Abstract
Objective
Although tight glucose control is widely used in hospitalized patients, there is concern that medication-induced hypoglycemia may worsen patient outcomes. We sought to determine if the mortality risk associated with hypoglycemia in hospitalized non-critically ill patients is linked to glucose-lowering medications (drug-associated hypoglycemia) or if it is merely an association mediated by comorbidities (spontaneous hypoglycemia).
Methods
Retrospective cohort of patients admitted to the general wards of an academic center during 2007. The in-hospital mortality risk of a hypoglycemic group (at least one blood glucose ≤ 70 mg/dl) was compared to that of a normoglycemic group using survival analysis. Stratification by subgroups of patients with spontaneous and drug-associated hypoglycemia was performed.
Results
Among 31,970 patients, 3,349 (10.5%) had at least one episode of hypoglycemia. Patients with hypoglycemia were older, had more comorbidities, and received more antidiabetic agents. Hypoglycemia was associated with increased in-hospital mortality (HR: 1.67, 95% CI, 1.33 to 2.09, p<0.001). However, this greater risk was limited to patients with spontaneous hypoglycemia (HR: 2.62, 95% CI, 1.97 to 3.47, p<0.001), not to those with drug-associated hypoglycemia (HR: 1.06, 95% CI, 0.74 to 1.52, p=0.749). After adjustment for patient comorbidities, the association between spontaneous hypoglycemia and mortality was eliminated (HR: 1.11, 95% CI, 0.76 to 1.64, p=0.582).
Conclusions
Drug-associated hypoglycemia was not associated with increased mortality risk in patients admitted to the general wards. The association between spontaneous hypoglycemia and mortality was eliminated after adjustment for comorbidities, suggesting that hypoglycemia may be a marker of disease burden rather than a direct cause of death.
Keywords: Hypoglycemia, mortality, hypoglycemia in general ward patients
Hyperglycemia in hospitalized patients with and without diabetes is common and has been implicated as a risk factor for increased morbidity and mortality 1–5. While a randomized controlled trial of “tight” glycemic control in critically ill patients has demonstrated decreased mortality6, other studies have shown no benefits or even increased mortality with this therapeutic approach 7–11. Despite these contradictory results in intensive care unit (ICU) patients, physicians have widely adopted tight glycemic control in hospitalized patients with hopes of improving outcomes. Enthusiasm for glucose-lowering interventions has been tempered by the concern that treatment-induced hypoglycemia may cause death. Although trials of intensive glucose control have shown higher rates of hypoglycemia than standard glucose management 9,12,13, and hypoglycemia has been associated with increased mortality 14–17, it is not clear whether hypoglycemia that occurs as a result of glucose-lowering therapy is associated with increased mortality.
Studies conducted in the outpatient setting usually serve to provide guidance in the management of hospitalized but not critically ill patients. In this regard, two multi-center outpatient clinical trials comparing the effects of intensive versus standard glycemic control in patients with advanced type 2 diabetes were recently completed and showed no significant reduction in cardiovascular disease outcomes nor any increased mortality with intensive glycemic control 18,19. A third outpatient trial, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study, was terminated because of increased mortality in participants randomized to receive intensive glycemic therapy 20. However, a post hoc analysis of ACCORD was unable to attribute the excess mortality observed in the intensive therapy group to severe hypoglycemia 21. Thus, it remains unclear whether hypoglycemia is responsible for increased mortality or it is just a marker of disease burden.
To address this important knowledge gap, we designed a retrospective observational study to determine first, whether hypoglycemia was associated with increased mortality in hospitalized but non-critically ill patients; and second, whether hypoglycemia associated with various illnesses that occurs in the absence of glucose-lowering therapy (“spontaneous hypoglycemia”) and hypoglycemia that is associated with initiation of glucose-lowering therapy (“drug-associated hypoglycemia”) carry similar prognostic implications. Specifically, we posited that if hypoglycemia per se were a direct cause of adverse outcomes, it would be expected to be associated with increased mortality regardless of its etiology. On the other hand, if hypoglycemia was a marker of disease burden, only spontaneous hypoglycemia would be associated with increased mortality.
RESEARCH DESIGN AND METHODS
Study Population
We examined a retrospective cohort of patients hospitalized at Montefiore Medical Center in Bronx, New York, from January 1st to December 31st, 2007. The data assembled were restricted to non-pregnant patients ages 21 years or greater, and included those with and without the concurrent diagnosis of diabetes, who were admitted to the general units. Patients admitted or transferred to medical or surgical intensive care units, and those discharged from the emergency room were excluded from this analysis. For patients with multiple admissions, only the earliest admission was considered as an index hospitalization. Patients were included if their record had at least one blood glucose level performed during the period of hospitalization, which yielded a starting data set of 31,970 patients. The diabetes subgroup (n = 10,832) included patients with both type 1 and type 2 diabetes determined from International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes (ICD-9 codes) of inpatient and outpatient charts.
Data Source, hypoglycemia and comorbidities definition, and medications
All data was extracted from the hospital information system using Clinical Looking Glass™ (version 2.1.5, Bronx, NY). We defined the “hypoglycemia” group as those patients with at least one laboratory-documented blood glucose level ≤ 70 mg/dl. We used this threshold according to the definition provided by the American Diabetes Association22. We only used chemistry profiles and excluded patients with point of care (POC) glucose values < 70 mg/dl because 1) these are entered into the computer system manually by nurses and they are subject to more data entry errors than those values directly transmitted from the laboratory, 2) we thought we would encounter multiple short and trivial episodes of hypoglycemia evidenced by POC only in the group receiving anti-diabetic agents that would not necessarily be seen in the chemistry profiles and that would not be associated with increased mortality, thus favoring our hypothesis, and 3) we wanted to choose a more conservative approach of clearly documented hypoglycemia in a laboratory chemistry profile that would most likely represent a true episode of hypoglycemia. The “normoglycemia” group consisted of patients with all glucose levels > 70 mg/dl. “Spontaneous hypoglycemia” was defined as hypoglycemia occurring in the absence of glucose-lowering interventions; “drug-associated hypoglycemia” was hypoglycemia occurring in patients who were receiving glucose-lowering medications. Comorbidities were determined from ICD-9 codes and, whenever possible, enriched by including patients who met laboratory criteria for disease, and consisted of: body mass index, diabetes mellitus, congestive heart failure, myocardial infarction, cerebro-vascular accident, cancer, chronic obstructive pulmonary disease, shock, albumin level (as a surrogate for chronic illness, malnutrition, or liver disease when low), white blood cell count, and renal failure defined as a serum creatinine level ≥ 2 mg/dl. All medications were prescribed electronically and those administered during the patients’ hospital stay were abstracted from the database. Anti-diabetic oral agents included sulfonylureas, metformin, thiazolidinediones (TZDs), glucagon-like peptide 1 (GLP-1) analogs, dipeptidyl peptidase 4 inhibitors (DPP-4i). Insulin therapy encompassed both human insulin and insulin analogs administered as basal (NPH-protamine insulin, or glargine), and/or bolus (regular insulin or rapid acting analogs).
Statistical analysis
All statistical analyses were performed using STATA/IC (version 10 for Windows; College Station, TX). Baseline demographic and clinical characteristics were compared between patients in the “hypoglycemia” group and patients in the “normoglycemia” group using Pearson X2 test for categorical variables and Student t test or Mann-Whitney test for continuous variables.
To determine if hypoglycemia was associated with decreased survival, in-hospital mortality rates were compared between the hypoglycemia group and the normoglycemia group using logistic regression. Mortality analysis was repeated stratified by the presence or absence of diabetes. We further examined the relationship between glycemia and in-hospital mortality using Kaplan-Meier survival estimates in the hypoglycemic and normoglycemic groups and conducted the remaining univariate and multivariate analyses using survival analysis. Proportionality assumptions were tested with Schoenfeld residuals and log-log plots.
Because we hypothesized that there would be a differential effect of hypoglycemia resulting from treatment with antidiabetic medication (drug-associated hypoglycemia) vs. spontaneous hypoglycemia, we explored the interaction between antidiabetic medications and hypoglycemia and conducted separate analyses for subgroups of patients with drug-associated vs. spontaneous hypoglycemia. We also conducted sensitivity analyses using a glucose cut-off of 50mg/dl, and we performed sub-analyses by class of anti-diabetic agent to determine the specific effect of drugs known to cause hypoglycemia (i.e. sulfonylureas and insulin) on mortality. We examined the association between number of hypoglycemic episodes and mortality in the drug-associated and spontaneous hypoglycemic groups. Patients without hypoglycemic episodes (normoglycemia) served as the reference group and were compared with patients having one, two, and three or more hypoglycemic episodes.
Multivariate Cox proportional hazards models were constructed to examine the independent association between hypoglycemia and mortality. We conducted stratified analyses for patients with drug-associated and spontaneous hypoglycemia. Patient characteristics previously demonstrated to be prognostically significant or thought to be clinically important, and covariates identified in bivariate analyses as predictors of in-hospital mortality were entered into the models. Covariates included demographic factors: age, sex, self-reported race/ethnicity; comorbidities: body mass index, diabetes mellitus, congestive heart failure, myocardial infarction, cerebro-vascular accident, cancer, chronic obstructive pulmonary disease, shock, albumin level (as a surrogate for chronic illness, malnutrition, or liver disease when low), white blood cell count, and renal failure defined as a serum creatinine level ≥ 2 mg/dl; and number of glucose determinations.
The literature reports an increase of in-hospital mortality risk of hypoglycemic compared to normoglycemic patients ranging between 60% and 300%.15–17,23 We performed a power calculation with the most conservative estimate of increased mortality risk in the hypoglycemic group. With our actual sample size, we calculated that we would have had 80% power to detect a 60% increase in mortality risk in hypoglycemic subjects compared to normoglycemic subjects using a two-tailed α of 0.05. All power determinations were calculated using PASS 11 2010 (version 11.0.2, 2010, http://www.ncss.com/pass.html).
RESULTS
Baseline characteristics
We identified 31,970 patients with at least one blood glucose determination during their hospitalization (mean age 61 ± 17.8 years, 58% females). Self-designated race/ethnicity was available in 92.6% of patients (Whites: 23.6%, Blacks: 32.2%, Hispanics: 36.8%, unknown: 7.4%). Table 1 presents baseline patient characteristics of those subjects who did (n= 3,349) and did not (n=28,621) develop hypoglycemia during their hospital stay. The proportion of females was similar between the two groups. There was a higher percentage of non-Hispanic Blacks in the hypoglycemic group. Compared with patients who did not develop hypoglycemia, those with hypoglycemic events were older, had a lower body mass index, had more co-morbidities including diabetes, and received more insulin, sulfonylureas, or a TZD. There were fewer patients in the hypoglycemia group receiving metformin.
Table 1.
Patient Characteristics by Glycemia Status
| Hypoglycemia (n=3,349) |
Normoglycemia (n=28,621) |
p-value | |
|---|---|---|---|
| Demographic data | |||
| Age in years, mean (SD) | 64.1 (17.3) | 60.6 (17.9) | <.001 |
| Female sex, n, (%) | 1,918 (57.3) | 16,765 (58.6) | 0.15 |
| Whites, n, (%) | 732 (21.9) | 6,829 (23.9) | 0.01 |
| Blacks, n, (%) | 1,234 (36.9) | 9,045 (31.6) | <.001 |
| Hispanics, n, (%) | 1,179 (35.2) | 10,577 (36.9) | 0.047 |
| Clinical data | |||
| Body mass index, mean(SD) | 27.1 (7.5) | 29.1 (7.8) | <.001 |
| Diabetes n, (%) | 1,717 (51.3) | 9,115 (31.9) | <.001 |
| Congestive heart failure n,(%) | 944 (28.2) | 3,984 (14.0) | <.001 |
| Myocardial infarction n, (%) | 311 (9.3) | 2,005 (7.1) | <.001 |
| Cerebro-vascular accident n, (%) | 318 (9.5) | 2,038 (7.2) | <.001 |
| Cancer n, (%) | 389 (11.6) | 2,355 (8.3) | <.001 |
| Shock n, (%) | 75 (2.24) | 134 (0.47) | <.001 |
| Chronic obstructive pulmonary disease n, (%) | 775 (23.2) | 5,969 (21.0) | 0.004 |
| White blood cell count, median (iq range) | 9.2 (6.8–12.8) | 8.7 (6.7–11.7) | <.001 |
| Albumin, mean (SD) | 3.46 (0.71) | 3.85 (0.56) | <.001 |
| Renal failure n, (%) | 804 (24.1) | 1,968 (7.0) | <.001 |
| In-hospital medications | |||
| Sulfonylureas, n, (%) | 342 (10.2) | 1,570 (5.5) | <.001 |
| Metformin, n, (%) | 169 (5.1) | 1,737 (6.1) | 0.02 |
| Thiazolidinediones, n, (%) | 132 (3.9) | 922 (3.22) | 0.03 |
| DPP-4i/GLP-1, n, (%) | 4 (0.12) | 33 (0.12) | 0.95 |
| Any insulin, n, (%) | 1,447 (43.2) | 4,650 (16.3) | <.001 |
| Any oral, n, (%) | 480 (14.3) | 3,154 (11.0) | <.001 |
| Any oral or insulin, n, (%) | 1,635 (48.8) | 6,670 (23.3) | <.001 |
Overall, 3,349 patients (10.5%) developed a total of 5,884 episodes of hypoglycemia. Spontaneous hypoglycemia occurred in 1,714 patients, drug-associated hypoglycemia happened in 1,635 individuals. Among patients with diabetes, those treated with insulin experienced higher rates of hypoglycemia compared with those who were not treated with insulin (23.7% [1,447/6,097 patients] vs 7.4% [1,902/25,873], p<0.001).
Unadjusted association between hypoglycemia and mortality
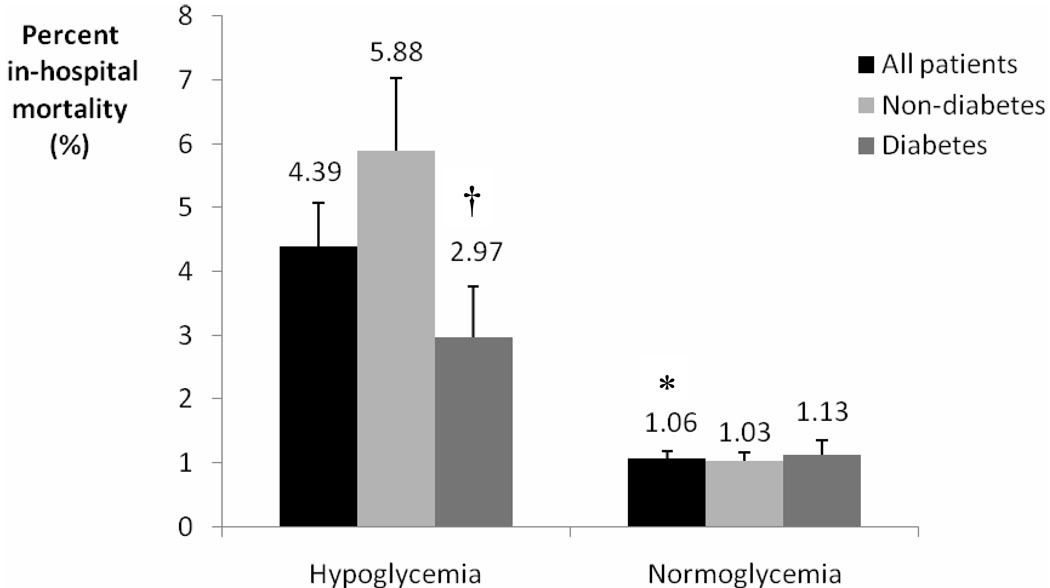
Figure 1 shows that patients with hypoglycemia had significantly higher in-hospital mortality than patients without hypoglycemia (4.39% [147/3,349] vs. 1.06% [304/28,621], p<0.001). Both diabetic and non-diabetic patients with hypoglycemia had significantly increased in-hospital mortality compared to patients without hypoglycemia. Non-diabetic patients with hypoglycemia had almost double the mortality rate than diabetic patients with hypoglycemia (5.88% vs 2.97%, p<0.001).
Figure 1.
Percent in-hospital mortality by glycemia status among all patients, patients with diabetes, and patients without diabetes.
* p <0.001 for all hypoglycemic versus normoglycemic patients.
† p <0.001 for non-diabetic hypoglycemic patients versus diabetic hypoglycemic patients.
Patients with hypoglycemia had significantly higher mortality compared to normoglycemic patients (HR: 1.67, 95% CI, 1.33–2.09, p<0.001, Table 2). However, the association between hypoglycemia and mortality was markedly different among subjects who developed it spontaneously vs. those who developed it following glucose-lowering therapy [p=0.001 for hypoglycemia × antidiabetic medications interaction]. Among patients not treated with insulin or oral antidiabetic agents (spontaneous hypoglycemia), those with hypoglycemia had significantly higher mortality compared with those who did not develop hypoglycemia (HR: 2.62, 95% CI, 1.97–3.47, p<0.001). In contrast, among patients treated with insulin or oral antidiabetic agents (drug-associated hypoglycemia), mortality hazards were similar between those who did and did not develop hypoglycemia (HR: 1.06, 95% CI, 0.74–1.52, p=0.749). Sensitivity analyses using a glucose cut-off of 50 mg/dl showed similar results. Table 2a shows a sub-group analysis by drug class. The specific group who developed hypoglycemia associated with sulfonylureas and/or insulin did not have an increased mortality hazard compared to the normoglycemic group on the same drugs. The small number of deaths observed in patients receiving Metformin, TZDs, as well as sulfonylureas likely reflects the fact that oral drugs are discouraged during hospitalization and insulin is preferentially used.
Table 2.
| Unadjusted in-hospital mortality of all hypoglycemic patients, patients with spontaneous hypoglycemia, and patients with drug-associated hypoglycemia compared to normoglycemic patients. | ||||
|---|---|---|---|---|
| Hazard ratio |
Number of deaths |
p-value | 95% CI | |
| All hypoglycemic patients | 1.67 | 451 | <0.001 | 1.33 to 2.09 |
| Spontaneous hypoglycemia | 2.62 | 287 | <0.001 | 1.97 to 3.47 |
| Drug-associated hypoglycemia | 1.06 | 164 | 0.749 | 0.74 to 1.52 |
| 2a – Sub-analysis of in-hospital mortality of patients who developed hypoglycemia compared to normoglycemic patients by class of anti-diabetic drug. | ||||
|---|---|---|---|---|
| Hazard ratio |
Number of deaths |
p-value | 95% CI | |
| Sulfonylureas | 0.90 | 14 | 0.880 | 0.23 to 3.48 |
| Metformin | 1.28 | 5 | 0.855 | 0.09 to 17.7 |
| Thiazolidinediones | 0.01 | 4 | 1 | - |
| Any insulin | 0.98 | 158 | 0.907 | 0.68 to 1.40 |
| Any sulfonylurea and/or insulin | 0.97 | 163 | 0.867 | 0.68 to 1.39 |
Of the 3,349 patients with hypoglycemia, 64.3% had 1 episode, 19.1% had 2 episodes, and 16.6% had 3 or more episodes. We found an association between the number of spontaneous hypoglycemic episodes and in-hospital mortality (p for trend <0.001), but there was no significant association between the number of drug-associated hypoglycemic events and in-hospital mortality (p for trend = 0.562, Table 3).
Table 3.
Number of hypoglycemic episodes and in-hospital mortality.
| Hazard ratio |
p-value | 95% CI | |
|---|---|---|---|
| Spontaneous hypoglycemia* | |||
| 1 epsiode | 1.73 | 0.006 | 1.17 to 2.57 |
| 2 episodes | 3.78 | <0.001 | 2.32 to 6.15 |
| 3 or more episodes | 4.86 | <0.001 | 3.11 to 7.60 |
| Drug-associated hypoglycemia† | |||
| 1 episode | 0.99 | 0.962 | 0.64 to 1.54 |
| 2 episodes | 1.12 | 0.683 | 0.64 to 1.96 |
| 3 or more episodes | 1.15 | 0.596 | 0.68 to 1.94 |
p for trend <0.001
p for trend= 0.562
Adjusted association between hypoglycemia and mortality
After multivariate adjustment for age, sex, race, and number of glucose determinations (Table 4, model 1), the association between hypoglycemia and mortality remained significantly different for patients with spontaneous hypoglycemia vs. those with drug-associated hypoglycemia (p<0.001 for adjusted interaction). Spontaneous hypoglycemia was significantly associated with higher risk of mortality (HR: 2.84, 95% CI, 2.14–3.76, p<0.001) while drug-associated hypoglycemia was not (HR: 0.95, 95% CI, 0.66–1.36, p=0.762). To determine if the association between hypoglycemia and mortality was attenuated after adjustment for comorbidities, we constructed serial regression models. In model 1, we adjusted for patient demographics and found a strong and significant association between spontaneous hypoglycemia and mortality (HR: 2.84, 95% CI, 2.14–3.76, p<0.001). In contrast, in model 2, after adjustment for patient demographics and comorbidities, the association between spontaneous hypoglycemia and mortality was eliminated (HR: 1.11, 95% CI, 0.76–1.64, p=0.582, Table 4, model 2). Among patients with drug-associated hypoglycemia, the relationship between hypoglycemia and mortality remained non-significant after adjustment for comorbidities (HR: 0.72, 95% CI, 0.45–1.13, p=0.155).
Table 4.
Adjusted in-hospital mortality of patients with spontaneous hypoglycemia and patients with drug-associated hypoglycemia compared to normoglycemic patients.
| Hazard ratio |
Number of deaths | p-value | 95% CI | |
|---|---|---|---|---|
| Model 1 | ||||
| Spontaneous hypoglycemia | 2.84 | 287 | <0.001 | 2.14 to 3.76 |
| Drug-associated hypoglycemia | 0.95 | 164 | 0.762 | 0.66 to 1.36 |
| Model 2 | ||||
| Spontaneous hypoglycemia | 1.11 | 171 | 0.582 | 0.76 to 1.64 |
| Drug-associated hypoglycemia | 0.72 | 114 | 0.155 | 0.45 to 1.13 |
Model 1: hypoglycemia adjusted by age, sex, race, and number of glucose determinations.
Model 2: hypoglycemia adjusted by age, sex, race, body mass index, diabetes mellitus, congestive heart failure, myocardial infarction, cerebro-vascular accident, cancer, chronic obstructive pulmonary disease, shock, white blood cell count, albumin, creatinine, number of glucose determinations.
DISCUSSION
In this large group of patients hospitalized in the general wards, hypoglycemia was associated with greater risk of in-hospital mortality, but this association only occurred in those who developed it spontaneously. In contrast, hypoglycemia that occurred with initiation of antidiabetic medications was not associated with higher in-hospital mortality. These findings suggest that hypoglycemia in hospitalized patients may be a marker of disease burden rather than a direct cause of death, results that should reassure clinicians who manage glucose levels in hospitalized patients in the general wards.
Additional evidence that hypoglycemia may not cause mortality is provided in our multivariate analyses. While the unadjusted analyses suggested a strong and significant association between spontaneous hypoglycemia and mortality, this association disappeared after adjusting for patient comorbidities. This suggests that spontaneous hypoglycemia may be a marker of disease burden, and might be used to identify a susceptible host with multiple comorbidities, but it might not be a direct cause of mortality. Our findings contrast with epidemiologic studies conducted mainly in type 1 diabetes subjects which have rendered hypoglycemia responsible for increased mortality24,25. A recent report of a young type 1 diabetic subject wearing a retrospective (non-real-time) continuous subcutaneous glucose monitoring system documented the occurrence of hypoglycemia at the time of the patient’s death26. Although drug-associated hypoglycemia is known to have deleterious effects on the central nervous system27, we did not find an association between drug-associated hypoglycemia and mortality in either univariate or multivariate analyses.
Our results support many observational studies which found that hypoglycemia was common during hospitalization and it was strongly associated with in-hospital mortality 10,15–17,23,28–31. Most studies, however, include critically ill patients. Two previous studies conducted among elderly patients (> 70 years of age) admitted to critical care and general ward units reported an association between hypoglycemia and in-hospital mortality16,28. Since elderly patients are at increased risk of developing comorbidities, the authors hypothesized that comorbidities, rather than hypoglycemia itself, would be responsible for the observed excess mortality. In these studies, as well as in others 29,30, it was not possible to determine if hypoglycemia was a direct cause of mortality. Our report extends these observations to a much younger population with less comorbidites as such found in the general hospital wards. One study excluded patients admitted to the ICU 23 and also showed an association between hypoglycemia and mortality. However, the authors could not distinguish between patients who developed hypoglycemia spontaneously vs. those who developed it as a consequence of glucose-lowering therapies23. Recently, Kosiborod et al. found increased mortality risk among patients with acute myocardial infarction developing hypoglycemia spontaneously, but not among those developing hypoglycemia as a consequence of glucose-lowering therapy31. Our results show a similar differential association but in non-critically ill patients. In addition, we provide further evidence that hypoglycemia behaves as a marker of disease rather than as a direct cause of death by showing that increase number of hypoglycemic episodes is associated with greater risk of hospital death only among patients developing hypoglycemia spontaneously. Moreover, when comorbidities are included in a multivariate model, the association between spontaneous hypoglycemia and mortality disappears.
Studies performed in outpatient populations are also pertinent when examining the role of hypoglycemia as a contributor to adverse outcomes versus a marker of disease burden. Two outpatient studies in individuals with type 2 diabetes showed no mortality benefit of tight glycemic control 18,19, while a third study, ACCORD, was prematurely stopped due to increased mortality in patients randomized to receive intensive glycemic therapy 20. A post-hoc analysis of ACCORD, however, could not attribute the excess mortality observed in the intensive therapy arm to severe hypoglycemia 21, suggesting that there are alternative explanations to the observed association between tight glycemic control and mortality independent of hypoglycemia. Some of the mechanisms contributing to increased mortality postulated by the ACCORD investigators include the magnitude or the speed of the reduction in glycated hemoglobin levels, or the development of adverse effects due to undetected interactions of various drug classes20. Recently, the authors from ADVANCE also studied the association between hypoglycemia and mortality and they concluded that while hypoglycemia may contribute to adverse outcomes, it is just as likely to be a marker of disease burden32. In our study, the fact that the association between spontaneous hypoglycemia and mortality disappeared after adjustment for comorbidities, and the fact that the number of hypoglycemic events was not associated with higher mortality risk in patients treated with antidiabetic agents (despite a much higher rate of hypoglycemic events in this group) suggest that hypoglycemia may not be a cause of mortality but rather a marker of poor prognosis in hospitalized patients.
Our study has several strengths. First, it was conducted in a highly diverse racial and ethnic patient base which should enhance the generalizability of our results. Second, we had a large data set that allowed us to perform sensitivity analyses using a lower glucose threshold (50mg/dl) and sub-analyses to examine the impact of different drug classes on hospital mortality. Finally, we designed a methodology that would allow us to distinguish mortality risks among hypoglycemic patients receiving and not receiving anti-diabetic drugs.
Despite its strengths, our study has several limitations. Because our analysis is retrospective and we were not able to document hypoglycemia at the time of death, we are not able to establish causality. However, prospective randomized trials are precluded for ethical reasons. In addition, we could not confirm a temporal relation between the administration of drugs and the occurrence of the hypoglycemic event. Despite the fact that drug-associated hypoglycemia was not associated with increased mortality, this study does not provide evidence that intensive therapy of hyperglycemia is beneficial in the general ward setting. An appropriately powered clinical trial of tight glycemic control in non-critically ill patients would be the adequate methodology to answer this question. Given the lack of randomization of our groups, we cannot exclude the possibility that antidiabetic agents might have been prescribed to an overall healthier population who tolerated hypoglycemia better and did not show evidence of increased mortality. Finally, the specific cause of hypoglycemia in patients who developed it spontaneously could not be established, and the specific cause of death could not be determined, so we considered all-cause mortality.
In conclusion, our study shows that while hypoglycemia is associated with increased in-hospital mortality among patients admitted to the general wards, this risk is confined to patients with spontaneous hypoglycemia. In contrast, drug-associated hypoglycemia is not associated with higher in-hospital mortality. While hypoglycemia remains an undesirable event and should be avoided when possible, these data suggest that hypoglycemia behaves as a marker of disease burden rather than as a direct cause of death.
Acknowledgements
Funding: This publication was made possible by the CTSA Grant UL1 RR025750 and KL2 RR025749 and TL1 RR025748 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessary represent the official view of the NCRR or NIH.
We thank Drs. Harry Shamoon, Norman Fleischer, and Martin I. Surks, Albert Einstein College of Medicine, for critically reading the manuscript and providing helpful suggestions.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement: LB, WNS, and JZ have not received any support from any organization for the submitted work; LB and WNS have no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; JZ serves on an advisory panel for Takeda Pharmaceutical North America, and on the speakers bureau for Amylin Pharmaceuticals, Eli Lilly, Merck, Novo Nordisk, and Sanofi-Aventis.
Contribution from authors: LB, WNS, and JZ had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. LB designed the study, researched the data, wrote, reviewed, and edited the manuscript. WNS contributed to data collection, researched the data, and contributed to writing, reviewing and editing the manuscript. JZ contributed to designing the study, writing, reviewing and editing the manuscript.
REFERENCES
- 1.Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003 Dec;78(12):1471–1478. doi: 10.4065/78.12.1471. [DOI] [PubMed] [Google Scholar]
- 2.Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999 May 25;99(20):2626–2632. doi: 10.1161/01.cir.99.20.2626. [DOI] [PubMed] [Google Scholar]
- 3.Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000 Mar 4;355(9206):773–778. doi: 10.1016/S0140-6736(99)08415-9. [DOI] [PubMed] [Google Scholar]
- 4.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002 Mar;87(3):978–982. doi: 10.1210/jcem.87.3.8341. [DOI] [PubMed] [Google Scholar]
- 5.Kosiborod M, Inzucchi SE, Spertus JA, et al. Elevated admission glucose and mortality in elderly patients hospitalized with heart failure. Circulation. 2009 Apr 14;119(14):1899–1907. doi: 10.1161/CIRCULATIONAHA.108.821843. [DOI] [PubMed] [Google Scholar]
- 6.van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001 Nov 8;345(19):1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- 7.Malmberg K, Ryden L, Efendic S, et al. Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year. J Am Coll Cardiol. 1995 Jul;26(1):57–65. doi: 10.1016/0735-1097(95)00126-k. [DOI] [PubMed] [Google Scholar]
- 8.Mehta SR, Yusuf S, Diaz R, et al. Effect of glucose-insulin-potassium infusion on mortality in patients with acute ST-segment elevation myocardial infarction: the CREATE-ECLA randomized controlled trial. JAMA. 2005 Jan 26;293(4):437–446. doi: 10.1001/jama.293.4.437. [DOI] [PubMed] [Google Scholar]
- 9.Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006 Feb 2;354(5):449–461. doi: 10.1056/NEJMoa052521. [DOI] [PubMed] [Google Scholar]
- 10.Finfer S, Chittock DR, Su SY, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009 Mar 26;360(13):1283–1297. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 11.Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008 Jan 10;358(2):125–139. doi: 10.1056/NEJMoa070716. [DOI] [PubMed] [Google Scholar]
- 12.Wiener RS, Wiener DC, Larson RJ. Benefits and risks of tight glucose control in critically ill adults: a meta-analysis. JAMA. 2008 Aug 27;300(8):933–944. doi: 10.1001/jama.300.8.933. [DOI] [PubMed] [Google Scholar]
- 13.Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006 Nov;55(11):3151–3159. doi: 10.2337/db06-0855. [DOI] [PubMed] [Google Scholar]
- 14.Svensson AM, McGuire DK, Abrahamsson P, Dellborg M. Association between hyper-and hypoglycaemia and 2 year all-cause mortality risk in diabetic patients with acute coronary events. Eur Heart J. 2005 Jul;26(13):1255–1261. doi: 10.1093/eurheartj/ehi230. [DOI] [PubMed] [Google Scholar]
- 15.Pinto DS, Skolnick AH, Kirtane AJ, et al. U-shaped relationship of blood glucose with adverse outcomes among patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2005 Jul 5;46(1):178–180. doi: 10.1016/j.jacc.2005.03.052. [DOI] [PubMed] [Google Scholar]
- 16.Kagansky N, Levy S, Rimon E, et al. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. 2003 Aug 11–25;163(15):1825–1829. doi: 10.1001/archinte.163.15.1825. [DOI] [PubMed] [Google Scholar]
- 17.Kosiborod M, Inzucchi SE, Krumholz HM, et al. Glucometrics in patients hospitalized with acute myocardial infarction: defining the optimal outcomes-based measure of risk. Circulation. 2008 Feb 26;117(8):1018–1027. doi: 10.1161/CIRCULATIONAHA.107.740498. [DOI] [PubMed] [Google Scholar]
- 18.Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med. 2009 Jan 8;360(2):129–139. doi: 10.1056/NEJMoa0808431. [DOI] [PubMed] [Google Scholar]
- 19.Patel A, MacMahon S, Chalmers J, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2560–2572. doi: 10.1056/NEJMoa0802987. [DOI] [PubMed] [Google Scholar]
- 20.Gerstein HC, Miller ME, Byington RP, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2545–2559. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonds DE, Miller ME, Bergenstal RM, et al. The association between symptomatic, severe hypoglycaemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ. 2010;340:b4909. doi: 10.1136/bmj.b4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005 May;28(5):1245–1249. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- 23.Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML. Hypoglycemia and clinical outcomes in patients with diabetes hospitalized in the general ward. Diabetes Care. 2009 Jul;32(7):1153–1157. doi: 10.2337/dc08-2127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skrivarhaug T, Bangstad HJ, Stene LC, Sandvik L, Hanssen KF, Joner G. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia. 2006 Feb;49(2):298–305. doi: 10.1007/s00125-005-0082-6. [DOI] [PubMed] [Google Scholar]
- 25.Feltbower RG, Bodansky HJ, Patterson CC, et al. Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes: results from the Yorkshire Register of diabetes in children and young adults. Diabetes Care. 2008 May;31(5):922–926. doi: 10.2337/dc07-2029. [DOI] [PubMed] [Google Scholar]
- 26.Tanenberg RJ, Newton CA, Drake AJ. Confirmation of hypoglycemia in the "dead-in-bed" syndrome, as captured by a retrospective continuous glucose monitoring system. Endocr Pract. 2010 Mar–Apr;16(2):244–248. doi: 10.4158/EP09260.CR. [DOI] [PubMed] [Google Scholar]
- 27.Cryer PE. Hypoglycemia, functional brain failure, and brain death. J Clin Invest. 2007 Apr;117(4):868–870. doi: 10.1172/JCI31669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shilo S, Berezovsky S, Friedlander Y, Sonnenblick M. Hypoglycemia in hospitalized nondiabetic older patients. J Am Geriatr Soc. 1998 Aug;46(8):978–982. doi: 10.1111/j.1532-5415.1998.tb02752.x. [DOI] [PubMed] [Google Scholar]
- 29.Fischer KF, Lees JA, Newman JH. Hypoglycemia in hospitalized patients. Causes and outcomes. N Engl J Med. 1986 Nov 13;315(20):1245–1250. doi: 10.1056/NEJM198611133152002. [DOI] [PubMed] [Google Scholar]
- 30.Stagnaro-Green A, Barton MK, Linekin PL, Corkery E, deBeer K, Roman SH. Mortality in hospitalized patients with hypoglycemia and severe hyperglycemia. Mt Sinai J Med. 1995 Nov;62(6):422–426. [PubMed] [Google Scholar]
- 31.Kosiborod M, Inzucchi SE, Goyal A, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009 Apr 15;301(15):1556–1564. doi: 10.1001/jama.2009.496. [DOI] [PubMed] [Google Scholar]
- 32.Zoungas S, Patel A, Chalmers J, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010 Oct 7;363(15):1410–1418. doi: 10.1056/NEJMoa1003795. [DOI] [PubMed] [Google Scholar]