logistic Regression Analysis for Selected Clinical Parameters and T wave Loop Complexity Ratio in Relation to Exercise-Induced Myocardial Ischemia
| Exercise-Induced Myocardial Ischemia n=34 | ||||
|---|---|---|---|---|
| Parameter | ||||
| β | P value | OR (95% CI) | Total R2 | |
| Age (years) | 0.05 | 0.11 | - | - |
| Smoking Status | − 0.59 | NS | - | - |
| Hypertension (BP≥140/90) | 0.44 | NS | - | - |
| Obesity (BMI≥30) | − 0.63 | NS | - | - |
| Abnormal CR24hrs (≥20%) | 1.52 | 0.01 | 4.6 (1.4–14.9) | 18.4 |
BP: Blood Pressure; BMI: Body Mass Index; CR24hrs: Average Complexity Ratio over 24 hrs.
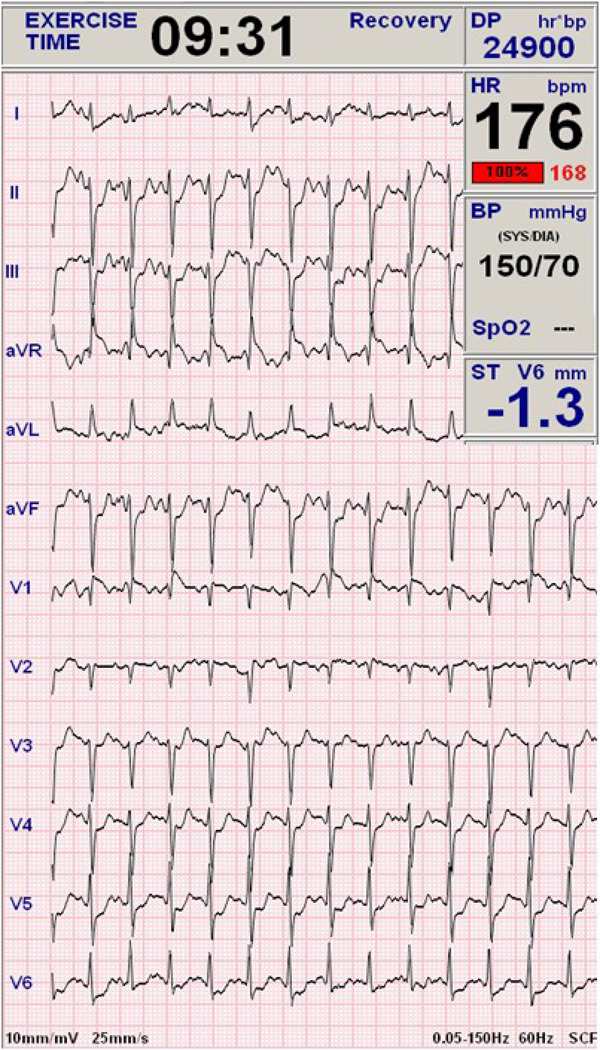
Figure 1. 12-lead ECG Revealing Exercise-Induced Myocardial Ischemia.
This recording was taken at the peak of an exercise-treadmill testing of a 52 year-old healthy male firefighter, non-obese, and non-smoker. The recording shows horizontal ST depression >1mm in V4–V6 that lasted for 3 minutes after stopping the test. The average 24hrs T wave loop complexity ratio obtained from the Holter was 20%.
DISCUSSION
Continuous 24-hour Holter ECG recording allows measuring the diurnal variability of ventricular repolarization, our findings showed that 16% of firefighters in the current investigation had increased T wave loop CR24hrs, which indicates a dispersed, heterogeneous ventricular repolarization, a marker of increased risk for arrhythmogenic mortality. After controlling for demographic and clinical indices previously reported to predict coronary artery disease (CAD) in firefighters (specifically hypertension, obesity, and smoking) , those with fatter T wave loop (CR24hrs ≥20%) were at least four times more likely to have exercise-induced myocardial ischemia on the ETT. Our findings are similar to previous studies were balloon-induced myocardial ischemia in catheterization lab was associated with transient alterations in T wave loop morphology mirroring a simultaneous repolarization dispersion.
Firefighters are at increased risk for cardiovascular mortality; approximately 39% of onduty deaths in this population are due to CAD 21. Almost one third of firefighters in the current investigation had exercise-induced myocardial ischemia during their peak ETT, which was much higher than previously reported rates of positive ETT in similar populations (13%) 22. Firefighters for this study were recruited from Western New York (WNY), therefore, the high rate of abnormal ETT can be partially related to the fact that the county has the highest rates of cardiovascular diseases in the nation 23. Moreover, we have previously defined a higher rate of metabolic syndrome in professional firefighters at WNY compared to general population 24, which constitutes a marker for CAD. Interestingly, there were no differences between firefighters with positive and negative ETT in regard to traditional risk factors (age, sex, obesity, smoking, or hypertension) or other clinical indices (average heart rate, QRS duration, QTc duration, or transient ST/T wave ischemic events). However, firefighters with positive ETT were on average 3 years more experienced and had 6.5 mmHg higher systolic blood pressure compared to those with negative ETT, suggesting possibly higher rates of occupational hazards exposure (e.g. carbon monoxide inhalation) and associated cardiovascular morbidity (e.g. elevated blood pressure and myocardial ischemia).
Myocardial ischemia induces electrophysiological alterations in action potentials, causing repolarization dispersion between normal and ischemic fibers and between epicardium and endocardium, establishing the basis for re-entrant depolarization dispersion currents and subsequent life-threatening ventricular arrhythmias 20. Even though not ideal, such minor electrical dispersion currents can be measured with surface electrical ECG measures 25. Berger et al 26 have demonstrated that repolarization lability, measured through beat-to-beat QT variance in patients with ischemic and non-ischemic cardiomyopathy, reflects a prolongation of the action potential due to alteration in calcium and potassium influx currents, in which most alteration happens in mildly symptomatic individuals where sudden cardiac death is most prevalent. In light of these mechanisms, the prevalent subclinical myocardial ischemia in the current investigation (33%), along with the associated repolarization dispersion (16%), can possibly explain the prevalent cardiac mortality previously reported in firefighters. Finally, the absent correlation between the distorted T wave loop (abnormal CR24hrs) and the transient ST/T wave ischemic events, documented during continuous Holter recording, suggests that each has a different pathological mechanism in relation to myocardial ischemia. The altered ventricular repolarization pattern (abnormal CR24hrs) can reflect prolonged subclinical myocardial ischemia possibly due to early CAD. Further investigation is needed to understand this relationship.
Limitations
There are no ETT gold standard criteria to identify myocardial ischemia in asymptomatic adults 11; the clinical criteria used to diagnose CAD are more rigid than that used in the current investigation (horizontal ST depression of 2mm vs 1mm, respectively). However, in populations with high prevalence of the disease (e.g. firefighters), a positive diagnostic test is usually more likely to indicate the outcome; some studies report that using more rigid criteria in screening asymptomatic firefighters might lack adequate sensitivity to detect CAD 22. Since we were concerned with detecting repolarization dispersion caused by subclinical myocardial ischemia, rather than significant CAD, less rigid criteria (ST segment depression of 1mm) were used to define exercise-induced myocardial ischemia. Additionally, the very wide 95% CI of odds ratio in the multivariate analysis reflects the small number of subjects with abnormal repolarization dispersion in the sample (n=17, 16%); which requires a larger sample size to validate the results.
CONCLUSIONS
Subclinical myocardial ischemia in asymptomatic adults is strongly correlated with altered ventricular repolarization. Such minor alterations in ventricular repolarization were successfully recorded with surface ECG, which enables this novel study to improve the clinical utility of non-invasive 12-lead ECG to detect early CAD through evaluating the PCA of ventricular repolarization rather than relying solely on transient ST segment changes that might lack adequate predictive values.
Acknowledgments
Supported by a Grant from the National Institutes of Health (R21 NR-011077, MGC)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Pentti MR. Dispersed measures of dispersed repolarization and depolarization: Scalars, vectors, angles, maps, and prospects for improved clinical utility. Journal of Electrocardiology. 2010;43(4):283–287. doi: 10.1016/j.jelectrocard.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Priori SG, Mortara DW, Napolitano C, et al. Evaluation of the Spatial Aspects of T-Wave Complexity in the Long-QT Syndrome. Circulation. 1997;96(9):3006–3012. doi: 10.1161/01.cir.96.9.3006. [DOI] [PubMed] [Google Scholar]
- 3.Prineas RJ, Grandits G, Rautaharju PM, Cohen JD, Zhang ZM, Crow RS. Long-term prognostic significance of isolated minor electrocardiographic T-wave abnormalities in middle-aged men free of clinical cardiovascular disease (The Multiple Risk Factor Intervention Trial [MRFIT]) American Journal of Cardiology. 2002;90(12):1391–1395. doi: 10.1016/s0002-9149(02)02881-3. [DOI] [PubMed] [Google Scholar]
- 4.Okin P, Devereux R, Fabsitz R, Lee E, Galloway J, Howard B. Principal Component Analysis of the T Wave and Prediction of Cardiovascular Mortality in American Indians: The Strong Heart Study. Circulation. 2002;105(6):714–719. doi: 10.1161/hc0602.103585. [DOI] [PubMed] [Google Scholar]
- 5.Beckerman J, Yamazaki T, Myers J, et al. T-Wave Abnormalities Are a Better Predictor of Cardiovascular Mortality than ST Depression on the Resting Electrocardiogram. Annals of Noninvasive Electrocardiology. 2005;10(2):146–151. doi: 10.1111/j.1542-474X.2005.05607.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lux RL, Gettes LS, Mason JW. Understanding proarrhythmic potential in therapeutic drug development: alternate strategies for measuring and tracking repolarization. Journal of Electrocardiology. 2006;39(4) Supplement 1:S161–S164. doi: 10.1016/j.jelectrocard.2006.05.020. [DOI] [PubMed] [Google Scholar]
- 7.Iacoviello M, Forleo C, Guida P, et al. Ventricular Repolarization Dynamicity Provides Independent Prognostic Information Toward Major Arrhythmic Events in Patients With Idiopathic Dilated Cardiomyopathy. Journal of the American College of Cardiology. 2007;50(3):225–231. doi: 10.1016/j.jacc.2007.02.071. [DOI] [PubMed] [Google Scholar]
- 8.Zabel M, Acar B, Klingenheben T, Franz MR, Hohnloser SH, Malik M. Analysis of 12-Lead T-Wave Morphology for Risk Stratification After Myocardial Infarction. Circulation. 2000;102(11):1252–1257. doi: 10.1161/01.cir.102.11.1252. [DOI] [PubMed] [Google Scholar]
- 9.Aigars R, Lennart B, Lars R, Jens J. Prediction of cardiovascular death and myocardial infarction by the QRS-T angle and T vector loop morphology after angioplasty in stable angina pectoris: an 8-year follow-up. Journal of Electrocardiology. 2010;43(4):310–317. doi: 10.1016/j.jelectrocard.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 10.Carey MG, Al-Zaiti S, Butler RA. Characteristics of the Standard 12-lead Holter ECG in Professional Firefighters. Paper presented at: Computing in Cardiology; Belfast, UK. 2010. [Google Scholar]
- 11.Gibbons R, Balady G, Beasley J, et al. ACC/AHA Guidelines for Exercise Testing: A Report of the American College of Cardiology/ American Heart Association/ Task Force on Practice Guidelines (Committee on Exercise Testing) Journal of the American College of Cardiology. 1997;30(1):260–311. doi: 10.1016/s0735-1097(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 12.Acar B, Yi G, Hnatkova K, Malik M. Spatial, temporal and wavefront direction characteristics of 12-lead T-wave morphology. Medical and Biological Engineering and Computing. 1999;37(5):574–584. doi: 10.1007/BF02513351. [DOI] [PubMed] [Google Scholar]
- 13.Lux R, Evans A, Burgess M, Wyatt R, Abildskov J. Redundancy reduction for improved display and analysis of body surface potential maps. I. Spatial compression. Circ Res. 1981;49(1):186–196. doi: 10.1161/01.res.49.1.186. [DOI] [PubMed] [Google Scholar]
- 14.Yi G, Prasad K, Elliott P, et al. T Wave Complexity in Patients with Hypertrophic Cardiomyopathy. Pacing and Clinical Electrophysiology. 1998;21(11):2382–2386. doi: 10.1111/j.1540-8159.1998.tb01186.x. [DOI] [PubMed] [Google Scholar]
- 15.Qiuzhen X, Shankara R. Algorithms for computerized QT analysis. Journal of Electrocardiology. 1998;30:181–186. doi: 10.1016/s0022-0736(98)80072-1. [DOI] [PubMed] [Google Scholar]
- 16.Dhamoon AS, Jalife J. The inward rectifier current (IK1) controls cardiac excitability and is involved in arrhythmogenesis. Heart Rhythm. 2005;2(3):316–324. doi: 10.1016/j.hrthm.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 17.Soteriades ES, Hauser R, Kawachi I, Liarokapis D, Christiani DC, Kales SN. Obesity and Cardiovascular Disease Risk Factors in Firefighters: A Prospective Cohort Study. Obesity. 2005;13(10):1756–1763. doi: 10.1038/oby.2005.214. [DOI] [PubMed] [Google Scholar]
- 18.Geibe JR, Holder J, Peeples L, Kinney AM, Burress JW, Kales SN. Predictors of On-Duty Coronary Events in Male Firefighters in the United States. The American Journal of Cardiology. 2008;101(5):585–589. doi: 10.1016/j.amjcard.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 19.Arini PD, Baglivo FH, Martinez JP, Laguna P. Ventricular repolarization dispersion during ischemia course measured by temporal and spatial electrocardiographic parameters. Paper presented at: Computers in Cardiology; 14–17 Sept. 2008.2008. [Google Scholar]
- 20.Lukas A, Antzelevitch C. Differences in the electrophysiological response of canine ventricular epicardium and endocardium to ischemia. Role of the transient outward current. Circulation. 1993;88(6):2903–2915. doi: 10.1161/01.cir.88.6.2903. [DOI] [PubMed] [Google Scholar]
- 21.Kales SN, Soteriades ES, Christophi CA, Christiani DC. Emergency duties and deaths from heart disease among firefighters in the United States. New England Journal of Medicine. 2007;356(12):1207–1215. doi: 10.1056/NEJMoa060357. [DOI] [PubMed] [Google Scholar]
- 22.Budoff MJ, Karwasky R, Ahmadi N, et al. Cost-effectiveness of multidetector computed tomography compared with myocardial perfusion imaging as gatekeeper to invasive coronary angiography in asymptomatic firefighters with positive treadmill tests. Journal of Cardiovascular Computed Tomography. 2009;3(5):323–330. doi: 10.1016/j.jcct.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart Disease and Stroke Statistics--2010 Update: A Report From the American Heart Association. Circulation. 2010;121(7):e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 24.Carey MG, Al-Zaiti SS, Liao LM, Martin HN, Butler RA. A Low-Glycemic Nutritional Fitness Program to Reverse Metabolic Syndrome in Professional Firefighters: Results of a Pilot Study. Journal of Cardiovascular Nursing. 2011 July/August;26(4):298–304. doi: 10.1097/JCN.0b013e31820344d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nash MP, Bradley CP, Paterson DJ. Imaging Electrocardiographic Dispersion of Depolarization and Repolarization During Ischemia: Simultaneous Body Surface and Epicardial Mapping. Circulation. 2003;107(17):2257–2263. doi: 10.1161/01.CIR.0000065602.78328.B5. [DOI] [PubMed] [Google Scholar]
- 26.Berger RD, Kasper EK, Baughman KL, Marban E, Calkins H, Tomaselli GF. Beat-to-Beat QT Interval Variability : Novel Evidence for Repolarization Lability in Ischemic and Nonischemic Dilated Cardiomyopathy. Circulation. 1997;96(5):1557–1565. doi: 10.1161/01.cir.96.5.1557. [DOI] [PubMed] [Google Scholar]