Abstract
Cervicogenic headache (CGH), as the diagnosis suggests, refers to a headache of cervical origin. Historically, these types of headaches were difficult to diagnose and treat because their etiology and pathophysiology was not well-understood. Even today, management of a CGH remains challenging for sports rehabilitation specialists. The purpose of this clinical suggestion is to review the literature on CGH and develop an evidence-led approach to assessment and clinical management of CGH.
Keywords: Headache, neck pain, muscle imbalance
BACKGROUND AND DIAGNOSIS
Cervicogenic headaches (CGHs) pose a challenge for many sports physical therapists because the head pain results from somewhere other than the head: the cervical spine. Interestingly, CGHs are one of the most common types of headache in weight-lifting athletes.1 Patients who have sustained whiplash or concussion injuries with resulting neck pain sometimes develop CGH.2,3 In fact, headaches developing 3 months or more after concussion are generally not caused by brain or head injury,4 suggesting a possible cervical spine etiology.
The International Headache Society5 published their International Classification of Headache Disorders 2nd edition, identifying 14 different types and sub classifications of headaches. There are 2 basic categories of headaches, primary and secondary. Primary headaches include those of vascular origin (cluster and migraine headaches) as well as those of muscular origin (tension-type headaches). Secondary headaches result from another source including inflammation or head and neck injuries. Norwegian physician Dr. Ottar Sjaastad coined the term, “cervicogenic headache” in 19836 by recognizing a sub-group of headache patients with concomitant head and neck pain; therefore, CGHs are considered “secondary headaches.”
The diagnostic criteria for CGH include headache associated with neck pain and stiffness. Cervicogenic headaches are unilateral, starting from one side of the posterior head and neck, migrating to the front, and sometimes are associated with ipsilateral arm discomfort.7 Sjaastad et al8 identified another type of CGH with bilateral head and neck pain, aggravated by neck positions and specific occupations such as hair-dressing, carpentry, and truck/tractor driving. The neck pain precedes or co-exists with the headache, and is aggravated by specific neck movements or sustained postures. Vincent9 described several factors to differentiate CGHs, including:
Unilateral pain with a facet ‘lock’ irradiating from the back of the head
Evidence of cervical dysfunction presenting during manual examination
May occur with trigger point palpation in the head or neck
Aggravated by sustained neck positions
Normal imaging
Because the diagnosis of CGH is relatively new, its particular etiology remains unclear. Sjasstad and his colleagues10 suggested that CGH is a “final common pathway” for pain generating disorders of the neck. Bogduk11 has proposed that the pathophysiology of CGH results from a convergence of sensory input from the upper cervical spine into the trigeminal spinal nucleus, including input from:
Upper cervical facets
Upper cervical muscles
C2-3 intervertebral disc
Vertebral and internal carotid arteries
Dura mater of the upper spinal cord
Posterior cranial fossa
The trigeminal pathway theory is somewhat supported by the fact that injection of the greater and lesser occipital nerves with steroids decrease headaches by blocking the trigeminal relay.12 Furthermore, Chua and colleagues13 recently reported impairments of sensory testing of the head in CGH patients compared to patients with neck dysfunction without headache. They concluded that the pathophysiology of CGH includes central sensitization of pain, likely from the trigeminal spinal nucleus.
Approximately 47% of the global population suffers from a headache,14,15 and 15-20 percent of those headaches are cervicogenic.16,17 Recently, CGHs were estimated to affect 2.2% of the population.7 Epidemiological researchers suggest a higher prevalence of headache in adults with neck pain.18 Females seem more predisposed to CGHs affecting 4 times as many women as men. Since CGHs commonly affect women, it is important to consider menstruation and hormonal shifts as a contributor to headaches. Menstrual-type headaches often occur 2 days before menstruation and last until the last day of the cycle. These headaches are usually migraine-type, but may be cervicogenic as well.19,20
Migraine or tension-type headaches can also present with neck pain, further complicating differential diagnosis; in fact, some migraine patients experience more neck pain than nausea.21 Up to 44% of CGH patients may have temporomandibular joint (TMJ) issues as well.22 Sports physical therapists should perform a comprehensive assessment of the neuromusculoskeletal system in patients with chronic headaches.
As with any differential diagnosis, it is important to first identify any “red flags” associated with headaches that may be a symptom of a serious condition. Patients with vertebral artery dissection present with concomitant headache and neck pain,23 so it is critical to rule out that condition in patients with headache and neck pain first. Red flag symptoms requiring further medical evaluation include:
Headaches that are getting worse over time
Sudden onset of severe headache
Headaches associated with high fever, stiff neck, or rash
Onset of headache after head injury
Problems with vision or profound dizziness
Radiological examination is of limited value in diagnosing CGHs. Coskun and colleagues24 found that nearly half of CGH patients as well as asymptomatic subjects had bulging cervical discs. The most important clinical finding to diagnose CGH is impairment of C1-C2 (atlanto-axial) motion.10 While typically associated with upper cervical dysfunction, some have suggested that CGHs can occur in patients with lower cervical dysfunction, particularly after trauma.25,26
Both history of trauma and patient age may be factors in differentiating upper or lower segmental CGHs. Preadolescent (10-13 year old) children with neck pain and headache have dysfunction of the lower cervical spine.27 Cervical osteoarthritis, common in many older patients may be associated with headache and cervical muscle dysfunction.28,29 In addition, physical impairments such as cervical range of motion and muscular strength can vary between traumatic and atraumatic CGHs.30 Clinicians should remember that diagnosis of CGH should be made by carefully examining the etiology of the headaches, not just the symptoms. Above all, successful treatment of CGH begins with a good clinical examination and accurate diagnosis.
ASSESSMENT
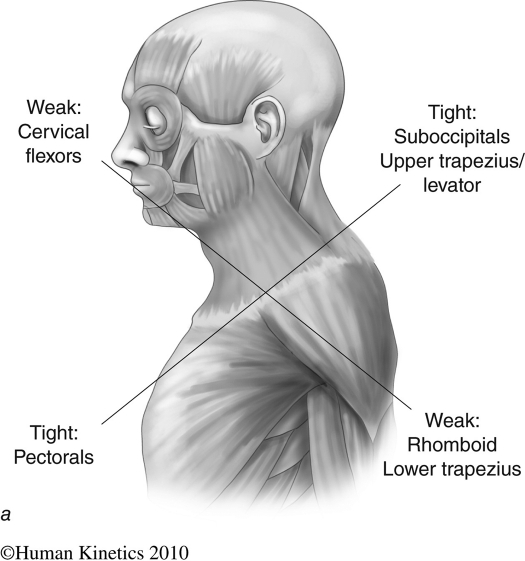
Because CGHs are a secondary type of headache, it is important to determine the primary causes that exist by performing a thorough musculoskeletal assessment, particularly of the cervical spine. Dr. Vladimir Janda noted specific patterns of muscle imbalance in patients with cervical dysfunction, including those with cervicogenic headaches.31 These patterns of muscle tightness and weakness, known as “Upper Crossed Syndrome” (Figure 1) were further described in several published studies on CGH.3,32–37 In addition, several published case studies38–40 describe CGH patients with presentations consistent with the Upper Crossed Syndrome.
Figure 1.
Janda's Upper Crossed Syndrome. (Permission of Human Kinetics)
Postural Assessment
Forward head posture is thought to increase stress on the upper cervical segments. Watson and Trott36 first noted that forward head posture was more common in CGH patients than other patients, which was also associated with weakness and decreased endurance of the deep neck flexors. More recently, however, Zito and colleagues37 found no significant differences in the prevalence of forward head posture in CGH or migraine patients compared to control subjects.
Active Range of Motion
Clinicians often measure active cervical ROM in patients with head and neck pain; however, author's results conflict on its validity in CGH. Some authors have reported significant decreases in active ROM in those with CGH,30,34,37,41 while others have found no significant differences in AROM when compared to asymptomatic subjects.3,42 These findings also suggest that subclassifying CGHs into traumatic versus atraumatic origin may be of value, since headache and neck ROM are inversely related in patients who have sustained a whiplash injury.43
Muscle Length
Consistent with Janda's Upper Crossed Syndrome, patients with CGH often present with tightness of the sternocleidomastoid, upper trapezius, levator, scalenes, suboccipitals, pectoralis minor, and pectoralis major.3,35,37 These muscle length tests are described elsewhere.44,45 Treleaven and colleagues3 used a tightness scale to rate muscle length using normal, slight, moderate, and severe tightness.
Muscle Strength and Activation
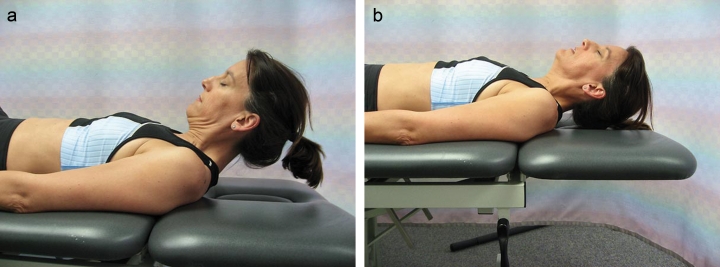
Janda also noted that patients with cervical dysfunction often have weakness of their deep neck flexors. Several researchers have confirmed decreased strength and endurance of the deep neck flexors in CGH patients.34–37,46 Janda recommended the active neck flexion movement pattern test to identify patients with weakness of the deep neck flexors.44 With the patient supine and knees bent, he or she is asked to lift the head and look at their toes (Figure 2). Normal movement produces a smooth reversal of the normal cervical lordosis, keeping the chin tucked. Weakness of the deep neck flexors is compensated by tightness of the SCM, producing an early protraction of the chin directly upward at the beginning of the motion.
Figure 2a and 2b.
Janda's Cervical Flexion text (a. Normal, b. Abnormal movement patterns)
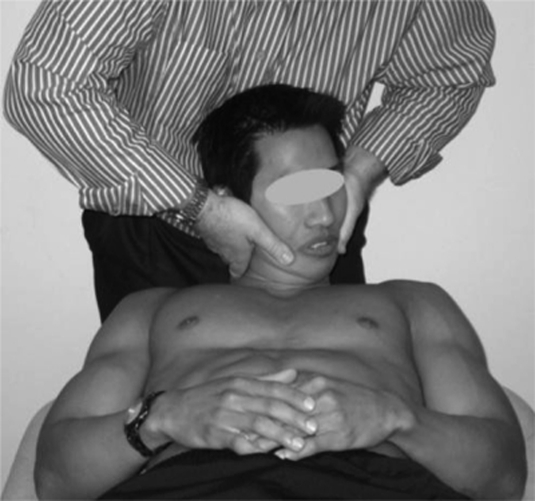
Jull and colleagues35 used the craniocervical flexion (CCF) test to demonstrate significant deep neck flexor weakness in CGH patients. The CCF test provides a reliable measure of deep neck flexor performance.47 During the CCF test (Figure 3), an inflatable cuff with a pressure sensor is inflated to 20 mm Hg and placed under the patient's neck while lying in supine. The patient performs gentle nodding motions of craniocervical flexion while maintaining the target pressure. The pressure is increased by 2 mm Hg over 5 incremental levels with progressive increases in craniocervical flexion range of motion until the patient is able to perform craniocervical flexion while maintaining 30 mm Hg.
Figure 3.
The CCF Test. The patient performs craniocervical flexion while maintaining a specific pressure, beginning at 20 mm Hg and ending at 30 mm Hg.
Other researchers have used electromyography (EMG) to examine neuromuscular function in CGH patients and have found that they exhibit abnormally high activation of the SCM and upper trapezius during muscular strength testing,32,33,37,48 as well as decreased deep neck flexor activation.33
Manual Assessment
Palpable joint dysfunction of the upper cervical spine discriminates between CGH and other headaches as well as control patients.34 Manual assessment of the upper cervical segmental mobility and pain has good reliability, with positive findings (pain produced with passive mobilization) in 63% of CGH patients49 and a sensitivity of 80%.37 All manual assessments of cervical patients should begin with a vertebrobasilar artery (VBA) test to rule out arterial insufficiency. Patients who sustain a VBA stroke often have preliminary symptoms of headache and neck pain,23 but the risk of VBA stroke after spinal manipulation remains minimal, roughly at the same level of risk as visiting a primary care physician.50
Cervical Flexion-Rotation Test
During the Cervical Flexion Rotation Test (CFR), the patient is supine and the examiner flexes the cervical spine fully in order to block rotational movement below the atlanto-axial articulation. The examiner then passively rotates the head left and right, determining range of motion (ROM) and end-feel. A firm end-feel with limited ROM presumes limited rotation of the atlas on the axis.
Using the CFR test, patients with CGH average 25-28° of A-A rotation to the side of the headache as compared to an average rotation of 44° in asymptomatic patients.42,51 Patients with migraine and other types of headaches may also be limited in CFR motion, averaging 42° and 35° respectively in either direction.51 Some authors have suggested that the degree of ROM restriction is not related to the severity of CGH symptoms,52 while others have found as little as 6° restriction can be related to headache intensity.42,53 The CFR has been shown to have an overall diagnostic accuracy of 85-91%.51,52 It is important to remember that limited rotation to one side may be due to tightness of the contralateral suboccipital muscles, and not necessarily impaired C1-2 rotation,54 thus a careful examination of soft tissue restriction is also important.
Breathing Pattern
Diaphragmatic breathing allows the lungs to fill on inspiration by increasing chest volume. In patients with diaphragm dysfunction, the accessory respiratory muscles (scalenes and SCM) lift the rib cage to facilitate lung filling during inspiration. These secondary muscles are often tight and hyperactive in patients with chronic neck pain due to deep neck flexor weakness.32,33,48 In faulty respiration patterns, these tight muscles are readily activated and continue to facilitate the patterns of muscle imbalance with each breath.
Soft Tissue Assessment
Cervicogenic headache patients have a high probability of having myofascial trigger point pain,54 particularly from overactivity of the SCM, upper trapezius, and temporalis.32 Myofascial trigger points of the SCM have a similar referred pain pattern to that seen in CGH (posterior to frontal). In fact, Jaeger55 found that 12 out of 12 CGH patients had at least 3 myofascial trigger points on their symptomatic side which reproduced their headaches over 50% of the time.
INTERVENTION
Medical management usually begins with pharmacologic intervention; however, CGH patients frequently do not respond to medications.57 More invasive procedures have been suggested in the literature such as occipital nerve blocks,12,41 anesthetic and steroid blockades,56,58,59 and treatment with pulsed radiofrequency energy.60 Because of the risks associated with these procedures, and the lack of well-controlled outcomes studies, more conservative interventions are typically prescribed.
As stated previously, an accurate diagnosis is the key to successful treatment. A comprehensive musculoskeletal examination will identify specific impairments upon which the sports physical therapist can focus in order to relieve CGH symptoms. Impairments associated with concomitant conditions such as TMJ disorder should be addressed which will improve outcomes.22 Several factors have been associated with better outcomes in CGH patients: older patients, provocation or relief of headache with movement, and gainful employment.61 A multi-modal approach including modalities, manual therapy, and therapeutic exercise is recommended to address individual impairments in CGH patients.62
Modalities
Modalities are frequently used by sports physical therapists to help reduce pain and facilitate healing. Few studies have investigated the effectiveness of modalities in CGH patients. There is some support for TENS16,63,64 and cryotherapy41 in combination with other therapies.
Low-level laser therapy (LLLT) is becoming an increasingly popular modality for treatment of a variety of musculoskeletal conditions. Unfortunately, there are no known clinical studies on the use of LLLT in CGH patients. In a recent systematic review, Chow et al65 concluded that LLLT reduces pain immediately after treatment in acute mechanical neck pain and up to 22 weeks after treatment in patients with chronic neck pain, while Leaver et al. suggested LLLT is more effective in the intermediate and long-term than short term.66 Furthermore, laser acupuncture was shown more effective than placebo in treating chronic tension-type headaches.67
Manual Therapy
Because CGH is related to cervical joint dysfunction, most studies on CGH treatment have focused on joint mobilization and manipulation. Several studies of varied research designs have shown that spinal manipulative therapy (SMT) is effective for CGH,70–75 particularly those focused on treatment of the upper cervical segments. Systematic reviews of randomized control trials using manual therapy in CGH patients suggest better outcomes compared to no treatment,76 although there is a need for more high quality clinical studies.77 Both mobilization and manipulation are effective for treatment of patients with cervical pain, although manipulation appears superior to mobilization in the short term.78 In addition, patients with neck pain with or without headache have more short-term relief when manual therapy is combined with exercise as compared to exercise alone.79
Muscle Stretching
Patients with CGHs often have tightness of the SCM, upper trapezius, levator, scalenes, suboccipitals, pectoralis minor, and pectoralis major.3,35,37 The post-isometric relaxation (PIR) technique is useful in helping reduce tightness and trigger point pain.80 PIR is performed by first passively lengthening the muscle, then having the patient lightly contract (10-20% of maximum) against resistance for 5 seconds passively before exhaling and relaxing the muscle and repeated. The clinician then takes up the slack within the muscle and repeats the technique 3 to 5 times.
Gebauer's Spray and Stretch® can also be used to address muscle tightness and trigger points located both in the cervical and facial musculature.Trigger points often refer pain in the cranial region, creating headache-like symptoms; muscles whose trigger points may present headache like symptoms include the suboccipitals, SCM, and temporalis.54 In addition, scalene trigger points can refer pain down the arm as is sometimes seen in CGH patients. Simons and colleagues offer an excellent description of the spray and stretch technique in their textbook.54
Instrument-Assisted Soft Tissue Mobilization (IASTM)
The fascia is an important and often overlooked tissue that often contributes to chronic musculoskeletal pain. Astute therapists realize that fascial contributors to pain must be addressed. Several different fascial layers exist in the cervical spine.81 Fascial connections exist between the suboccipital muscles and upper cervical dura, which attaches to the cranial fossa and C2 vertebra.82 Adhesions in these fascial connections may restrict normal movement of muscle between fascial planes. While no studies have examined the efficacy of IASTM in headache or neck patients, clinicians may use techniques such as Graston® Technique or ASTYM® to address soft-tissue restrictions and pain in the upper cervical region, particularly in the suboccipitals, SCM, upper trapezius, and levator. Manual myofascial stretching is a hallmark of soft tissue intervention in patients with cervical pain and dysfunction. While instruments can facilitate soft tissue assessment and mobilization, hands-on myofascial techniques can also be helpful.
Therapeutic Exercise
Unfortunately, there are few studies focusing on the effectiveness of therapeutic exercise in patients with CGH.72,83 With this lack of specific evidence, and until more is available, clinicians may make clinical decisions on exercise prescription based on research conducted in patients with either chronic neck pain or headaches. As stated previously, clinicians should address individual impairments in CGH patients which may include poor posture, motor control, muscle length, and muscle strength and endurance impairments.
Therapeutic exercise intervention should start by addressing and teaching postural awareness. Patients with cervical pain often exhibit forward head posture and rounded shoulders associated with muscle imbalance. Reinforcing good posture through regular cuing can help reinforce the stretching and strengthening exercises to restore muscle balance. A good ‘proprioceptive posture’ begins from the core, ensuring the patient knows how to activate the transverse abdominus and brace the entire core. In addition, patients should be instructed in proper diaphragmatic breathing to reduce activation of accessory respiratory muscles as suggested in Travel's textbook.54
Cervicogenic headaches are thought to be a dysfunction of the sensorimotor system, rather than a true structural problem.31 Sensorimotor dysfunction manifests itself in the neuromusculoskeletal system in motor control and movement impairments. Jull and colleagues used a specific exercise, the ‘craniocervical flexion’ (CCF) exercise for activating the deep neck flexors in patients with chronic cervical pain.72,84 In their randomized controlled trial of 200 patients with CGH, Jull and colleagues found that 6 weeks of the CCF exercise was as effective as spinal manipulation at reducing headache frequency and intensity, as well as cervical pain up to 1 year.
During the CCF exercise, an inflatable pressure cuff is placed behind the neck as the patient lies supine as described previously for the CCF Test (Recall Figure 3). The cuff is inflated to 20 mm Hg and the patient is instructed to very slowly flex the upper cervical spine with a gentle nodding motion and hold steady for 10 seconds without activating the SCM. The exercise is progressed by increasing the cuff inflation by 10 mm Hg toward a goal of 40 mm Hg. Compared to normal cervical flexion, the CCF has lower activation of the SCM,85–88 which may be desirable in patients with muscle imbalance. While this biofeedback using the pressure gauge may be effective, similar exercises can be performed at home using a towel roll. Begin in supine with the exercise and progress to combining with bilateral arm raise. Further progress the patient to a sitting position with their back against a wall while performing the same exercise. Finally, other unsupported postures must be utilized to allow patients to transition to normal, functional movement positions.
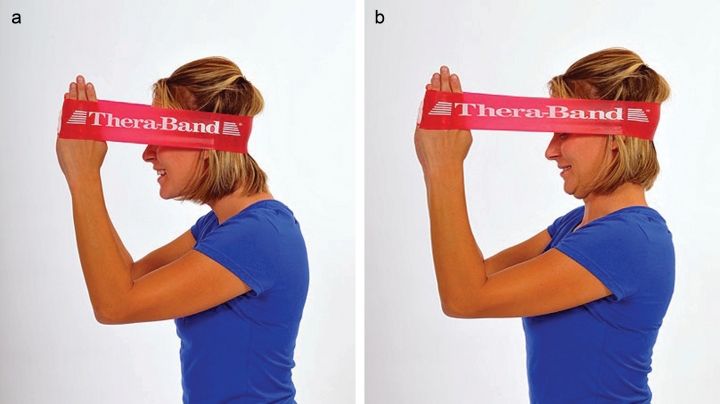
Jull and colleagues84 reported that their CCF exercise was more effective than a strengthening exercise involving resisted neck flexion in patients with chronic neck pain; however, Ask et al89 found no significant difference between the CCF exercise and a ‘dynamic isometric’ neck strengthening exercise using elastic bands in whiplash patients. Their strengthening program was based on work by Dr. Jari Ylinen and his colleagues in Finland on women with chronic neck pain. The exercise program has been shown to be effective in reducing chronic neck pain90 as well as cervicogenic headaches.83 Ylinen's program includes a high-intensity, 4-direction dynamic isometric exercise of the cervical spine and strengthening and stretching exercises for the upper quarter. The patient stabilizes the neck and performs a ‘hip-hinge’ over 20-30 degrees against elastic band resistance (Figure 5). The exercise is performed in flexion, extension, and sidebending to both sides.
Figure 5.
Dynamic Cervical Extension Exercise. The patient performs a ‘hip hinge’, stabilizing the cervical spine against the resistance in 4 directions (Used with permission of The Hygenic corporation).
Figure 4.
Cervical Flexion-Rotation Test. The cervical spine is fully flexed and rotated to right and left while noting range of motion and pain. (From: Hall, Toby; Briffa, Kathy; Hopper, Diana, ‘Clinical Evaluation of Cervicogenic Headache: A Clinical Perspective’, Journal of Manual & Manipulative Therapy, 16(2), 2008, pp. 73-80. Used with Permission of Maney Publishing)
Van Ettekoven and Lucas92 completed a 6-week randomized controlled trial on patients with tension-type headaches who were assigned to either a passive (massage and manual therapy) or active (massage, manual therapy and exercise) group. The exercise group performed craniocervical flexion exercise (Figure 6) against an elastic resistance band for 6 weeks. The exercise group had significantly reduced frequency, intensity and duration up to 6 months after the program. Although this study was not performed on patients with CGH, the positive results lend support for utilizing this exercise in CGH patients.
Figure a-b:
Craniocervical flexion against elastic band loop. Begin with cervical spine in protraction (a). Maintain hand position while retracting against the tension in the band (b). (Used with permission of The Hygenic Corporation).
Exercises to improve upper quarter strength, particularly of the axio-scapulo-humeral musculature, are important.93 Most recently, Andersen and colleagues94 demonstrated that 2 minutes per day, 5 days per week of a standing lateral raise exercise with elastic tubing significantly reduced neck-shoulder pain and headaches in office workers. Several other clinical intervention studies on chronic neck pain and CGH83,94–96 have utilized a variety of upper quarter strengthening exercises including:
Shoulder abduction
Shoulder retraction
Lat pull-down
Push-up
Chest press
Shrug
Arm curl
Bent-over row
Chest flies
Adding upper quarter exercises for patients with cervical dysfunction is important in order to integrate ‘global’ muscles that have connections to the cervical spine through anatomical chains; most notably those connecting the axial and appendicular skeletons.
Finally, because CGHs are thought to be a dysfunction of the sensorimotor system, rather than a true structural problem, sensorimotor training should be included in the rehabilitation program.97 Sensorimotor exercises include progressive exercise on unstable surfaces to promote reflexive stabilization and postural stability. Unstable surfaces such as exercise balls or foam pads can be used to add challenge to the cervical spine as well as the whole-body for stabilization exercises (Figure 7). These final stages of the rehabilitation program for CGH patients can be progressed toward functional activities to return the patient or athlete to full participation.
Figure 7.
Cervical stabilization using a mini-ball with resisted scapular retraction (Used with permission of The Hygenic Corporation).
In summary, CGHs are caused by neck dysfunction, typically of the upper cervical spine, although the specific etiology remains unclear. Cervicogenic headaches are associated with musculoskeletal dysfunction and muscle imbalance with characteristic patterns of muscle weakness and tightness. A thorough history and clinical examination will lead to an accurate diagnosis. As with other musculoskeletal dysfunctions, a multi-modal physical therapy intervention is recommended to address individual impairments including modalities, manual therapy, and therapeutic exercise. It's important for sports physical therapists to make an accurate diagnosis and provide an appropriate intervention to return the athlete with CGHs to sports as soon as possible.
REFERENCES
- 1. Rifat S.F., Moeller J.L., Diagnosis and management of headache in the weight-lifting athlete. Curr Sports Med Rep, 2003. 2(5): p. 272–5 [DOI] [PubMed] [Google Scholar]
- 2. Drottning M., Cervicogenic headache after whiplash injury. Curr Pain Headache Rep, 2003. 7(5): p. 384–6 [DOI] [PubMed] [Google Scholar]
- 3. Treleaven J., Jull G., Atkinson L., Cervical musculoskeletal dysfunction in post-concussional headache. Cephalalgia, 1994. 14(4): p. 273–9; discussion 257. [DOI] [PubMed] [Google Scholar]
- 4. Stovner L.J., et al. , Headache after concussion. Eur J Neurol, 2009. 16(1): p. 112–20 [DOI] [PubMed] [Google Scholar]
- 5. The International Classification of Headache Disorders: 2nd edition. Cephalalgia, 2004. 24 Suppl 1: p. 9–160 [DOI] [PubMed] [Google Scholar]
- 6. Sjaastad O., et al. , “Cervicogenic” headache. An hypothesis. Cephalalgia, 1983. 3(4): p. 249–56 [DOI] [PubMed] [Google Scholar]
- 7. Antonaci F., Sjaastad O., Cervicogenic headache: a real headache. Curr Neurol Neurosci Rep, 2011. 11(2): p. 149–55 [DOI] [PubMed] [Google Scholar]
- 8. Sjaastad O., Wang H., Bakketeig L.S., Neck pain and associated head pain: persistent neck complaint with subsequent, transient, posterior headache. Acta Neurol Scand, 2006. 114(6): p. 392–9 [DOI] [PubMed] [Google Scholar]
- 9. Vincent M.B., Cervicogenic headache: a review comparison with migraine, tension-type headache, and whiplash. Curr Pain Headache Rep, 2010. 14(3): p. 238–43 [DOI] [PubMed] [Google Scholar]
- 10. Sjaastad O., Fredriksen T.A., Pfaffenrath V., Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache, 1998. 38(6): p. 442–5 [DOI] [PubMed] [Google Scholar]
- 11. Bogduk N., Cervicogenic headache: anatomic basis and pathophysiologic mechanisms. Curr Pain Headache Rep, 2001. 5(4): p. 382–6 [DOI] [PubMed] [Google Scholar]
- 12. Anthony M., Cervicogenic headache: prevalence and response to local steroid therapy. Clin Exp Rheumatol, 2000. 18(2 Suppl 19): p. S59–64 [PubMed] [Google Scholar]
- 13. Chua N.H., et al. , Differences in sensory processing between chronic cervical zygapophysial joint pain patients with and without cervicogenic headache. Cephalalgia, 2011 [DOI] [PubMed] [Google Scholar]
- 14. Stovner L., et al. , The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia, 2007. 27(3): p. 193–210 [DOI] [PubMed] [Google Scholar]
- 15. Jensen R., Stovner L.J., Epidemiology and comorbidity of headache. Lancet Neurol, 2008. 7(4): p. 354–61 [DOI] [PubMed] [Google Scholar]
- 16. Haldeman S., Dagenais S., Cervicogenic headaches: a critical review. Spine J, 2001. 1(1): p. 31–46 [DOI] [PubMed] [Google Scholar]
- 17. Nilsson N., The prevalence of cervicogenic headache in a random population sample of 20–59 year olds. Spine (Phila Pa 1976), 1995. 20(17): p. 1884–8 [DOI] [PubMed] [Google Scholar]
- 18. Hagen K., et al. , The co-occurrence of headache and musculoskeletal symptoms amongst 51 050 adults in Norway. Eur J Neurol, 2002. 9(5): p. 527–33 [DOI] [PubMed] [Google Scholar]
- 19. Lieba-Samal D., Wober C., Sex Hormones and Primary Headaches Other than Migraine. Curr Pain Headache Rep, 2011 [DOI] [PubMed] [Google Scholar]
- 20. Miziara L., et al. , [Menstrual headache: semiological study in 100 cases]. Arq Neuropsiquiatr, 2003. 61(3A): p. 596–600 [DOI] [PubMed] [Google Scholar]
- 21. Calhoun A.H., et al. , The prevalence of neck pain in migraine. Headache, 2010. 50(8): p. 1273–7 [DOI] [PubMed] [Google Scholar]
- 22. von Piekartz H., Ludtke K., Effect of treatment of temporomandibular disorders (TMD) in patients with cervicogenic headache: a single-blind, randomized controlled study. Cranio, 2011. 29(1): p. 43–56 [DOI] [PubMed] [Google Scholar]
- 23. Lee V.H., et al. , Incidence and outcome of cervical artery dissection: a population-based study. Neurology, 2006. 67(10): p. 1809–12 [DOI] [PubMed] [Google Scholar]
- 24. Coskun O., et al. , Magnetic resonance imaging of patients with cervicogenic headache. Cephalalgia, 2003. 23(8): p. 842–5 [DOI] [PubMed] [Google Scholar]
- 25. Hong J.P., et al. , Clinical assessment of patients with cervicogenic headache: a preliminary study. Chang Gung Med J, 2010. 33(1): p. 58–66 [PubMed] [Google Scholar]
- 26. Diener H.C., et al. , Lower cervical disc prolapse may cause cervicogenic headache: prospective study in patients undergoing surgery. Cephalalgia, 2007. 27(9): p. 1050–4 [DOI] [PubMed] [Google Scholar]
- 27. Weber Hellstenius S.A., Recurrent neck pain and headaches in preadolescents associated with mechanical dysfunction of the cervical spine: a cross-sectional observational study with 131 students. J Manipulative Physiol Ther, 2009. 32(8): p. 625–34 [DOI] [PubMed] [Google Scholar]
- 28. Gogia P.P., Sabbahi M.A., Electromyographic analysis of neck muscle fatigue in patients with osteoarthritis of the cervical spine. Spine (Phila Pa 1976), 1994. 19(5): p. 502–6 [DOI] [PubMed] [Google Scholar]
- 29. Uthaikhup S., Sterling M., Jull G., Cervical musculoskeletal impairment is common in elders with headache. Man Ther, 2009. 14(6): p. 636–41 [DOI] [PubMed] [Google Scholar]
- 30. Dumas J.P., et al. , Physical impairments in cervicogenic headache: traumatic vs. nontraumatic onset. Cephalalgia, 2001. 21(9): p. 884–93 [DOI] [PubMed] [Google Scholar]
- 31. Janda V., Muscles and motor control in cervicogenic disorders, in Physical therapy of the cervical and thoracic spine, Grant R., Editor 1994, Churchill Livingstone: Edinburgh: p. 195–215 [Google Scholar]
- 32. Bansevicius D., Sjaastad O., Cervicogenic headache: the influence of mental load on pain level and EMG of shoulder-neck and facial muscles. Headache, 1996. 36(6): p. 372–8 [DOI] [PubMed] [Google Scholar]
- 33. Falla D.L., Jull G.A., Hodges P.W., Patients with neck pain demonstrate reduced electromyographic activity of the deep cervical flexor muscles during performance of the craniocervical flexion test. Spine (Phila Pa 1976), 2004. 29(19): p. 2108–14 [DOI] [PubMed] [Google Scholar]
- 34. Jull G., et al. , Cervical musculoskeletal impairment in frequent intermittent headache. Part 1: Subjects with single headaches. Cephalalgia, 2007. 27(7): p. 793–802 [DOI] [PubMed] [Google Scholar]
- 35. Jull G., et al. , Further clinical clarification of the muscle dysfunction in cervical headache. Cephalalgia, 1999. 19(3): p. 179–85 [DOI] [PubMed] [Google Scholar]
- 36. Watson D.H., Trott P.H., Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia, 1993. 13(4): p. 272–84; discussion 232. [DOI] [PubMed] [Google Scholar]
- 37. Zito G., Jull G., Story I., Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther, 2006. 11(2): p. 118–29 [DOI] [PubMed] [Google Scholar]
- 38. Moore M.K., Upper crossed syndrome and its relationship to cervicogenic headache. J Manipulative Physiol Ther, 2004. 27(6): p. 414–20 [DOI] [PubMed] [Google Scholar]
- 39. van Duijn J., van Duijn A.J., Nitsch W., Orthopaedic manual physical therapy including thrust manipulation and exercise in the management of a patient with cervicogenic headache: a case report. J Man Manip Ther, 2007. 15(1): p. 10–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. McDonnell M.K., Sahrmann S.A., Van Dillen L., A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: a case report. J Orthop Sports Phys Ther, 2005. 35(1): p. 3–15 [DOI] [PubMed] [Google Scholar]
- 41. Knackstedt H., et al. , Cervicogenic headache in the general population: the Akershus study of chronic headache. Cephalalgia, 2010. 30(12): p. 1468–76 [DOI] [PubMed] [Google Scholar]
- 42. Hall T., Robinson K., The flexion-rotation test and active cervical mobility—a comparative measurement study in cervicogenic headache. Man Ther, 2004. 9(4): p. 197–202 [DOI] [PubMed] [Google Scholar]
- 43. Kasch H., et al. , Headache, neck pain, and neck mobility after acute whiplash injury: a prospective study. Spine (Phila Pa 1976), 2001. 26(11): p. 1246–51 [DOI] [PubMed] [Google Scholar]
- 44. Page P., Frank C.C., Lardner R., Assessment and treatment of muscle imbalance: The Janda Approach 2010, Champaign, IL: Human Kinetics [Google Scholar]
- 45. Kendall F.P., et al. , Muscles. Testing and function with posture and pain. 5th ed2005, Baltimore, MD: Lippincott Williams & Wilkins [Google Scholar]
- 46. Jull G., Management of cervical headache. Man Ther, 1997. 2(4): p. 182–190 [DOI] [PubMed] [Google Scholar]
- 47. Falla D., et al. , An electromyographic analysis of the deep cervical flexor muscles in performance of craniocervical flexion. Phys Ther, 2003. 83(10): p. 899–906 [PubMed] [Google Scholar]
- 48. Barton P.M., Hayes K.C., Neck flexor muscle strength, efficiency, and relaxation times in normal subjects and subjects with unilateral neck pain and headache. Arch Phys Med Rehabil, 1996. 77(7): p. 680–7 [DOI] [PubMed] [Google Scholar]
- 49. Hall T., et al. , Reliability of manual examination and frequency of symptomatic cervical motion segment dysfunction in cervicogenic headache. Man Ther, 2010. 15(6): p. 542–6 [DOI] [PubMed] [Google Scholar]
- 50. Cassidy J.D., et al. , Risk of vertebrobasilar stroke and chiropractic care: results of a population-based case-control and case-crossover study. Spine (Phila Pa 1976), 2008. 33(4 Suppl): p. S176–83 [DOI] [PubMed] [Google Scholar]
- 51. Hall T.M., et al. , Comparative analysis and diagnostic accuracy of the cervical flexion-rotation test. J Headache Pain, 2010. 11(5): p. 391–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ogince M., et al. , The diagnostic validity of the cervical flexion-rotation test in C1/2-related cervicogenic headache. Man Ther, 2007. 12(3): p. 256–62 [DOI] [PubMed] [Google Scholar]
- 53. Hall T.M., et al. , The relationship between cervicogenic headache and impairment determined by the flexion-rotation test. J Manipulative Physiol Ther, 2010. 33(9): p. 666–71 [DOI] [PubMed] [Google Scholar]
- 54. Simons D.G., Travell J.G., Simons L.S., Travell & Simons' myofascial pain and dysfunction: the trigger point manual. Volume 1. The upper body. 2nd ed1999, Philadelphia: Lippincott Williams & Wilkins [Google Scholar]
- 55. Jaeger B., Are “cervicogenic” headaches due to myofascial pain and cervical spine dysfunction? Cephalalgia, 1989. 9(3): p. 157–64 [DOI] [PubMed] [Google Scholar]
- 56. Bovim G., Berg R., Dale L.G., Cervicogenic headache: anesthetic blockades of cervical nerves (C2-C5) and facet joint (C2/C3). Pain, 1992. 49(3): p. 315–20 [DOI] [PubMed] [Google Scholar]
- 57. Bogduk N., Govind J., Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment. Lancet Neurol, 2009. 8(10): p. 959–68 [DOI] [PubMed] [Google Scholar]
- 58. Martelletti P., et al. , Epidural corticosteroid blockade in cervicogenic headache. Eur Rev Med Pharmacol Sci, 1998. 2(1): p. 31–6 [PubMed] [Google Scholar]
- 59. Zhou L., et al. , Upper cervical facet joint and spinal rami blocks for the treatment of cervicogenic headache. Headache, 2010. 50(4): p. 657–63 [DOI] [PubMed] [Google Scholar]
- 60. Zhang J., Shi D.S., Wang R., Pulsed radiofrequency of the second cervical ganglion (C2) for the treatment of cervicogenic headache. J Headache Pain, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Fleming R., Forsythe S., Cook C., Influential variables associated with outcomes in patients with cervicogenic headache. J Man Manip Ther, 2007. 15(3): p. 155–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Provinciali L., et al. , Multimodal treatment to prevent the late whiplash syndrome. Scand J Rehabil Med, 1996. 28(2): p. 105–11 [PubMed] [Google Scholar]
- 63. Haspeslagh S.R., et al. , Randomised controlled trial of cervical radiofrequency lesions as a treatment for cervicogenic headache [ISRCTN07444684]. BMC Anesthesiol, 2006. 6: p. 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Farina S., et al. , Headache and cervical spine disorders: classification and treatment with transcutaneous electrical nerve stimulation. Headache, 1986. 26(8): p. 431–3 [DOI] [PubMed] [Google Scholar]
- 65. Chow R.T., et al. , Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. Lancet, 2009. 374(9705): p. 1897–908 [DOI] [PubMed] [Google Scholar]
- 66. Leaver A.M., et al. , Conservative interventions provide short-term relief for non-specific neck pain: a systematic review. J Physiother, 2010. 56(2): p. 73–85 [DOI] [PubMed] [Google Scholar]
- 67. Ebneshahidi N.S., et al. , The effects of laser acupuncture on chronic tension headache—a randomised controlled trial. Acupunct Med, 2005. 23(1): p. 13–8 [DOI] [PubMed] [Google Scholar]
- 68. Enwemeka C.S., et al. , The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg, 2004. 22(4): p. 323–9 [DOI] [PubMed] [Google Scholar]
- 69. Johnson D., Phototherapy 101. 3rd edition. ed2010, Solon, Ohio: MultiRadiance Medical [Google Scholar]
- 70. Haas M., et al. , Dose response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. J Manipulative Physiol Ther, 2004. 27(9): p. 547–53 [DOI] [PubMed] [Google Scholar]
- 71. Haas M., et al. , Dose response and efficacy of spinal manipulation for chronic cervicogenic headache: a pilot randomized controlled trial. Spine J, 2010. 10(2): p. 117–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Jull G., et al. , A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine (Phila Pa 1976), 2002. 27(17): p. 1835–43; discussion 1843. [DOI] [PubMed] [Google Scholar]
- 73. Nilsson N., A randomized controlled trial of the effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther, 1995. 18(7): p. 435–40 [PubMed] [Google Scholar]
- 74. Schoensee S.K., et al. , The effect of mobilization on cervical headaches. J Orthop Sports Phys Ther, 1995. 21(4): p. 184–96 [DOI] [PubMed] [Google Scholar]
- 75. Nilsson N., Christensen H.W., Hartvigsen J., The effect of spinal manipulation in the treatment of cervicogenic headache. J Manipulative Physiol Ther, 1997. 20(5): p. 326–30 [PubMed] [Google Scholar]
- 76. D'sylva J., et al. , Manual therapy with or without physical medicine modalities for neck pain: a systematic review. Man Ther, 2010. 15(5): p. 415–33 [DOI] [PubMed] [Google Scholar]
- 77. Fernandez-de-Las-Penas C., et al. , Spinal manipulative therapy in the management of cervicogenic headache. Headache, 2005. 45(9): p. 1260–3 [DOI] [PubMed] [Google Scholar]
- 78. Gross A., et al. , Manipulation or mobilisation for neck pain: a Cochrane Review. Man Ther, 2010. 15(4): p. 315–33 [DOI] [PubMed] [Google Scholar]
- 79. Miller J., et al. , Manual therapy and exercise for neck pain: A systematic review. Man Ther, 2010 [DOI] [PubMed] [Google Scholar]
- 80. Lewit K., Simons D.G., Myofascial pain: relief by post-isometric relaxation. Arch Phys Med Rehabil, 1984. 65(8): p. 452–6 [PubMed] [Google Scholar]
- 81. Porterfield J.A., DeRosa C., Mechanical neck pain: perspectives in functional anatomy 1995, Philadelphia, PA: WB Saunders [Google Scholar]
- 82. Hack G.D., et al. , Anatomic relation between the rectus capitis posterior minor muscle and the dura mater. Spine (Phila Pa 1976), 1995. 20(23): p. 2484–6 [DOI] [PubMed] [Google Scholar]
- 83. Ylinen J., et al. , Effect of neck exercises on cervicogenic headache: a randomized controlled trial. J Rehabil Med, 2010. 42(4): p. 344–9 [DOI] [PubMed] [Google Scholar]
- 84. Jull G.A., et al. , The effect of therapeutic exercise on activation of the deep cervical flexor muscles in people with chronic neck pain. Man Ther, 2009. 14(6): p. 696–701 [DOI] [PubMed] [Google Scholar]
- 85. Cagnie B., et al. , The use of functional MRI to evaluate cervical flexor activity during different cervical flexion exercises. J Appl Physiol, 2008. 104(1): p. 230–5 [DOI] [PubMed] [Google Scholar]
- 86. Falla D., et al. , Further evaluation of an EMG technique for assessment of the deep cervical flexor muscles. J Electromyogr Kinesiol, 2006. 16(6): p. 621–8 [DOI] [PubMed] [Google Scholar]
- 87. O'Leary S., et al. , Specific therapeutic exercise of the neck induces immediate local hypoalgesia. J Pain, 2007. 8(11): p. 832–9 [DOI] [PubMed] [Google Scholar]
- 88. O'Leary S., et al. , Muscle specificity in tests of cervical flexor muscle performance. J Electromyogr Kinesiol, 2007. 17(1): p. 35–40 [DOI] [PubMed] [Google Scholar]
- 89. Ask T., Strand L.I., Skouen J.S., The effect of two exercise regimes; motor control versus endurance/strength training for patients with whiplash-associated disorders: a randomized controlled pilot study. Clin Rehabil, 2009. 23(9): p. 812–23 [DOI] [PubMed] [Google Scholar]
- 90. Ylinen J., et al. , Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA, 2003. 289(19): p. 2509–16 [DOI] [PubMed] [Google Scholar]
- 91. Vassiliou T., et al. , Physical therapy and active exercises—an adequate treatment for prevention of late whiplash syndrome? Randomized controlled trial in 200 patients. Pain, 2006. 124(1–2): p. 69–76 [DOI] [PubMed] [Google Scholar]
- 92. van Ettekoven H., Lucas C., Efficacy of physiotherapy including a craniocervical training programme for tension-type headache; a randomized clinical trial. Cephalalgia, 2006. 26(8): p. 983–91 [DOI] [PubMed] [Google Scholar]
- 93. Gross A.R., et al. , Knowledge to action: a challenge for neck pain treatment. J Orthop Sports Phys Ther, 2009. 39(5): p. 351–63 [DOI] [PubMed] [Google Scholar]
- 94. Andersen L.L., et al. , Effect of brief daily exercise on headache among adults - secondary analysis of a randomized controlled trial. Scand J Work Environ Health, 2011 [DOI] [PubMed] [Google Scholar]
- 95. Ylinen J., Physical exercises and functional rehabilitation for the management of chronic neck pain. Eura Medicophys, 2007. 43(1): p. 119–32 [PubMed] [Google Scholar]
- 96. Randlov A., et al. , Intensive dynamic training for females with chronic neck/shoulder pain. A randomized controlled trial. Clin Rehabil, 1998. 12(3): p. 200–10 [DOI] [PubMed] [Google Scholar]
- 97. Kristjansson E., Treleaven J., Sensorimotor function and dizziness in neck pain: implications for assessment and management. J Orthop Sports Phys Ther, 2009. 39(5): p. 364–77 [DOI] [PubMed] [Google Scholar]