Abstract
This paper reports on a study designed to explore factors contributing to better outcomes for substance abusing pregnant and parenting women in residential treatment, and, as a result, contribute to better outcomes for their children. The setting was three live-in units focusing in supporting both abstinence from substances and mother-child relationship. Participants were 18 mother-baby pairs in treatment from perinatal phase to 4 months of child’s age. Pilot results demonstrated more sensitive maternal interaction tended to be associated with higher pre-and postnatal reflective functioning and better child developmental scores at 4 months of child’s age. Reflective functioning (RF) refers to the essential human capacity to understand behavior in light of underlying mental states and intentions. An indicated conclusion is that enhancement of maternal reflective ability seems an important focus in developing the content and effectiveness of interventions for substance abusing mothers.
Keywords: substance abuse, pregnancy, motherhood, early parenting intervention
Introduction
Clinical and theoretical background
Substance-abusing pregnant and parenting women typically are a group characterized by cumulative psychosocial risk factors (Grella, Joshi, & Hser, 2000; Mayes & Truman, 2002; Pajulo, 2001; Suchman, Mayes, Conti, Slade, & Rounsaville, 2004). In addition to substance effects per se, all these factors have a cumulative negative effect on the well-being of the mother and the child and on the quality of their relationship. Quality of early care and postnatal caregiving environment combined with the neurophysiological vulnerability of the exposed child are considered most important for the prognosis of child development and psychosocial outcome in later years (Carmichael Olson, O’Connor, & Fitzgerald, 2001; Lester & Tronick, 1994; Mayes & Truman, 2002; Suchman, McMahon, Slade, & Luthar, 2005).
A substance abusing mother and her exposed child are difficult regulatory partners for each other: the exposed infant often has an impaired ability to regulate his states, and the mother usually has a reduced capacity to read the child’s communicative signals (Beeghly & Tronick, 1994). This combination easily leads to viciously negative cycle that culminates in withdrawal from interaction and increased risk for child neglect and abuse (Kalland, 2001).
There is an ongoing debate in Finnish society about the rights of the pregnant women compared to the rights of her unborn child. One question regards the need for change in legislation to allow taking the substance abusing pregnant woman into institution-based treatment against her will, in order to protect the child. One severe problem, however, is that referral to treatment does not work even with those mothers who would enter the treatment voluntarily, and that there are far too few treatment places for mother-child couples together. Even more importantly, the content of the interventions, which should be specifically designed for parenting women together with their children, has not received enough attention. Objective research is strongly needed to be used in the process of developing the content of the treatment.
During the last 10 years, British psychoanalysts have increasingly drawn attention to the importance of the concept of reflective functioning in human development. We propose that this concept has a strong relevance in the situation of substance abusing parents. The term reflective functioning (RF) refers to the psychological processes underlying an individual’s capacity to understand oneself and others in terms of mental states (feelings, beliefs, intentions and desires), and to reason about one’s own and others’ behavior in relation to these (Fonagy, Gergely, Jurist, & Target, 2002). In addition to being a metacognitive capacity, reflective functioning refers to the ability to hold, regulate, and experience emotions. Reflective functioning makes it possible for a mother to behave sensitively with her child (Meins, Fernyhough, Fradley, & Tuckey, 2001), and is considered an important contributor in the intergenerational transmission of attachment security. Deprived and traumatized mothers who nonetheless are highly reflective are more likely to have securely attached children, whereas deprived mothers with low reflectiveness almost invariably have been found to have insecure children (Fonagy, Steele, & Steele, 1991; Fonagy et al., 1995). There are a few data showing that among substance using mothers, reflective abilities toward their children are generally low (Suchman, Altomare, Moller, Slade, & Mayes, 2003; Suchman et al., 2004; Truman, Levy, & Mayes, 2004). However, it is considered a parental capacity which can be enhanced by intervention (Goyette-Ewing, Slade, Knoebber, Gilliam, Truman, & Mayes, 2002; Schechter, Zeanah, & Myers, 2002; Schechter, Kaminer, Grienenberger, & Amat, 2003; Suchman et al., 2003; Suchman et al., 2004). There are no empirical studies yet showing the level of RF among substance-addicted mothers in pregnancy and early postnatal period.
Research context
A parenting intervention using an attachment perspective with substance dependent mothers and their babies has been developed in residential treatment units in Finland since 1990. At the present time, seven units using this perspective work in different parts of the country, funded by both local governments and the Slot Machine Association. The units are part of the child protection field in the social welfare sector (Federation of Mother and Child Homes and Shelters). The average duration of treatment has been 6 months (range from 1 month to over a year, depending, usually, either upon the mother’s own willingness or upon the amount of funding received from the government). The treatment starts usually about 2 months before the birth of the baby. The referral to the unit is made by a social welfare agency, delivery hospital, well-baby clinic, or by the mother herself due to her primary problem with alcohol and/or other drugs. The two main aims in the treatment are to intensively support the mother in her efforts toward abstinence and to support her relationship with her child. The personnel in the units come from the substance abuse field, family and infant work, child protection field, and adult or child psychiatry. The units have the capacity to serve five mother-baby-couples, and one place for a whole family to live-in. The treatment occurs throughout each day on all days of the week. Detoxification and other medical or mental health treatment are provided outside the unit. The homogenity in the way of working across the units is maintained through the similarity of initial training, regular supervision by mother-infant work specialists, and through check-ups with questionnaires concerning the content of the work. A detailed description of the way of relationship-based intervention in these units has been published in a separate article (Pajulo, Suchman, Kalland, & Mayes, 2006).
Aim of the present study
The study is an observational, prospective 2-year follow-up study of an ongoing residential intervention for substance abusing mothers and babies. The purpose of the study is to explore factors related to treatment outcome (followed for two years), in terms of quality of mother-child interaction, abstinence from substances and child development. Due to some interesting preliminary findings, the results regarding the treatment outcome at the end of the residential treatment period of first 18 mother-baby pairs are reported in this article.
We hypothesize that:
Despite their multi-risk background, there are clear individual differences in the mothers’ capacity for sensitivity with their child, and that higher level of maternal RF is associated with more sensitive interaction behavior with the child postnatally.
The residential treatment intervention enhances maternal RF between the prenatal and postnatal assessment period
Methods
Participants
The participants were 18 mother-baby pairs who lived in three of the treatment units and entered the units during pregnancy (n=12) or straight after delivery (within 2 weeks) (n=6). All of the mothers participating stayed in residential treatment for at least 4 months postnatally. During the data collection period there were three mothers out of all potential participants who refused to participate, and three mothers who started in the study, but interrupted their treatment and participation before the 4 months time-point.
Procedure
All data collection was carried out by the treatment unit staffs, as they were trained in that personally by the PI. An outside psychologist carried out child development assessments. All questionnaire data were collected so that the personnel interviewed the mother and filled in the questionnaires together with her. Exceptions from this were the questionnaires regarding maternal psychiatric symptomatology, which were enclosed in an envelope by the mother and returned directly to their personal research folder. Scoring of the videomeasures and interviews were made by separate experienced outside raters who were blind to other data and to each others’ ratings. All Care Index ratings were also double-coded. The research plan was approved by the joint ethical committee of Pirkanmaa Hospital District and University of Tampere.
Data collection time points
Data collection time points were the following: during pregnancy (background data, pregnancy RF interview), at 1 month of child’s age (delivery and somatic data), 3 months (psychiatric symptoms questionnaires), and 4 months of child’s age (maternal sensitivity, maternal RF, child development). All mothers attended all measures (n=18) except for the prenatal RF interviews: ten mothers could be interviewed for RF already during pregnancy.
Measures
Maternal sensitivity
The Care-Index for infants and toddlers (Crittenden, 2003) is an assessment of playful interaction occurring under non-threatening conditions. The interaction segments (7–10 minutes) are videotaped and scored from the tapes. Sensitivity to infant signals is considered as a dyadic construct; as any pattern of adult behavior that pleases the infant and increases the infant’s comfort and attentiveness and reduces its distress and disengagement (Ainsworth, Blehar, Waters, & Wall, 1978). The behavioral items cover seven aspects: 1) facial expression 2) verbal expression 3) position and body contact 4) affection 5) turn-taking contingencies 6) control 7) choice of activity. Points 11–14 on the sensitive scale can be considered sufficient for the designation of “sensitive” parenting, between 7–10 as “adequate,” 5–6 as “intervention range,” and 0–4 as “high risk” (controlling, unresponsive) parenting. The Care-Index has been largely used both for clinical and research purposes (Cassidy, Zoccolillo, & Hughes, 1996; Ciotti, Lambruschi, Pittino, & Crittenden, 1998; Cramer, Robert-Tissot, Stern, & Serpa-Rusconi, 1990; Crittenden & Bonvillian, 1984; Crittenden, 1992; Pacquette, Bigras, Zoccolillo, Tremblay, Labelle, & Azar, 2001; Patino, 1993; Ward & Carlson, 1995).
Maternal reflective functioning
Pregnancy Interview (PI) (Slade, Bernbach, Grienenberger, Levy, & Locker, 2002, 2005) is a 24- item semistructured interview, asking about the emotional experience of this pregnancy; view of the baby and view of the relationship between the mother and the baby, thoughts, feelings and changes experienced in relation to partner and own mother. Parental Development Interview Revised (PDI-R) (Slade et al. 2002, 2005) is a 40-item semistructured interview asking about the parent’s view of the child, view of her relationship with the child, experience of being a parent, childhood experiences of her own parents, dependence of the child, experiences of separation with the child, and views of the future. Both interviews are audiotaped and scored from the transcribed narratives by experienced and reliable coder. A parent’s responses to individual questions are scored along a continuous scale (−1 – 9) with anchor points describing different levels of RF ability described in detail in the manual. In evaluating parental RF ability from a transcript, three main criteria for true reflectiveness are considered: 1) the parent’s awareness of the nature of mental states (e.g. opacity and being susceptible to disguise) 2) parent’s effort to tease out mental states underlying behavior, and 3) parent’s ability to recognize developmental aspects of mental states. The number of signs of true reflectiveness found in the transcribed narrative is the basis in scoring. The more there are specific and different signs of RF, the more positive (higher) is the score, with a score of −1 indicating a rejection of RF, scores of 0–2 indicating very weak ability for RF, a score 3 indicating weak ability, scores of 4–5 representing a normal or close to normal ability and scores 6–9 representing high or exceptionally high ability for RF. Fresh and spontaneous expressions of specific episodes are especially looked for; the importance of episodic memory is emphasized (Fonagy, Steele, & Steele, 1991; Fonagy, Steele, Moran, Steele, & Higgitt, 1991; Grienenberger, Kelly, & Slade, 2005; Slade, Grienenberger, Bernbach, Levy, & Locker, 2005; Fonagy & Target, 1996). Episodic memory is regarded clinically as the most important memory system, as significant changes in understanding and behavior happen there. General expressions, opinions, or clichés (signs of semantic memory in the left brain hemisphere) are not regarded as signs of RF. For example, a person may report that she/he (cognitively) understands some issue, but is not acting according to this understanding. The RF scale has been validated using samples of ordinary pregnant women and mothers with small children (Fonagy, Steele, & Steele, 1991; Fonagy, Steele, Moran, Steele, & Higgitt, 1991; Grienenberger, Kelly, & Slade, 2005; Slade, Grienenberger, Bernbach, Levy, & Locker, 2005), psychiatric patients, and borderline personality disorder patients (Fonagy & Target, 1996).
Maternal psychiatric symptoms
Edinburgh Postnatal Depression Screen (EPDS) (Cox, Holden, & Sagovsky, 1987) is a 10-item self-report scale, which covers the common symptoms of depression during the previous week. It includes questions about ability to see the funny side of things, ability to enjoy things, amount of self-blaming, crying, feelings of stress, sadness and worry, and difficulties in sleeping. Each of the ten items is scored on a four-point scale (0 to 3), with a total score ranging from 0 to 30. In screening major and minor depression for research purposes, the cut-off point of 12/13 is recommended (Murray & Cox, 1990), and used in this study. With the cut-off point of 12/13, 81 % of the major depressions and 52 % of the minor depressions become identified (Brockington, 1996).
Brief Symptom Inventory (BSI) (Derogatis, 1993), derived from the Symptom Checklist –90 (SCL –90-R), is a multidimensional symptom inventory designed to reflect the psychological symptom patterns of respondents in community, medical, and psychiatric settings. It is a 53- item self-report questionnaire concerning psychopathology and psychological distress, asking to report how much discomfort each item caused them during the past week, including the current day. Each item is rated on a five-point scale of distress, ranging from 0= “not at all” to 4=”extremely.” The reading skills of the mothers in our study group were adequate to rate the questionnaires by themselves. The theoretical range of the BSI sum is thus from 0 to 212 and, for the global symptom index and subscale indexes from 0 to 4. Internal consistency has ranged from 0.71 on the Psychoticism dimension to 0.85 on Depression dimension (Derogatis, 1993).
Child developmental status
Bayley Scales of Infant Development (BSID II) (Bayley, 1993) was used to identify developmental delays in infants. The mental scale contains 178 items that assess abilities such as memory, habituation, problem solving, number concepts, language, and social skills. The motor scale has 111 items that assess coordination and control of gross and fine motor skills. Internal consistency (Cronbach’s alpha, mean) for the mental scale has been 0.88 and for motor scale 0.84 (Nellis & Gridley, 1994). The results are reported as standard scores with a mean of 100 and a standard deviation of 15 and are referred to as the Mental Development Index (MDI) and Psychomotor Development Index (PDI), respectively. The classifications are: accelerated performance (115 and above), within normal limits (85–114), mildly delayed performance (70–84), significantly delayed performance (69 and below). The normative data for the BSID II was originally obtained from a sample of 1,700 subjects (infants) in the U.S. The measure is widely used both in clinical work and research also in Finland.
Other measures
Data regarding sociodemographic factors, substance abuse history, current use of substances, pregnancy, and delivery data were obtained with questionnaires designed for use in this study and were completed by the mothers together with a staff member. All knowledge that was available from the statements from social welfare, well baby clinics and hospitals was also used in completing these questionnaires.
Statistical analysis
Mean values in groups were compared with two-sample t-test or with one-way analysis of variance, depending on the number of groups in the comparison. Associations between two variables were analyzed using Pearson’s correlation coefficient. P-values less than 0.05 were considered as statistically significant. However, due to the small sample size, tendencies of associations are also presented.
Results
Background characteristics
The mean age of the mothers was 25 years (SD 5.9, range 17–37 years). About 40 % were single mothers, 70 % were having their first child, and 70 % entered the residential treatment during (late) pregnancy (mean weeks of gestation 31, range 21–39 weeks).
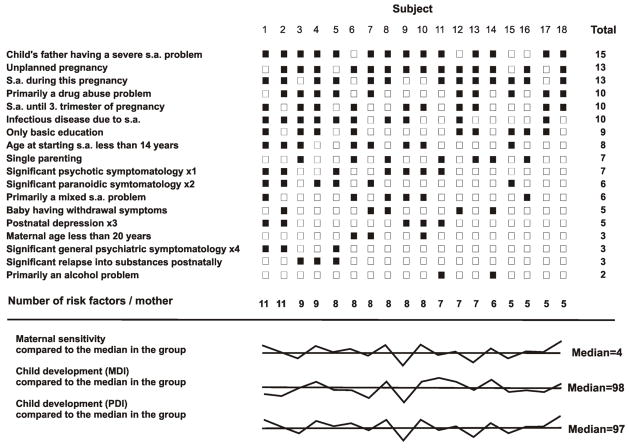
One mother was from an ethnic minority (Romany). Most of the mothers (56 %) had primarily a drug problem, 33 % had a poly-substance abuse problem (alcohol and drugs) and only two mothers (11 %) had primarily an alcohol problem. The reported amount of substance abuse during this pregnancy varied from daily use of multiple drugs until the third trimester at its worst to no substance abuse during this pregnancy. The most commonly used drugs were hashish, amphetamine and illegal use of buprenorphine, and the most common route of administration was intravenous. Nearly all pregnancies were full-term, with no major somatic problems. None of the babies had otherwise any diagnosed somatic disease or organic failure at the age of 4 months, and all mothers were the primary caregivers of their child at that point. For more details regarding the background characteristics see Figure 1.
Figure 1. Potential risk factors in maternal background and current situation, in comparison with maternal sensitivity and child developmental scores.
Eighteen mother-baby pairs in residential treatment due to maternal substance abuse problem. (x1=BSI psychotic symptom index > 0.97, x2=BSI paranoidic symptom index >1.48, x3=EPDS sum score ≥12, x4=BSI-GSI >1.32).
Child development
All babies were developing within normal limits at 4 months of age. The mean Mental Development Index of BSID was 99 (SD 6.7, range 85–109), and the mean Psychomotor Development Index was 98 (SD 5.7, range 86–107). All mothers had attended all routine well-baby clinic check-ups for their child’s development postnatally. From these visits, six babies had been referred for further examination in the hospital due to some somatic concern, but no major somatic problems were found.
Maternal psychiatric symptoms
Five mothers (28%) were screened as having postnatal depression (EPDS) at the 4 months point. The amount of global psychiatric symptomatology (BSI-GSI) was found to be higher in the pilot group than in a Finnish community sample (Holi, Sammallahti, & Aalberg, 1998), but the difference was not statistically significant. The global symptom mean in pilot group was significantly lower than in psychiatric outpatient sample (p=<0.001). Strikingly, more paranoidic and psychotic symptomatology was found among the pilot group mothers than in a community sample (p=0.01 and 0.03 respectively). The comparisons with community and outpatient samples are presented in Table 1.
Table 1.
Psychiatric symptomatology among mothers in residential substance abuse treatment together with their baby (Group 1, n=18). Comparison with a community sample (Group 2, n=337) and a psychiatric outpatient sample (Group 3, n=249) (Holi et al. 1998).
| Group 1 (n=18) | Group 2 (n=337) | Group 3 (n=249) | Comp. between Groups 1&2 | Comp. between Groups 1&3 | |||
|---|---|---|---|---|---|---|---|
| Scale | BSI | BSI | BSI | t | p | t | p |
| Possible range | 0–4 | 0–4 | 0–4 | ||||
| BSI Global Symptom Index | −1.58 | 0.13 | 4.9 | <0.001 | |||
| Mean | 0.83 | 0.60 | 1.56 | ||||
| SD | 0.61 | 0.44 | 0.61 | ||||
| BSI Paranoidic Symptom Index | −2.83 | 0.01 | 0.33 | 0.74 | |||
| Mean | 1.11 | 0.53 | 1.18 | ||||
| SD | 0.86 | 0.58 | 0.82 | ||||
| BSI Psychotic Symptom Index | −2.23 | 0.04 | 0.88 | 0.39 | |||
| Mean | 0.76 | 0.31 | 0.94 | ||||
| SD | 0.85 | 0.40 | 0.65 | ||||
Maternal reflective functioning
Among those ten mothers who entered the treatment during pregnancy early enough and were able to become interviewed before delivery (n=10), prenatal maternal RF ranged from “very weak” to “weak” (mean 2.1, SD 1.1, range 0–3.5). At 4 months postpartum, maternal RF (total score) ranged from “very weak” to “normal” (mean 3.1, SD 1.0, range 1–5). At the 4 months point, five mothers (28%) scored within the RF range of “close to normal to normal” (scores 4–5). Among those ten mothers who were assessed for their RF ability at two time points (i.e. pregnancy and 4 months postpartum), RF total score increased with 60% of the mothers; range of increase being 0.5–2 points. RF remained at the prenatal level for the rest. The increase in maternal RF during the treatment period was statistically significant (p=0.03).
Maternal sensitivity
Maternal sensitivity in interaction with the child at 4 months of the child’s age (assessed with Care Index) ranged from “total failure” to “adequate” (mean 4.3, SD 2.4, range 0–9). Ten mothers (55%) scored within “high risk” range (scores 0–4) and eight mothers (45%) scored within the “intervention” or “adequate” ranges (scores 5–10). None of the mothers was assessed to be within the “sensitive” range at this point.
Maternal sensitivity and other variables
There was a tendency of higher maternal sensitivity at 4 months of child’s age to be associated with higher maternal RF during pregnancy (r=0.48, p=0.15), higher maternal RF postnatally (r=0.35, p=0.17), and higher child development scores at 4 months point (Bayley Scales MDI: r=0.48, p=0.04; Bayley Scales PDI: r=0.37, p=0.13). Maternal sensitivity was not associated with maternal age (r=0.06, p=0.82), number of depressive symptoms (r=0.12, p=0.62), general symptom index (r=0.11, p=0.65), paranoidic symptom index (r=0.04, p=0.88), psychotic symptom index (r=0.23, p=0.35), or having postnatal substitution medication (p=0.90). A slight tendency of association was found between maternal unresponsive behavior and the length of maternal substance abuse history (in years) (r=0.31, p=0.20).
Discussion
Limitations of the study
Small sample size, lack of control group, and diversity of substance abuse history among the mothers are all severe limitations of the study. However, the decision to explore “within-group” differences in a clinical reality was conscious, as several previous studies have already shown the average weakness in the interaction capacities of substance abusing mothers compared with normative and other clinical groups, but there is very little understanding of the variation seen in treatment outcome. Also, a control group with the same characteristics but without an intervention would be difficult and even unethical to obtain.
Child development
All children were developing within normal limits at the age of 4 months. However, two babies (11 %) received MDI scores and two babies (11 %) PDI scores less than 90. In this study, the mothers had used different substances and to different extent during pregnancy. In previous studies using BSID to assess child cognitive development in later years, the findings regarding effect of substance-exposure have been contradictory. They have ranged from a remarkable effect to no effect, and have been considered to be dependent on other environmental factors and gender of the child, not on substance use per se (Barth & Needell, 1996; Bauman & Levine, 1986; Moe & Slinning, 2001). The drug-exposed children’s developmental scores on the Bayley Scales have been found to decrease over time when the caregiver is not in a treatment intervention (Hurt, Brodsky, Betancourt, Braitman, Malmud, & Giannetta, 1995; Schuler, Nair, Harrington, 2003). Lower mean development scores on the Bayley Scales at 4 months of age have been related to maternal postnatal substance use and poorer maternal interaction quality (Blackwell, Kirkhart, Schmitt, & Kaiser, 1998). Mothers’ sustained abstinence from substances and intensive support for mother-child interactions after the residential period are likely of crucial importance for the prognosis of the child’s development.
Among the pilot study group, maternal sensitivity in interaction varied from very high risk style to normal interactive style. However, remarkably, many mothers were assessed to be within the “high risk” range regarding their sensitivity toward the child at four months of the child’s age. Taking into account the enormous importance that sensitive parenting is considered to have for secure attachment and child development, this result is alarming. We need more understanding about the key elements which should be focused on and included in interventions.
In previous empirical studies regarding maternal interaction behaviour, substance-abusing mothers have been found to be less sensitive in interaction with their children, less emotionally engaged, attentive, resourceful, flexible and contingent, to experience less pleasure in the interaction and to be more intrusive in their behaviour (Eiden, 2001; Johnson, Morrow, Accornero, Lihua, Anthony, & Bandstra, 2002; LaGasse et al., 2003; Mayes & Truman, 2002; Pajulo, Savonlahti, Sourander, Ahlqvist, Helenius, & Piha, 2001). Mother-baby pairs have shown fewer moments of dyadic interaction, the quality of the dyadic interaction has lacked enthusiasm and mutual enjoyment, and has included more dyadic conflict and less mutual arousal (Burns, Chetnik, Burns, Clark, 1991; Burns, Chetnik, Burns, & Clark, 1997; Eiden, 2001; Mayes, Feldman, Granger, Haynes, Bornstein, & Schottenfeld, 1997).
Although the RF level within the pilot group was generally weak, individual differences were found, as scores were ranging from very weak to normal. In accordance with our hypothesis, higher level of maternal RF tended to be associated with more sensitive interaction behavior with the child postnatally.
The few previous studies on maternal reflective abilities have shown that RF is generally weak among substance abusing populations (Suchman, DeCoste, Schmitt, Legow, & Mayes, 2007). Maternal RF has been found to predict child attention, withdrawal, social skills, adaptability to parenting stress and parent-child dysfunction, and to mediate the link between drug use, child social skills, parent distress and parent-child dysfunction between mothers and their 4–8 years old children (Truman et al., 2004).
We also hypothesized that the residential treatment intervention enhances maternal RF between the prenatal and postnatal assessment period. Among those mothers who completed assessments of their reflective ability both in pregnancy (i.e. who entered the unit early enough) and at 4 months postpartum the RF score increased. We propose that this increase is due to the intervention. However, we don’t know if RF might have increased anyway, as part of a natural mental maturational process preparing the mother for maternity. In another recent study using outpatient, 12-week intervention and the same RF measures with substance abusing mothers, RF was found to increase with marginal significance (p=0.10) (Suchman et al. 2007). The items in the two RF interviews were different, naturally due to the fact that they are used in different phases (pregnancy vs. postnatal period). One might speculate that this also would have lead to different RF scores. However, the ratings were carried out by the same outside rater and according to precisely the same scoring system.
Previous studies have shown high rate of co-morbidity between substance abuse and psychiatric symptomatology among women (Luthar, Cushing, Merikangas, & Rounsaville, 1998). The amount of severe psychotic and paranoid symptoms within this group, however, raises concern. It seems that more attention should be paid to the type of psychiatric symptomatology of the mothers, and more active cooperation between residential treatment providers and adult psychiatrists is also perhaps warranted, at least in our country.
Maternal psychiatric symptomatology is considered to be one of the strongest risk factors for maternal sensitivity (Seifer & Dickstein, 2000). According to the pilot findings, the relation between the two seems to be more complex. By clinical experience, some depressed mothers have shown a capacity to relate to their child in a surprisingly sensitive way, and somehow to protect that area in their life from the deleterious effects of a psychiatric problem. We propose that higher maternal reflective functioning may be the factor “breaking through,” making it possible for a mother to behave more sensitively with her child even in situations characterized by other severe risks.
Conclusions and clinical implications
There is a great need for theoretically driven and accurately focused interventions among psychosocial high-risk groups. We propose that the concept of parental reflective functioning has especially strong relevance for substance abusing mother-baby couples and their treatment. The crucial question with these mother-baby pairs is how to ensure a sustained abstinence from substances and good enough interaction between the mother and the child after the intensive support in residential setting. We propose that maternal RF plays a key role in both of these aims, especially in its emphasis on how well the mother is able to keep the child in her mind. We are now collecting 2-year follow-up data with a larger sample of mother-baby pairs in treatment to explore this.
How is it that facilitating effective parenting among substance using women may also facilitate their efforts toward abstinence? We suggest that this relates to the relationship between central reward pathways in the brain and the capacity to invest in another person as in parenting or to become addicted. Many of the abused substances have been shown to affect the dopaminergic pathways in the brain, areas which are associated with initiation of behavior, hedonic reward and motivation. These central dopaminergic pathways are also critically involved in an adult’s capacity to invest in the care of the new infant. Drug abuse may be seen as a co-optation or hijacking of this endogenous value system. As a consequence, once this system is coopted by an addiction to a drug of abuse, the individual is less able to invest in caring for an infant or another person and there is competition between investment in craving the drug and in caring for the infant (Leckman & Mayes, 1998). In the treatment model described in this article, the mothers are helped to invest in their child instead of substances, and to “reset” the focus of the reward system by intensively facilitating and enhancing the mother’s satisfaction with positive interaction experiences with her baby and with being a parent. The individual becomes less focused on her relationship with and craving for the drug and more on her preoccupation with and investment in the infant.
Although the treatment model presented here already contains elements of enhancing maternal RF, there is still a lot that could be done more accurately and systematically with that focus in mind, so that more mothers could transition from the high-risk to the reflective and more sensitive levels in interactions with their children.
Contributor Information
Marjukka Pajulo, Turku University Hospital (Finland), Child Psychiatry Clinic, infant psychiatric team
Nancy Suchman, Assistant Professor, Dept. of Psychiatry, Yale University School of Medicine, CT, USA
Mirjam Kalland, Associate Professor, Dept. of Social and Family services, University of Helsinki, Finland
Jari Sinkkonen, Save the Children Organization, Finland
Hans Helenius, Dept. of Biostatistics, University of Turku, Finland
Linda Mayes, Professor, Child Study Center, Yale University, CT, USA
References
- Ainsworth MDS, Blehar MC, Waters E, Wall S. Patterns of attachment: assessed in the strange situation and at home. Hillsdale, NJ: Lawrence Erlbaum; 1978. [Google Scholar]
- Barth RD, Needell B. Outcomes of drug-exposed children four years post-adoption. Children and Youth Services Review. 1996;18:37–56. [Google Scholar]
- Bauman P, Levine SA. The development of children of drug addicts. International Journal of Addiction. 1986;21:849–863. doi: 10.3109/10826088609027399. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant Development. 2 (BSID II) San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- Beeghly M, Tronick EZ. Effects of prenatal exposure to cocaine in early infancy: toxic effects on the process of mutual regulation. Infant Mental Health Journal. 1994;15(2):158–175. [Google Scholar]
- Blackwell P, Kirkhart K, Schmitt D, Kaiser M. Cocaine/polydrug-affected dyads: implications for infant cognitive development and mother-infant interaction during the first six postnatal months. Journal of Applied Developmental Psychology. 1998;19(2):235–248. [Google Scholar]
- Brockington I. Motherhood and mental illness. New York: Oxford University Press Inc; 1996. [Google Scholar]
- Burns K, Chetnik L, Burns WJ, Clark R. Dyadic disturbances in cocaine-abusing mothers and their infants. Journal of Clinical Psychology. 1991;47(2):316–319. doi: 10.1002/1097-4679(199103)47:2<316::aid-jclp2270470220>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Burns KA, Chetnik L, Burns WJ, Clark R. The early relationship of drug abusing mothers and their infants: an assessment at eight to twelve months of age. Journal of Clinical Psychology. 1997;53:279–287. doi: 10.1002/(sici)1097-4679(199704)53:3<279::aid-jclp11>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Carmichael Olson H, O’Connor M, Fitzgerald HE. Lessons learned from study of the developmental impact of parental alcohol use. Infant Mental Health Journal. 2001;22(3):271–290. [Google Scholar]
- Cassidy B, Zoccolillo M, Hughes S. Psychopathology in adolesecent mothers and its effects on mother-infant interactions: a pilot study. Canadian Journalof Psychiatry. 1996;41:379–384. doi: 10.1177/070674379604100609. [DOI] [PubMed] [Google Scholar]
- Ciotti F, Lambruschi F, Pittino B, Crittenden P. La valutazione della relatzione precoce madre-bambino in una popolazione di madri con una storia di tossicodipendenza attraverso l’uso del CARE-Index. Psicoterapia Cognitiva e Comportamentale. 1998;4:53–59. [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Cramer B, Robert-Tissot C, Stern DN, Serpa-Rusconi S. Outcome evaluation in brief mother-infant psychotherapy: a preliminary report. Infant Mental Health Journal. 1990;11:278–300. [Google Scholar]
- Crittenden P. Children’s strategies for coping with adverse home environments. Child Abuse and Neglect: The International Journal. 1992;16:329–343. doi: 10.1016/0145-2134(92)90043-q. [DOI] [PubMed] [Google Scholar]
- Crittenden P. Coding manual. Miami, USA: Family Relations Institute; 2003. Care Index for Infants and Toddlers. [Google Scholar]
- Crittenden P, Bonvillian JD. The effect of maternal risk status on maternal sensitivity to infant cues. American Journal of Orthopsychiatry. 1984;54:250–262. doi: 10.1111/j.1939-0025.1984.tb01492.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory (BSI): administration, scoring and procedures manual. 3. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Eiden R. Maternal substance use and mother-infant feeding interactions. Infant Mental Health Journal. 2001;22(4):497–411. [Google Scholar]
- Fonagy P, Steele M, Moran GS, Steele H, Higgitt AC. Measuring the ghosts in the nursery: a summary of the main findings of the Anna Freud Centre/University College London Parent-Child Study. Bulletin of the Anna Freud Center. 1991;14:115–131. [Google Scholar]
- Fonagy P, Target M. Playing with reality: theory of mind and the normal development of psychic reality. International Journal of Psychoanalysis. 1996;77:217–233. [PubMed] [Google Scholar]
- Fonagy P, Gergely G, Jurist E, Target M. Affect regulation, mentalization and the development of the self. New York: Other Press; 2002. [Google Scholar]
- Fonagy P, Steele H, Steele M. Maternal representations of attachment during pregnancy predict the organization of infant-mother attachment at one year of age. Child Development. 1991;62:891–905. doi: 10.1111/j.1467-8624.1991.tb01578.x. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Steele M, Steele H, Leigh T, Kennedy R, Mattoon G, Target M. Attachment, the reflective self and borderline states: the predictive specificity of the Adult Attachment Interview and pathological emotional development. In: Goldberg S, Muir R, Kerr J, editors. Attachment theory: social, developmental and clinical perspectives. New York: Analytic Press; 1995. pp. 233–278. [Google Scholar]
- Goyette-Ewing M, Slade A, Knoebber K, Gilliam W, Truman S, Mayes L. Manual for scoring. Yale Child Study Center; CT, USA: 2002. Parents first: a developmental parenting program. [Google Scholar]
- Grella CE, Joshi V, Hser YI. Program variation in treatment outcomes among women in residential drug treatment. Evaluation Review. 2000;24(4):364–383. doi: 10.1177/0193841X0002400402. [DOI] [PubMed] [Google Scholar]
- Grienenberger J, Kelly K, Slade A. Maternal reflective functioning, mother-infant affective communication and infant attachment: exploring the link between mental states and observed caregiving behaviour. Attachment and Human Development. 2005;7(3):299–311. doi: 10.1080/14616730500245963. [DOI] [PubMed] [Google Scholar]
- Hurt H, Brodsky N, Betancourt L, Braitman L, Malmud E, Giannetta J. Cocaine-exposed children: follow-up through 30 months. Journal of Developmental and Behavioral Pediatrics. 1995;16:29–35. [PubMed] [Google Scholar]
- Johnson AL, Morrow CE, Accornero VH, Lihua X, Anthony JC, Bandstra ES. Maternal cocaine use: estimated effects on mother-child play interactions in the preschool period. Developmental and Behavioral Pediatrics. 2002;23(4):191–202. doi: 10.1097/00004703-200208000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalland M. Kiintymyssuhdeteorian kliininen merkitys. Soveltaminen erityistilanteissa (Clinical relevance of attachment theory. Specific situations) In: Sinkkonen J, Kalland M, editors. Varhaiset ihmissuhteet ja niiden häiriintyminen (Early human relationships and their disturbances) Helsinki: WSOY; 2001. pp. 198–233. [Google Scholar]
- LaGasse LL, Messenger D, Lester BM, Seifer R, Tronick EZ, Bauer CR, Shankaran S, Bada HS, Wright LL, Smeriglio VL, Finnegan LP, Maza PL, Liu J. Prenatal drug exposure and maternal and infant feeding behaviour. Archives of Disease in Childhood. 2003;88(5):391–399. doi: 10.1136/fn.88.5.F391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leckman JF, Mayes LC. Understanding developmental psychopathology: how useful are evolutionary accounts? Journal of American Academy of Child and Adolescent Psychiatry. 1998;37(10):1011–1021. doi: 10.1097/00004583-199810000-00010. [DOI] [PubMed] [Google Scholar]
- Lester BM, Tronick EZ. The effects of prenatal cocaine exposure and child outcome. Infant Mental Health Journal. 1994;15(2):107–120. [Google Scholar]
- Luthar SS, Cushing G, Merikangas KR, Rounsaville BJ. Multiple jeopardy: risk and protective factors among addicted mothers’ offspring. Development and Psychopathology. 1998;10(1):117–136. doi: 10.1017/s0954579498001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayes L, Truman S. Substance abuse and parenting. In: Bornstein M, editor. Handbook of parenting, volume 4. Social conditions and applied parenting. 2. Mahvah, NJ: Lawrence Erlbaum Associates; 2002. pp. 329–359. [Google Scholar]
- Mayes L, Feldman R, Granger R, Haynes O, Bornstein M, Schottenfeld R. The effects of polydrug use with and without cocaine on mother-infant interaction at 3 and 6 months. Infant Behavior and Development. 1997;20(4):489–502. [Google Scholar]
- Meins E, Fernyhough C, Fradley E, Tuckey M. Rethinking maternal sensitivity: Mother’s comments on infants’ mental processes predict security of attachment at 12 months. Journal of Child Psychology and Psychiatry. 2001;42(5):647–648. [PubMed] [Google Scholar]
- Moe V, Slinning K. Children prenatally exposed to substances: gender-related differences in outcome from infancy to 3 years of age. Infant Mental Health Journal. 2001;22:334–350. [Google Scholar]
- Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh Postnatal Depression Scale (EPDS) Journal of Reproductive and Infant Psychology. 1990;8:99–107. [Google Scholar]
- Nellis L, Gridley B. Review of the Bayley Scales of Infant Development, 2nd edition. Journal of School Psychology. 1994;32:212–219. [Google Scholar]
- Pacquette D, Bigras M, Zoccolillo M, Tremblay R, Labelle ME, Azar R. Comparison de la sensibilite parentale entre des meres adolescentes et des meres adultes peu scolarisees. Revue de Psychoeducation et d’Orientation. 2001;30:283–298. [Google Scholar]
- Pajulo M. Doctoral thesis. University of Turku; Finland: 2001. Early motherhood at risk: mothers with substance dependency. [Google Scholar]
- Pajulo M, Savonlahti E, Sourander A, Ahlqvist S, Helenius H, Piha J. An early report on the mother-baby interactive capacity of substance-abusing mothers. Journal of Substance Abuse Treatment. 2001;20:143–151. doi: 10.1016/s0740-5472(00)00161-6. [DOI] [PubMed] [Google Scholar]
- Pajulo M, Suchman N, Kalland M, Mayes LC. Enhancing the effectiveness of residential treatment for substance abusing pregnant and parenting women: focus on maternal reflective functioning and mother-child relationship. Infant Mental Health Journal. 2006;27(5):448–465. doi: 10.1002/imhj.20100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patino FL. Mothers’ prenatal attachment history, attachment status and social support satisfaction as predictors of postnatal maternal sensitivity. Dissertation Abstracts International. 1993;53:3787. [Google Scholar]
- Schechter DS, Kaminer T, Grienenberger JF, Amat J. Fits and starts: a motherinfant case-study involving intergenerational violent trauma and pseudoseizures across three generations. Infant Mental Health Journal. 2003;24(5):510–528. doi: 10.1002/imhj.10070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schechter DS, Zeanah C, Myers MM. Negative and distorted maternal attributions among violence-exposed mothers of very young children before and after single-session feedback: are maternal psychopathology and reflective functioning predictive?. Paper presented at the meeting of the World Association of Infant MentalHealth; Amsterdam, The Netherlands. 2002. [Google Scholar]
- Schuler M, Nair P, Harrington D. Developmental outcome of drug-exposed children through 30 months: a comparison of Bayley and Bayley II. Psychological Assessment. 2003;15(3):435–438. doi: 10.1037/1040-3590.15.3.435. [DOI] [PubMed] [Google Scholar]
- Seifer R, Dickstein S. Parental mental illness and infant development. In: Zeanah CH, editor. Handbook of infant mental health. New York: The Guilford Press; 2000. pp. 145–160. [Google Scholar]
- Slade A, Bernbach E, Grienenberger J, Levy DW, Locker A. The parent development interview and The pregnancy interview. Yale Child Study Center; CT, USA: 2002, 2005. Manual for scoring. [Google Scholar]
- Slade A, Grienenberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning and attachment: considering the transmission gap. Attachment and Human Development. 2005;7(3):283–298. doi: 10.1080/14616730500245880. [DOI] [PubMed] [Google Scholar]
- Suchman N, DeCoste C, Schmitt N, Legow N, Mayes L. The Mothers and Toddlers Program: Preliminary findings from an attachment-based parenting intervention for substance abusing mothers. Psychoanalytic Psychology. 2007 doi: 10.1037/0736-9735.25.3.499. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman NE, Altomare M, Moller F, Slade A, Mayes L. Emotionally responsive parenting: a new parenting intervention for drug dependent mothers. Paper presented at the Annual Meeting of College on Problems of Drug Dependence; Bal Harbour, FL, USA. 2003. [Google Scholar]
- Suchman NE, Mayes L, Conti J, Slade A, Rounsaville B. Rethinking parenting interventions for drug dependent mothers: from behavioural management to fostering emotional bonds. Journal of Substance Abuse Treatment. 2004;27:179–185. doi: 10.1016/j.jsat.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Suchman NE, McMahon TJ, Slade A, Luthar SS. How early bonding, depression, illicit drug use and perceived support work together to influence drug dependent mothers’ caregiving. American Journal of Orthopsychiatry. 2005;75(3):431–445. doi: 10.1037/0002-9432.75.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Truman SD, Levy D, Mayes LC. Reflective functioning as mediator between drug use, parenting stress and child behaviour. 2004 Unpublished manuscript. [Google Scholar]
- Ward MJ, Carlson EA. The predictive validity of the Adult Attachment Interview for adolescent mothers. Child Development. 1995;66:69–79. doi: 10.1111/j.1467-8624.1995.tb00856.x. [DOI] [PubMed] [Google Scholar]